Abstract
We surveyed 700 veterans who were outpatients in a non–Veterans Affairs (VA) multihospital system. Our objective was to assess the prevalence of mental disorders and service use among these veterans. The majority were Vietnam veterans (72.0%), and male (95.9%), and 40.4% reported recently using the VA for care. The prevalence of lifetime post-traumatic stress disorder (PTSD) was 9.6%, lifetime depression 18.4%, and lifetime mental health service use 50.1%. In multivariate analyses, significant factors associated with PTSD, depression, and mental health service use were low self-esteem, use of alcohol/drugs to cope, history of childhood adversity, high combat exposure, and low psychological resilience. VA service use was associated with greater mental health service use and combat exposure. With the exception of alcohol misuse, the mental health status of veterans seen in non-VA facilities appeared to be better than reported in past studies. Because most veterans have access to both VA and non-VA services, these findings have implications for veterans and outcomes research.
Keywords: Postdeployment health, post-traumatic stress disorder, depression, alcohol misuse, service use, combat exposure, psychosocial factors, social work
INTRODUCTION
The objective of the current study is to assess the prevalence of mental health disorders and variations in service use among previously deployed U.S. veterans seen in non-Veterans Affairs (VA) health systems. This study is important because the majority of veterans today have private health insurance and/or Medicare coverage and receive some or all their care from non-VA institutions (Carey et al., 2008; Elbogen et al., 2013; Liu et al., 2010; Liu et al., 2011; Shen, Hendricks, Zhang, & Kazis, 2003; Trivedi et al., 2012; U.S. Department of Veterans Affairs, 2002; U.S. Department of Veterans Affairs, 2010). In addition, given current policy changes (Leider, Castrucci, Russo, & Hearne, 2015), the availability of health care options for veterans will likely increase, so non-VA health services research will be needed for service planning. Given the service options available for veterans today and the ongoing nature of contemporary defense and warfighting, there are few definitive data sources related to service use and health status for veterans (Boscarino, 2007). However, with the widespread use of electronic health records (EHRs), veteran status information can be routinely captured in most non-VA health care systems. The knowledge gained from studying veterans in non-VA health care systems is important for monitoring the quality of care and for outcomes research beyond the VA health care system (Boscarino, Sitarik, et al., 2014).
Previous studies of Vietnam veterans suggested high rates of post-traumatic stress disorder (PTSD) and other mental conditions among these former service members (Kulka et al., 1990b). While subsequent studies suggested that these estimates may have been high, a significant proportion of these veterans, perhaps as high as 15%, appear to be impaired by combat-related trauma (Dohrenwend et al., 2006). Similarly, initial research related to service in Afghanistan and Iraq suggests that significant numbers of military personnel developed mental health disorders following their deployments (Hoge et al., 2004). Current research suggests that the prevalence of PTSD may be as high as 15% among these recent service members (Booth-Kewley, Larson, Highfill-McRoy, Garland, & Gaskin, 2010), although some estimates have been lower (Kok, Herrell, Thomas, & Hoge, 2012). While the reported prevalence of PTSD and related disorders among deployed U.S. veterans has varied depending on the assessment method and service era studied, it generally has been reported to be about 10% to 15% (Dohrenwend et al., 2006; LeardMann et al., 2009; Stimpson, Thomas, Weightman, Dunstan, & Lewis, 2003)—sufficiently prevalent to be of public health concern (Levy & Sidel, 2009; Spelman, Hunt, Seal, & Burgo-Black, 2012). Given the research noted, our hypothesis was that the prevalence of mental disorders among veterans in the current study be would similar to that reported in recent community studies.
Our current study was guided by a “psychosocial-stressor” model used in previous research (Boscarino, 1995; Boscarino, Hoffman, Adams, Figley, & Solhkhah, 2014; Hobfoll & Lerman, 1988). This model suggests that the availability of psychosocial resources and risk factors in the pre- and posttrauma periods affect reactions to environmental stressors and, thus, the onset of health problems and/or initiation of treatment seeking in the posttrauma period (Adams, Boscarino, & Galea, 2006; James, Van Kampen, Miller, & Engdahl, 2013; Yamashita, 2012). This model is consistent with the “stressor-strain” model used in contemporary military research (Adler & Castro, 2013). As in past research, this psychosocial-stressor model guided our study design, instrument selection, and data analysis approach (Boscarino, Adams, & Figley, 2004; Rosen et al., 2012). This analytical model has utility in health research conducted among veterans, and other trauma-exposed populations, because it facilitates intervention-focused strategies based on a robust psychosocial knowledge base in behavioral health (Adams et al., 2006; Boscarino, Hoffman, et al., 2014; Boscarino, Lu, et al., 2015; Rosen et al., 2012; Yamashita, 2012).
METHODS
Participants
For the current study, using a computer-generated algorithm we recruited a random sample of community-based U.S. military veterans, ages 18 to 74, who were outpatients in the Geisinger Health System (GHS). Geisinger collects veteran status information on all adult patients, which is stored in EHRs. Altogether, 700 previously deployed veterans were recruited for diagnostic interviews using EHRs. With patient consent, trained and supervised interviewers recruited veterans and administered structured diagnostic interviews by telephone in December 2011 and January 2012. Interviews were conducted in English, and those who were institutionalized or incapable of completing a 50-minute interview were excluded. All veterans recruited reported at least one warzone deployment. This research project was approved by the Institutional Review Board (IRB) of GHS.
Study Setting
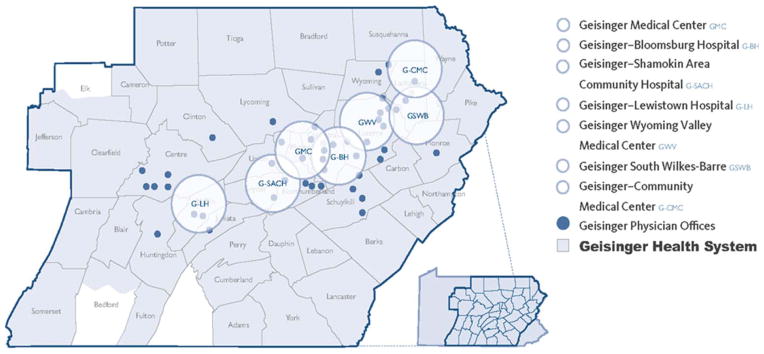
This study was conducted among outpatients at GHS. Geisinger is a large, integrated health care organization in Pennsylvania and one of largest integrated health services organizations in the United States involved in public health research (Moorman et al., 2013). This system serves more than 3 million residents throughout 44 counties in central, south central, and northeast Pennsylvania. Geisinger is physician led and composed of 21,500 employees, including a 1,000-member multispecialty group practice, eight hospital campuses, two research centers, and a 467,000-member health plan (see http://www.geisinger.org). Geisinger has a large social work staff, which is typical of health care systems in the United States (Beder, 2006). Approximately 40,000 of Geisinger’s patients are current or former U.S. service members. Thus, Geisinger is essentially the equivalent of a large Veterans Integrated Service Network (VISN) in the VA system for veterans residing in central and northeastern Pennsylvania (see Figure 1).
FIGURE 1.
Geisinger Health System’s service area, hospitals, and outpatient clinics in Pennsylvania.
Study Measures
Assessment of PTSD, depression, and alcohol misuse
To assess PTSD, we used a diagnostic instrument based on the American Psychiatric Assoication’s Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), which was originally developed for the National Women’s Study (NWS) and has been used in other trauma studies (Boscarino, Galea, et al., 2004; Boscarino, Adams, & Figley, 2011; Galea et al., 2002; Resnick, Kilpatrick, Dansky, Saunders, & Best, 1993). To meet criteria for PTSD, veterans had to meet the full DSM-IV PTSD diagnostic criteria (A through F) for this disorder. To date, the NWS instrument has been used in a number of national and regional trauma studies (Boscarino, Galea, et al., 2004; Boscarino, Adams, & Figley, 2011; Galea et al., 2002; Resnick et al., 1993) and has been validated using the Structured Clinical Interview for DSM (SCID) (Kilpatrick et al., 1998). Cronbach’s alpha for this scale in the current study was 0.918.
Depression was assessed using a version of SCID’s major depressive disorder scale, consistent with the DSM-IV criteria and also used in other the national studies (Acierno et al., 2000). This measure has also been used in telephone-based surveys of trauma survivors (Boscarino, Galea, et al., 2004; Boscarino, Adams, & Figley, 2011; Galea et al., 2002; Resnick et al., 1993). Data related to the validity of this depression scale were previously reported and suggest that this scale can diagnose depression in population studies (Boscarino, Galea, et al., 2004; Kilpatrick et al., 2003). To meet criteria in the current study, subjects had to meet the criteria for depression for lifetime and/or for the past 12 months.
Alcohol misuse was assessed by two measures: one measured alcohol dependence symptoms in the past 12 months and the other measured heavy alcohol use in the past 30 days (Allen & Columbus, 1995; O’Brien, 2008). For alcohol consumption, we asked respondents to report the number of days they consumed alcohol in the past month and then the number of drinks they drank on the days they consumed alcohol (Boscarino, Kirchner, Hoffman, Sartorius, & Adams, 2011). Those who consumed 40 or more drinks in the past month (11.9%) were classified as heavy drinkers. We also inquired about alcohol misuse based on the CAGE Questionnaire (King, 1986), a widely used and validated measure of alcohol dependence symptoms (O’Brien, 2008). Those who reported two or more CAGE symptoms in the past 12 months (e.g., thought they should cut down on drinking, criticized about drinking) were classified as having probable alcohol dependence.
Assessment of mental health service utilization
Mental health service use was assessed using survey instruments from the National Comorbidity Study (Kessler et al., 1999). These instruments have been extensively used in previous mental health studies (Boscarino, Adams, et al., 2004; Boscarino, Galea, et al., 2004; Boscarino, Adams, & Figley, 2011). For these measures, we asked participants about receiving any counseling from helping professionals or self-help groups, such as a psychiatrist, a counselor, a physician, or Alcoholics Anonymous, for problems with emotions, nerves, or the use of alcohol or drugs. Previous reports related to the reliability and validity of these measures have been reported elsewhere and suggest that these are good measures of mental health service utilization (Boscarino, Adams, et al., 2004; Boscarino, Galea, et al., 2004; Boscarino, Adams, & Figley, 2011).
Assessment of mental health risk and protective factors
Potential mental health risk and protective factors assessed included demographic factors (age, gender, race, marital status, education, and employment status), warzone deployments, combat exposure, self-esteem, use of drugs/ alcohol to cope postdeployment, exposure to adverse childhood events, and psychological resilience, all derived from the survey instrument. As suggested, our study was guided by a psychosocial-stress approach used in previous studies, which is focused on the availability of psychosocial resources in the pre- and posttrauma periods and the impact of environmental factors in the onset and course of mental disorders and treatment seeking (Adams et al., 2006; Adams & Boscarino, 2011; Rosen et al., 2012; Yamashita, 2012). Warzone exposure was based on self-report and included the Korean war, Vietnam war, Persian Gulf war, Afghanistan/Iraq war, and “other” warzone deployments as currently defined by the VA (http://www.va.gov). Combat exposure was based on a version of the Combat Experience Scale, a widely used and validated measure of combat exposure (Hoge et al., 2004; Janes, Goldberg, Eisen, & True, 1991). Versions of this scale have been used in military health studies since the Vietnam war period (Boscarino, 1995). Cronbach’s alpha for this exposure scale in the current study was 0.806.
Self-esteem was measured by a 5-item version of the Rosenberg Scale (e.g., feel like a person of worth, certainly feel useless at times), a scale widely used in previous trauma studies (Boscarino & Adams, 2009; Boscarino, Hoffman, et al., 2014). The reliability and validity of this scale is reported to be good (Robinson, Shaver, & Wrightsman, 1991; Sinclair et al., 2010). Cronbach’s alpha for this scale in the current study was 0.721.
For use of alcohol/drugs to cope postdeployment, we used the drug and alcohol items from the brief coping scale (BCS) (e.g., “Since your warzone service, have you been doing the following: using alcohol or other drugs to make you feel better?”). The BCS is a widely used, validated measure of coping used in previous research (Carver, 1997). Cronbach’s alpha for this sub-scale in the current study was 0.909. For adverse childhood events, we included a valid and reliable 12-item scale used in past studies: the Adverse Childhood Events (ACE) scale (Binder et al., 2008; Dong et al., 2004). Items in this scale asked respondents to report how often as a child did a parent hit them, how often they went hungry, and the like. Cronbach’s alpha for this scale in the current study was 0.842.
Finally, for psychological resilience we used the 5-item version of the Connor-Davidson Resilience Scale (CD-RISC) (Campbell-Sills & Stein, 2007). Items in this measure included reports related to being able to adapt to change, having a strong sense of purpose, and so on. CD-RISC has been extensively used in clinical research and is reported to be a valid and reliable measure of psychological resilience (Connor & Davidson, 2003). Cronbach’s alpha for the CD-RISC scale in the current study was 0.796.
Data Analyses
Statistical analyses include descriptive statistics and analyses assessing the association between mental health status and potential risk/protective factors. Based on previous research, scale measures for combat exposure, childhood adversity, self-esteem, and psychological resilience were categorized into clinical cut points described in detail elsewhere (Adams & Boscarino, 2015; Adams et al., 2006; Adams & Boscarino, 2011; Boscarino, 1995; Boscarino, Galea, et al., 2004). For multivariate analyses, we used logistic regression, whereby key risk/protective factors (e.g., self-esteem, resilience, adversity, combat exposure) were used to estimate the likelihood (i.e., odds ratios [ORs]) for PTSD, depression, and mental health service utilization, respectively, controlling for age, gender, marital status, level of education, and other factors that might confound these associations by including the latter in the analyses. All the variables shown in the final multivariate models are included in the analyses presented in Tables 1 through 4. Because our analysis was cross-sectional and some of the outcomes assessed were likely associated with the predictor variable (e.g., alcohol dependence and use of alcohol/drugs to cope postdeployment), we assessed several measures for collinearity to avoid reporting spurious findings and report these results. Next, we tabulated VA service use by mental health status to assess this association, as shown in Table 5. In the Discussion section of the article, we also compared study results to those of similar populations of veterans and nonveterans using the comparable assessment methods (Boscarino et al., 2012; Pietrzak & Cook, 2013). Analyses were conducted using Stata, version 13.1 software (Stata Corporation, 2013).
TABLE 1.
Profile of Deployed Veterans in Veterans Cohort Study (N = 700)
| Study Variable | N | % or Mean | 95% CI |
|---|---|---|---|
| Age (mean) | 700 | 58.9 | 58.1–59.7 |
| Male gender | 671 | 95.9 | 94.1–97.1 |
| White race | 653 | 93.3 | 91.2–94.9 |
| Married | 557 | 79.6 | 76.4–82.4 |
| Some college or higher | 399 | 57.0 | 53.3–60.6 |
| Employed | 313 | 44.7 | 41.1–48.4 |
| OEF/OIF veteran | 96 | 13.7 | 11.4–16.5 |
| Served multiple combat tours | 200 | 28.6 | 25.3–32.0 |
| High combat exposure | 148 | 21.1 | 18.3–24.3 |
| Ever used VA health care services | 354 | 50.6 | 46.9–54.3 |
| Currently use VA health care services | 283 | 40.4 | 36.8–44.2 |
| Ever used mental health counseling services | 351 | 50.1 | 46.4–53.9 |
| Used mental health counseling services—past year | 153 | 21.9 | 18.9–25.1 |
| Lifetime major depression | 129 | 18.4 | 15.7–21.5 |
| Major depression—past year | 44 | 6.2 | 4.7–8.3 |
| Lifetime PTSD | 67 | 9.6 | 7.6–12.0 |
| PTSD—past year | 47 | 6.7 | 5.1–8.8 |
| Alcohol Dependence—past year | 87 | 12.4 | 10.2–15.1 |
| Heavy drinking—past month | 83 | 11.9 | 9.6–14.5 |
| Low self-esteem | 195 | 27.9 | 24.7–31.3 |
| Used alcohol/drugs to cope postdeployment | 95 | 13.6 | 11.2–16.3 |
| History of high childhood adversity | 133 | 19.0 | 16.3–22.1 |
| Low psychological resilience | 149 | 21.3 | 18.4–24.5 |
Note. Study veterans included Vietnam (72.0%), Gulf (9.7%), Afghanistan/Iraq (13.7%), and other warzone veterans (4.6%). Service branches included Air Force (21.3%), Army (55.4%), Navy (10.6%), and Marines (12.0%). EF/OIF = Operation Enduring Freedom/Operation Iraqi Freedom; PTSD = post-traumatic stress disorder; VA = Veterans Affairs.
TABLE 4.
Multivariate Logistic Regressions Predicting Current Alcohol Dependence/Heavy Use
| Variables a | Current Dependence OR (95% CI) p Value |
Current Heavy Use OR (95% CI) p Value |
|---|---|---|
| Age (years) | 0.97 (0.94–1.01) 0.093 | 0.99 (0.95–1.02) 0.470 |
| Male gender | 2.26 (0.55–9.19) 0.458 | 1.93 (0.373–9.97) 0.433 |
| White race | 0.70 (0.28–1.78) 0.458 | 1.24 (0.42–3.62) 0.700 |
| Married | 0.66 (0.36–1.20) 0.174 | 0.64 (0.36–1.16 0.140) |
| Some college or higher | 1.69 (0.97–2.92) 0.062 | 0.91 (0.55–1.51) 0.714 |
| Employed | 1.74 (0.98–3.07) 0.057 | 1.21 (0.69–2.11) 0.501 |
| OEF/OIF veteran | 0.77 (0.28–2.11) 0.608 | 0.79 (0.26–2.37) 0.673 |
| Served multiple combat tours | 0.89 (0.50–1.58) 0.683 | 0.80 (0.44–1.43) 0.443 |
| High combat exposure | 1.13 (0.61–2.07) 0.702 | 1.61 (0.91–2.85) 0.103 |
| Low self-esteem | 1.36 (0.76–2.45) 0.303 | 0.79 (0.43–1.45) 0.449 |
| Used alcohol/drugs to cope postdeployment | 12.05 (6.84–21.21) < 0.001 | 9.14 (5.22–16.00) < 0.001 |
| History of high childhood adversity | 0.48 (0.24–0.98) 0.043 | 0.40 (0.19–0.83) 0.015 |
| Low psychological resilience | 1.18 (0.63–2.21) 0.596 | 0.86 (0.45–1.65) 0.645 |
Note. OEF/OIF = Operation Enduring Freedom/Operation Iraqi Freedom.
All variables shown are included in the logistic regression models.
TABLE 5.
Mental Health Status by History of VA Service Use (N =700)
| Study Variable | Total % (N) | Ever Used VA% (N) | Never Used VA% (N) | χ2 (p Value) | Currently Using VA% (N) | Not Currently Using VA% (N) | χ2 (p Value) |
|---|---|---|---|---|---|---|---|
| Lifetime PTSD | 9.6 (67) | 11.6 (41) | 7.5 (26) | (0.067) | 11.0 (31) | 8.6 (36) | (0.306) |
| Current PTSD | 6.7 (47) | 7.9 (28) | 5.5 (19) | (0.201) | 8.1 (23) | 5.8 (24) | (0.219) |
| Current alcohol dependence | 12.4 (87) | 13.8 (49) | 11.0 (38) | (0.252) | 12.7 (36) | 12.2 (51) | (0.847) |
| Current heavy alcohol use | 11.9 (83) | 11.6 (41) | 12.1 (42) | (0.820) | 9.5 (27) | 13.4 (56) | (0.118) |
| Lifetime depression | 18.4 (129) | 19.2 (68) | 17.6 (61) | (0.590) | 20.5 (58) | 17.0 (71) | (0.245) |
| Current depression | 6.2 (44) | 6.8 (24) | 5.8 (20) | (0.585) | 7.4 (21) | 5.5 (23) | (0.308) |
| Ever mental health counseling | 50.1 (351) | 55.1 (195) | 45.1 (156) | (0.008) | 56.9 (161) | 45.6 (190) | (0.003) |
| Current mental health counseling | 21.9 (153) | 26.3 (93) | 17.3 (60) | (0.004) | 29.3 (83) | 16.8 (70) | (< 0.001) |
| High combat exposure | 21.1 (148) | 64.2 (95) | 35.8 (53) | (< 0.001) | 56.1 (83) | 43.9 (65) | (< 0.001) |
Note. PTSD = post-traumatic stress disorder; VA = Veterans Affairs.
RESULTS
As documented elsewhere (Hoffman, Zhang, Erlich, & Boscarino, 2012), the survey cooperation rate for this survey was approximately 65%. Using the medical and demographic data in the EHRs, and with IRB approval, we examined the differences between survey respondents and nonrespondents in terms of gender, race, age, marital status, primary care physician status, employment status, smoking status, and the prevalence of major health conditions. The only significant differences found were that survey respondents tended to be younger and married (p < 0.05). In the discussion that follows, we note the potential limitations of this bias in the current study. Examination of the era status distribution of GHS veterans indicated that 72.0% were Vietnam, 9.7% Gulf War, 13.7% Afghanistan/Iraq, and 4.6% were “other” warzone veterans (refer to Table 1, bottom). The mean age of these veterans was 58.9 years (SD = 11.31); 95.9% were males; and 93.3% were classified as White. Also, 79.6% were married and 57.0% had an educational attainment that included some college or higher (Table 1). Noteworthy is that 28.6% of veterans served multiple combat tours. Furthermore, while 50.6% of GHS veterans reported ever having used the VA for health care, 40.4% reported they were currently using the VA for health care. In addition, 50.1% reported having sought mental health counseling at some time in the past, and 21.9% reported that they have sought these services within the past 12 months. The prevalence of current depression among veterans was 6.2% (95% CI = 4.7–8.3) and the prevalence of lifetime depression was 18.4% (95% CI = 15.7–21.5). The prevalence of current PTSD was 6.7% (95% CI = 5.1–8.8), and the lifetime prevalence of PTSD was 9.6% (95% CI = 7.6–12.0). Table 1 also shows factors that might have contributed to mental health status among veterans, including low self-esteem (27.9%), use of alcohol/drugs to cope postdeployment (13.6%), history of childhood adversity (19%), and low psychological resilience (21.3%).
Table 2 presents the multivariate prediction results for lifetime PTSD, depression, and lifetime mental health treatment seeking. As seen, lifetime PTSD is positively associated with multiple combat tours (OR = 1.96, p = 0.028), high combat exposure (OR = 2.15, p = 0.014), using alcohol or drugs to cope postdeployment (OR = 3.90, p < 0.001), history of childhood adversity (OR = 2.91, p < 0.001), and lower psychological resilience (OR = 4.02, p < 0.001). Being married appears to be protective for lifetime PTSD (OR = 0.52, p = 0.035). The associations for lifetime depression are similar, except that younger age (OR = 0.95, p = 0.009) and Operating Enduring Freedom/ Operation Iraqi Freedom (OEF/OIF) veteran status (OR = 0.38, p = 0.047) are protective and low self-esteem is a risk factor (OR = 2.26, p = 0.001). Having ever sought mental health treatment was positively associated with some college or higher education (OR = 1.58, p = 0.009), lower self-esteem (OR = 2.09, p < 0.001), using alcohol or drugs to cope postdeployment (OR = 2.27, p = 0.002), history of childhood adversity (OR = 1.98, p = 0.003), high combat exposure (OR = 1.82, p = 0.005), and lower psychological resilience (OR = 3.07, p < 0.001). Younger age (OR = 0.96, p = 0.002) and being married (OR = 0.58, p = 0.010) appeared to be protective for lifetime mental health treatment seeking.
TABLE 2.
Multivariate Logistic Regressions Predicting Lifetime PTSD, Depression, and Mental Health Counseling (N = 700)
| Variables a | Lifetime PTSD OR (95% CI) p Value |
Lifetime Depression OR (95% CI) p Value |
Lifetime Counseling OR (95% CI) p Value |
|---|---|---|---|
| Age (years) | 0.99 (0.96–1.03) 0.752 | 0.95 (0.93–0.99) 0.009 | 0.96 (0.94–0.99) 0.002 |
| Male gender | 1.20 (0.32–4.55) 0.785 | 0.64 (0.24–1.72) 0.377 | 1.31 (0.52–3.32) 0.572 |
| White race | 0.70 (0.27–1.83) 0.465 | 1.21 (0.51–2.89) 0.664 | 1.22 (0.61–2.42) 0.571 |
| Married | 0.52 (0.28–0.96) 0.035 | 0.63 (0.39–1.03) 0.066 | 0.58 (0.38–0.88) 0.010 |
| Some college or higher | 1.32 (0.72–2.42) 0.365 | 0.93 (0.59–1.46) 0.749 | 1.58 (1.12–2.22) 0.009 |
| Employed | 0.85 (0.45–1.61) 0.614 | 0.69 (0.43–1.13) 0.142 | 1.02 (0.70–1.48) 0.923 |
| OEF/OIF veteran | 1.12 (0.34–3.63) 0.855 | 0.38 (0.15–0.99) 0.047 | 0.48 (0.22–1.02) 0.057 |
| Served multiple combat tours | 1.96 (1.08–3.57) 0.028 | 1.54 (0.96–2.47) 0.075 | 0.88 (0.60–1.28) 0.509 |
| Low self-esteem | 1.01 (0.53–1.92) 0.981 | 2.26 (1.43–3.59) 0.001 | 2.09 (1.41–3.09) < 0.001 |
| Used alcohol/drugs to cope postdeployment | 3.90 (2.08–7.31) < 0.001 | 2.48 (1.45–4.23) 0.001 | 2.27 (1.34–3.86) 0.002 |
| History of high childhood adversity | 2.91 (1.61–5.27) < 0.001 | 2.28 (1.42–3.69) 0.001 | 1.98 (1.27–3.09) 0.003 |
| High combat exposure | 2.15 (1.16–3.95) 0.014 | 1.09 (0.66–1.82) 0.736 | 1.82 (1.19–2.76) 0.005 |
| Low psychological resilience | 4.02 (2.14–7.53) < 0.001 | 3.26 (2.02–5.26) < 0.001 | 3.07 (1.94–4.87) < 0.001 |
Note. OEF/OIF = Operation Enduring Freedom/Operation Iraqi Freedom; PTSD = post-traumatic stress disorder.
All variables shown are included in the logistic regression models.
The multivariate results for current PTSD, depression, and mental health treatment seeking were similar. Several exceptions were that use of alcohol/drugs to cope (OR = 1.80, p = 0.145) and childhood adversity (OR = 1.86, p = 0.099) were not associated with depression (Table 3). In addition, being employed was protective (i.e., negatively associated) for current mental health treatment seeking (OR = 0.58, p = 0.02). However, the results for current alcohol misuse were different. As shown in Table 4, the best predictor of current alcohol dependence on the CAGE scale (OR = 12.05, p < 0.001), as well as current heavy alcohol use (OR = 9.14, p < 0.001), was use of alcohol/drugs to cope postdeployment. In these models, however, for both current alcohol dependence (OR = 0.48, p = 0.043) and heavy alcohol use (OR = 0.40, p = 0.015), history of childhood adversity appeared to be protective for (i.e., negatively associated with) these outcomes. However, when we removed the alcohol/drug coping variable from the logistic models, childhood adversity was not significant in either of these alcohol prediction models, suggesting that collinearity between the coping measure and respective dependent variables likely contributed to a spurious association. We confirmed this collinearity by assessing the Kappa statistic between the CAGE measure and the alcohol/drug coping scale used, and this statistic was high (κ < 0.40, p < 0.001). This statistic was similar for heavy alcohol use and the alcohol/drug coping measure as well (κ = 0.30, p < 0.001).
TABLE 3.
Multivariate Logistic Regressions Predicting Current PTSD, Major Depression, and Mental Health Counseling (N = 700)
| Variables a | Current PTSD OR (95% CI) p Value |
Current Depression OR (95% CI) p Value |
Current Counseling OR (95% CI) p Value |
|---|---|---|---|
| Age (years) | 0.98 (0.94–1.03) 0.454 | 0.92 (0.88–0.96) <0.001 | 0.97 (0.94–1.00) 0.063 |
| Male gender | 2.43 (0.42–13.96) 0.320 | 0.96 (0.25–3.78) 0.959 | 0.50 (0.20–1.28) 0.148 |
| White race | 0.50 (0.18–1.43) 0.194 | 3.41 (0.66–17.80) 0.145 | 0.86 (0.39–1.85) 0.691 |
| Married | 0.44 (0.22–0.89) 0.022 | 0.71 (0.34–1.52) 0.382 | 0.65 (0.41–1.04) 0.073 |
| Some college or higher | 1.28 (0.63–2.58) 0.491 | 1.08 (0.52–2.24) 0.842 | 1.36 (0.89–2.09) 0.157 |
| Employed | 0.87 (0.41–1.85) 0.711 | 0.60 (0.28–1.30) 0.197 | 0.58 (0.36–0.92) 0.020 |
| OEF/OIF veteran | 0.82 (0.22–3.10) 0.765 | 0.28 (0.08–1.03) 0.055 | 0.79 (0.32–1.93) 0.611 |
| Served multiple combat tours | 1.88 (0.94–3.76) 0.073 | 1.54 (0.73–3.24) 0.253 | 1.16 (0.74–1.83) 0.509 |
| Low self-esteem | 1.69 (0.81–3.54) 0.166 | 3.73 (1.74–8.00) 0.001 | 2.80 (1.82–4.31) <0.001 |
| Used alcohol/drugs to cope postdeployment | 3.43 (1.68–7.01) 0.001 | 1.80 (0.82–3.96) 0.145 | 2.75 (1.64–4.62) <0.001 |
| History of high childhood adversity | 2.89 (1.46–5.73) 0.002 | 1.86 (0.89–3.86) 0.099 | 1.67 (1.04–2.68) 0.034 |
| High combat exposure | 2.12 (1.05–4.26) 0.035 | 1.30 (0.60–2.81) 0.506 | 2.40 (1.52–3.78) <0.001 |
| Low psychological resilience | 3.19 (1.53–6.66) 0.002 | 3.48 (1.63–7.43) 0.001 | 2.07 (1.30–3.29) 0.002 |
Note. OEF/OIF = Operation Enduring Freedom/Operation Iraqi Freedom; PTSD = post-traumatic stress disorder.
All variables shown are included in the logistic regression models.
To determine if lifetime or current VA health care use differed by mental health status, we cross-tabulated these variables (Table 5). As can be seen, both lifetime and current VA health care use are associated with mental health service use (both lifetime and current mental health service use, p < 0.01), as well as high combat exposure (p < 0.001). Examination of the demographic variables associated with lifetime and current VA health care service use suggested that current VA use was associated only with not being employed (p = 0.01). No other demographic variables were associated with VA service use, neither lifetime VA service use nor current use (demographic results available upon request from the first author).
DISCUSSION
The objective of the current study was to assess the prevalence of and risk factors for mental health disorders among previously deployed veterans seen in a large non-VA health care system. Most veterans do not use the VA system and the majority also have access to alternative health care services (Elbogen et al., 2013; Liu et al., 2010; Liu et al., 2011; Shen et al., 2003; U.S. Department of Veterans Affairs, 2002; U.S. Department of Veterans Affairs, 2010). As shown, the largest group of veterans included in the current study was Vietnam veterans. This is important because this cohort of service members is both Medicare eligible and also a higher user of health care services. Understanding the prevalence of and risk factors for mental health disorders among U.S. veterans seen in non-VA facilities, and their patterns of service use, are essential for both VA and non-VA service providers (Boscarino, Larson, Ladd, Hill, & Paolucci, 2010). This is significant because many veterans who use the VA today also use non-VA facilities, as noted, which complicates the continuity of care delivery and makes assessing health outcomes difficult (Liu et al., 2010; Liu et al., 2011). In addition to alternative health care coverage, convenience is another reason for non-VA service use among veterans, especially among those residing in nonurban areas (Boscarino, Larson, et al., 2010). To achieve our study objective, we surveyed a random sample of community-based veterans who were outpatients in GHS, a large, multihospital system located in Pennsylvania. All GHS veterans studied served at least one previous war-zone deployment. With the exception of race (U.S. Census Bureau, n.d.), the demographic profile of veterans studied in the current study matched the demographic profile of veterans in the United States under 75 years of age, which was the age cutoff for our study.
As seen, 40.4% of veterans report they are currently using the VA for health care services. The best predictors of PTSD, depression, and mental health service use were low self-esteem, use of alcohol or drugs to cope postdeployment, history of childhood adversity, high combat exposure, and low psychological resilience. Being married and younger age were negatively associated with these outcomes. Although somewhat tautological, the use of alcohol/drugs to cope postdeployment was strongly associated with current alcohol misuse, including current alcohol dependence and heavy drinking (both about 12% prevalence). Similarly, lifetime and current VA health care use were associated with mental health service use and history of high combat exposure. Noteworthy is that, with the exception of alcohol misuse, the prevalence of mental health disorder for GHS veterans appears to be somewhat lower than reported for veterans, which is typically 10% to 15% for current mental disorders (Booth-Kewley et al., 2010; Hoge et al., 2004; Kulka et al., 1990a). In fact, the prevalence of mental disorders among veterans in the current study appears to be closer to that reported for the general U.S. population and in other nonveteran trauma studies (Boscarino et al., 2012; Kessler et al., 2005). In addition, the prevalence of general mental health treatment seeking also appears to be comparable to that reported for nonveteran adults (Kessler et al., 1999; Kessler & Wang, 2008), consistent with our study hypothesis. Within this context, it has recently been reported that most community-based veterans are relatively well adjusted (Pietrzak & Cook, 2013), and this finding is consistent with our results. Finally, only about 40% of GHS veterans reported recently using the VA for health care, and those who did were more likely to have a history of mental health counseling and higher combat exposure levels (Table 5). This finding is consistent with higher impairment typically reported among VA service users and the fact that many of these VA users are seeking (or have sought) disability compensation from the VA, typically for PTSD (Elbogen et al., 2013; Hermes, Hoff, & Rosenheck, 2014; Hynes et al., 2007).
Compared to similar populations and using the same assessment methods, we found that GHS veterans in the current study appear to have a comparable prevalence of current PTSD (6.7%, 95% CI = 5.1–8.8), compared to community-based adults exposed to the World Trade Center disaster (7.3%, 95% CI = 6.3–8.5), adults seen in outpatient clinics for chronic noncancer pain (9.9%, 95% CI = 7.8–12.4), and adult patients discharged from a regional trauma center (11.8%, 95% CI = 7.7–16.5) (Boscarino et al., 2012). In addition, comparison of the demographic profile of GHS veterans in the current study is similar to the demographic profile of U.S. veterans generally, with the exception of race, whereby the current study population has a higher prevalence of Whites, compared to the U.S. veteran population (93.3% versus 83.7%) (U.S. Census Bureau, n.d.).
There were some study limitations for this research. First, our interview data were based on self-report, and our study was cross-sectional. Also, the current study included only previously deployed U.S. veterans who were predominantly men and outpatients in a large, multihospital health care system located in Pennsylvania. In addition, comparison of survey responders to nonresponders suggested that survey responders tended to be younger and married. Furthermore, our study excluded those too ill to be surveyed and those who were institutionalized. These factors may have further biased our results and may limit study generalization. Despite these limitations, our findings suggest that factors associated with PTSD, depression, and mental health service use among previously deployed veterans seen in non-VA settings are low self-esteem, use of alcohol or drugs to cope postdeployment, history of childhood adversity, high combat exposure, and low psychological resilience. Use of alcohol/drugs to cope was the best predictor of current alcohol misuse and the prevalence of alcohol misuse, at about 12%, was high. Both lifetime and current VA service use were positively associated with having received mental health counseling and having high combat exposure, suggesting that the VA will likely play a key role in meeting veterans’ health care needs in the future.
The current prevalence of mental health disorders among previously deployed GHS veterans, comparable to the rates found in civilian populations exposed to trauma (Boscarino et al., 2012), is likely due to the selection biases associated with those who use the VA for health care (Carey et al., 2008). The rates of mental health treatment seeking, similar to rates reported for the U.S. civilian populations, are also noteworthy, given the average age and male distribution of our study population. However, findings related to use of alcohol and drugs to cope postdeployment and mental health status and the prevalence of current alcohol misuse are of concern (James et al., 2013). While there has been research showing that trauma exposure is a risk factor for substance misuse (Boscarino, Rukstalis, et al., 2010; Boscarino, Kirchner, et al., 2011), the positive associations found for use of alcohol/drugs to cope and the adverse mental health outcomes assessed are worthy of additional investigation (James et al., 2013; O’Brien, Oster, & Morden, 2012). This also applies to the negative associations found for self-esteem, childhood adversity, combat exposure, and psychological resilience. Psychosocial risk factors such as these have been studied in recent years, and harm-reduction strategies are currently available to address these issues in medical social work and other clinical fields (Adams & Boscarino, 2015; Adams & Boscarino, 2011; Beder, 2006; Boscarino, Hoffman, et al., 2014; Spelman et al., 2012).
In summary, with some exceptions, the prevalence of mental disorders among previously deployed service members seen in the current study appear to be similar to those reported for trauma-exposed nonveterans (Boscarino et al., 2012). It is noteworthy that the prevalence of PTSD in the veterans studied, about 7%, is the approximate rate reported in earlier national studies of community-based veterans (Centers for Disease Control, 1988). Further research is recommended to confirm these findings. The knowledge gained from studying veterans in non-VA health care systems is relevant today, especially given the changing U.S. marketplace under current health care reform (Buttorff, Tunis, & Weiner, 2013). The greater availability of health care options for veterans will likely increase non-VA service use, so non-VA health services research will be needed for service planning and outcomes research (Kizer & Jha, 2014). Currently, as in the past, few definitive sources of data are related to the health status of the veteran population (Boscarino, 2007). This has been, no doubt, exacerbated by the ongoing and dynamic nature of warfighting that has evolved following the Vietnam war (Boscarino, 2007). Consequently, many recent veterans’ studies have been conducted post hoc using available data assets coupled with follow-up surveys (Crawford et al., 2013; LeardMann et al., 2009; Rosen et al., 2012). In addition, most veterans are not seen in VA facilities, and the ones who are seen in these facilities appear to be more impaired, distorting the overall clinical picture (Hynes et al., 2007). This is an issue at this time because there are few unbiased source populations with which to study the long-term health effects of warzone exposures among veterans (Boscarino, 2007).
As suggested, most veterans today have other health care coverage and use non-VA facilities, so it is important to study them in these other health care environments. Similar studies are also important because data suggest that non-VA health care providers, including non-VA social workers, may be unprepared to treat former service members (Boscarino, Larson, et al., 2010; Spelman et al., 2012), so in-service provider interventions may be required in the future (Adams, Laraque, Chemtob, Jensen, & Boscarino, 2013). Given the widespread use of EHR systems, veteran status information can be captured and can become part of the patient’s medical record at most non-VA facilities. To our knowledge, this is one of the first studies to detail mental health disorders, treatment seeking, and mental health risk factors among U.S. veterans seen in a large, non-VA health care system using this approach. As suggested, these findings may have implications for deployed veterans and for outcomes research (Sayer, Carlson, & Frazier, 2014). Finally, as was seen in our study, consistent predictors of mental health status among previously deployed veterans were self-esteem, use of alcohol or drugs to cope postdeployment, history of childhood adversity, combat exposure, and psychological resilience—clinical issues that medical social workers have been better trained to address than most health care providers (Beder, 2006). While this was a cross-sectional study, it may be useful to focus on these key risk factors in designing interventions for veterans and other trauma-exposed populations in the future. Given current medical technology, we have shown that it is feasible to conduct robust studies of formerly deployed veterans in large, non-VA health care environments, contributing to health services research for veterans and potentially contributing to improved quality of care for former service members. It is very likely that non-VA hospital social workers will be at the vanguard of these future efforts.
Acknowledgments
The assistance of Joseph J. Boscarino, Department of Psychology, Ram-apo College of New Jersey, Mahwah, NJ, is gratefully acknowledged in the preparation of this manuscript.
FUNDING
Support for this study was provided in part by the Geisinger Auxiliary Fund, the Kline & Ditty Health Fund, and the National Institute of Mental Health (Grant No. R21-MH-086317) to Dr. Boscarino.
References
- Acierno R, Kilpatrick DG, Resnick H, Saunders B, De Arellano M, Best C. Assault, PTSD, family substance use, and depression as risk factors for cigarette use in youth: Findings from the National Survey of Adolescents. Journal of Traumatic Stress. 2000;13(3):381–396. doi: 10.1023/A:1007772905696. [DOI] [PubMed] [Google Scholar]
- Adams RE, Boscarino JA. A structural equation model of perievent panic and posttraumatic stress disorder after a community disaster. Journal of Traumatic Stress. 2011;24(1):61–69. doi: 10.1002/jts.20603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RE, Boscarino JA. Volunteerism and well-being in the context of the World Trade Center terrorist attacks. International Journal of Emergency Mental Health. 2015;17(1):274–282. doi: 10.4172/1522-4821.1000158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RE, Boscarino JA, Galea S. Social and psychological resources and health outcomes after the World Trade Center disaster. Social Science and Medicine (1982) 2006;62(1):176–188. doi: 10.1016/j.socscimed.2005.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adams RE, Laraque D, Chemtob CM, Jensen PS, Boscarino JA. Does a one-day educational training session influence primary care pediatricians’ mental health practice procedures in response to a community disaster? Results from the Reaching Children Initiative (RCI) International Journal of Emergency Mental Health. 2013;15(1):3–14. [PubMed] [Google Scholar]
- Adler AB, Castro CA. An occupational health model for the military. Military Behavioral Health. 2013;1(1):41–51. [Google Scholar]
- Allen JP, Columbus M, editors. Assessing alcohol problems: A guide for clinicians and researchers. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. [Google Scholar]
- Beder J. Hospital social work: The interface of medicine and caring. New York, NY: Routledge; 2006. [Google Scholar]
- Binder EB, Bradley RG, Liu W, Epstein MP, Deveau TC, Mercer KB, Ressler KJ. Association of FKBP5 polymorphisms and childhood abuse with risk of posttraumatic stress disorder symptoms in adults. Journal of the American Medical Association. 2008;299(11):1291–1305. doi: 10.1001/jama.299.11.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth-Kewley S, Larson GE, Highfill-McRoy RM, Garland CF, Gaskin TA. Correlates of posttraumatic stress disorder symptoms in Marines back from war. Journal of Traumatic Stress. 2010;23(1):69–77. doi: 10.1002/jts.20485. [DOI] [PubMed] [Google Scholar]
- Boscarino JA. Post-traumatic stress and associated disorders among Vietnam veterans: The significance of combat exposure and social support. Journal of Traumatic Stress. 1995;8(2):317–336. doi: 10.1007/BF02109567. [DOI] [PubMed] [Google Scholar]
- Boscarino JA. Vietnam veterans, postwar experiences, and health outcomes. In: Fink G, editor. Encyclopedia of stress. 2. New York, NY: Academic Press; 2007. pp. 830–838. [Google Scholar]
- Boscarino JA, Adams RE. PTSD onset and course following the World Trade Center disaster: Findings and implications for future research. Social Psychiatry and Psychiatric Epidemiology. 2009;44(10):887–898. doi: 10.1007/s00127-009-0011-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE, Figley CR. Mental health service use one year after the World Trade Center disaster: Implications for mental health care. General Hospital Psychiatry. 2004;26(5):346–358. doi: 10.1016/j.genhosppsych.2004.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE, Figley CR. Mental health service use after the World Trade Center disaster: Utilization trends and comparative effectiveness. Journal of Nervous and Mental Disease. 2011;199(2):91–99. doi: 10.1097/NMD.0b013e3182043b39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Galea S, Adams RE, Ahern J, Resnick H, Vlahov D. Mental health service and medication use in New York City after the September 11, 2001, terrorist attack. Psychiatric Services. 2004;55(3):274–283. doi: 10.1176/appi.ps.55.3.274. [DOI] [PubMed] [Google Scholar]
- Boscarino JA, Hoffman SN, Adams RE, Figley CR, Solhkhah R. Mental health outcomes among vulnerable residents after Hurricane Sandy: Implications for disaster research and planning. American Journal of Disaster Medicine. 2014;9(2):107–120. doi: 10.5055/ajdm.2014.0147. [DOI] [PubMed] [Google Scholar]
- Boscarino JA, Kirchner HL, Hoffman SN, Sartorius J, Adams RE. PTSD and alcohol use after the World Trade Center attacks: A longitudinal study. Journal of Traumatic Stress. 2011;24(5):515–525. doi: 10.1002/jts.20673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Kirchner HL, Hoffman SN, Sartorius J, Adams RE, Figley CR. The New York PTSD Risk Score for Assessment of Psychological Trauma: Male and female versions. Psychiatry Research. 2012;200(2–3):827–834. doi: 10.1016/j.psychres.2012.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Larson S, Ladd I, Hill E, Paolucci SJ. Mental health experiences and needs among primary care providers treating OEF/OIF veterans: Preliminary findings from the Geisinger Veterans Initiative. International Journal of Emergency Mental Health. 2010;12(3):161–170. [PubMed] [Google Scholar]
- Boscarino JA, Lu M, Moorman AC, Gordon SC, Rupp LB, Spradling PR, Holmberg SD. Predictors of poor mental and physical health status among patients with chronic hepatitis C infection: The Chronic Hepatitis Cohort Study (CHeCS) Hepatology. 2015;61(3):802–811. doi: 10.1002/hep.27422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Rukstalis M, Hoffman SN, Han JJ, Erlich PM, Gerhard GS, Stewart WF. Risk factors for drug dependence among out-patients on opioid therapy in a large U.S. health care system. Addiction. 2010;105(10):1776–1782. doi: 10.1111/j.1360-0443.2010.03052.x. [DOI] [PubMed] [Google Scholar]
- Boscarino JA, Sitarik A, Gordon SC, Rupp LB, Nerenz DR, Vijayadeva V, Lu M. Risk factors for hepatitis C infection among Vietnam era veterans versus nonveterans: Results from the Chronic Hepatitis Cohort Study (CHeCS) Journal of Community Health. 2014;39(5):914–921. doi: 10.1007/s10900-014-9863-5. [DOI] [PubMed] [Google Scholar]
- Buttorff C, Tunis SR, Weiner JP. Encouraging value-based insurance designs in state health insurance exchanges. American Journal of Managed Care. 2013;19(7):593–600. [PubMed] [Google Scholar]
- Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the Connor-Davidson Resilience Scale (CD-RISC): Validation of a 10-item measure of resilience. Journal of Traumatic Stress. 2007;20(6):1019–1028. doi: 10.1002/jts.20271. [DOI] [PubMed] [Google Scholar]
- Carey K, Montez-Rath ME, Rosen AK, Christiansen CL, Loveland S, Ettner SL. Use of VA and Medicare services by dually eligible veterans with psychiatric problems. Health Services Research. 2008;43(4):1164–1183. doi: 10.1111/j.1475-6773.2008.00840.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol’s too long: Consider the brief COPE. International Journal of Behavioral Medicine. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control. Health status of Vietnam veterans. I. Psychosocial characteristics: The Centers for Disease Control Vietnam Experience Study. Journal of the American Medical Association. 1988;259(18):2701–2707. [PubMed] [Google Scholar]
- Connor KM, Davidson JR. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC) Depression and Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Crawford EF, Fulton JJ, Swinkels CM, Beckham JC, Calhoun PS VA Mid-Atlantic MIRECC OEF/OIF Registry Workgroup. Diagnostic efficiency of the AUDIT-C in U.S. veterans with military service since September 11, 2001. Drug and Alcohol Dependence. 2013;132(1–2):101–106. doi: 10.1016/j.drugalcdep.2013.01.012. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, Marshall R. The psychological risks of Vietnam for U.S. veterans: A revisit with new data and methods. Science. 2006;313(5789):979–982. doi: 10.1126/science.1128944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong M, Giles WH, Felitti VJ, Dube SR, Williams JE, Chapman DP, Anda RF. Insights into causal pathways for ischemic heart disease: Adverse Childhood Experiences Study. Circulation. 2004;110(13):1761–1766. doi: 10.1161/01.CIR.0000143074.54995.7F. [DOI] [PubMed] [Google Scholar]
- Elbogen EB, Wagner HR, Johnson SC, Kinneer P, Kang H, Vasterling JJ, Beckham JC. Are Iraq and Afghanistan veterans using mental health services? New data from a national random-sample survey. Psychiatric Services. 2013;64(2):134–141. doi: 10.1176/appi.ps.004792011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Ahern J, Resnick H, Kilpatrick D, Bucuvalas M, Gold J, Vlahov D. Psychological sequelae of the September 11 terrorist attacks in New York City. New England Journal of Medicine. 2002;346(13):982–987. doi: 10.1056/NEJMsa013404. [DOI] [PubMed] [Google Scholar]
- Hermes ED, Hoff R, Rosenheck RA. Sources of the increasing number of Vietnam era veterans with a diagnosis of PTSD using VHA services. Psychiatric Service. 2014;65(6):830–832. doi: 10.1176/appi.ps.201300232. [DOI] [PubMed] [Google Scholar]
- Hobfoll SE, Lerman M. Personal relationships, personal attributes, and stress resistance: Mothers’ reactions to their child’s illness. American Journal of Community Psychology. 1988;16(4):565–589. doi: 10.1007/BF00922772. [DOI] [PubMed] [Google Scholar]
- Hoffman SN, Zhang X, Erlich PM, Boscarino JA. Grapheme-color synesthesia and posttraumatic stress disorder: Preliminary results from the Veterans Health Study. Psychosomatic Medicine. 2012;74(9):912–915. doi: 10.1097/PSY.0b013e3182731007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351(1):13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Hynes DM, Koelling K, Stroupe K, Arnold N, Mallin K, Sohn MW, Kok L. Veterans’ access to and use of Medicare and Veterans Affairs health care. Medical Care. 2007;45(3):214–223. doi: 10.1097/01.mlr.0000244657.90074.b7. [DOI] [PubMed] [Google Scholar]
- James LM, Van Kampen E, Miller RD, Engdahl BE. Risk and protective factors associated with symptoms of post-traumatic stress, depression, and alcohol misuse in OEF/OIF veterans. Military Medicine. 2013;178(2):159–165. doi: 10.7205/milmed-d-12-00282. [DOI] [PubMed] [Google Scholar]
- Janes GR, Goldberg J, Eisen SA, True WR. Reliability and validity of a combat exposure index for Vietnam era veterans. Journal of Clinical Psychology. 1991;47(1):80–86. doi: 10.1002/1097-4679(199101)47:1<80::aid-jclp2270470112>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey replication. Archives of General Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Wang PS. The descriptive epidemiology of commonly occurring mental disorders in the United States. Annual Review of Public Health. 2008;29:115–129. doi: 10.1146/annurev.publhealth.29.020907.090847. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Zhao S, Katz SJ, Kouzis AC, Frank RG, Edlund M, Leaf P. Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. American Journal of Psychiatry. 1999;156(1):115–123. doi: 10.1176/ajp.156.1.115. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Freedy JR, Pelcovitz D, Resick P, Roth S, van der Kolk B. The posttraumatic stress disorder field trial: Evaluation of the PTSD construct—Criteria A through E. In: Widiger T, Frances A, Pincus H, et al., editors. DSM-IV sourcebook. Washington, DC: American Psychiatric Association Press; 1998. pp. 803–844. [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the National Survey of Adolescents. Journal of Consulting and Clinical Psychology. 2003;71(4):692–700. doi: 10.1037/0022-006x.71.4.692. [DOI] [PubMed] [Google Scholar]
- King M. At-risk drinking among general practice attenders: Validation of the CAGE questionnaire. Psychological Medicine. 1986;16(1):213–217. doi: 10.1017/s0033291700002658. [DOI] [PubMed] [Google Scholar]
- Kizer KW, Jha AK. Restoring trust in VA health care. New England Journal of Medicine. 2014;371:295–297. doi: 10.1056/NEJMp1406852. [DOI] [PubMed] [Google Scholar]
- Kok BC, Herrell RK, Thomas JL, Hoge CW. Posttraumatic stress disorder associated with combat service in Iraq or Afghanistan: Reconciling prevalence differences between studies. Journal of Nervous and Mental Disease. 2012;200(5):444–450. doi: 10.1097/NMD.0b013e3182532312. [DOI] [PubMed] [Google Scholar]
- Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS. The National Vietnam Veterans Readjustment Study: Tables of findings and technical appendices. New York, NY: Brunner/Mazel; 1990a. [Google Scholar]
- Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS. Trauma and the Vietnam War generation: Report of findings from the National Vietnam Readjustment Study. New York, NY: Brunner/Mazel; 1990b. [Google Scholar]
- LeardMann CA, Smith TC, Smith B, Wells TS, Ryan MA Millennium Cohort Study Team. Baseline self reported functional health and vulnerability to post-traumatic stress disorder after combat deployment: Prospective U.S. military cohort study. BMJ. 2009;338:b1273. doi: 10.1136/bmj.b1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leider JP, Castrucci BC, Russo P, Hearne S. Perceived impacts of health care reform on large urban health departments. Journal of Public Health Management and Practice. 2015;21(Suppl 1):S66–S75. doi: 10.1097/PHH.0000000000000145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy BS, Sidel VW. Health effects of combat: A life-course perspective. Annual Review of Public Health. 2009;30:123–136. doi: 10.1146/annurev.publhealth.031308.100147. [DOI] [PubMed] [Google Scholar]
- Liu CF, Chapko M, Bryson CL, Burgess JF, Jr, Fortney JC, Perkins M, Maciejewski ML. Use of outpatient care in Veterans Health Administration and Medicare among veterans receiving primary care in community-based and hospital outpatient clinics. Health Services Research. 2010;45(5 Pt 1):1268–1286. doi: 10.1111/j.1475-6773.2010.01123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu CF, Manning WG, Burgess JF, Jr, Hebert PL, Bryson CL, Fortney J, Maciejewski ML. Reliance on Veterans Affairs outpatient care by Medicare-eligible veterans. Medical Care. 2011;49(10):911–917. doi: 10.1097/MLR.0b013e31822396c5. [DOI] [PubMed] [Google Scholar]
- Moorman AC, Gordon SC, Rupp LB, Spradling PR, Teshale EH, Lu M Chronic Hepatitis Cohort Study Investigators. Baseline characteristics and mortality among people in care for chronic viral hepatitis: The Chronic Hepatitis Cohort Study. Clinical Infectious Diseases. 2013;56(1):40–50. doi: 10.1093/cid/cis815. [DOI] [PubMed] [Google Scholar]
- O’Brien CP. The CAGE questionnaire for detection of alcoholism: A remarkably useful but simple tool. Journal of the American Medical Association. 2008;300(17):2054–2056. doi: 10.1001/jama.2008.570. [DOI] [PubMed] [Google Scholar]
- O’Brien CP, Oster M, Morden E, editors. Substance use disorders in the US Armed Forces. Washington, DC: National Academy Press; 2012. [Google Scholar]
- Pietrzak RH, Cook JM. Psychological resilience in older U.S. veterans: Results from the National Health and Resilience in Veterans Study. Depression and Anxiety. 2013;30(5):432–443. doi: 10.1002/da.22083. [DOI] [PubMed] [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology. 1993;61(6):984–991. doi: 10.1037/0022-006X.61.6.984. [DOI] [PubMed] [Google Scholar]
- Robinson JP, Shaver PR, Wrightsman LS, editors. Measures of personality and social psychological attitudes. Vol. 1: Measures of social psychological attitudes. 2. San Diego, CA: Academic Press; 1991. pp. 115–160. [Google Scholar]
- Rosen RC, Marx BP, Maserejian NN, Holowka DW, Gates MA, Sleeper LA, Keane TM. Project VALOR: Design and methods of a longitudinal registry of post-traumatic stress disorder (PTSD) in combat-exposed veterans in the Afghanistan and Iraqi military theaters of operations. International Journal of Methods in Psychiatric Research. 2012;21(1):5–16. doi: 10.1002/mpr.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayer NA, Carlson KF, Frazier PA. Reintegration challenges in U.S. service members and veterans following combat deployment. Social Issues and Policy Review. 2014;8(1):33–73. doi: 10.1111/sipr.12001. [DOI] [Google Scholar]
- Shen Y, Hendricks A, Zhang S, Kazis LE. VHA enrollees’ health care coverage and use of care. Medical Care Research and Review. 2003;60(2):253–267. doi: 10.1177/1077558703060002007. [DOI] [PubMed] [Google Scholar]
- Sinclair SJ, Blais MA, Gansler DA, Sandberg E, Bistis K, LoCicero A. Psychometric properties of the Rosenberg Self-Esteem Scale: Overall and across demographic groups living within the United States. Evaluation and the Health Professions. 2010;33(1):56–80. doi: 10.1177/0163278709356187. [DOI] [PubMed] [Google Scholar]
- Spelman JF, Hunt SC, Seal KH, Burgo-Black AL. Post deployment care for returning combat veterans. Journal of General Internal Medicine. 2012;27(9):1200–1209. doi: 10.1007/s11606-012-2061-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stata Corporation. Stata, Version 13.1. College Station, TX: Stata Corporation; 2013. [Google Scholar]
- Stimpson NJ, Thomas HV, Weightman AL, Dunstan F, Lewis G. Psychiatric disorder in veterans of the Persian Gulf War of 1991: Systematic review. British Journal of Psychiatry. 2003;182:391–403. doi: 10.1192/bjp.182.5.391. [DOI] [PubMed] [Google Scholar]
- Trivedi AN, Grebla RC, Jiang L, Yoon J, Mor V, Kizer KW. Duplicate federal payments for dual enrollees in Medicare Advantage plans and the Veterans Affairs health care system. Journal of the American Medical Association. 2012;308(1):67–72. doi: 10.1001/jama.2012.7115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. Veteran status: 2012 American community survey 1-year estimates [table] n.d Retrieved from http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_12_1YR_S2101&prodType=table.
- U.S. Department of Veterans Affairs. 2001 National survey of veterans (NSV): Final report. Washington, DC: U.S. Department of Veterans Affairs; 2002. [Google Scholar]
- U.S. Department of Veterans Affairs. National survey of veterans, active duty services members, demobilized national guard and reserve members, family members, and surviving spouses. Washington, DC: U.S. Department of Veterans Affairs; 2010. Final Report ed. [Google Scholar]
- Yamashita J. A review of psychological assessments for disaster mental health studies. Psychological Trauma. 2012;4:560–567. doi: 10.1037/a0025952. [DOI] [Google Scholar]