Abstract
Studies on the role of diet in the development of chronic diseases often rely on self-report surveys of dietary intake. Unfortunately, many validity studies have demonstrated that self-reported dietary intake is subject to systematic underreporting, although the vast majority of such studies have been conducted in industrialized countries. The aim of this study was to investigate whether or not systematic reporting error exists among individuals of African ancestry (n=324) in five countries distributed across the Human Development Index scale, a United Nations statistic devised to rank countries on non-income factors plus economic indicators. Using two 24-hour recalls to assess energy intake and the doubly labeled water method to assess total energy expenditure, we calculated the difference between these two values to identify underreporting of habitual energy intake in selected communities in Ghana, South Africa, Seychelles, Jamaica and the United States. Under-reporting of habitual energy intake was observed in all countries. The South African cohort displayed the greatest mean % under-reporting: −52.1% ([self-report - expenditure/expenditure]×100) compared to −22.5%, −17.9%, −25.0%, and −18.5%, for, Ghana, Jamaica, Seychelles and the United States cohorts, respectively. Body mass index was the most consistent predictor of underreporting compared to other factors. We conclude that there is substantial under-reporting in populations across the whole range of the human development index and that this systematic error increases according to an individual’s body mass index.
Keywords: diet assessment, 24h recall, doubly labeled water, human development index
INTRODUCTION
Energy imbalance, manifested as either underweight or overweight, is implicated in countless health problems and can lead to premature death. While undernutrition has long been the major health risk in developing countries, the contemporary primary concern is now over-nutrition, which often exists contemporaneously with undernutrition. This shift in focus has been driven by the rapid increases in the prevalence of obesity across virtually every segment of nearly all populations around the world. According to the World Health Organization (WHO), obesity (body mass index [BMI]≥30 kg/m2) is increasing globally with many countries having rates greater than 10% and a few, particularly among Pacific Island nations, having rates in excess of 50% 1. Not surprisingly, public health investigators have undertaken numerous studies to understand the causes of the increase in the rates of obesity. Many of these have focused on potential dietary causes including energy intake collected using self-report dietary instruments; however, self-reports are subject to both random error, which with averaging can still produce accurate results, and systematic error, which will introduce bias that may lead to erroneous conclusions regarding both the absolute amounts of foods consumed and the relationship between energy intake and nutritionally-related diseases2, 3.
Many studies have been conducted in industrialized countries to assess the validity of self-reported dietary intake across different age groups and ethnicities. In general, these studies have verified the finding of systematic underreporting in self-reported dietary intake assessments with increasing bias as BMI increases 4. Relatively few studies, however, have been conducted in developing countries, and a large fraction of those have relied on indirect methods such as comparing self-reported energy intake with physiologically plausible energy requirements, calculated as multiples of resting metabolic rate (RMR) 5, 6. A more accurate assessment of underreporting can be obtained using the biomarker approach of measured energy expenditure based on the doubly labeled water (DLW) method 7.
Assessment of underreporting by comparison of reported energy intake to actual total energy expenditure is a corollary of the first law of thermodynamics: energy may neither be created nor destroyed. Metabolizable energy intake must equal total energy expenditure plus change in body energy stores. In weight-stable adults, change in energy stores is small and, therefore, energy intake nearly equals total energy expenditure. Habitual energy intake, i.e., an individual’s typical energy intake which maintains weight, is therefore taken to equal total energy expenditure. Actual energy intake may differ from habitual energy intake under certain conditions such as weight loss where the reporting of energy intake can differ from habitual energy intake due to a reporting error or due to energy restriction during the reporting period 8. Both causes, however, result in a systematic error in the assessment of habitual energy intake. The Modeling the Epidemiologic Transition Study (METS) included DLW measures and provides an opportunity to study underreporting in community-based cohorts from five countries at differing stages of social and economic development as categorized by the Human Development Index (HDI). Participation in METS provided us with an opportunity to assess the accuracy of self-reported dietary energy intake across the spectrum of the HDI and thus contribute to filling the gap in knowledge of systematic reporting errors in developing countries. We hypothesized that underreporting would be observed in all five countries, but that it would be increase between sites with increasing HDI and between individuals with increasing BMI.
EXPERIMENTAL METHODS
Participants
A total of 2500 young adults (ages 25–45, ~60% female) were recruited in 2010 for participation in METS 9. Of this total, a subsample of 375 (75 per site), were randomly selected to participate in the DLW protocol. The five sites included communities in rural Ghana, urban South Africa, Seychelles, urban Jamaica, and suburban United States. The communities were not randomly selected and, thus, our sample should not be viewed as representative of each country’s entire population but rather representations of the lifestyles, including diet and physical activity patterns, of the respective communities. Individuals with infectious diseases such as malaria, those who were HIV-positive, and pregnant women were excluded from the study. Each of the cohorts was of Black African ancestry and displayed a wide range of mean BMI: from an average of 24 kg/m2 in rural Nkwantakese (Ghana) to 32 kg/m2 in suburban Maywood, IL (USA). The five countries studied were selected to be diverse with respect to economic and social development as defined by the United Nations Human Development Index (HDI) of 2010 (10). The US has been defined as a very high HDI country, Jamaica and the Seychelles as high HDI, South Africa as middle HDI, and Ghana as low-middle HDI 10.
The specific sites have been described by Luke at al. 9. Briefly, the site in Ghana was the rainforest village of Nkwantakese and is in the Afigya Sekyere District in the Ashanti Region. This village has a population of 16,965 and is about 20 km from Kumasi, the second largest city in Ghana. Approximately 10% of the men in our Ghanaian cohort commute to Kumasi for work daily while a large proportion of the women (40%) work in Kumasi or nearby villages as traders. Approximately a quarter of both men and women engage in subsistence agricultural work. In South Africa, the town studied was Khayelitsha, the 3rd largest township in South Africa. Located next to Cape Town, the township has a population of almost 500,000 and an unemployment rate of 40 percent. Unemployment among our cohort was much lower than the community average at about 10%. A significant proportion of both men and women (>70%) were engaged in routine manual or service occupations such as construction or transport among the men and trading among the women. In Jamaica, the participants studied were from the capital and largest city, Kingston, which has a population of 651,880. As in South Africa, many of the male participants (>30%) were engaged in construction work with another 20% working as mechanics or craftsmen. Women were predominantly engaged in routine manual and service occupations. In Seychelles, participants were from the main island (Mahé, 27 km in length, which contributes to 90% of the total population of the country) with a majority of them commuting for work to the capital, Victoria. Seychelles has a population of approximately 87,000 and the archipelago is located in the Indian Ocean, about 1,600 km east of Kenya. Occupations for the Seychellois cohort varied considerably, especially for the men, with a lower proportion of manual labor than any of the other sites (40% vs. 50–90%). The study site in the US was Maywood, IL with a population of 24,903. A suburb of Chicago, Maywood is a working class, predominantly African-American community. Over 50% of the men were engaged in routine service occupations while about 45% of the women had clerical or service representative positions.
Participants at each site were recruited by local investigators and recruiting strategies within each site were at the discretion of the lead investigator. In Ghana, door-to-door recruitment was used. Researchers in Seychelles, as well as South Africa, used sex- and age-stratified random samples, which were produced from each country’s national census. For Jamaica, a fixed point in each district was determined (e.g. north-west corner), and from there random sampling occurred by means of door-to-door recruitment. Recruiters in Maywood used a similar approach, in which all city blocks in the community were randomized and then door-to-door recruitment took place. This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Institutional Review Boards or Ethics Committees each of the six institutions 9. Written informed consent was obtained from all participants.
Protocol
The participants reported to their site-specific field clinic in the morning, after an overnight fast, and baseline measurements were performed. Each participant underwent measurements of total energy expenditure by doubly labeled water, dietary intake by 24-hour recall, body weight and height, while age and years of education were obtained by interview. The body weight measurement was repeated at the end of the DLW period, approximately 7 days later. One additional 24-hour dietary recall was collected from each participant 6–9 days after the first visit.
Energy Intake (24-Hour Recall)
Two 24-hour dietary recalls were obtained from each participant to provide an estimate of habitual intake 11. The recalls were performed by trained interviewers using a multiple-pass method, as designed by the Medical Research Council (MRC) of South Africa 12, in which participants reported specific foods consumed and their amounts. Recall interview scripts were translated into the local language, where appropriate. These scripts guided the recording of all foods consumed on the previous day, first by a quick list and then by a meal by meal listing, followed by probing for commonly unreported foods. The assignment of portion size was based on representative photos of small, medium and large portions of all foods and food mixtures commonly consumed locally, as well as on the use of representative spoons, cups, bowls and plates. Details on preparation methods were sought with particular emphasis on cooking method and type of oils used, if appropriate.
In an effort to maximize consistency of the format of the interview across field sites and thus minimize between site methodological biases; interviewers were either trained dieticians or nutritionists and who had attended dietary recall training at Loyola 11. Because there were differences in the specific foods commonly consumed across the five countries, the methodology allowed for these differences. For example, prior to the initiation of participant enrollment, a dietetic consultant visited all the sites to photograph all commonly observed local foods and food mixtures at varying portion sizes (half, typical, and one-and-one-half), to obtain local recipes, identify local measuring tools and to identify foods that might be commonly unreported foods. The photographs with portion size estimates were based upon a system developed and utilized in South Africa12. The MRC dietetic consultant also monitored the local field staff in conducting 24-hour recall interviews in an effort to increases fidelity of the recall method. All recalls and details were recorded on standardized paper forms that were structured to coincide with the order of the script.
The recalls were digitized and sent to the Coordinating Center at Loyola University Chicago where analysis of the data was done using the Nutrient Data System for Research (NDSR; University of Minnesota, Minneapolis, MN) 9, by the study dietician. All recalls were assessed in an on-going manner by the study dietician at Loyola, with requests for clarification relayed back to the sites immediately. Energy and nutrient contents of mixed food dishes from each of the sites that were not already part of NDSR were calculated from regional sources, e.g, West African, East African, South African or Caribbean nutrient databases 13–17. These data were then used to identify comparable foodstuffs in the NDSR database. The lead study dietician from Loyola traveled to the Ghana and Seychelles sites approximately 6 months after initiation of participant enrollment to clarify any questions that arose during coding in regards to local ingredients and recipes. Issue that were not resolved during this visit with regard to the Jamaica and South Africa sites were settled via e-mail and telephone discussions.
For the present analyses, energy intake was calculated for each food and quantity eaten and then totaled for each day. Total energy intake (TEI) was calculated as the mean of energy intake calculated from the two days of recalls and expressed as kilojoules per day.
Total Energy Expenditure (Doubly Labeled Water Method)
The doubly labeled water method (DLW) was used to measure total energy expenditure (TEE) in the participants. In this method, a dose of doubly labeled water is administered and concentrations of 2H and 18O were measured in subsequent time and date stamped samples of urines, using mass spectrometry; the total amount of carbon dioxide produced by the body in the interval can be estimated from the differential in elimination rates over time of 2H and 18O. The method has been described in detail elsewhere18. DLW is the standard for assessing TEE: Urines collected at each site were transferred in o-ring sealed, freezer safe, plastic vials and kept frozen at each site. These were periodically shipped to Loyola in chilled thermo-boxes and stored frozen until shipped to the central analysis lab at the University of Wisconsin. TEE estimates in this laboratory have been shown to be unbiased and have a 1 sigma precision of 7% when analyzed along with laboratory water standards in each batch that had been calibrated against international stable isotope water standards 4.
A baseline sample of urine was collected and then a loading dose of the isotopic water was ingested by mouth. Urine samples were then collected 1, 3, and 4 hours after the loading dose. Seven days later, participants returned to the study centers and provided two urine samples at a one-hour interval as their final urine samples. Carbon dioxide production in each individual was calculated from the 2H and 18O elimination rates and TEE calculated using the modified Wier equation and the average food quotient for each site 2. The results of the TEE analyses were then combined with reported TEI; the proportion of underreporting was assessed by the ratio TEI/TEE.
Anthropometric Measurements
Height was measured to the nearest 0.1 cm using a wall-mounted standard stadiometer (Invicta Stadiometer, Invicta, London, UK) without shoes and the participant’s head held in the Frankfort plane 9. Similarly, weight was measured with the participant in light clothing and without shoes to the nearest 0.1 kg (Seca 770, Hamburg, Germany). The same model standard calibrated balance was used at each of the five sites 9. Body mass index was calculated as weight (kg)/height2 (m2). Weight was also measured at the end of the 7-day DLW period to assess whether or not there was measurable change in body stores as estimated from weight change over the week of DLW measurement. Weight change was tracked to permit the estimation of energy imbalance and thus to distinguish between undereating and underreporting in cases where TEI was less than TEE. Undereating, i.e. negative energy balance, results in loss of body energy stores and hence body weight, while weight stability indicates underreporting of energy intake. Years of education and age were self-reported by each participant.
Statistical Analysis
Self-reported TEI data were compared to objectively measured TEE data. The primary outcome variable was the ratio of TEI based on 24-hour diet recalls divided by TEI based on DLW (i.e. TEI/TEE). A value of 1.0 would indicate perfect reporting with no error. Percent misreporting was calculated as (TEI − TEE)/TEE * 100; here a 0 would indicate no difference between reported and measured values.
Data from the US site was used as the reference against which data from each of the other four countries were compared, as Maywood is a suburban, industrialized location and represents a community that we considered similar in nature to many previous studies of underreporting in industrialized countries. Associations between degree of underreporting and BMI, sex, age and/or years of formal education were investigated, first in univariate models and then in a single multivariate model. Body mass index was examined both as a continuous variable in the models and also as a categorical value; the degree of underreporting was calculated using standard BMI categories: underweight (BMI<18.5), healthy weight (18.5 – 24.9), overweight (25.0 – 29.9) and obese (≥30.0). Likewise, years of education were included as continuous variables in the models and by site-specific tertiles.
Self-reported energy intake was also assessed for physiological plausibility, i.e. too low to meet requirements for resting metabolic rate and minimal physical activity. The standard chosen was the Goldberg threshold which is based on estimated RMR. Dietary reports in which self-reported energy intake was < 1.35 times calculated RMR were viewed as physiologically implausible outliers and deleted from the data set. Resting metabolic rate was calculated using the Mifflin-St. Joer equation: RMR=9.99 × weight + 6.25 × height − 4.92 × age −166 × sex + 5, where sex = 1 or 0 for females or males, respectively 6.
RESULTS
Of the 375 participants in the DLW protocol, data from 324 were used in these analyses. Those excluded from the dataset included 21 participants who were missing measurements for TEE and 13 participants missing both 24-hour dietary recalls. Data from 17 participants were identified as outliers that had excessive numerical influence based on TEI/TEE ratios, i.e., more than 2 standard deviations from the mean, and were dropped from the data set.
Participant characteristics are presented in Table 1. As expected due to study design, body weight and BMIs among the men increased with increasing HDI rank; the pattern was less consistent among the women, with South Africans having a higher mean BMI that either Seychelles or Jamaica yet lower HDI rank. Although TEI was significantly less than TEE in all sites (p<0.001), among both men and women of South Africa, the difference was considerably larger than in the other four sites. The intra-individual coefficient of variation for self-reported TEI was significantly greater among South Africans (16.9%; p<0.01) than any of the other sites (US = 0.6%, Seychelles = 0.02%, Jamaica = 0.7% and Ghana = 1.2%; mean of all sites = 2.8%). With the exception of South Africa (r = −0.20), the correlation between TEI and TEE was consistent across the four other sites, ranging from 0.21 to 0.28 (mean of all sites, r = 0.27).
Table 1.
| n | Age (y) | Weight (kg) | Height (cm) | BMI (kg/m2) | Education (y) | TEE (MJ/d) | TEI (MJ/d) | |
|---|---|---|---|---|---|---|---|---|
| Men | ||||||||
| US | 33 | 34(5) | 91 (24) | 179 (6) | 28 (8) | 13(2) | 13.0 (2.9) | 10.1 (3.5) |
| Seychelles | 35 | 34 (5) | 73 (11) | 170 (6) | 25 (4) | 12 (2) | 12.1 (1.9) | 8.4 (2.1) |
| Jamaica | 29 | 34 (6) | 73 (14) | 177 (6) | 23 (4) | 10 (3) | 10.6 (1.9) | 8.5 (2.4) |
| South Africa | 20 | 33 (6) | 65 (14) | 168 (4) | 23 (4) | 10 (2) | 10.0 (1.8) | 4.4 (1.5) |
| Ghana | 31 | 36 (6) | 62 (7) | 169 (6) | 22 (2) | 9 (3) | 12.1 (1.9) | 9.1 (1.8) |
| Women | ||||||||
| US | 30 | 35 (6) | 91 (17) | 164 (5) | 34 (7) | 13 (2) | 9.8 (1.5) | 7.9 (2.7) |
| Seychelles | 37 | 33 (6) | 77 (18) | 163 (6) | 29 (6) | 13 (2) | 9.3 (1.6) | 7.1 (1.8) |
| Jamaica | 34 | 35 (6) | 76 (15) | 164 (6) | 28 (6) | 11 (2) | 8.7 (1.3) | 7.0 (1.7) |
| South Africa | 39 | 34 (6) | 84 (25) | 162 (7) | 32 (9) | 10 (2) | 9.7 (1.8) | 4.4 (1.2) |
| Ghana | 36 | 35 (6) | 64 (16) | 158 (5) | 26 (7) | 6 (4) | 10.0 (1.9) | 7.6 (1.6) |
| Combined | ||||||||
| US | 63 | 34 (6) | 91 (21) | 172 (9) | 31 (8) | 13 (2) | 11.5 (2.8) | 9.0 (3.3) |
| Seychelles | 72 | 33 (6) | 75 (15) | 167 (7) | 27 (5) | 12 (2) | 10.7 (2.2) | 7.7 (2.0) |
| Jamaica | 63 | 34 (6) | 75 (15) | 170 (9) | 26 (5) | 11 (3) | 9.6 (1.9) | 7.7 (2.2) |
| South Africa | 59 | 34 (6) | 78 (24) | 164 (7) | 29 (9) | 10 (2) | 9.8 (1.8) | 4.4 (1.3) |
| Ghana | 67 | 35 (6) | 63 (13) | 163 (8) | 24 (6) | 7 (4) | 10.9 (2.1) | 8.3 (1.9) |
| Total | 324 | 34 (6) | 76 (20) | 167 (9) | 27 (7) | 11 (3) | 10.5 (2.3) | 7.5 (2.7) |
TEE, total energy expenditure; TEI, total energy intake
Sites listed from highest Human Development Index rank to lowest
Weight change over the week of the DLW measurement period was calculated, except in Ghana where weights were not available for most subjects at the end of the assessment period. Weight changes over the seven days of the DLW period averaged 0.25 kg or less in every subgroup; none were significantly different from zero (Table 2). For the entire cohort, there was power to detect an 80 g weight change, which, assuming an energy equivalence of 31.0 kJ/g, corresponds to a change in energy stores of 2481 kJ/week or 356 kJ/d out of an average TEE of 10.51 MJ/d. Thus, a difference between reported TEI and TEE larger than 3.4% of TEE for entire cohort or about 7% for an individual site represents a significant contribution from underreporting.
Table 2.
| Weight Change (kg) | ||
|---|---|---|
| Men | Women | |
| US | 0.11 (1.5) | 0.05 (1.0) |
| Seychelles | −0.01 (0.9) | 0.17 (0.7) |
| Jamaica | −0.12 (0.9) | 0.25 (1.1) |
| South Africa | 0.05 (1.2) | 0.13 (1.0) |
| Total | 0.01 (1.0) | 0.12 (0.8) |
Weight change data not available for Ghana
Sites listed from highest Human Development Index rank to lowest
The mean percentage underreporting ([TEI−TEE]/TEE)*100 for all subjects combined was −27% (SD=26), significantly different from zero (p<0.001). Underreporting was observed in all five countries and for both sexes (Figure 1). The mean percentages of underreporting for all males and females were −26% (SD=26) and −27% (SD=27), respectively; sex was not a significant predictor of underreporting in the univariate model.
Figure 1.
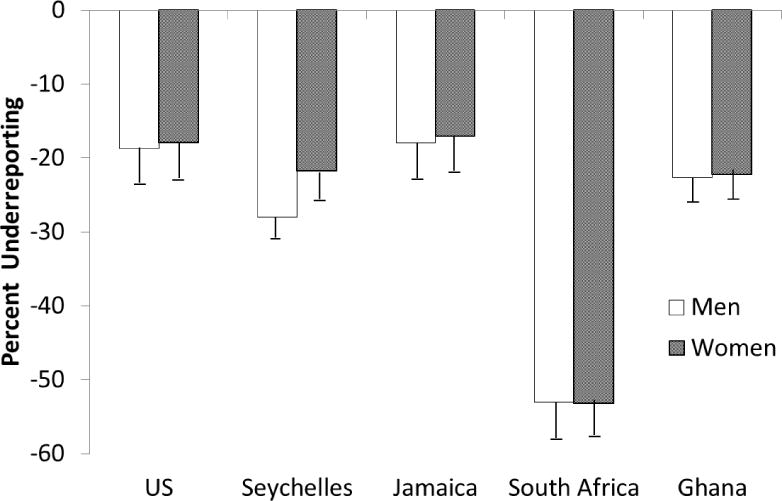
Percent of energy intake underreporting relative to measured energy expenditure by site, organized from highest to lowest United Nations Human Development Index ranking.
For the entire data set, all BMI categories underreported and the degree of underreporting increased with increasing BMI. The values for each group were: underweight by −15.4% (SD=32.3); healthy weight by −22.3% (SD=23.8); overweight by −23.0% (SD=28.1); and obese by−36.5% (SD=25.9) (p for trend <0.001). The underreporting distribution by BMI is shown for sex and site in Figure 2.
Figure 2.
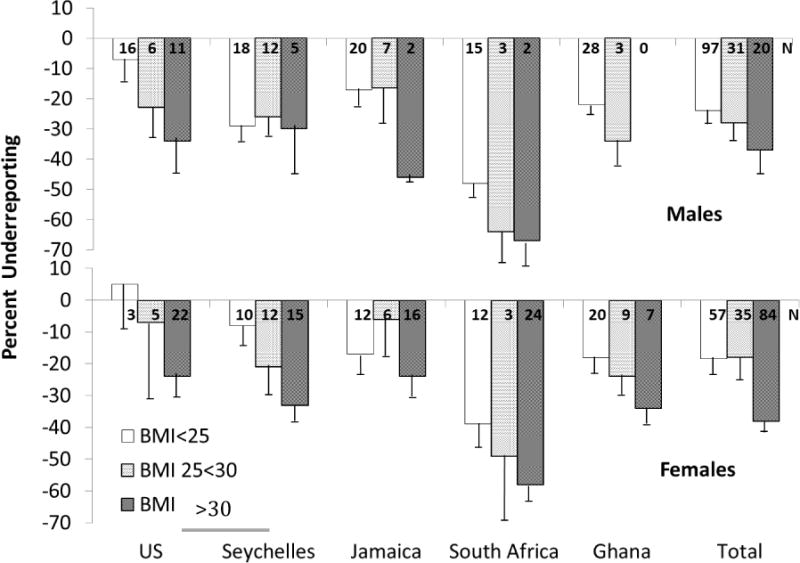
Percent of energy intake underreporting relative to energy expenditure as a function of body mass index (BMI). Panel A displays the results for men and panel B displays the results for women. Error bars indicate the standard error of the mean (SEM); the number at the top of each bar represents the number of participant in each BMI grouping by site.
When tested for the entire cohort, degree of underreporting did not differ by site-specific tertile of education (p=0.22), however for both the South African and Seychellois sites, there was less underreporting as the level of education increased (p<0.001 and 0.03, respectively). This was countered in the US site, where underreporting tended to increase with tertile of education, moving from lowest to highest (p=0.065). Thus, the influence of education was not consistent between sites.
Combined Model
When the predictors were combined in a final multivariate model, site, BMI and gender were found to be significant, but age and years of education, or tertiles of education, were not (Table 3). For every 1 BMI unit increase, underreporting of TEI increased by 1.3%; after controlling for the other covariates, including BMI, women underreported less than men by 9.6%. Compared to the United States, underreporting was significantly greater in Ghana by 12.6%, the Seychelles by 12.4% and South Africa by 38.3% (all p<0.02), with the level of underreporting in South Africa also being significantly greater than any of the other four countries (p<0.001). The significantly greater degree of underreporting in the South African participants was identified as a cause for concern early in the study. To determine whether or not the method being used by the Loyola dietitian, ie, translation of local foods to foodstuffs available in NDSR, was perhaps not capturing energy content appropriately, the first 24 2-day sets of recalls were sent back to University of Cape Town and analyzed by their on-staff, well-trained registered dietitian utilizing the local nutrient database, FoodFinder® Version 3 (National Nutritional Intervention Unit, MRC, Parow, Cape Town, South Africa, 2002). The mean difference between the Loyola and University of Cape Town values was −78 kcal/day; the correlation between the site values was 0.88. Thus it was decided that in order to maintain consistency across sites, all analyses continued to be conducted at Loyola.
Table 3.
Multivariate Associations between Selected Factors and Percent Underreporting in Individuals*
| β coefficient | Std. Error | p-value | |
|---|---|---|---|
| BMI (kg/m2) | −1.3 | 0.2 | <0.001 |
| Sex** | 9.6 | 2.9 | 0.001 |
| Age (y) | −0.1 | 0.2 | 0.77 |
| Education (tertile**) | 1.9 | 1.8 | 0.31 |
| Site vs US | |||
| Seychelles | −12.4 | 4.0 | 0.002 |
| Jamaica | −6.4 | 4.2 | 0.13 |
| South Africa | −38.3 | 4.2 | <0.001 |
| Ghana | −12.6 | 5.1 | 0.013 |
| Intercept | 6.2 | 10.9 | 0.57 |
Dependent variable in the regression model is % underreporting of TEI; a negative β-coefficient indicates an inverse association, i.e., as BMI increases, the TEI/TEE decreases (the percent underreporting is greater)
Men = 0, women = 1; site-specific lowest tertile of education = 1, highest = 3
The degree of underreporting did not correlate with the economic development index as hypothesized. The rank correlation of underreporting ratio versus HDI was f=0.19 (r2, NS).
Effect of Goldberg cutoff
The use of the Goldberg threshold to eliminate physiologically implausible self-reports of energy intake was investigated 19. A large proportion (73%) of the dietary reports fell outside of the Goldberg threshold for dietary energy. The greatest proportion of implausible values was observed in South Africa with 83% of participants failing the Goldberg test. As expected, the use of the Goldberg threshold, however, did reduce the mean value of underreporting, but resulted in the majority of dietary self-reports being dropped. The mean percentages of implausible reporters identified by the Goldberg threshold were 57%, 73%, 75%, 83%, and 64% for the US, Seychelles, Jamaica, South Africa, and Ghana, respectively When limiting the analysis to the sole reports identified as plausible by the Goldberg cutoffs, the reported energy intakes (TEI) were quite similar to the TEE values. The average underreporting relative to TEE in these remaining 94 participants averaged 2±22% (NS).
DISCUSSION
The main conclusion from this study is that adults from five countries across a large HDI spectrum all tend to dramatically underreport dietary energy intake and that these self- reports are therefore invalid estimates of true energy intake. Our findings extend prior findings of underreporting in high HDI countries to those of middle and low-middle HDI. Variation in the magnitude of underreporting between the five countries was not associated with HDI status as we had hypothesized. As expected from findings in high HDI countries, the difference was strongly associated with participants’ BMI. Our findings are the most accurate available to date because underreporting was evaluated using the TEE assessed with the objective DLW criterion method.
We compared underreporting in four of the countries against the US because there have been multiple studies performed in the US using DLW. The OPEN study employed a 24-hour recall and found TEI averaged −18 and −11% less than TEE for females and males, respectively, which is very similar to the TEI among US females in our study, but not as great as found among our US males 20. The OPEN population was older, had accumulated more years of formal education and was mostly white, thus differing in demographic character from the US cohort in our study. In the other large adult study of underreporting by 24-hour recall, results among women also were similar to findings in our cohort (−2004 vs −1766 kJ/d), but again men in our cohort had larger underreports (−2469 vs −356 kJ/d) (21). Again, the participants in this study had different demographic characteristics than participants in our study, e.g. the former were slightly older and racial make-up was not provided. Finally, in one study that included over 118 participants of European and 115 of African ancestries, it was found that those of African ancestry underreported 3 percentage points more than Europeans 22. For comparison with our study, the combined male/female cohort in the Arab et al. study underreported by 11% using a computer-assisted 24-hour recall. Taken together, our US results are not dissimilar to those of reports from other large cohorts, but males in our cohort appear to underreport more than observed by others.
Our study was not the first assessment of underreporting in countries of less than high HDI. In a review by Scagliusi et al., 5, only two DLW studies were identified and third was reported later. A very small study from Swaziland found no underreporting, while results from studies in Mexico and Brazil (−21 and −17%, respectively) were consistent with our findings in the Seychelles, Jamaica, and Ghana. All studies were conducted among females. The study from Swaziland appears to be an outlier possibly due to the small number of participants (n=14) who were young (18–28 years) female students 23. Nine studies from other developing countries in the review by Scagliusi et al. 5 relied on underreporting assessed using the Goldberg criteria rather than TEE measured using the DLW method. Each study used a slightly different method of analysis, but in each population it was also concluded that dietary intake was underreported 5. Mennen et al. 24 conducted the only other multi-country study to our knowledge. This study was also performed in participants of both sexes of African ancestry in urban Jamaica, rural and urban Cameroon, and the United Kingdom. The study used food frequency questionnaires (FFQ) for measuring TEI and a calculated TEE based on predicted RMR and a minimal physiologic activity factor to estimate underreporting 24. The women and men from Jamaica both underreported significantly more than the participants from urban and rural Cameroon. Those from the UK had the highest underreporting values but were very similar to those from Jamaica 24. Thus, although they found underreporting in all countries, they reported a strong relationship between increasing underreporting and increasing economic development, which is in contrast to our findings. MacIntyre et al. 25 also tested the accuracy of a FFQ in a population of South Africans, and made their assessment tool culturally specific by including traditional local foods. They reported a much lower ratio of energy intake to calculated RMR than did Mennen et al 24 for the Cameroonians, suggesting a larger degree of underreporting, which, although less than we observed in South Africans, was more similar to our general findings when we averaged across countries. The percentage of underreporters in these studies varied between 10 and 75% with a median of 22%. In our study the percentage of underreporters using the Goldberg cutoff was much higher and varied from 83% in South Africa to 57% in the United States. Our findings in the South African cohort were surprising compared to the report cited above, which found only 43% of their cohort were classified as underreporters by FFQ, while we employed trained interviewers and a multiple-pass recall, which in other studies has performed better than FFQ.
We found BMI was by far the most consistent predictor of underreporting. It was the strongest predictor and observed in each of the 5 countries. This is consistent with the studies conducted by Mennen et al 24, MacIntyre et al 25, and Bedard et al 26, as well as every study included in the review by Scagliusi et al 5. The consistency between our findings and the results of many other studies strengthens the conclusion that BMI is a major predictor of underreporting in populations of African descent regardless of the degree of social and economic development for the country and does so by providing a more quantitative measure.
Our results with respect to sex, however, did not totally agree with previous studies. While more men were classified as underreporters, the difference between sexes in our multivariate model was smaller than found by others, with the exception of the Seychelles 3, 5 Assessment of underreporting, however, was not the primary aim of METS and thus we did not include measures of body image or social desirability which could help explain underreporting patterns. Differences in body weight ideals between men and women underlie the need for further studies to asses underreporting according to BMI and gender in different socio-cultural contexts. The inclusion of this and other psychological measures would have been valuable to explain site specific differences in underreporting as well as a possible role or modifying effect of education 27. In the United States underreporting only tended to increase with more education, but decreased with more education in South Africa and the Seychelles, while no association was seen in the other two countries. We suggest that further studies of dietary underreporting include psychological and cultural measures, as well as indicators of political or social significance. For example, participants in some situations may fear losing food- assistance if they report a large dietary intake or may feel a general distrust of authorities and purposely try minimize information provided to authority figures.
To provide a comparison with several other studies, we applied the Goldberg cutoff method to our data set in order to eliminate dietary reports in which the reported intake was so low relative to physiologic energy requirements that it can be reasoned the reported intake is too low to represent habitual energy intake 19. After eliminating reported intakes that were ≤ 1.35 × REE we did find that the average reported energy intakes did not differ from the energy expenditure biomarker of habitual energy intake. The use of the Goldberg cutoff, however, had a significant cost with regard to loss of data. This cutoff eliminated 73% of the intake records and raises concern over whether the remaining data are representative of all of the cohorts.
The severe under-reporting from the South African cohort was unexpected and cannot be explained based on the data we collected. The TEE values used as the criterion method for estimating habitual energy intake fell on the same line describing the relationship between TEE and fat-free mass and the fat-free masses were consistent with the participant BMIs (data not presented). As indicated above, the dietary coding as performed at Loyola was double checked and confirmed by the co-investigator from South Africa, who had adapted the recall methodology for use in the METS study. As such, we do not believe the discrepancy is due to methodological error. We are left to speculate that severe under-reporting by the South African cohort is due to a concern by participants over loss of food assistance or some other factor that caused them to resist answering the dietary recall questions more accurately.
As indicated above, one of the limitations of this data analysis is the absence of psychological measures. A further limitation of our study is that the participant samples were not representative of the country as a whole and our results are therefore more reflective of the community from which the data were taken. It is probable that there is more variation within each country than we report here. Also, virtually all subjects were of African ancestry by design and inference of our findings is thus limited to a single race, although to multiple countries of origin. The 24-hour recalls cover only a short time-frame and were carried out mostly during weekdays and thus may not be completely representative of the average for the participant had weekends been included. Seasonal effects could have skewed these measurements as well as personal situations such as injury or illness to prevent physical activity. In addition, different individuals collected the dietary data in each site, which could lead to biases between countries in our measurements.
Another limitation of our study is that 51 participants in the study were not included in the final analysis. The number of lost cases were not unexpected, however. There were 19 participants who did not have TEE values, which is close to the 4% average for other studies. Those without dietary recall data were 3% of the cohort, which does not seem excessive, and the 4% eliminated as outside 2 SD of the country specific mean with respect to reporting error was as expected based on statistics. It should also be noted that the characteristics of these participants were within 0.33 SD units of the means 324 subjects reported herein with respect to height, weight, age, and years of education and where data was available for dietary energy recall and TEE. The 17 excluded as outliers did display a trend away from under-reporting, but their inclusion would have changed the mean underreporting for the cohort from −27% to −23%, which would not have influenced the conclusions.
A major inference from our study is that underreporting of dietary intake among adults appears to be an almost universal problem. Such underreporting complicates the study of diet and health because without an accurate picture of what an individual is consuming on a regular basis, care should be taken when interpreting any study based on self-reported dietary data. Clearly, our study and others invalidate the use of self-reported energy intake data for use in estimating energy balance until an accurate assessment method is identified. Also, because it is still unclear what components of the diet are underreported, self-reported dietary pattern data must be interpreted with caution 28–30. Our study found that dietary intake underreporting was strongly associated with BMI. Since social patterning of BMI may differ in low and high income countries, further studies should assess cross-cultural mechanisms underlying the association between BMI and underreporting, e.g. body weight ideals in different socio-cultural contexts. This study and others further demonstrate the need for research directed towards development of objective methods for the measurement of diet.
Figure 3.
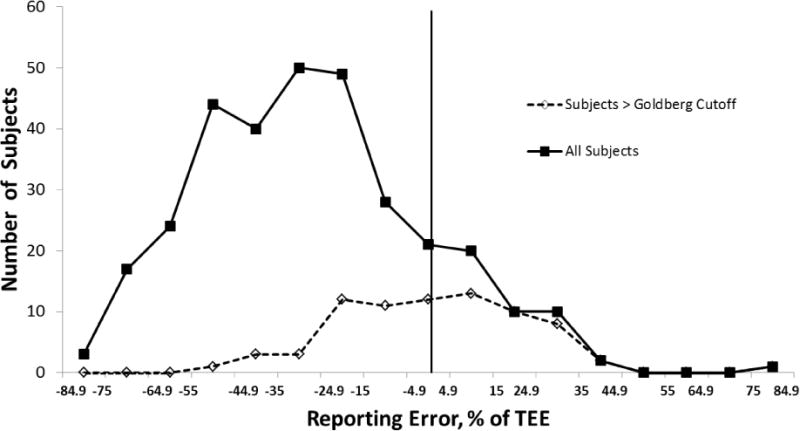
Distribution of energy intake reporting error relative to measured total energy expenditure for the entire cohort (solid line) and those that pass the Goldberg cutoff of 1.35 × predicted resting energy expenditure (dotted line). The vertical line represents 0% error.
Acknowledgments
We would like to thank the METS participants as well as the field staffs in each of our study sites.
FINANCIAL SUPPORT
This research was supported in part by the National Institutes of Health (DK080763).
Footnotes
CONFLICT OF INTEREST
DAS is a co-inventor on a patent application for a method to estimate energy balance.
AUTHOR CONTRIBUTIONS
Each of the authors made a substantive contribution to the completion of this manuscript. AL, JPR, PB, TEF, EVL, LRD, RAD and DAS were instrumental in formulating the research questions in the METS project. AL, JPR, PB, TEF, EVL, LRD, RAD, RSC and DAS were involved in designing the study as it was conducted. EK carried out the dietary assessments across all sites and LO conducted the laboratory work. LO, AL, LRD and DAS contributed to data analysis. LO, AL, PB, LRD and DAS contributed to the writing and editing of the final manuscript.
References
- 1.World Health Organization. Global Database on Body Mass Index. 2006 http://apps.who.int/bmi/ (accessed June 2014)
- 2.Trabulsi J, Schoeller DA. Evaluation of dietary assessment instruments against doubly labeled water, a biomarker of habitual energy intake. Am J Physiol Endcrinol Metab. 2001;281:E891–E899. doi: 10.1152/ajpendo.2001.281.5.E891. [DOI] [PubMed] [Google Scholar]
- 3.Subar AF, Kipnis V, Troiano RP, et al. Using intake biomarkers to evaluate the extent of dietary misreporting in a large sample of adults: The observing protein and energy nutrition (OPEN) study. Am J Epidemiol. 2003;158:1–13. doi: 10.1093/aje/kwg092. [DOI] [PubMed] [Google Scholar]
- 4.Neuhouser M, Tinker L, Shaw PA, et al. Use of recovery biomarkers to calibrate nutrient consumption self-reports in the Women’s health initiative. Am J Epidemiol. 2008;167:1247–1259. doi: 10.1093/aje/kwn026. [DOI] [PubMed] [Google Scholar]
- 5.Scagliusi FB, Ferriolli E, Lancha AH., Jr Underreporting of energy intake in developing nations. Nutr Rev. 2006;64:319–330. doi: 10.1301/nr.2006.jul.319-330. [DOI] [PubMed] [Google Scholar]
- 6.Frankenfield D, Roth-Yousey L, Compher C. Comparison of predictive equations for resting metabolic rate in healthy nonobese and obese adults: A systematic review. J Am Diet Assoc. 2005;105:775–789. doi: 10.1016/j.jada.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Schoeller DA. Validation of habitual energy intake. Public Health Nutr. 2002;5:883–888. doi: 10.1079/PHN2002378. [DOI] [PubMed] [Google Scholar]
- 8.Prentice AM, Black AE, Coward WA, et al. High levels of energy expenditure in obese women. Br Med J (Clin Res Ed) 1986;292:983–987. doi: 10.1136/bmj.292.6526.983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luke A, Bovet P, Forrester TE, et al. Protocol for the modeling the epidemiologic transition study: A longitudinal observational study of energy balance and change in body weight, diabetes and cardiovascular disease risk. BMC Public Health. 2011;11:927. doi: 10.1186/1471-2458-11-927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barro RJ, Lee JW. A New Data Set of Educational Attainment in the World, 1950–2010. The National Bureau of Economic Research. 2010 http://www.nber.org/papers/w15902 (accessed April 2011)
- 11.Gibson RS. The Principles of Nutritional Assessment. 2nd. New York: Oxford University Press; 1990. Methods for measuring food consumption of individuals; pp. 41–43. [Google Scholar]
- 12.Steyn NP, Senekal M. A Guide for the Use of the Dietary Assessment and Education Kit (DAEK) Medical Research Council of South Africa; Cape Town, South Africa: 2005. [Google Scholar]
- 13.Sharma S, Yacavone XC, Samuda PM, et al. Nutritional composition of commonly consumed composite dishes for Afro-Carribbeans (mainly Jamaicans) in the United Kingdom. Intl J Food Sci Nutr. 2009;60:140–50. doi: 10.1080/09637480902755079. [DOI] [PubMed] [Google Scholar]
- 14.U.S. Department of Health Education and Welfare and Food - Nutrition Program, Agricultural Organization of the United Nations. Food Composition Table for Use in Africa. Bethesda, MD: Public Health Service; 1968. [Google Scholar]
- 15.The Caribbean and Nutrition Institute. Food Composition Tables for Use in the English-speaking Caribbean. Vienna: World Health Organization; 1998. [Google Scholar]
- 16.Langenhovan ML, Conradle PJ, Wolmarans P, et al. MRC Food Quantities Manual. 2nd. Cape Town, South Africa: Medical Research Council; 1991. [Google Scholar]
- 17.Sehmi JK. National Food Composition Tables and the Planning of Satisfactory Diets in Kenya. Nairobi, Kenya: Ministry of Health; 1993. [Google Scholar]
- 18.International Atomic Energy Agency. (IAEA Human Health Series No. 3).Assessment of Body Composition and Total Energy Expenditure in Humans Using Stable Isotope Techniques. 2009 http://www-pub.iaea.org/MTCD/publications/PDF/Pub1370_web.pdf.
- 19.Goldberg GR, Black AE, Jebb SA, et al. Critical evaluation of energy intake data using fundamental principles of energy physiology: 1. Derivation of cut-off limits to identify under-recording. Eur J Clin Nutr. 1991;45:569–581. [PubMed] [Google Scholar]
- 20.Tooze JA, Krebs-Smith SM, Troiano RP, et al. The accuracy of the Goldberg method for classifying misreporters of energy intake on a food frequency questionnaire and 24-h recalls: comparison with doubly labeled water. Eur J Clin Nutr. 2012;66:569–576. doi: 10.1038/ejcn.2011.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Novotny JA, Rumpler WV, Riddick H, et al. Personality characteristics as predictors of underreporting of energy intake on 24-hour dietary recall interviews. J Am Diet Assoc. 2003;103:1146–1151. doi: 10.1016/s0002-8223(03)00975-1. [DOI] [PubMed] [Google Scholar]
- 22.Arab L, Tseng CH, Ang A, et al. Validity of a multipass, web-based, 24-hour self-administered recall for assessment of total energy intake in blacks and whites. Am J Epidemiol. 2011;174:1256–1265. doi: 10.1093/aje/kwr224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huss-Asmore R, Goodman JL, Sibiya TE, et al. Energy expenditure of young Swazi women as measured by the doubly labeled water method. Eur J Clin Nutr. 1989;43:737–774. [PubMed] [Google Scholar]
- 24.Mennen LI, Jackson M, Cade J. Underreporting of energy intake in four populations of African origin. Int J Obes Metab Disord. 2000;24:882–887. doi: 10.1038/sj.ijo.0801246. [DOI] [PubMed] [Google Scholar]
- 25.MacIntyre UE, Venter CS, Vorster HH. A culture-sensitive quantitative food frequency questionnaire used in an African population: 2. Relative validation by 7-day weighted records and biomarkers. Public Health Nutr. 2001;4:45–51. doi: 10.1079/phn200041. [DOI] [PubMed] [Google Scholar]
- 26.Bedard D, Shatenstein B, Nadon S. Underreporting of energy intake from a self-administered food-frequency questionnaire completed by adults in Montreal. Public Health Nutr. 2004;7:675–681. doi: 10.1079/PHN2003578. [DOI] [PubMed] [Google Scholar]
- 27.Alwan H, Viswanathan B, Williams J, et al. Association between weight perception and socioeconomic status among adults in the Seychelles. BMC Public Health. 2010;10:467. doi: 10.1186/1471-2458-10-467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lafay L, Mennen L, Basdevant A, et al. Does energy intake underreporting involve all kinds of food or only specific food items? Results from the Fleurbaix Laventie Ville Santé (FLVS) study. Int J Obes Relat Metab Disord. 2000;24:1500–1506. doi: 10.1038/sj.ijo.0801392. [DOI] [PubMed] [Google Scholar]
- 29.Cagliusi FB, Ferriolli E, Pfrimer K, et al. Under-reporting of energy intake is more prevalent in a healthy dietary pattern cluster. Br J Nutr. 2010;100:1060–1068. doi: 10.1017/S0007114508971300. [DOI] [PubMed] [Google Scholar]
- 30.Suchanek P, Poledne R, Hubacek JA. Dietary intake reports fidelity–fact or fiction? Neuro Endocrinol Lett. 2011;32(Suppl 2):29–31. [PubMed] [Google Scholar]


