Abstract
Objective
To evaluate stillbirth trends by gestational age.
Methods
National Center for Health Statistics’ fetal death and live birth data files were used to analyze the 2006 and 2012 cohorts of deliveries and compute gestational age-specific stillbirth rates at 20+ weeks of gestation using two methods: traditional (for example, still pregnant at 38 weeks). Changes in rates and in the percent distribution of stillbirths and live births were assessed.
Results
In 2006 and 2012, the stillbirth rate was 6.05 stillbirths per 1,000 deliveries. There was little change in the percent distribution of stillbirths by gestational age from 2006–2012. However, the percent distribution of live births by gestational age changed considerably: births at 34––38 weeks decreased by 10–16%, and births at 39 weeks increased by 17%. Traditionally computed stillbirth rates were unchanged at most gestational ages, but rose at 24–27, 34–36, 37 and 38 weeks. However, rates were influenced by decreases in births at those gestational ages; the pattern of stillbirths by gestational age was unchanged. In contrast, there were no differences in prospective stillbirth rates at 21–42 weeks of gestation.
Conclusion
The lack of change in prospective stillbirth rates from 2006–2012 suggests that preventing non–medically indicated deliveries before 39 weeks did not increase the U.S. stillbirth rate.
Introduction
Stillbirth, or the spontaneous death of a fetus after 20 completed weeks of gestation, is an important reproductive health indicator, and a significant public health problem (1–3). A recent report identified a plateau in the U.S. stillbirth rate (6.05 stillbirths per 1,000 live births and stillbirths in 2006 and 2012), but did not examine trends by detailed gestational age (4). Investigating trends in stillbirth by gestational age is important as a marker of pregnancy health, and also in the context of recent changes in the gestational age distribution of related reproductive health indicators. For example, the decline in the preterm birth rate from 2006–2012 is related to a decline in births at 34–38 weeks and an increase in births at 39+ weeks of gestation (5). Recent declines in cesarean delivery rates at 38 weeks and induction rates at 36–38 weeks may be related to initiatives to reduce non–medically indicated deliveries prior to 39 weeks (6–7). Also, after a plateau from 2000–2005, the US infant mortality rate declined by 13% from 2005–2012 (8), due in part to a shift in births to later gestational ages where the risk of infant mortality is lower (3,8). Although there is broad support within the medical community for reducing non–medically indicated deliveries before 39 weeks of gestation (9), some have suggested that longer pregnancies might lead to an increase in stillbirth (10, 11). Thus, our purpose was to compare and contrast trends in stillbirth by gestational age from 2006 to 2012 using two different methods of computing stillbirth rates.
Materials and Methods
We utilized data from the United States’ fetal death and live birth data files, which are part of the National Vital Statistics System (5, 12). These data files contain information from all Reports of Fetal Death and Certificates of Live Birth filed in in the United States and transmitted to the National Center for Health Statistics (5, 12). Data are reported by the vital statistics registration specialist or attending physician in the hospital, and are subject to editing and quality control checks at both the state and national levels (5, 12, 13). Although reporting requirements for fetal deaths vary somewhat by state, fetal mortality rates from the National Vital Statistics System are generally shown for fetal deaths at 20 weeks of gestation or more (otherwise known as stillbirths) (4, 12). Variables included in this study are considered to be reasonably well reported in both birth and fetal death data sets (14, 15). Since the study was based on de-identified, aggregated data from US government public-use data sets, the study was exempt from requiring IRB approval.
2006 was chosen as the base year for the analysis, since this was when the preterm birth rate began to decline (5), and 2012 as the final year, since data from this year were the latest available at the time of manuscript preparation.. The entire cohort of United States’ deliveries (live births plus stillbirths) in 2006 was compared to the entire cohort of deliveries in 2012. Since the overall stillbirth rate was the same in 2006 and 2012, all changes shown are due to differences in patterns by gestational age. Trends from 2006–2012 were examined for: 1) the percent distribution of stillbirths and live births by gestational age; 2) traditional gestational age-specific stillbirth rates; and 3) prospective stillbirth rates. Traditional gestational age-specific stillbirth rates are computed as the:
Thus, for a fetus at 38 weeks of gestation, the traditional stillbirth rate is:
In contrast, the prospective stillbirth rate is the:
The number of live births plus stillbirths at a given gestational age or greater is a good approximation of the number of women who are pregnant, and thus at risk of stillbirth, at that gestational age. For this reason, the prospective stillbirth rate is often preferred for measuring stillbirth risk, since the denominator represents the population at risk of the event (i.e. pregnant women) at a given gestational age (16–18). Comparisons were made for the overall population, and for non-Hispanic black, non-Hispanic white, and Hispanic women. Comparisons were tested for statistical significance using two tailed t-tests (8), and text statements that a given rate is higher or lower than another rate indicates that the rates are significantly different (p < 0.05). Not stated responses (<.0.4% for gestational age and <0.8% for race/ethnicity) were dropped before measures were computed. Since the study included the complete population of events (a total of 50,045 stillbirths and 8,268,441 live births in 2006 and 2012), it had considerable power to detect statistical differences, although this varied somewhat by race/ethnicity and gestational age. For example, for the total population at 20 weeks, a 6% or more difference in prospective stillbirth rates between 2006 and 2012 was detectible, whereas for Hispanic women at 40 weeks a 20% or more difference in rates was detectible.
Results
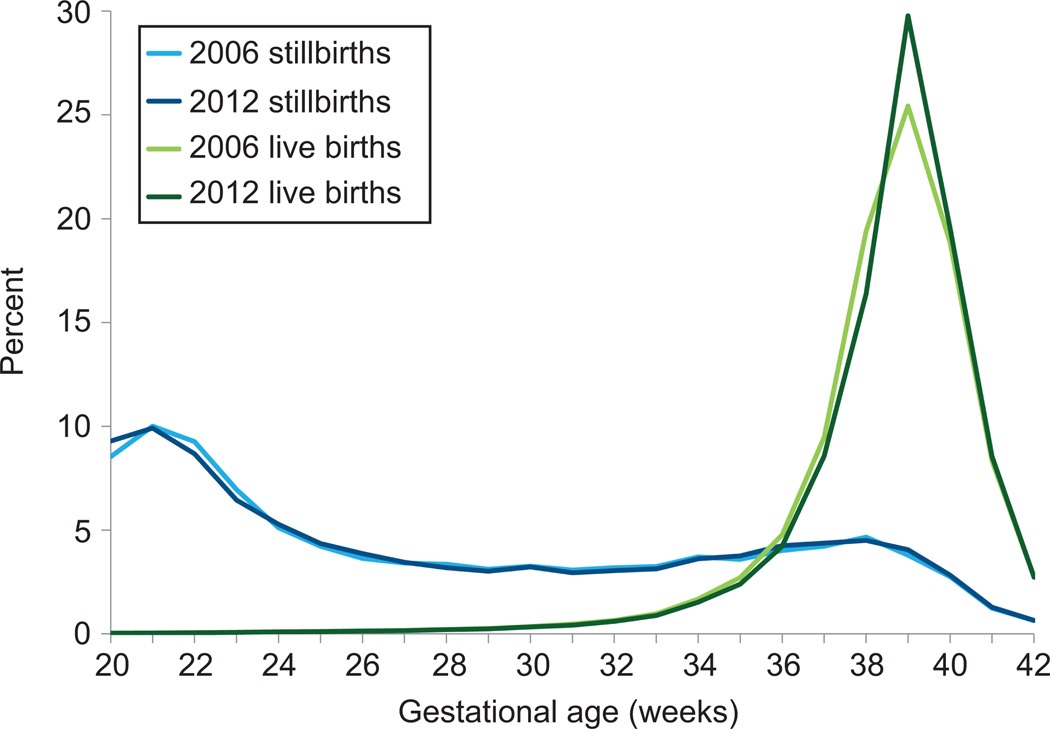
From 2006–2012, there was no significant change in the percent distribution of stillbirths from 24 to 42 weeks of gestation (Figure 1). However, the percent of stillbirths at 20 weeks was 9% higher and the percent at 22–23 weeks was 6–7% lower in 2012 than in 2006. The apparent 9% increase in stillbirths at 20 weeks was due to improvements in reporting of early stillbirths among some states (12).
Figure 1.
Percent distribution of stillbirths and live births by gestational age, United States, 2006 and 2012. Data from the Centers for Disease Control and Prevention/National Center for Health Statistics, National Vital Statistics System.
There were larger changes in the percent distribution of live births by gestational age from 2006 to 2012, with the largest changes occurring between 34 and 39 weeks of gestation (Figure 1). From 2006–2012, the percent of births declined by 12% at 34–36 weeks, by 10% at 37 weeks, and by 16% at 38 weeks of gestation. In contrast, the percent of births at 39 weeks rose by 17% from 2006–2012.
In 2012, the United States’ stillbirth rate was 6.05 stillbirths per 1,000 live births and stillbirths, the same as in 2006 (Table 1). Traditional gestational age-specific stillbirth rates are highest at the earliest gestational ages, decline until the lowest rates are reached at 39–41 weeks of gestation, and then increase slightly for stillbirths at 42 or more weeks of gestation. Traditional stillbirth rates for most gestational-age groups did not change significantly from 2006–2012. However, for the total population, stillbirth rates increased by 6% at 24–27 weeks of gestation, and by 15–16% at 34–36, 37 and 38 weeks of gestation. The increase in the stillbirth rate at 34–36, 37, and 38 weeks of gestation from 2006–2012 was influenced by the decline in births at these gestational ages, since births largely comprise the denominator of stillbirth rates. There were no significant changes in the pattern of stillbirth at 34–38 weeks during this period (Figure 1). In contrast, the 2012 stillbirth rate of 0.82 at 39 weeks was lower than the rate of 0.89 in 2006, although the difference was not statistically significant.
Table 1.
Traditional stillbirth rates by gestational age and race–ethnicity, United States, 2006 and 2012
| Gestational age (weeks) |
Total | Non-Hispanic white | Non-Hispanic black | Hispanic | ||||
|---|---|---|---|---|---|---|---|---|
| 2006 | 2012 | 2006 | 2012 | 2006 | 2012 | 2006 | 2012 | |
| Total | 6.05 | 6.05 | 4.81 | 4.91 | 10.73 | 10.67 | 5.29 | 5.33 |
| 20–23 | 500.62 | 510.24 | 520.45 | 535.18 | 443.19 | 456.74 | 496.12 | 507.00 |
| 24–27 | 161.57 | 171.40* | 171.57 | 180.43 | 133.42 | 149.56* | 156.09 | 164.03 |
| 28–31 | 56.37 | 59.14 | 51.94 | 55.31 | 58.60 | 65.53* | 54.23 | 53.66 |
| 32–33 | 23.29 | 24.56 | 21.88 | 24.22 | 26.06 | 27.56 | 21.53 | 20.70 |
| 34–36 | 7.37 | 8.56* | 6.74 | 7.97* | 8.80 | 10.86* | 6.87 | 7.88* |
| 37 | 2.67 | 3.08* | 2.29 | 2.97* | 3.60 | 3.88 | 2.51 | 2.53 |
| 38 | 1.44 | 1.66* | 1.26 | 1.60* | 1.83 | 2.05 | 1.50 | 1.48 |
| 39 | 0.89 | 0.82 | 0.77 | 0.70 | 1.27 | 1.28 | 0.92 | 0.77 |
| 40 | 0.88 | 0.87 | 0.74 | 0.85 | 1.36 | 1.22 | 0.89 | 0.66* |
| 41 | 0.89 | 0.90 | 0.76 | 0.80 | 1.45 | 1.08 | 0.89 | 1.00 |
| 42+ | 1.76 | 1.69 | 1.59 | 1.46 | 2.31 | 2.19 | 1.75 | 1.87 |
statistically significant at p<.05.
Data from Centers for Disease Control and Prevention. Vital statistics data available online. Fetal death data files. Available at: http://www.cdc.gov/nchs/data_access/VitalStatsOnline.htm. Retrieved September 22, 2015.
For non-Hispanic white women, stillbirth rates were higher in 2012 than in 2006 at 34–36, 37, and 38 weeks of gestation, and for non-Hispanic black women, at 24–27, 28–31 and 34–36 weeks of gestation. For Hispanic women, stillbirth rates increased at 34–36 weeks and decreased at 39 weeks of gestation. Race/ethnic-specific rates at all other gestational ages did not change significantly from 2006–2012.
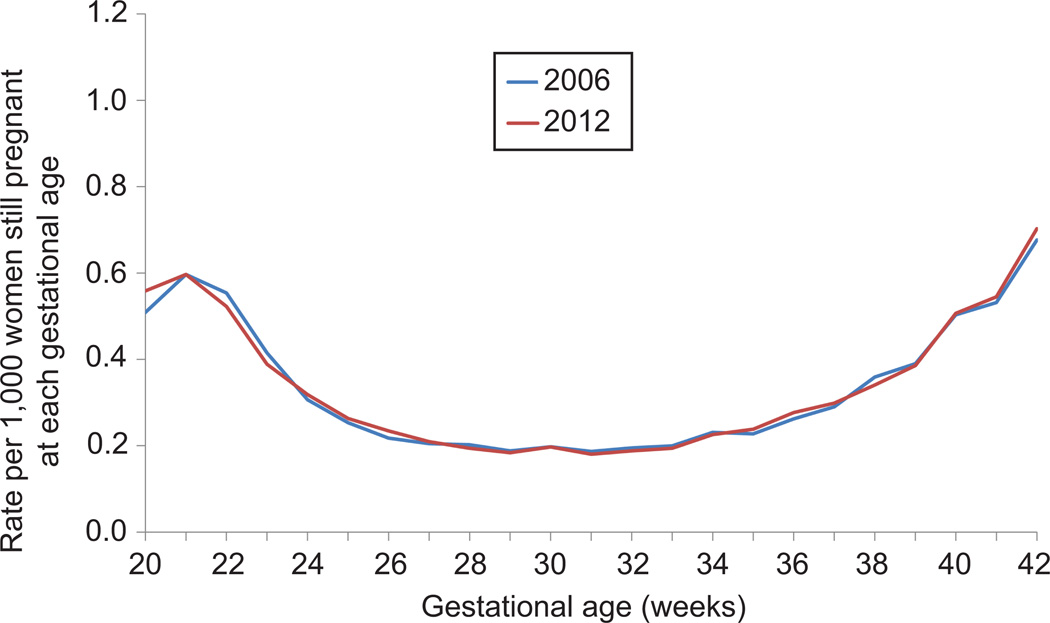
In contrast to traditional stillbirth rates, the prospective stillbirth rate follows a U-shaped curve, with the highest risk of stillbirth at <24 and >38 weeks of gestation (Figure 2). From 2006–2012, there were no statistically significant differences in the prospective stillbirth rate at any gestational age from 21–42 weeks of gestation. The increase in the stillbirth rate at 20 weeks of gestation from 2006 to 2012 is likely related to improvements in some states in reporting of early stillbirths during this period (12). In contrast to the traditional stillbirth rate, there was no change in the prospective stillbirth rate at 34–36, 37, and 38 weeks from 2006 to 2012.
Figure 2.
Prospective stillbirth rate by single weeks of gestation, United States, 2006 and 2012. The prospective stillbirth rate is the number of stillbirths at a given gestational age per 1,000 live births and stillbirths at that gestational age or greater. Data from the Centers for Disease Control and Prevention/National Center for Health Statistics, National Vital Statistics System.
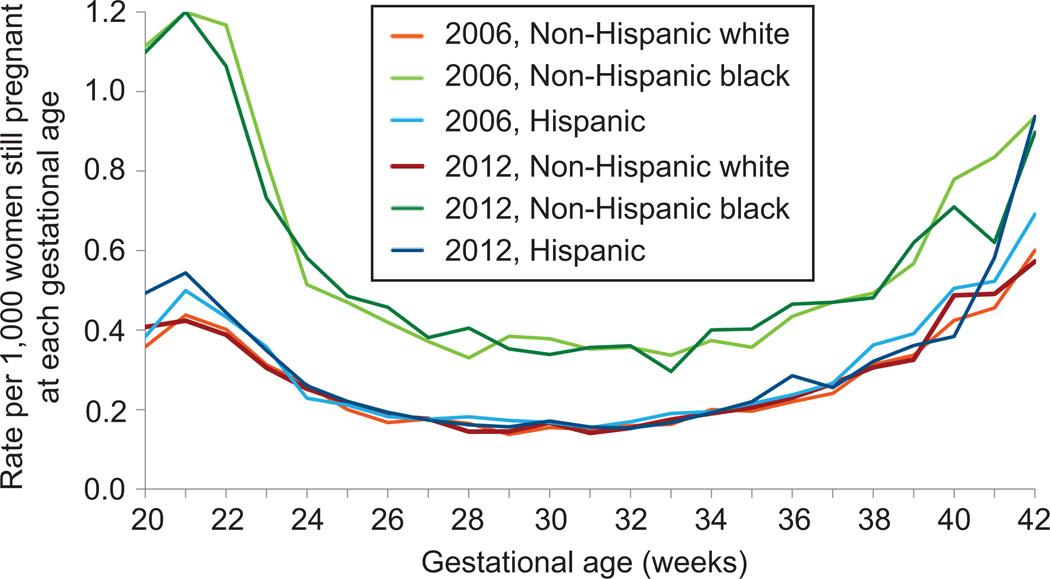
Prospective stillbirth rates for non-Hispanic white, non-Hispanic black, and Hispanic women followed a similar U-shaped curve to the overall population; however rates for non-Hispanic black women were consistently higher than for non-Hispanic white and Hispanic women (Figure 3). From 2006–2012, there were no significant differences in prospective stillbirth rates for non-Hispanic white, non-Hispanic black and Hispanic women at most gestational ages. For non-Hispanic white women, the 2012 rate was significantly higher at 20 weeks, and for non-Hispanic black women at 28 weeks of gestation. For Hispanic women the 2012 rate was higher at 20 and 36 weeks, and lower at 40 weeks of gestation. However, these small racial and ethnic differences in rates did not lead to any significant change in the overall rate from 2006–2012.
Figure 3.
Prospective stillbirth rate by single weeks of gestation and race/ethnicity, United States, 2006 and 2012.The prospective stillbirth rate is the number of stillbirths at a given gestational age per 1,000 live births and stillbirths at that gestational age or greater. Data from the Centers for Disease Control and Prevention/National Center for Health Statistics, National Vital Statistics System.
Discussion
From 2006–2012 in the U.S., there was no increase in the overall stillbirth rate and there was no change in the distribution of stillbirths from 24 to 42 weeks of gestation. In contrast, live births which mostly comprise the denominator of traditional stillbirth rates decreased by 10–16% at 34–36, 37 and 38 weeks, and increased by 17% at 39 weeks of gestation. Influenced by these changes, traditional stillbirth rates increased at 34–36, 37, and 38 weeks of gestation; the decrease at 39 weeks was not statistically significant. In contrast, there were no significant differences in the prospective stillbirth rate from 21–42 weeks of gestation from 2006–2012, both for the total population and for non-Hispanic white women. Prospective stillbirth rates were also mostly unchanged for non-Hispanic black and Hispanic women from 2006–2012.
The prospective stillbirth rate is preferred for measuring stillbirth risk, since the denominator is the number of women who are pregnant, and thus at risk of stillbirth, at a given gestational age (16–19). In contrast, traditional stillbirth rates exhibit considerable volatility in the face of changes in the distribution of live births by gestational age. In addition, a recent NICHD study found that 83% of stillbirths of 20 weeks of gestation or more occur before labor and delivery (20). For these stillbirths, the prospective stillbirth rate (where the denominator is all pregnant women) may be a better measure of stillbirth risk, as there is little relationship between stillbirth before labor and the specific week of delivery that comprises the denominator of traditional stillbirth rates (16). For these reasons, the prospective stillbirth rate appears to be a more reliable indicator of stillbirth trends during times when the distribution of live births by gestational age is changing.
The recent shift in the distribution of live births by gestational age may be linked to ACOG recommendations to reduce non–medically indicated deliveries before 39 weeks of gestation (9), and to the adoption of non–medically indicated delivery before 39 weeks as a Joint Commission National Quality Core Measure (21). In a hospital-based study, the shift in non–medically indicated deliveries to 39+ weeks was larger for white, multiparous women, with private insurance (i.e., women at lower risk of poor delivery outcome), suggesting that the women who continue to deliver at 34–38 weeks may be at higher risk (11). However, we did not find an increase in prospective stillbirth risk at 34–38 weeks of gestation for non-Hispanic white women at the national level.
The lack of improvement in stillbirth risk in the United States from 2006 to 2012 is disappointing. Recently released data for 2013 show a stillbirth rate of 5.96, compared to 6.05 in 2012, although the difference is not statistically significant (22). It is important to note that both infant and perinatal mortality rates declined during this period (8, 22). The US perinatal (stillbirths at 20+ weeks of gestation plus infant deaths at <28 days of age) mortality rate declined from 10.49 in 2006 to 10.05 in 2012 (22), while the infant mortality rate declined from 6.68 infant deaths per 1,000 live births in 2006 to 5.98 in 2012 (8). Notably, infant mortality rates at 34–36 and 37–38 weeks of gestation were essentially unchanged between 2006 and 2012 (8). This, in conjunction with the stabilization in the prospective stillbirth rate, suggests a lack of change in perinatal mortality risk for late preterm and early term infants from 2006–2012. To decrease the stillbirth rate, research is needed to identify women early in pregnancy at the highest risk for stillbirth for more careful monitoring and potential intervention. Still, the lack of change in the prospective stillbirth rate from 2006–2012 suggests that preventing non–medically indicated deliveries before 39 weeks did not increase the stillbirth rate at the national level.
Footnotes
Comments and views of the author(s) do not necessarily represent the views of the NICHD.
Financial Disclosure
The authors did not report any potential conflicts of interest.
References
- 1.Goldenberg RL, Kirby R, Culhane JF. Sillbirth: A review. Journal of Maternal, Fetal and Neonatal Medicine. 2004;16:79–94. doi: 10.1080/14767050400003801. [DOI] [PubMed] [Google Scholar]
- 2.Froen JF, Cacciatore J, McClure Em, Kuti O, Jokhio AH, Islam M, Shiffman J. Stillbirths: Why they matter. Lancet. 2011;377:1353–1365. doi: 10.1016/S0140-6736(10)62232-5. [DOI] [PubMed] [Google Scholar]
- 3.Darmstdt GL, Shiffman J, Lawn JE. Advancing the newborn and stillbirth global agenda: Priorities for the next decade. Arch Dis Child. 2015;100(suppl 1):s13–s18. doi: 10.1136/archdischild-2013-305557. [DOI] [PubMed] [Google Scholar]
- 4.Gregory EW, MacDorman MF, Martin JA. NCHS data brief no. 169. Hyattsville, MD: National Center for Health Statistics; 2014. Nov, Trends in fetal and perinatal mortality, United States, 2000–2012. [PubMed] [Google Scholar]
- 5.Martin JA, Hamilton BE, Osterman MJK, Curtin SC, Mathews TJ. National vital statistics reports. 9. Vol. 62. Hyattsville, MD: National Center for Health Statistics; 2013. Births: Final data for 2012. [PubMed] [Google Scholar]
- 6.Osterman MJK, Martin JA. NCHS data brief no. 124. Hyattsville, MD: National Center for Health Statistics; 2013. Changes in cesarean delivery rates by gestational age: United States, 1996–2011. [PubMed] [Google Scholar]
- 7.Osterman MJK, Martin JA. NCHS data brief no. 155. Hyattsville, MD: National Center for Health Statistics; 2014. Recent declines in induction of labor by gestational age. [PubMed] [Google Scholar]
- 8.Mathews TJ, MacDorman MF, Thoma ME. National vital statistics reports. 9. Vol. 64. Hyattsville, MD: National Center for Health Statistics; 2015. Infant mortality statistics from the 2013 period linked birth/infant death data set. [PubMed] [Google Scholar]
- 9.American College of Obstetricians and Gynecologists. ACOG Committee Opinion No. 561: Non-medically indicated early-term deliveries. Obstet Gynecol. 2013;121(4):911–915. doi: 10.1097/01.AOG.0000428649.57622.a7. [DOI] [PubMed] [Google Scholar]
- 10.Myers SA, Waters TP, Dawson NV. Fetal, neonatal and infant death and their relationship to best gestational age for delivery at term: Is 39 weeks best for everyone? Journal of Perinatology. 2014;34:503–507. doi: 10.1038/jp.2014.9. [DOI] [PubMed] [Google Scholar]
- 11.Ehrenthal DB, Hoffman MK, Xioazhang J, Ostrum G. Neonatal outcomes after implementation of guidelines limiting elective delivery before 39 weeks of gestation. Obstet Gynecol. 2011;118(5):1047–1055. doi: 10.1097/AOG.0b013e3182319c58. [DOI] [PubMed] [Google Scholar]
- 12.National Center for Health Statistics. User Guide to the 2012 Fetal Death Public-Use File. Hyattsville, MD: National Center for Health Statistics; 2014. [Accessed August 28, 2014]. Available from: http://www.cdc.gov/nchs/data_access/VitalStatsOnline.htm. [Google Scholar]
- 13.National Center for Health Statistics. Guide to Completing the Facility Worksheets for the Certificate of Live Birth and Report of Fetal Death. Hyattsville, MD: National Center for Health Statistics; 2012. update. Available at: http://www.cdc.gov/nchs/data/dvs/GuidetoCompleteFacilityWks.pdf. [Google Scholar]
- 14.Lee EJ, Gambatese M, Begier E, Soto A, Das T, Madsen A. Understanding perinatal death: A systematic analysis of New York City Fetal and neonatal death vital record data and implications for improvement, 2007–2011. Matern Child Health J. 2014;18(8):1945–1954. doi: 10.1007/s10995-014-1440-0. [DOI] [PubMed] [Google Scholar]
- 15.Martin JA, Wilson EC, Osterman MJK, Saadi EW, Sutton SR, Hamilton BE. Assessing the quality of medical and health data from the 2003 birth certificate revision: Results from two states. National vital statistics reports. 2013;62(2) [PubMed] [Google Scholar]
- 16.Caughey AB. Measuring perinatal complications: Methodologic issues related to gestational age. BMC Pregnancy and Childbirth. 2007;7:18. doi: 10.1186/1471-2393-7-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kramer MS, Liu S, Luo Z, Yuan H, Platt RW, Joseph SA. Analysis of perinatal mortality and its components: Time for a change? Am J Epidemiol. 2002;156(6):493–497. doi: 10.1093/aje/kwf077. [DOI] [PubMed] [Google Scholar]
- 18.Yudkin PL, Wood L, Redman CWG. Risk of unexplained stillbirth at different gestational ages. Lancet. 1987;329(8543):1192–1194. doi: 10.1016/s0140-6736(87)92154-4. [DOI] [PubMed] [Google Scholar]
- 19.Joseph KS. Incidence-based measures of birth, growth restriction, and death can free perinatal epidemiology from erroneous concepts of risk. Journal of Clinical Epidemiology. 2004;57:889–907. doi: 10.1016/j.jclinepi.2003.11.018. [DOI] [PubMed] [Google Scholar]
- 20.Stillbirth Collaborative Research Network Writing Group. Causes of death among stillbirths. JAMA. 2011;306(22):2459–2468. doi: 10.1001/jama.2011.1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joint Commission. Specifications manual for joint commission national quality core measures. [Accessed July 25, 2014];Version 2014 A1. Available from: https://manual.jointcommission.org/releases/TJC2014A1/rsrc/Manual/TableOfContentsTJC/PC_2014A1.pdf. [Google Scholar]
- 22.MacDorman MF, Gregory ECW. National vital statistics reports. 8. Vol. 64. Hyattsville, MD: National Center for Health Statistics; 2015. Fetal and Perinatal Mortality, United States, 2013. [PubMed] [Google Scholar]