Abstract
Purpose
Although eliminating health disparities by race, ethnicity, and socioeconomic status (SES) is a top public health priority internationally and in the United States, weight-related racial/ethnic and SES disparities persist among adults and children in the United States. Few studies have examined how these disparities have changed over time; these studies are limited by the reliance on rate differences or ratios to measure disparities. We sought to advance existing research by using a set of disparity metrics on both the absolute and relative scales to examine trends in childhood obesity disparities over time.
Methods
Data from 7066 children, ages 2 to 18 years, in the National Health and Nutrition Examination Surveys were used to explore trends in racial/ethnic and SES disparities in pediatric obesity from 2001 to 2010 using a set of different disparity metrics.
Results
Racial/ethnic and SES-related disparities in pediatric obesity did not change significantly from 2001 to 2010 and remain significant.
Conclusions
Disparities in obesity have not improved during the past decade. The use of different disparity metrics may lead to different conclusions with respect to how disparities have changed over time, highlighting the need to evaluate disparities using a variety of metrics.
Keywords: Inequities, Inequalities, Children, Adolescents, Weight, Socioeconomic status, Measurement, Ethnic differences
Introduction
The global burden of obesity is substantial [1,2] and is projected to increase dramatically during the next 20 years [1]. Some of the greatest rates of obesity are observed in the United States, where recent estimates indicate that 17% of U.S. youth are obese (body mass index [BMI] ≥95th percentile for age and gender) [3,4], placing them at risk for high cholesterol, hypertension, depression, decreased quality of life, type 2 diabetes, and asthma [5,6]. Although the high prevalence of obesity across all age groups warrants attention, the fact that most obese children go on to become obese adults [7] highlights the importance of addressing obesity early in life.
Eliminating health disparities by race, ethnicity, and socioeconomic status (SES) is a top public health priority in the United States [8–10] and international settings [11]. However, low-income and some racial and ethnic subgroups remain more likely to suffer from a variety of diseases and health risks, including obesity and weight-related diseases [5,9,12–15]. These disparities are evident as early as the pre-school years [16–18].
There is substantial research documenting the existence of sociodemographic and economic disparities in childhood obesity; fewer studies have examined changes in disparities over time [19]. Some studies have suggested that disparities in the prevalence of obesity among youth have increased [8,19–23], whereas other research has suggested that disparities have decreased [15,24–26]. However, in previous research, the magnitude of disparities is typically quantified using rate or odds ratios (RR and OR), or rate differences (RD), with little attention given to the underlying value judgments implicit in these metrics [27].
Various disparity measures can produce results that are qualitatively and quantitatively different when the same data are examined [27,28]. Disparities can be measured on an absolute or relative scale and by weighting subpopulations equally or according to size. If the prevalence of a disease is low, disparities measured on the relative scale might appear large whereas those measured on the absolute scale might be small [28,29]. Disparities can appear to decrease over time because the better-off groups experience decreases in health or because the worse-off groups experience improvements [27]. From a public health perspective, only the latter scenario is desirable, although the metrics commonly used to assess health disparities (e.g., RR and RD) and trends over time do not capture this distinction. Other available measures of disparity are more sensitive to improvements in health among the worst-off subgroups.
Recent publications have offered guidance on more sophisticated approaches to the measurement of health disparities over time [27,28,30–32]. It is important for researchers to examine several disparity measures with an understanding of the utility and implicit values prioritized by different metrics [27,30–32]. For example, absolute metrics can provide evidence of the distribution of the disease burden across subpopulations, which may be paramount for public health practitioners and decision-makers in prioritizing what populations to target for interventions and what policies might offer the greatest return on investment. Conversely, relative indices of inequality may be of greater importance to epidemiologists interested in causal determinants and social justice advocates for whom equity is a goal in itself. Relative indices can also be compared across a variety of health indicators and outcomes, whereas absolute metrics are often not directly comparable.
More rigorous quantification of trends in disparities in childhood obesity is critical to guide the development of interventions and policies to address health disparities and to evaluate progress toward eliminating disparities. The objectives of this study were to evaluate how racial/ethnic and SES disparities in obesity among youth have changed over time using several disparity measures.
Methods
Data source and study population
Data from 2 cycles of the National Health and Nutrition Examination Surveys (NHANES), conducted in 2001–2002 and 2009–2010, were used in this analysis. NHANES is a cross-sectional survey of the civilian, noninstitutionalized U.S. population [33]. NHANES uses a complex multistage probability sampling design, with some subgroups oversampled. This study used data from 7066 children ages 2 to 18 years who completed the body measures component in the mobile examination center (MEC) of NHANES. The response rates for this age group range from approximately 85% to 88% for the 2 survey cycles. Standardized weight and height measures collected in the MEC were used to calculate age- and sex-specific BMI percentiles, according to the 2000 Centers for Disease Control and Prevention growth charts [34,35]. Children were classified as obese if they had a sex- and age-specific BMI percentile ≥95, according to criteria established by the International Task Force on Obesity [36]. Other variables include age (years), sex, race/ethnicity (non-Hispanic white, non-Hispanic black, and Mexican-American), and income-to-poverty ratio (0%–100% of federal poverty level [FPL], 101%–200% FPL, 201%–400% FPL, and >400% FPL). Children identifying as other races or ethnicities were included in the sample for analyses, but results for these groups are not reported separately because of small sample sizes.
Disparity metrics
We selected metrics that 1) give additional influence to the groups with the poorest health outcomes; 2) can assess disparities on both the relative and absolute scale; 3) can be used to evaluate ordered (i.e., SES) and unordered (i.e., racial and ethnic) groups; and 4) can be used to compare multiple groups (as opposed to pairwise comparisons between the “best” and “worst” groups, such as the RR and RD). We calculated metrics by weighting groups equally and again weighting by population size to illustrate potential differences according to each method. Weighting groups equally implies that differences between subpopulations are important regardless of the relative size of the subgroups. Population weighting, by contrast, gives all individuals equal weight and accounts for changes in the distribution of population subgroups over time. Population-weighted metrics are more robust to the instability of health status estimates among small subgroups over time [31]. The more commonly used RD and RR, in which subgroups are equally weighted also are reported for comparison.
Absolute measures
The between-group variance (BGV) summarizes the squared deviations from a population average, weighted by population size.
Where pj is group j’s population size, yj is group j’s mean health status and μ is the population average health status. The BGV is a useful metric for measuring absolute disparity for unordered groups because it is weighted by population size and is sensitive to larger deviations from the population average [37].
The absolute concentration index (ACI) is based on the relative concentration index (RCI; described in the paragraph to follow) but assesses the extent to which disease is concentrated among ranked groups on the absolute scale [32].
where RCI is the relative concentration index and μ is the population average health status. When health outcomes are expressed in terms of negative events (e.g., obesity, death), a negative ACI indicates that the most advantaged groups have better health outcomes than the least advantaged groups.
Relative measures
The index of disparity (ID) is the summed differences between several group rates and a reference rate (typically the best rate) [38], where rj is the health status of group j and J is the number of groups.
The ID weights groups equally.
The Theil index (T) and mean log deviation (MLD) are used to measure the disproportionate burden of disease across a population.
Where pj is the proportion of the population in group j and rj is the ratio of the mean health status in group j relative to the mean health status for the population. Both T and MLD are population-weighted and more sensitive to larger deviations from the population average because of the use of the logarithm (implying that reductions in inequality should ideally be achieved by improving the health status of the worst-off) [27]; T is more sensitive to changes in groups with a greater burden of disease and MLD is more sensitive to changes in groups with a greater share of the population. T and MLD are appropriate for both ordered (e.g., SES) and unordered groups (e.g., racial and ethnic subpopulations) [32].
The RCI is used to measure the degree to which disease is concentrated among ranked or ordered groups [39].
Where pj is the group’s population share, μj is the group’s mean health status, and Rj is the relative rank of the jth group:
Where pr is the cumulative share of the population up to and including group j. A negative RCI indicates that the most advantaged groups have better health outcomes than the least-advantaged groups. The concentration index is bounded by the prevalence of disease when the outcome is binary [40].
In all cases, the metrics are expressed in terms of adverse events [28]: a greater prevalence of obesity is negative. For the metrics to be comparable, they are presented as % change from the 2001–2002 and 2009–2010 survey cycles. For the RD, RR, and ID, the group with the lowest prevalence of obesity for each period was used as the reference rate: non-Hispanic white for the race/ethnicity comparison, and >400% FPL for the SES comparison.
Statistical methods
Multivariable logistic regressions were used to generate adjusted probabilities (prevalence) of obesity over survey cycles by race/ethnicity and income-to-poverty ratio (PIR), adjusted for age and gender. Stata 12SE survey commands and MEC sample weights were used to account for the complex sampling design of NHANES [41]. HD*Calc was used to generate estimates of racial/ethnic and SES disparities over time [42]. HD*Calc estimates standard errors and 95% confidence intervals for each metric at each time point, which were used to assess significance (α = 0.05). Disparity metrics were calculated weighted equally and again by subgroup population size for comparison. Because some subgroups are oversampled in NHANES, raw counts could not be used to estimate subgroup size to calculate population-weighted metrics. Therefore, weighted proportions by subgroup were calculated and multiplied by 100,000 to generate estimates of the relative subgroup size in a hypothetical sample of 100,000 persons. These estimates were used to calculate the population-weighted metrics in HD*Calc. Variance estimates accounted for the complex survey design by using Taylor series linearization. Sensitivity analyses included using crude subgroup prevalence estimates to calculate disparity metrics and comparing results to the adjusted estimates.
Results
Sociodemographic characteristics and the prevalence of obesity among children over the 2 NHANES survey cycles, 2001–2002 and 2009–2010, are listed in Table 1 [43].
Table 1.
Sociodemographic characteristics of U.S. children, 2–18 years, 2001–2010
| 2001–2002 (n = 3805) | 2009–2010 (n = 3261) | |
|---|---|---|
| Age | 9.6 (9.5–9.8) | 10.0 (9.8–10.2) |
| Female | 50.0 (48.2–51.9) | 49.0 (46.2–51.8) |
| Race or ethnicity* | ||
| Non-Hispanic white | 69.1 (63.9–74.3) | 66.4 (59.3–73.4) |
| Non-Hispanic black | 16.8 (11.4–22.3) | 16.0 (12.9–19.1) |
| Mexican-American | 14.1 (10.2–18.0) | 17.6 (10.7–24.6) |
| PIR | ||
| 0–100% FPL | 23.0 (20.4–25.5) | 23.2 (20.0–26.5) |
| 101–200% FPL | 25.1 (21.9–28.3) | 23.3 (19.9–26.6) |
| 201–400% FPL | 28.9 (26.2–31.6) | 27.6 (23.5–31.7) |
| >400% FPL | 23.0 (19.7–26.4) | 25.9 (21.4–30.4) |
| Obese (%)† | 11.5 (9.7–13.3) | 12.3 (10.9–13.7) |
CI = confidence interval; FPL = federal poverty level; PIR = income-to-poverty ratio.
Values indicate weighted means/proportions (95% CIs).
Children identifying as races or ethnicities other than those listed were included in the sample for analyses, but results are not reported for these groups due to small sample sizes.
Prevalence of obesity is based on International Task Force for Obesity cutoffs, which produce estimates lower than previous analyses using U.S. growth curve cutoffs [43].
Overall, the sample characteristics were relatively stable over time. The mean age of participating children was 9.6 in 2001–2002 and 10.0 in 2009–2010. The proportion of children identifying as Mexican-American was 14% in 2001–2002 and approximately 18% in 2009–2010. There were subtle shifts in the distribution of children across PIR categories; in 2001–2002, a greater proportion of children fell in the middle-PIR categories (101%–400% FPL), whereas in 2009–2010, the distribution was more even across the 4 PIR groups. Finally, the proportion of children classified as obese was 12.3% in 2009–2010, compared with 11.5% in 2001–2002. These estimates are lower than those reported by Ogden et al. [4] because of the use of the International Task Force on Obesity cutoffs, which have been shown to produce lower estimates of obesity prevalence compared with U.S. growth curve cutoffs or World Health Organization criteria [43].
Racial and ethnic disparities
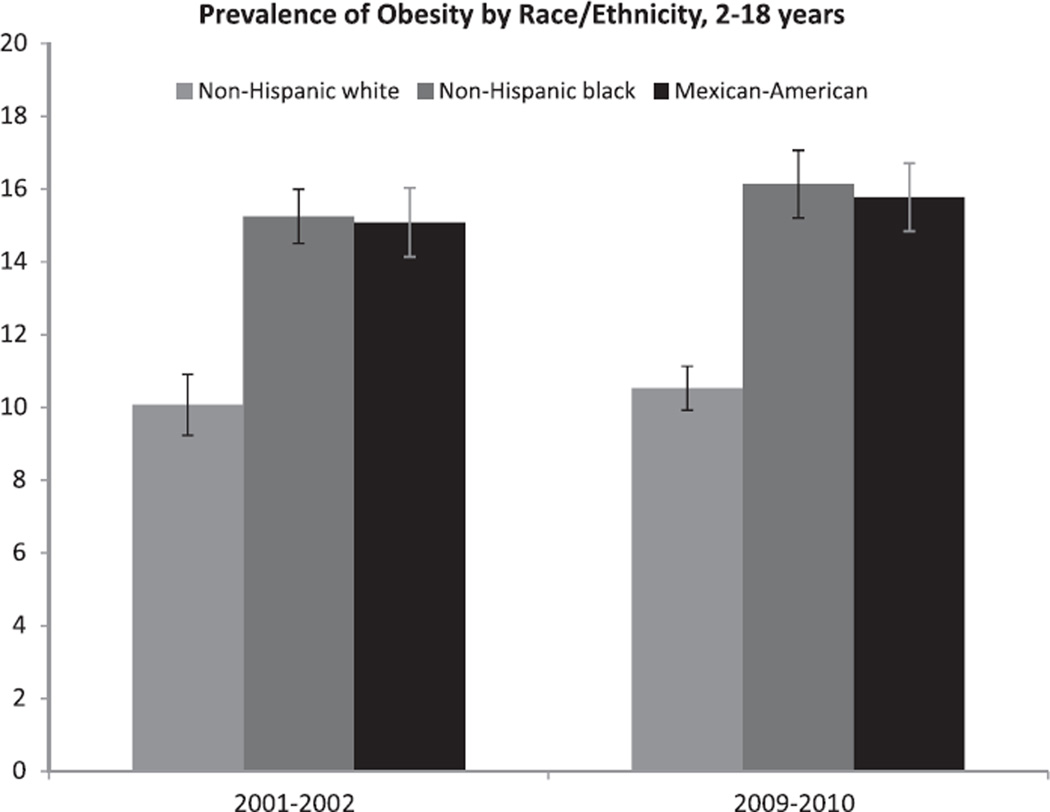
The prevalence of obesity among non-Hispanic White, non-Hispanic black and Mexican-American youth from 2001–2002 to 2009–2010 can be seen in Figure 1. The prevalence of obesity increased slightly among all groups, significantly only for non-Hispanic black youth for whom the odds of obesity was 42% greater in 2009–2010 compared with 2001–2002 (OR 1.42, 95% confidence interval 1.08–1.88).
Fig. 1.
Prevalence of obesity among non-Hispanic White, non-Hispanic black, and Mexican-American youth between 2 and 18 years, 2001–2002 and 2009–2010.
Table 2 includes the racial/ethnic disparity metric estimates over time. Across all disparity metrics, racial and ethnic disparities were statistically significant in 2001–2002 and 2009–2010. Disparities in obesity prevalence by race and ethnicity did not change significantly from 2001–2002 to 2009–2010 by any disparity metric.
Table 2.
Racial and ethnic disparities by absolute and relative metrics, 2001–2010*
| 2001–2002 Metric (95% CI) | 2009–2010 Metric (95% CI) | Absolute difference (95% CI) | |
|---|---|---|---|
| Absolute measures | |||
| RD, equal weight† | 5.2 (3.0–7.4) | 5.6 (3.2–8.0) | 0.4 (−3.7, 2.8) |
| Between-group variance, equal weight | 5.8 (1.1–10.4) | 6.6 (1.6–11.5) | 0. 8 (−7.6, 6.0) |
| Between-group variance, population weight | 5.6 (1.1–10.0) | 6.6 (1.1–11.5) | 1.0 (−7.6, 5.6) |
| Relative measures | |||
| RR, equal weight† | 1.5 (1.3–1.8) | 1.5 (1.3–1.8) | 0.0 (−0.4, 0.4) |
| Index of disparity, equal weight† | 50.6 (23.3–77.8) | 51.5 (26.3–76.7) | 0.9 (−38.1, 36.2) |
| Mean log deviation, equal weight† | 17.7 (2.5–32.9) | 18.3 (4.1–32.4) | 0.6 (−21.3, 20.2) |
| Mean log deviation, population weight | 18.8 (1.9–35.7) | 20.7 (3.7–36.3) | 1.2 (−24.7, 22.2) |
| Theil index, equal weight | 16.7 (2.9–30.5) | 17.2 (4.4–30.1) | 0.5 (−19.4, 18.4) |
| Theil index, population weight | 19.5 (1.8–37.3) | 20.7 (3.7–37.6) | 1.1 (−25.7, 23.5) |
ID = index of disparity; RD = rate difference; RR = rate ratio.
All metrics were statistically significantly different from zero (or 1, for the RR), indicating significant disparities at both time periods. There were no significant differences between time periods for any disparity metrics. Positive absolute differences indicate widening disparities across all metrics. Slight discrepancies in values between columns are due to rounding.
For the RD, RR, and ID, the reference group was non-Hispanic white; the group with the greatest prevalence of obesity was non-Hispanic black.
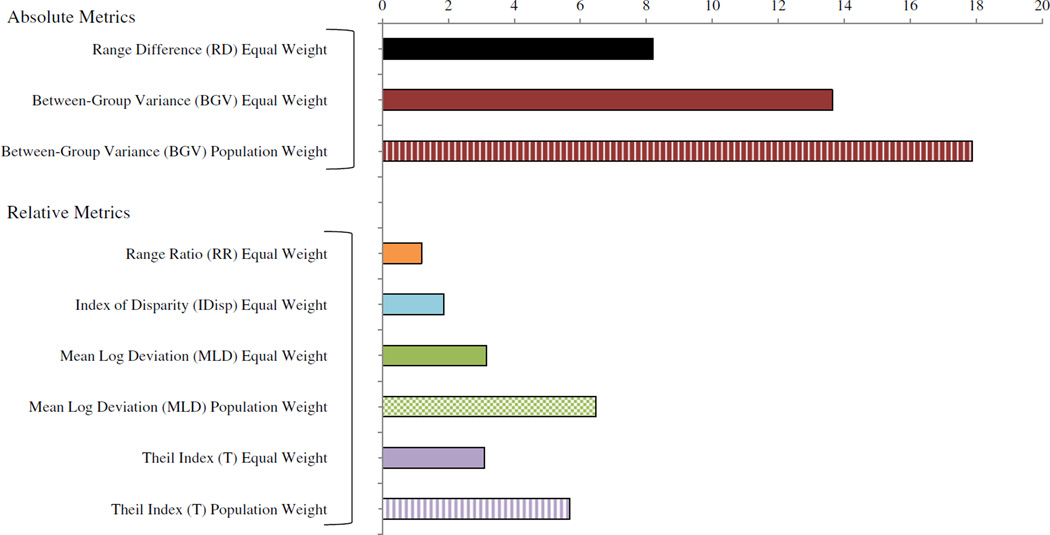
Change (%) in disparity metrics from 2001–2002 to 2009–2010 can be seen in Figure 2. Racial and ethnic disparities as measured on the absolute scale appeared to increase (not significantly) over time. Disparities as measured on the relative scale appeared to increase to a lesser extent; these changes were not statistically significant.
Fig. 2.
Change (%) in racial and ethnic disparities among youth between 2 and 18 years, 2001–2002 to 2009–2010. Increasing values on all disparity metrics indicate widening disparities.
Socioeconomic disparities
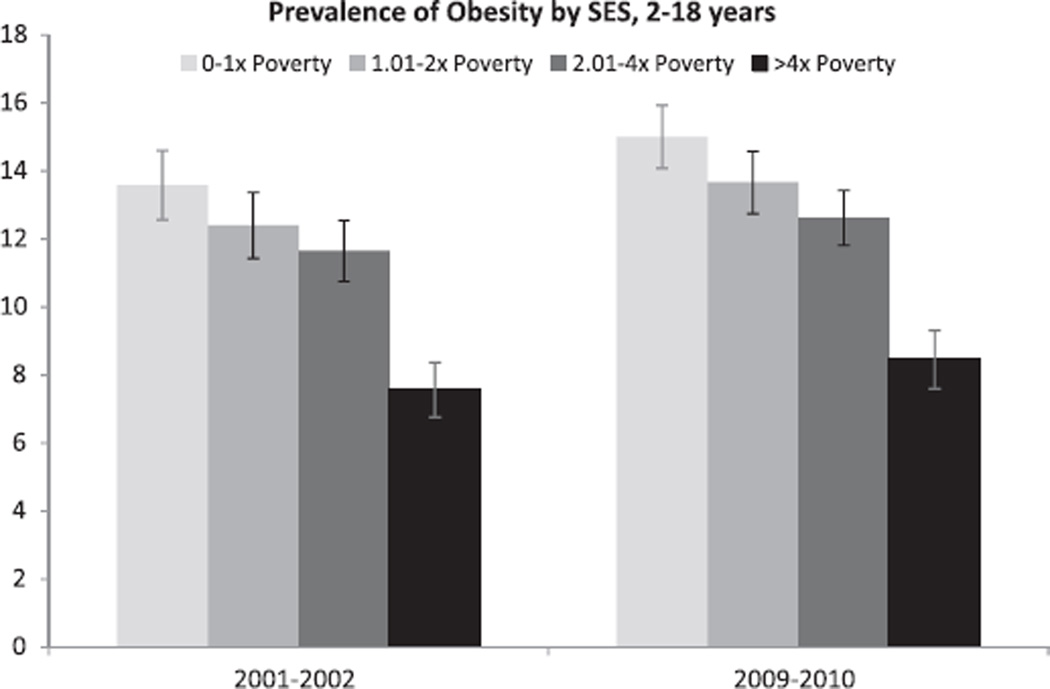
The prevalence of obesity among youth ages 2 to 18 years from 2001 to 2010 by SES can be seen in Figure 3.
Fig. 3.
Prevalence of obesity among youth between 2 and 18 years by PIR, 2001–2002 and 2009–2010.
The prevalence of obesity increased slightly among all groups, though not significantly. Table 3 includes the SES disparity metric estimates over time. Across all disparity metrics, SES disparities were statistically significant in 2001–2002 and 2009–2010.
Table 3.
SES disparities by absolute and relative metrics, 2001–2010*
| 2001–2002 Metric (95% CI) | 2009–2010 Metric (95% CI) | Absolute difference (95% CI) | |
|---|---|---|---|
| Absolute measures | |||
| Rate difference, equal weight† | 6.0 (3.5–8.6) | 6.6 (4.1–9.0) | 0.5 (−4.1, 3.0) |
| Between-group variance, equal weight | 5.1 (1.1–9.1) | 6.0 (1.7–10.3) | 0.9 (−6.8, 5.0) |
| Between-group variance, population weight | 4.7 (1.0–8.5) | 6.0 (1.7–10.3) | 1.2 (−7.0, 4.5) |
| Absolute concentration index, equal weight | −1.2 (−1.7, 0.7) | −1.3 (−1.8, 0.8) | 0.1 (−0.6, 0.8) |
| Absolute concentration index, population weight | −1.1 (−1.6, 0.6) | -1.3 (−1.8, 0.8) | 0.2 (−0.5, 0.9) |
| Relative measures | |||
| Rate ratio, equal weight† | 1.8 (1.4–2.3) | 1.8 (1.4–2.2) | 0.0 (−0.6, 0.6) |
| Index of disparity, equal weight† | 65.7 (28.2–103.3) | 62.8 (28.4–97.1) | −3.0 (−48.9, 53.9) |
| Mean log deviation, equal weight | 23.4 (4.2–42.6) | 22.3 (4.9–39.7) | −1.1 (−24.8, 27.0) |
| Mean log deviation, population weight | 21.7 (3.9–39.4) | 22.4 (4.8–40.0) | 0.8 (−25.8, 24.2) |
| Theil index, equal weight | 21.5 (4.8–38.2) | 20.6 (5.4–35.9) | −0.9 (−21.8, 23.5) |
| Theil index, population weight | 19.8 (4.4–35.3) | 20.9 (5.4–36.4) | 1.0 (−22.9, 20.8) |
| Relative concentration index, equal weight | −10.4 (−14.8, 6.0) | −10.4 (−14.3, 6.5) | 0.0 (−5.9, 5.9) |
| Relative concentration index, population weight | −9.9 (−14.2, 5.6) | −10.5 (−14.5, 6.6) | 0.6 (−5.2, 6.5) |
FPL = federal poverty level; ID = index of disparity; RD = rate difference; RR = rate ratio.
All metrics were statistically significantly different from zero (or 1, for the RR), indicating significant disparities at both time periods. There were no significant differences between time periods for any disparity metrics. Positive absolute differences indicate widening disparities across all metrics. Slight discrepancies in values between columns are due to rounding.
For the RD, RR, and ID, the reference group was >400% FPL; the group with the highest prevalence of obesity was 0–100% FPL.
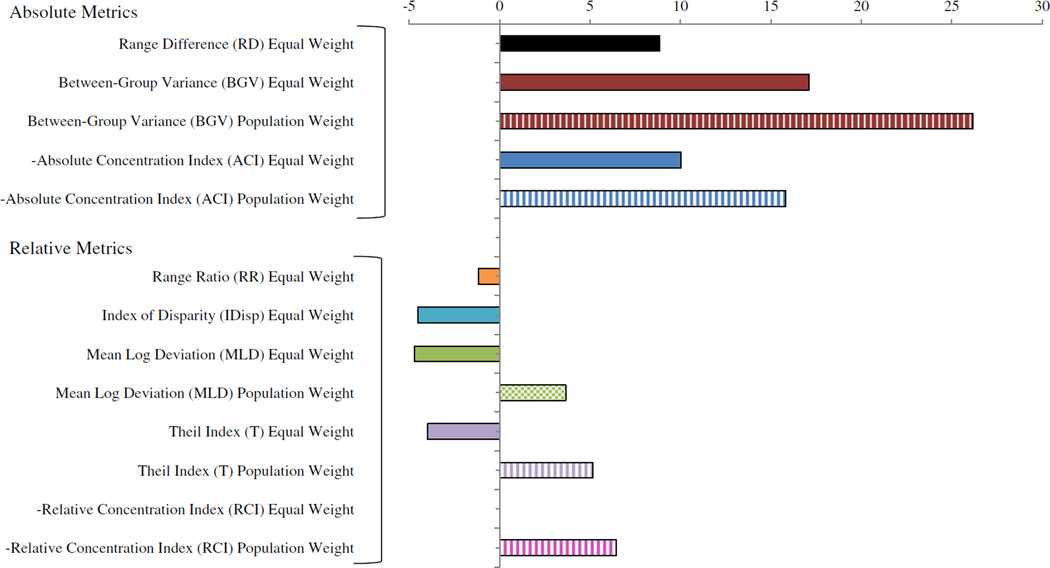
Disparities in obesity prevalence by SES did not change significantly from 2001–2002 to 2009–2010 by any disparity metric. Change (%) in SES disparity metrics from 2001–2002 to 2009–2010 can be seen in Figure 4.
Fig. 4.
Change (%) in SES disparities among youth between 2 and 18 years, 2001–2002 to 2009–2010. Increasing values on all disparity metrics indicate widening disparities; the ACI and RCI were multiplied by −1 so that increasing values would be consistent with worsening disparities.
Disparities by SES on the relative scale appeared to decrease (not significantly) based on the metrics that used equal weighting, including the RR, ID, MLD and T. Metrics that were population weighted (i.e., MLD, T, RCI) appeared to increase over time, though not significantly.
Discussion
In this study we examined changes in racial/ethnic and SES disparities in pediatric obesity in the United States during the past decade by using a variety of disparity metrics. Consistent with previous research, results suggest that significant racial/ethnic and SES disparities persist on both the relative and absolute scales. Extending previous work, our findings suggest that racial/ethnic and SES-related disparities have not changed appreciably since 2001, as assessed on both the absolute and relative scale. Previous research on how disparities in pediatric obesity have changed over time has been inconsistent, with some studies reporting increasing disparities [8,19–23] and other studies reporting decreasing disparities [15,24–26]. However, these studies are limited by the exclusive reliance on RDs or RRs. Few studies have used alternative metrics to assess disparities, and no published research to date has used multiple disparity metrics. Additionally, methodological differences across studies may have contributed to inconsistent findings.
One study used the RCI to examine trends in SES disparities in overweight among U.S. youth (10–18 years) in NHANES, from 1971 to 2002 [26]. Authors report that the pattern of changing SES-related disparities in overweight varied by racial and ethnic subgroup but that SES disparities generally decreased during the 1990s [26]. Singh et al. [19] used the ID to look at disparities in prevalence of overweight and obesity (BMI ≥85th percentile) among children 10–17 years. Authors report that between 2003 and 2007, racial/ethnic disparities increased by approximately 211%, and SES disparities increased by approximately 30%. These estimates are greater than those reported in the present study, possibly because of the use of parent-reported weight and height and the use of crude subgroup prevalence rates unadjusted for age and gender in Singh et al. [19]. The accuracy of parent-reported height and weight is inversely associated with child weight status, and these associations differ by race/ethnicity [44,45]. Thus, measures of disparities based on parent-reported height and weight could be biased.
In addition, in the present study, the use of crude subgroup prevalence rates resulted in more variable estimates of the % change in disparity metrics, which could have been a consequence of differences in the age distribution by subgroup over time. If there were a greater number of older children in the sample over time (a greater proportion of whom are obese), and this shift was differential by racial/ethnic or SES subgroup, the estimated disparities on the basis of crude rates would be confounded by the shift in the underlying age distribution. These factors could explain why racial/ethnic disparities were reported to increase by more than 200% over 4 years by Singh et al. [19].
In addition to evaluating various metrics as statistical tools with inherent strengths and limitations, the selection of disparity metrics can lead to qualitatively different answers to the question of whether health inequality is increasing or decreasing [30,31,46]. Subsequently, such choices have implications for how, or whether to address certain inequities in health. In this study, though there were no statistically significant changes over time by any metric, the magnitude and directionality of change differed between metrics that weighted subgroups equally and by population size. The greater % change in disparity metrics that were population-weighted was likely attributable to these metrics being influenced by the changing underlying population distribution of youth in various racial/ethnic or PIR categories (i.e., a greater proportion of children identified as Mexican-American in 2009–2010 compared with 2001–2002).
In addition, although SES disparities on the absolute scale uniformly increased (though not significantly), changes in SES disparities on the relative scale were mixed. The apparent increases in SES disparity metrics on the absolute scale were driven by the greater absolute increase in prevalence of obesity among youth in the lowest-income group (13.6% in 2001–2002 to 15.0% in 2009–2010) compared with youth in the highest-income group (7.6% in 2001–2002 to 8.5% in 2009–2010), although the prevalence of obesity increased among all groups. On the relative scale, the equally-weighted relative metrics appeared to decrease because the prevalence of obesity among all groups increased, thereby increasing the denominator of the relative comparisons. The population-weighted relative metrics appeared to increase because there were a greater proportion of children in the lowest- and highest-PIR groups in 2009–2010 compared with 2001–2002. Consequently, the subgroups at the extremes were given more weight in 2009–2010, resulting in apparent increases in the relative disparity metrics.
The elimination of health disparities has been a national priority for years, but disparities in pediatric obesity by race/ethnicity and SES have not improved over a decade. Although setting the elimination of health disparities on the national agenda is a first critical step, strategies to achieve this goal have not been developed and implemented on a wide enough scale to move the needle with respect to disparities at a national level. Moreover, population-based efforts to address the obesity epidemic could worsen racial/ethnic and SES disparities because the better-off groups may be more likely to benefit from population-based initiatives. For example, efforts to improve school food and physical activity environments may disproportionately benefit children attending schools with a greater level of resources.
This pattern was evident after the “Back-to-Sleep” campaign was initiated in 1994 to reduce deaths attributed to sudden infant death syndrome (SIDS). Although the campaign was effective in reducing the prevalence of SIDS overall, benefits of the initiative were not equally distributed, and disparities in SIDS widened after the campaign [47–49]. The burden of obesity affects all racial/ethnic and SES subpopulations, leading some to suggest that population-based approaches are necessary [26]. However, in developing and implementing population-based initiatives, potential effects on disparities need to be evaluated.
This study has some limitations. First, data are cross-sectional, and results could be influenced by sampling differences across survey cycles. Second, NHANES does not allow for the examination of smaller racial and ethnic subgroups such as American-Indian and Alaskan Native or those of multiple races. In addition, when stratified by age, gender, race/ethnicity, or PIR, some subgroup sizes were rather small, which may have resulted in unstable prevalence rates by survey cycle and limited power to detect statistically significant differences over time or to explore differences within groups (i.e., SES disparities within racial and ethnic subgroups, or differences by age group). We attempted to mitigate this problem by using logistic regressions to generate adjusted (marginal) estimates of the prevalence of obesity by subgroup while adjusting for age and gender. This method provided more stable estimates of the disparity metrics; however, it may have introduced additional error related to the model.
A comparison of the disparity metrics based on the crude and adjusted estimates of prevalence indicated the overall pattern was consistent, but the metrics derived from the “crude” prevalence estimates were much more variable. This additional variation is likely due to the substantial variation in the prevalence of obesity across age and gender strata, making it important to account for changes in the distribution of those characteristics. Sample size considerations precluded stratified analyses by age and gender groups, thus we chose to present disparity metric estimates based on adjusted prevalence estimates. Because of the use of adjusted estimates, findings may not be directly comparable to those based on crude prevalence.
With respect to the disparity metrics selected, because most metrics have been adapted from economic applications, they use either the population average or the “best” group’s rate as the reference. This can imply that equity is the primary goal, even if it is achieved by a reduction in health for the most advantaged group. Moreover, the more sophisticated disparity metrics lack clear interpretations regarding the magnitude of existing disparities, beyond being able to determine if the metric is significantly different from zero. More methodological research is needed on metrics that allow for comparisons to an “ideal” rate or value (e.g., Healthy People 2020 target), and on metrics that are more easily interpretable. Finally, relying solely on individual-level measures of wealth and race/ethnicity may mask differences in environments [50]. More research is needed to explore the contribution of neighborhood factors (e.g., segregation, SES) to disparities in obesity, and how disparities may vary geographically.
Despite the aforementioned limitations, this study has several strengths. This is one of the first studies to examine racial and ethnic and SES disparities in pediatric obesity over time using a nationally representative sample and multiple disparity metrics on both the absolute and relative scales. Methods and results are germane to a variety of health risks and outcomes in both the United States and international settings. Disparities by race/ethnicity and SES are complex and multi-faceted; future research needs to move beyond the reliance on a single, limited metric such as the RD or RR.
Acknowledgments
The findings and conclusions in this paper are those of the author(s) and do not necessarily represent the official position of the National Center for Health Statistics, Centers for Disease Control and Prevention.
References
- 1.Kelly T, Yang W, Chen CS, Reynolds K, He J. Global burden of obesity in 2005 and projections to 2030. Int J Obes. 2008;32(9):1431–1437. doi: 10.1038/ijo.2008.102. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Obesity: Preventing and Managing the Global Epidemic. WHO Technical Report Series 894. [accessed 07.25.12];2004 http://whqlibdoc.who.int/trs/WHO_TRS_894.pdf. [PubMed]
- 3.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 4.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daniels SR, Arnett DK, Eckel RH, Gidding SS, Hayman LL, Kumanyika S, et al. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation. 2005;111(15):1999–2012. doi: 10.1161/01.CIR.0000161369.71722.10. [DOI] [PubMed] [Google Scholar]
- 6.Lobstein T, Baur L, Uauy R. Obesity in children and young people: a crisis in public health. Obes Rev. 2004;5(Suppl. 1):4–85. doi: 10.1111/j.1467-789X.2004.00133.x. [DOI] [PubMed] [Google Scholar]
- 7.Singh AS, Mulder C, Twisk JW, van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008;9(5):474–488. doi: 10.1111/j.1467-789X.2008.00475.x. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. CDC health disparities and inequalities report –United States, 2011. MMWR. 2011;60(Suppl.):1–113. [PubMed] [Google Scholar]
- 9.U.S. Department of Health and Human Services. Washington (DC): Government Printing Office; 2000. Healthy people 2010: understanding and improving Health. [Google Scholar]
- 10.U.S. Department of Health and Human Services. Washington (DC): Government Printing Office; 2010. Healthy people 2020: improving the health of Americans. [Google Scholar]
- 11.World Health Organization. Geneva, Switzerland: WHO Press; 2010. [accessed 07.25.12]. Equity, Social Determinants and Public Health Programmes. http://whqlibdoc.who.int/publications/2010/9789241563970_eng.pdf. [Google Scholar]
- 12.Deitel M. The Surgeon-General’s call to action to prevent an increase in overweight and obesity. Obes Surg. 2002;12:3–4. doi: 10.1381/096089202321144487. [DOI] [PubMed] [Google Scholar]
- 13.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291(23):2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 14.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA. 2002;288(14):1728–1732. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 15.Wang Y, Beydoun MA. The obesity epidemic in the United States–gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 16.Anderson SE, Whitaker RC. Prevalence of obesity among US preschool children in different racial and ethnic groups. Arch Pediatr Adolesc Med. 2009;163(4):344–348. doi: 10.1001/archpediatrics.2009.18. [DOI] [PubMed] [Google Scholar]
- 17.Howe LD, Tilling K, Galobardes B, Smith GD, Ness AR, Lawlor DA. Socioeconomic disparities in trajectories of adiposity across childhood. Int J Pediatr Obes. 2011;6(2–2):e144–e153. doi: 10.3109/17477166.2010.500387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Y. Disparities in pediatric obesity in the United States. Adv Nutr. 2011;2:23–31. doi: 10.3945/an.110.000083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singh GK, Siahpush M, Kogan MD. Rising social inequalities in US childhood obesity, 2003–2007. Ann Epidemiol. 2010;20(1):40–52. doi: 10.1016/j.annepidem.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 20.Bethell C, Simpson L, Stumbo S, Carle AC, Gombojav N. National, state, and local disparities in childhood obesity. Health Affairs. 2010;29(3):347–356. doi: 10.1377/hlthaff.2009.0762. [DOI] [PubMed] [Google Scholar]
- 21.Beydoun MA, Wang Y. Socio-demographic disparities in distribution shifts over time in various adiposity measures among American children and adolescents: what changes in prevalence rates could not reveal. Int J Pediatr Obes. 2010;6:21–35. doi: 10.3109/17477166.2010.488693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miech RA, Kumanyika SK, Stettler N, Link BG, Phelan JC, Chang VW. Trends in the association of poverty with overweight among US adolescents, 1971–2004. JAMA. 2006;295(20):2385–2393. doi: 10.1001/jama.295.20.2385. [DOI] [PubMed] [Google Scholar]
- 23.Stamatakis E, Wardle J, Cole TJ. Childhood obesity and overweight prevalence trends in England: evidence for growing socioeconomic disparities. Int J Obes. 2010;34:41–47. doi: 10.1038/ijo.2009.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brunt H, Lester N, Davies G, Williams R. Childhood overweight and obesity: is the gap closing the wrong way? J Public Health. 2008;30(2):145–152. doi: 10.1093/pubmed/fdn010. [DOI] [PubMed] [Google Scholar]
- 25.Wang Y, Zhang Q. Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. Am J Clin Nutr. 2006;84(4):707–716. doi: 10.1093/ajcn/84.4.707. [DOI] [PubMed] [Google Scholar]
- 26.Zhang Q, Wang Y. Using concentration index to study changes in socioeconomic inequality of overweight among US adolescents between 1971 and 2002. Int J Epidemiol. 2007;36(4):916–925. doi: 10.1093/ije/dym064. [DOI] [PubMed] [Google Scholar]
- 27.Harper S, King NB, Meersman SC, Reichman ME, Breen N, Lynch J. Implicit value judgments in the measurement of health inequalities. Milbank Q. 2010;88(1):4–29. doi: 10.1111/j.1468-0009.2010.00587.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Keppel K, Pamuk E, Lynch J, Carter-Pokras O, Kim I, Mays V, et al. Methodological issues in measuring health disparities. Vital Health Stat 2. 2005;141:1–16. [PMC free article] [PubMed] [Google Scholar]
- 29.Keppel KG, Pearcy JN, Klein RJ. Statistical notes, no. 25. Hyattsville, MD: National Center for Health Statistics; 2004. Measuring progress in Healthy People 2010; pp. 1–16. [PubMed] [Google Scholar]
- 30.Harper S, Lynch J. Methods for measuring cancer disparities: using data relevant to Healthy People 2010 cancer-related objectives. Bethesda (MD): National Cancer Institute; 2005. [Google Scholar]
- 31.Harper S, Lynch J. Selected comparisons of measures of health disparities: a review using databases relevant to Healthy People 2010 cancer-related objectives. Bethesda (MD): National Cancer Institute; 2007. [Google Scholar]
- 32.Harper S, Lynch J, Meersman SC, Breen N, Davis WW, Reichman ME. An overview of methods for monitoring social disparities in cancer with an example using trends in lung cancer incidence by area-socioeconomic position and race-ethnicity, 1992–2004. Am J Epidemiol. 2008;167(8):889–899. doi: 10.1093/aje/kwn016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.National Center for Health Statistics. National Health and Nutrition Examination Survey: Questionnaires, datasets, and related documentation. [accessed 25.07.12]; http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.
- 34.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data. 2000;(314):1–27. [PubMed] [Google Scholar]
- 35.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11. 2002;246:1–190. [PubMed] [Google Scholar]
- 36.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320(7244):1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chakravarty SR. The variance as a subgroup decomposable measure of inequality. Soc Indic Res. 2001;53:79–95. [Google Scholar]
- 38.Pearcy JN, Keppel KG. A summary measure of health disparity. Public Health Rep. 2002;117(3):273–280. doi: 10.1016/S0033-3549(04)50161-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kakwani N, Wagstaff A, vanDoorslaer E. Socioeconomic inequalities in health: measurement, computation, and statistical inference. J Econometrics. 1997;77:87–103. [Google Scholar]
- 40.Wagstaff A. The bounds of the concentration index when the variable of interest is binary, with an application to immunization inequality. Health Econ. 2005;14(4):429–432. doi: 10.1002/hec.953. [DOI] [PubMed] [Google Scholar]
- 41.StataCorp. Stata Statistical Software. Release 12. College Station, TX: StataCorp LP; 2011. [Google Scholar]
- 42.Division of Cancer Control and Population Sciences, Surveillance Research Program and Applied Research Program; National Cancer Institute. [accessed 25.07.12];Health Disparities Calculator. 2011 http://seer.cancer.gov/hdcalc/
- 43.Shields M, Tremblay MS. Canadian childhood obesity estimates based on WHO, IOTF and CDC cut-points. Int J Pediatr Obes. 2010;5(3):265–273. doi: 10.3109/17477160903268282. [DOI] [PubMed] [Google Scholar]
- 44.Akinbami LJ, Ogden CL. Childhood overweight prevalence in the United States: the impact of parent-reported height and weight. Obesity. 2009;17(8):1574–1580. doi: 10.1038/oby.2009.1. [DOI] [PubMed] [Google Scholar]
- 45.O’Connor DP, Gugenheim JJ. Comparison of measured and parents’ reported height and weight in children and adolescents. Obesity. 2011;19(5):1040–1046. doi: 10.1038/oby.2010.278. [DOI] [PubMed] [Google Scholar]
- 46.Asada Y. Health inequality: morality and measurement. Toronto: University of Toronto Press Inc; 2007. [Google Scholar]
- 47.Corwin MJ, Lesko SM, Heeren T, Vezina RM, Hunt CE, Mandell F, et al. Secular changes in sleep position during infancy, 1995–1998. Pediatrics. 2003;111(1):52–60. doi: 10.1542/peds.111.1.52. [DOI] [PubMed] [Google Scholar]
- 48.Hunt CE, Hauck FR. Sudden infant death syndrome. CMAJ. 2006;174(13):1861–1869. doi: 10.1503/cmaj.051671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pickett KE, Luo Y, Lauderdale DS. Widening social inequalities in risk for sudden infant death syndrome. Am J Public Health. 2005;95(11):1976–1981. doi: 10.2105/AJPH.2004.059063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhang Q, Wang Y. Socioeconomic inequality of obesity in the United States: do gender, age, ethnicity matter? Soc Sci Med. 2004;58(6):1171–1180. doi: 10.1016/s0277-9536(03)00288-0. [DOI] [PubMed] [Google Scholar]