Abstract
Objective
To examine the mediating role of parenting stress (both parental distress and stress due to dysfunctional interactions in the mother-daughter relationship [PSDI]) in the link between childhood attention-deficit/hyperactivity disorder (ADHD) status and several important young-adult outcomes.
Methods
The diverse sample comprised 140 girls with ADHD and 88 age- and ethnicity-matched comparisons, evaluated at ages 6–12 years and followed prospectively for 5 years (mean age = 14.2) and 10 years (mean age = 19.6).
Results
(a) The PSDI experienced by a mother during her daughter’s adolescence mediated the link between her daughter’s childhood ADHD status and adult externalizing and internalizing symptoms. (b) PSDI also mediated the link between ADHD status and young adult non-suicidal self-injury and had an indirect effect in the relation between childhood ADHD and young-adult depressive symptoms. (c) The mediating role of PSDI with respect to internalizing symptoms and depressive symptoms remained in place even when covarying adolescent internalizing/depressive symptoms.
Conclusion
Parenting stress, particularly related to maternal perceptions of dysfunctional interactions with adolescent daughters, serves as a key mediator in the association between childhood ADHD status and important domains of young-adult functioning. Minimizing parenting stress and dysfunctional mother-daughter interactions during adolescence might reduce the risk of adverse adult outcomes for girls with ADHD.
Keywords: attention-deficit/hyperactivity disorder, parenting, parent-child relationship, stress
Numerous studies have shown that a majority of children diagnosed with attention-deficit/hyperactivity disorder (ADHD) continue to experience detrimental impairments in adulthood and are prone to more adverse outcomes than their peers. In particular, these individuals experience lower educational attainment (e.g., complete fewer years of education with lower grade point averages), have poorer work performance, and show more social problems than other young adults (Barkley, Fischer, Smallish, and Fletcher, 2006; Biederman, et al., 2008; see reviews in Barkley, 2015; Hinshaw & Scheffler, 2014). Furthermore, children diagnosed with ADHD also have an elevated risk of developing other psychiatric disorders—including antisocial, anxiety, mood, and substance use disorders—by early adulthood (Biederman et al., 2006; Meinzer et al., 2013; Charach, Yeung, Troy, & Lillie, 2011). However, little is known about how parenting-related stress experienced by the parents of these children during adolescence may influence these outcomes. Our objective is to investigate the mediating role of parenting stress—particularly the stress experienced by the parents of girls with ADHD during adolescence—in the development of adverse young adult outcomes.
Parenting and Related Stress
It has been well-established that parenting is part of a bidirectional and dynamic process in which both the parent and child influence each other (Pettit & Arsiwalla, 2008; see also Bell, 1968, for a classic formulation). In some parent-child dyads, this bidirectional process can perpetuate increasingly negative, transactional interactions, which can lead to the development of problem behaviors. In particular, Patterson’s (2002) coercion model postulates that unskilled parents, in an attempt to control a defiant and oppositional child, may inadvertently reinforce problem behavior by increasing their initial aversive reaction to the child’s behavior and then eventually relenting when the child’s behavior worsens. Ultimately, the parent learns to withdraw in order to avoid these aversive interactions. This pattern of coercion negatively influences the parent-child relationship and increases the child’s risk for the development of deviant behaviors, particularly aggression (Patterson, 2002).
Abidin’s model focuses on parental stress in the attempt to explain why some parents are prone to engage in dysfunctional parenting (Abidin, 1992). Parental stress can be described as the negative feelings that a parent has toward the self or toward his or her children, which result from a mismatch between perceived resources and the demands of his or her parenting role (Morgan, Robinson, & Aldridge, 2002; Deater-Deckard, 1998). Abidin posits that the amount of parenting stress experienced by a parent is a function of both parental characteristics (e.g., their sense of competence; the quality of their relationship with their child) and the child’s characteristics (e.g., adaptability; demandingness). In combination with life stressors (e.g., loss; divorce), these mutually interactive characteristics can lead to increased risk for dysfunctional parenting (Abidin, 1995; Morgan et al., 2002).
Pelham et al. (1997) examined the effects of child behavior on parental stress. Parents were asked to interact with child confederates who either displayed typical behavior or were trained to display the symptoms of a behavioral disorder. Those parents who interacted with a child mimicking externalizing behavior reported more distress, greater feelings of role inadequacy, and more anxiety, depression, and hostility than those parents interacting with control confederates. Crucially, when this group of parents was subsequently given unlimited access to alcohol while waiting to engage in a second interaction with the same child, they consumed more alcohol than the control parents. Thus, the child’s problematic behavior not only influenced the level of distress felt by the parent but also subsequent parental coping strategies.
Stress in Families with Children with ADHD
Parents of children with ADHD may be particularly prone to parenting stress because, as a function of their children’s symptoms, they may experience greater parenting demands than other parents. For example, DuPaul, McGoey, Eckert, and VanBrankle (2001) found that, when asked to perform a task by their parents, children with ADHD exhibited twice the level of noncompliance and had levels of inappropriate behaviors that were equivalent to five times the levels displayed by control children. Their parents concurrently reported higher levels of stress than parents of children without ADHD. The association between a child’s ADHD symptoms and parental stress is likely to be mediated by the child’s difficulty with self-regulation (Graziano, McNamara, Geffken, & Reid, 2011). That is, parents of children with ADHD may have to exert considerable effort to correct their children’s behaviors and to compensate for their children’s difficulties with behavioral and emotion self-regulation, which may, in turn, lead them to experience parenting stress. As a result, these parents have trouble utilizing appropriate coping strategies when faced with stressful situations (DuPaul et al., 2001).
Parents of children with ADHD are also prone to dysfunctional interactions with their children and, thus, may be susceptible to the stress associated with these interactions. In particular, such parents tend to display more negative behaviors toward their children than other parents and respond to problematic behaviors with higher levels of reprimands and corrective actions (DuPaul et al, 2001; Modesto-Lowe, Danforth, & Brooks, 2008). The direction of effects is substantially related to the child’s problem behavior. For example, Barkley, Karlsson, Pollard, and Murphy (1985) showed that the receipt of stimulant medication by the child with ADHD reduced parental control and direction. This linked to the child’s greater compliance and attention.
Past research has also linked negative parental behaviors to reciprocal increases in problematic behavior in children with ADHD. In particular, negative maternal behaviors during parent-child interactions have been associated with stealing and noncompliance during classroom and playground activities in boys with ADHD, even taking into account the boys’ levels of noncompliance and negativity during the parent-child interactions (Anderson, Hinshaw, & Simmel, 1994). Aggressive discipline methods and poor parental coping strategies have also been associated with increases in hyperactive symptoms in children with ADHD (Woodward, Taylor, & Dowdney, 1998). Such effects are even found in adoptive families of children with ADHD symptoms (see Harold et al., 2013), which control for gene-environment correlation, revealing that psychosocial as well as genetic processes are at work. In short, dysfunction within families of children with ADHD may be perpetuated by a bidirectional process in which adverse actions from both the parent and the child influence each other, fueling additional stress in the relationship as well as parental perceptions of negativity in relevant interactions.
The stress fueled by dysfunctional parent-child interactions may be particularly salient as children transition to adolescence. During this transition, adolescents begin to spend less time with their parents and more time with peers, and they begin to make normative bids for more autonomy (Eccles, 1999). This tendency is likely to increase tension in the parent-child relationship. Specifically, parents report increases in the affective intensity of parent-child conflict during adolescence (Laursen, Coy, & Collins, 1998). Accordingly, parents report parenting a 14-year-old child as being more stressful than parenting a 10-year-old child. In particular, they report increases in the stress associated with dysfunctional parent-child interactions as their child enters teenage years (Putnick, Bornstein, Hendricks, Painter, Suwalsky & Collins, 2010). Families of adolescents with ADHD—particularly those with comorbid oppositional defiant disorder—have been shown to display more conflict than families of comparison adolescents (Barkley, Fischer, Edelbrock, & Smallish, 1991). Thus, these families are prone to experience higher levels of stress associated with such dysfunctional interactions than other families.
Managing parental stress is important because such stress is associated with poor outcomes in children. For example, parenting stress has been shown to be a predictor of behavioral problems and externalizing issues in young children (Benzies, Harrison, & Magill-Evans, 2004; Heller, Baker, Henker, & Hinshaw, 1996). Parental stress related to dysfunctional interactions in the parent-child relationship has been linked to later offspring internalizing symptoms during adolescence (Costa, Weems, Pellerin, & Dalton, 2006). Yet few studies have examined the associations between stress experienced by parents and longer-term child outcomes, extending into young adulthood. This empirical gap is particularly wide for families with children diagnosed with ADHD, particularly for girls with this condition. Because females normatively begin to experience increases in internalizing behaviors as they transition to adolescence (Nolen-Hoeksema & Girgus, 1994), they may be more likely than their male peers to develop internalizing symptoms in response to the stress experienced by their parents during this period. Hence, our focus herein is on the role of parental stress—specifically during adolescence, a particularly challenging period for the parent-child relationship—on key youngadult problems domains in their female offspring.
As noted above, children with ADHD are more prone to adverse adult outcomes than their peers. In addition to poorer education, social, and occupational outcomes, recent research has suggested that they have increased risk for self-harm behaviors in early adulthood. Specifically, young women with a childhood diagnosis of ADHD (particularly when marked by impulsivity) reported far more non-suicidal self-injury (NSSI) and suicide attempts than comparison women (Swanson, Owens, & Hinshaw, 2014). Thus, we investigate the role of parental stress in such elevated risk for NSSI and suicide, as well as for outcomes of depression, internalizing symptoms more generally, and externalizing symptoms.
Hypotheses
We investigate two aspects of parental stress: parental distress and stress-inducing dysfunctional parent-child interactions (PSDI). Parental distress refers to the personal stress that a parent has over his or her parenting role, whereas PSDI addresses a parent’s perception of dysfunction in the parent-child relationship that contributes to his or her feelings of parental stress. Because parents of children with ADHD tend to experience greater parenting demands than other parents, we predict that they will report more parental distress and PSDI than parents of our comparison sample. We also specifically examine how these aspects of stress mediate the pathways between childhood ADHD status and six young-adult criterion measures (i.e., self-reported depressive symptoms; self- and parent-reported externalizing and internalizing symptoms; NSSI severity and frequency; and suicide attempts). Accordingly, for all six outcomes, we expect that both indicators of parental stress (i.e., distress and PSDI) will mediate the links between childhood ADHD status and their young-adult outcomes.
Method
Overview
The current data were drawn from a longitudinal study of elementary-school-aged girls with and without ADHD. Initial data were collected during three summer enrichment programs that took place from 1997 to 1999. Each summer, a new cohort of girls with ADHD participated in a five-week program that offered a combination of classroom, art, drama, and playground activities, along with a group-matched comparison sample of girls without ADHD. Specifically, comparison girls were recruited to be similar, in terms of age and ethnicity, to the ADHD sample. Parents and teachers completed questionnaires as part of the screening process; girls and their families then went through a thorough assessment battery pertaining to ADHD status as well as comorbidities, impairments, and academic, social, and cognitive functioning. All evaluations were conducted during a period in which girls with prior medication histories were not receiving stimulant medication. See Hinshaw (2002) for additional details.
The families were invited to participate in 5-year and 10-year follow-up studies after their initial participation. Participants completed a thorough evaluation, spanning two half-days at our lab/clinic (occasionally, telephone interviews or home visits were performed). Hinshaw, Owens, Sami, & Fargeon (2006) and Hinshaw et al. (2012) provide full information about the follow-up.
Participants
The original sample consisted of 140 girls with ADHD (mean age = 9.7) and 88 comparison girls (mean age = 9.4) at baseline (Wave 1). The sample was ethnically diverse (53% White, 27% African American, 11% Latina, and 9% Asian American). The ADHD sample was recruited through medical settings (e.g., health maintenance organizations), mental health centers, pediatric practices, and local school districts. Advertisements were also placed in local newspapers and parenting newsletters. Comparison girls were recruited through school districts and local community centers and through advertisements in the local newspapers and parenting newsletters. Eligible families were sent packets about the program and then screened for ADHD status. ADHD diagnosis was made on the basis of initial ratings from parents and teachers, with initial screening criteria set somewhat low to avoid prematurely excluding potentially eligible girls. Yet for final eligibility in the ADHD group, the girl had to meet full criteria for ADHD (either Combined or Inattentive type) with respect to diagnostic interview criteria (i.e., at least six impairing symptoms of inattention for ADHD-Inattentive or at least six inattention and six hyperactivity-impulsivity symptoms for ADHD-Combined). For eligibility in the comparison group, a diagnosis of ADHD needed to be absent (see Hinshaw, 2002).
Of the original 228 families, 209 (92%) participated in the five-year follow-up study (designated as Wave 2; mean age = 14.2) and 216 (95%) participated in the 10-year follow-up study (designated as Wave 3: mean age = 19.6). See Hinshaw et al. (2006) and Hinshaw et al. 2012) for more information. The parental stress measures below were administered at the Wave 2 follow-up; the primary caregiver served as the informant. In 94% of the cases, this was the child’s mother (1% were fathers, 1% were stepmothers, 3% were grandmothers, and 1% were other relatives). In order to focus on the parental stress that is specific to mothers, we only included those families in which the parental stress measure was completed by the mother (120 girls with ADHD and 81 comparison girls) in our analysis.
Measures
Parental Stress during adolescence
Parenting distress and parental stress regarding dysfunctional interactions (PSDI)
These constructs were assessed via the Parenting Stress Index-Short Form (PSI-SF), a self-report measure assessing the personal stress experienced by parents in their parenting role (Abidin, 1995). Mothers rated each item on a 5-point scale (5 = strongly disagree, 1 = strongly agree). The subscale tapping parental distress consists of 12 items (e.g., “I feel that I cannot handle things”) that measure the stress a parent feels in her/his parental role. The Parental-Child Dysfunctional Interaction subscale, which taps PSDI, consists of 12 items (e.g., “My child does not like me or want to be close”) that focus on parents’ perception of their interactions with their child and their perception of how reinforcing their child is toward them (Abidin, 1995). The items were coded so that higher scores represent higher levels of stress-related dysfunctional interactions. The test-retest reliability and internal consistency of the PSI-SF have been well established, with the reliability of the subscales ranging from .68 to .85 and the internal consistency ranging from .80 to .87 (Abidin & Brunner, 1995). Previous research has also established its validity with respect to other indicators of parental stress and family dysfunction (Haskett, Ahern, Ward, & Allaire, 2006). In our sample, the internal consistency (Cronbach’s alpha) of the parental distress scale and the dysfunctional interaction scale (measuring PSDI) at Wave 2 were .87 and .89 respectively.
Young-adult outcomes
Externalizing and internalizing behaviors
Composites of scores using data from both the Adult Behavior Checklist (ABCL) and the Adult Self Report (ASR) were created to measure externalizing and internalizing behaviors. The ABCL and ASR are 126-item measures that parallel each other. ABCL is completed by a caregiver, whereas the ASR is completed by the young adult. Both informants are asked to rate items assessing the young adult’s behavior using a 3-point scale (0 = never happened; 2 = happened with great frequency or great intensity). These measures have extensively established internal consistency, test-retest reliability, and validity. Cronbach’s alphas for the internalizing and the externalizing scales have been reported at as .80 and .92, respectively on the ABCL, with parallel figures being .89 and .91 for the ASR (Achenbach & Rescorla, 2003). The raw scores on these scales are converted to T-scores using age and gender norms. Composites were then created by taking the mean of these scores. In our study, the parent-reported ABCL was correlated with the ASR at r (170) =.44, p <.001 for internalizing behaviors and r (170) =.49, p <.001 for externalizing behaviors.
Youth-reported depression
The young women’s self-reported depressive symptoms were measured via the Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996). This measure comprises 21 items and is used to assess the presence of depressive symptoms including negative mood, interpersonal problems, and negative self-esteem. Participants are asked to rate the presence of each symptom during the past two weeks on a 4 point scale (i.e. “0” indicates an absence of a symptom; “3” indicates the presence of an extreme form of a symptom). Both the test-retest reliability and internal consistency of the CDI have been well established: internal consistency = .92 in outpatient populations and .93 in college age students; test–retest reliability averages .93 (Beck et al., 1996). In our sample, the internal consistency of this measure was .93.
Nonsuicidal Self-injury (NSSI)
NSSI was assessed using a modified version of the Self-Injury Questionnaire (SIQ) for which participants were asked if they had deliberately injured themselves in the past year using six different methods (Claes, Vandereycken, & Vertommen, 2001). If a method was endorsed, participants were asked how frequently they engaged in this method on a 6-point scale (1 = only once; 6= a couple of times a day). A sum of the frequency of scores across the six methods was taken and used in the present analyses. This measure was validated in a sample of individuals with eating disorders and was found to have an internal consistency of .621 (see Vanderlinden & Vandereychen, 1997; Claes & Vandereycken, 2007). A similar internal consistency of .60 was found in our sample. A 4-point score assessing the severity of NSSI endorsed was also created. This score was informed by a lethality continuum of potential tissue damage postulated by Skeggs (2005) and confirmed by factor analysis. It was created based on the highest level of severity endorsed on the SIQ with a score of “0” representing non-endorsement of any NSSI behaviors,”1” representing low severity of NSSI methods, “2” representing mild-moderate severity of NSSI methods, and “3” representing the endorsement of the highest level of severity (see Swanson et al., 2014).
Number of suicide attempts
The Barkley Suicide Questionnaire (Barkley & Murphy, 2006) and the Family Information Packet (FIP) were used to assess suicide attempts. The Barkley Suicide Questionnaire is a self-report questionnaire in which participants were asked three yes/no questions: “have you ever attempted suicide”, “have you ever considered suicide”, “have you ever been hospitalized for an attempt?” The FIP, which was completed by the parents, was a comprehensive, year-by-year grid requesting information about significant events in the young adult’s life, including suicide attempts. Information from both measures was used to create a dichotomous self-injury variable indicating whether or not a participant had made a suicide attempt. In the single case for which an attempt was endorsed on the FIP but not on the Barkley Suicide Questionnaire, the individual was counted as positive for a suicide attempt.
Covariates
Several important background variables, scored at Wave 1, were included as covariates in the mediation analyses: (a) age, (b) maternal education, and (c) parent-reported family income. We also performed a second set of analyses with the young women’s adolescent externalizing, internalizing, and depressive symptoms as covariates, in order to assess the mediating role of parental stress in the link between ADHD and the development of internalizing, externalizing, and depressive symptoms, beyond levels of those same outcomes measured during adolescence. That is, for each adult criterion variable, we added the respective adolescent variable as a covariate in addition to age, maternal education, and family income. The girls’ adolescent internalizing and externalizing symptoms were reported by the mothers in Wave 2 using the Child Behavior Checklist (CBCL), which is a 113-item measure that parallels the ABCL (Achenbach, 1991). The girls’ adolescent depressive symptoms were self-reported using the short form of the Children's Depression Inventory (Kovacs, 1992).
In previous findings, we have found that externalizing symptoms mediated the link between childhood ADHD status and young adult NSSI, whereas internalizing symptoms mediated the link between childhood ADHD status and young adult suicide attempts (Swanson et al., 2014). Thus, for NSSI frequency and severity we used adolescent externalizing symptoms as the additional covariate; for suicide attempt count we used internalizing symptoms.
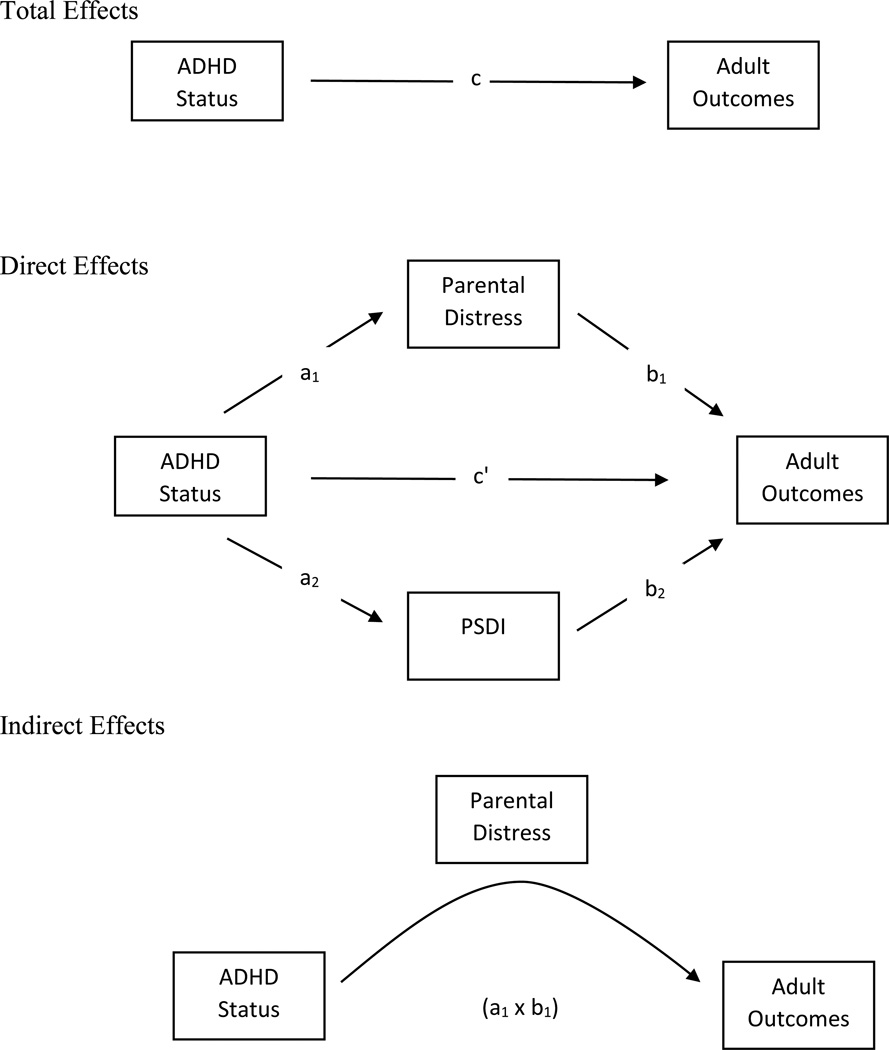
Statistical Analyses
Statistical analyses were performed using SPSS Version 22. T-tests were conducted to assess diagnostic group differences with respect to covariates, putative mediator variables, and young-adult criterion measures. We then performed sophisticated mediator analyses with the bootstrapping procedure of Preacher and Hayes (2008) to examine the mediating role of each of the two parental stress measures in the link between childhood ADHD status and each criterion variable. In this procedure, 10,000 random samples are drawn from the original data with replacement. A point estimate of the mediated effect is determined for each sample, with 95% bias-corrected confidence intervals determined from the distribution of these estimates. Intervals are considered statistically significant if they do not contain 0. Least-squares regressions were performed to ensure that predictor-mediator and mediator-outcome pathways were in hypothesized directions. We only performed multi-meditator models for those criterion measures that were significantly correlated with both mediator variables. In those models, Wave 1 ADHD status was the predictor, Wave 2 parental distress and PSDI were tested together as potential mediators, and each Wave 3 outcome variable (i.e., internalizing symptoms, self-reported depression symptoms, externalizing symptoms, NSSI severity, NSSI frequency, and suicide attempt count) served as the criterion measure. Figure 1 provides a graphical representation of the pathways and effects explored. We performed the meditational analyses both with and without use of the adolescent psychopathology covariates (see Covariates, above).
Figure 1.
Graphical Representation of Mediation Model. The total effect is composed of the direct effect (c’) and indirect effects (the product of a and b). (See Preacher and Hayes, 2008 for more information)
Results
Table 1 presents scores for the ADHD and comparison samples with respect to demographic, mediating, and behavioral variables. The diagnostic groups were statistically indistinguishable with respect to age, family income, and maternal education. However, a chisquare test did reveal a significant difference in the ethnic composition of the groups, χ2(4), N = 201 = 9.30, p <.05, with a higher percentage of Asian American girls in the comparison group. Furthermore, the young women who were diagnosed with ADHD in childhood had far worse scores on all adult behavioral outcomes, and their mothers also had significantly higher Wave 2 parental distress and PSDI scores than the mothers of comparison girls.
Table 1.
Demographics, Mediators, and Outcome Variables
| ADHDa | Comparisonb | T-test | Cohen’s | |||
|---|---|---|---|---|---|---|
| M | SD | M | SD | t (df) | d | |
| Demographic Variables (Wave 1) | ||||||
| Age (months) | 115.95 | 20.66 | 111.84 | 19.30 | −1.42 (199) | .21 |
| Ethnicity (%) | ||||||
| Caucasian | 60.8 | 46.9 | ||||
| African American | 22.5 | 27.2 | ||||
| Hispanic | 11.7 | 11.1 | ||||
| Asian American | 4.2 | 14.8 | ||||
| Total Annual Family Incomec | 6.47 | 2.59 | 6.81 | 2.37 | .94 (197) | −.14 |
| Maternal Educationd | 4.76 | .88 | 4.98 | .95 | 1.66 (199) | −.24 |
| Mediators (Wave 2) | ||||||
| Parental Distress | 2.24 | .80 | 1.88 | .55 | −3.69 (192)** | .52 |
| PSDI | 2.25 | .80 | 1.68 | .67 | −5.35 (192)** | .77 |
| Adolescent Covariates (Wave2) | ||||||
| Internalizing Behaviors | 56.50 | 10.81 | 45.57 | 10.94 | −6.92 (194)** | 1.01 |
| Externalizing Behaviors | 61.67 | 10.87 | 45.80 | 9.92 | −10.38 (194)** | 1.53 |
| Self-reported BDI | 7.53 | 5.87 | 5.01 | 5.28 | −3.10 (198)** | .45 |
| Outcome Variables (Wave 3) | ||||||
| Internalizing Behaviors | 56.83 | 11.29 | 49.04 | 10.57 | −4.84 (190)** | .71 |
| Externalizing Behaviors | 59.43 | 10.25 | 48.64 | 8.56 | −7.69 (190)** | 1.14 |
| Self-reported BDI | 11.37 | 10.18 | 8.32 | 10.72 | −1.99 (187)* | .29 |
| NSSI Frequency | 3.01 | 4.47 | .93 | 1.83 | −4.28 (176)** | .61 |
| NSSI Severity | .93 | 1.07 | .32 | .66 | −4.70 (177)** | .69 |
| Suicide Attempt Counte | 19 (17.1%) | 4 (5.1%) | ||||
Notes: PSDI= Parental Stress due to Dysfunctional Parent-Child Interactions; NSSI= Nonsuicidal Self-Injury
n=120
n=81
For total annual family income, 1 <$10,000; 9 >$75,000.
For maternal education, 1 = less than 8th grade; 6 = advanced or professional degree
For suicide attempt count, χ2(1, N = 199) = 6.30, p <.05
p < .05,
p < .01.
Table 2 presents intercorrelations between the parental stress and behavioral variables. Neither of the parenting stress variables was significantly correlated with suicide attempt count. Thus, mediational analyses were not performed for this criterion measure. Parental distress was also not significantly correlated with depressive symptoms, but PSDI was. Thus, for the meditational analyses including depressive symptoms, only PSDI was explored as a possible mediator.
Table 2.
Summary of Correlations for Mediators and Outcomes
| Measures | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. W2 Parental Distress |
- | - | - | - | - | - | - |
| 2. W2 PSDI |
.69** | - | - | - | - | - | - |
| 3. Externalizing Behaviors |
.30** | .43** | - | - | - | - | - |
| 4.Internalizing Behaviors |
.30** | .47** | .75** | - | - | - | - |
| 5. Self-Reported BDI |
.09 | .22** | .57** | .65** | - | - | - |
| 6. NSSI Frequency |
.23** | .21** | .33** | .33** | .22** | - | - |
| 7. NSSI Severity |
.28** | .30** | .38** | .36** | .23** | .80** | - |
| 8. Suicide Attempt Count |
.13 | .11 | .22* | .33** | .18** | .46** | .50** |
p < .05
p < .01.
Mediational Analyses
The results for the mediational analyses are presented in Tables 3, 4, 5, and 6.
Table 3.
Summary of mediation results with age, maternal education, and family income as covariates
| Dependent variable (DV) and Mediators (M) |
Effects of IV on M (a) |
Effects of M on DV (b) |
Indirect effects (a x b) |
Bootstrap 95% CI for Indirect Effects |
Direct effects (c’) |
Total effects (c) |
Adj. R2 for Model |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | b | SE | b | SE | Lower | Upper | b | SE | b | SE | ||
| Internalizing | |||||||||||||
| Parental Distress | .35** | .11 | −.96 | 1.43 | −.34 | .54 | −1.61 | .57 | 4.53** | 1.62 | 7.11** | 1.64 | .22 |
| PSDI | .50** | .11 | 5.85** | 1.39 | 2.92a | 1.01 | 1.35 | 5.38 | |||||
| Externalizing | |||||||||||||
| Parental Distress | .35** | .11 | −.71 | 1.31 | −.25 | .48 | −1.25 | .71 | 8.97** | 1.48 | 10.68** | 1.45 | .27 |
| PSDI | .50** | .11 | 3.94** | 1.27 | 1.96a | 75 | .80 | 3.80 | |||||
| Self-reported BDI | |||||||||||||
| PSDI | .52** | .11 | 2.69* | 1.05 | 1.39a | .58 | .46 | 2.77 | 1.12 | 1.65 | 2.51 | 1.58 | .03 |
Notes: The independent variable (IV) is ADHD Status
Significant point estimate (p < 0.05).
p < .05,
p < .01.
Table 4.
Summary of mediation results with age, maternal education, and family income as covariates
| Dependent variable (DV) and Mediators (M) |
Effects of IV on M (a) |
Effects of M on DV (b) |
Indirect effects (a x b) |
Bootstrap 95% CI for Indirect Effects |
Direct effects (c’) |
Total effects (c) |
Adj. R2 for Model |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | b | SE | b | SE | Lower | Upper | b | SE | b | SE | ||
| NSSI (frequency) | |||||||||||||
| Parental Distress | .37** | .11 | .83 | .51 | .31 | .25 | −.05 | .97 | 1.66** | .58 | 2.07** | .55 | .08 |
| PSDI | .48** | .11 | .22 | .50 | .10 | .27 | −.39 | .70 | |||||
| NSSI (severity) | |||||||||||||
| Parental Distress | .37** | .11 | .11 | .13 | .01 | .06 | −.06 | .18 | 48** | .15 | .64** | .15 | .13 |
| PSDI | .47** | .11 | .25* | .13 | .12a | .07 | .01 | .30 | |||||
Notes: The independent variable (IV) is ADHD Status
Significant point estimate (p < 0.05).
p < .05,
p < .01.
Table 5.
Summary of mediation results with age, maternal education, family income, and adolescent variables as covariates
| Dependent variable (DV) and Mediators (M) |
Effects of IV on M (a) |
Effects of M on DV (b) |
Indirect effects (a x b) |
Bootstrap 95% CI for Indirect Effects |
Direct effects (c’) |
Total effects (c) |
Adj. R2 for Model |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | b | SE | b | SE | Lower | Upper | b | SE | b | SE | ||
| Internalizingb | |||||||||||||
| Parental Distress | .09 | .11 | −1.67 | 1.43 | −.15 | .26 | −1.09 | .14 | 2.88 | 1.69 | 3.86* | 1.73 | .25 |
| PSDI | .11* | .11 | 5.05** | 1.40 | 1.13a | 1.13 | .13 | 2.84 | |||||
| Externalizingc | |||||||||||||
| Parental Distress | −.07 | .12 | −1.46 | 1.23 | .10 | .11 | −.16 | .95 | 4.63** | 1.62 | 4.68** | 1.62 | .38 |
| PSDI | −.03 | .12 | 1.76 | 1.26 | −.05 | .26 | −.85 | .31 | |||||
| Self-reported BDId | |||||||||||||
| PSDI | .46** | .11 | 2.16* | 1.03 | 1.00a | .52 | .18 | 2.23 | .18 | 1.61 | 1.18 | 1.56 | .07 |
Notes: The independent variable (IV) is ADHD Status
Significant point estimate (p < 0.05)
Wave 2 Internalizing added as covariate,
Wave 2 Externalizing added as covariate,
Wave 2 BDI scores added as covariate
p < .05,
p < .01
Table 6.
Summary of mediation results with age, maternal education, family income, and adolescent variables as covariates (continued)
| Dependent variable (DV) and Mediators (M) |
Effects of IV on M (a) |
Effects of M on DV (b) |
Indirect effects (a x b) |
Bootstrap 95% CI for Indirect Effects |
Direct effects (c’) |
Total effects (c) |
Adj. R2 for Model |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| b | SE | b | SE | b | SE | Lower | Upper | b | SE | b | SE | ||
| NSSI (frequency)b | |||||||||||||
| Parental Distress | −.07 | .12 | .76 | .52 | −.05 | .11 | −.42 | .09 | 1.47* | .68 | 1.41* | .68 | .07 |
| PSDI | −.07 | .12 | .13 | .53 | −.01 | .08 | −.23 | .10 | |||||
| NSSI (severity)c | |||||||||||||
| Parental Distress | .08 | .11 | .11 | .14 | .01 | .02 | −.01 | .09 | .47** | .16 | .52** | .16 | .13 |
| PSDI | .17 | .12 | .25 | .13 | .04 | .04 | −.01 | .17 | |||||
Notes: The independent variable (IV) is ADHD Status
Significant point estimate (p < 0.05),
Wave 2 Externalizing added as covariate,
Wave 2 Externalizing added as covariate
p < .05
p < .01
ADHD-Internalizing linkage
When controlling for age, maternal education, and family income, there was a significant and positive relation between Wave 1 ADHD status and Wave 3 internalizing symptoms, b = 7.11, standard error [SE] = 1.64, t(182) = 4.34, p <.001 (i.e., c path). PSDI was a significant partial mediator of this relation, indirect effect [IE] = 2.92, SE = 1.01, CI95 = 1.35–5.38. Parental distress was not a significant partial mediator, IE = −.34, SE = .54, CI95 = −1.61–.57.
The relation between Wave 1 ADHD status and Wave 3 internalizing symptoms remained significant when covarying Wave 2 internalizing symptoms, b = 3.86 , SE = 1.73, t(182) = 2.23, p <.05. In these analyses, PSDI also served a significant full mediator, IE = 1.13, SE = 1.13, CI95 = .13–2.84, but parental distress was not a significant mediator, IE = −.15, SE = .26, CI95 = −1.09–.14.
ADHD-Depression linkage
When controlling for age, maternal education, and family income, the relation between Wave 1 ADHD status and Wave 3 depressive symptoms was not significant: b = 2.51 , SE = 1.58, t(180) = 1.58, p >.05. However, despite insignificant total effects for the relation between ADHD and depressive symptoms, a significant indirect effect was found for PSDI, IE = 1.39, SE = .58, CI95 = .46–2.77.2
Parallel results were found when Wave 2 depressive symptoms were added as a covariate. The relation between Wave 1 ADHD status and Wave 3 depressive symptoms remained non-significant: b = 1.18, SE = 1.56, t(179) = .76, p >.05. Significant indirect effects were found for PSDI, IE = 1.00, SE = .52, CI95 = .18–2.23.
ADHD-Externalizing linkage
When controlling for age, maternal education, and family income, there was a significant and positive relation between Wave 1 ADHD status and Wave 3 externalizing symptoms, b = 10.18 , SE = 1.45, t(182) = 7.35, p <.001. Parental distress was not a significant mediator, IE = −.25, SE = .48, CI95 = −1.25–.71. However, PSDI was a significant partial mediator, IE = 1.96, SE = .75, CI95 = .80–3.80.
The relation between Wave 1 ADHD status and Wave 3 externalizing symptoms remained when covarying Wave 2 externalizing symptoms, b = 4.68, SE = 1.62, t(181) = 2.90, p <.01. However, neither parental distress, IE = .10, SE = .11, CI95 = −.16–.95, nor PSDI, IE = −.05, SE = .26, CI95 = −.85–.31 remained as significant mediators with such stringent control.
ADHD-NSSI frequency linkage
When controlling for age, maternal education, and family income, the relation between Wave 1 ADHD status and Wave 3 NSSI frequency was significant: b = 2.07, SE = .55, t(168) = 3.74, p <.001. Neither parental distress served, IE = .31, SE = .25, CI95 = −.05–97; nor PSDI, IE = .10 SE = .27, CI95 = −.39–.70 served as significant mediators.
The relation between ADHD status and NSSI frequency was retained when Wave 2 externalizing symptoms was added as a covariate, b = 1.41, SE = .68, t (167) = 2.08, p <.05. However, neither parental distress, IE = −.05, SE = .11, CI95 = −.42–.09, nor PSDI, IE = −.01, SE = .08, CI95 = −.23–.10, was a significant mediator with such stringent control.
ADHD-NSSI severity linkage
When controlling for age, maternal education, and family income, the relation between Wave 1 ADHD status and Wave 3 NSSI severity was significant: b = .64 , SE = .15, t(169) = 4.36 p <.001. Parental distress did not serve as a mediator, IE = .01, SE = .06, CI95 = −.06–.18. However, PSDI, IE = .12, SE = .07, CI95 = .01–.30, did serve as a partial mediator.
When Wave 2 externalizing was added as a covariate, the relation between ADHD status and Wave 3 NSSI severity remained significant, b = .52, SE = .16, t(168) = 3.21, p >.05. Neither parental distress, IE = .01, SE = .02, CI95 = −.01–.09, nor PSDI, IE = .04, SE = .04, CI95 = −.01–.17, remained as significant mediators here.
Discussion
As predicted, the mothers of young women diagnosed with childhood ADHD reported experiencing more parental distress and PSDI during their daughter’s adolescence than did comparison mothers. Furthermore, and crucially, PSDI served as a mediator between childhood ADHD status and several criterion measures (i.e., externalizing and internalizing outcomes as well as NSSI severity), even though parental distress did not. PSDI continued to serve as a mediator between ADHD and internalizing symptoms and had an indirect effect in the relation between ADHD and depressive symptoms, even with stringent means of statistical control (i.e., including an adolescent version of the criterion variables as a covariate). The strong suggestion is that PSDI plays a role (independent of parental distress) in the pathway from childhood ADHD toward young-adult internalizing and depressive symptoms.
Our findings are consistent with previous research reporting that children diagnosed with ADHD—particularly girls—are more prone to adverse adult outcomes than their peers (e.g. Barkley et al., 2006; Biederman et al., 2006, Biederman et al., 2008). As noted earlier, mothers of children with ADHD are likely to experience greater parental demands because of their child’s symptoms and difficulties with self-regulation; this increases their own vulnerability to parental stress (Granziano et al., 2011; Du Paul et al., 2001). Our results suggest that the parental stress associated with dysfunction in the parent-child relationship plays a key role in the development of adverse outcomes.
Abidin’s stress model (1992) suggests that certain child factors (in this case, the child’s ADHD status) and parent factors (in this case, the parent’s perception of her interactions with her child) contribute to the amount of stress a parent feels, which, in turn, affects her parenting ability. Maladaptive parenting practices have been shown to exacerbate the symptoms of ADHD, which can lead to adverse outcomes in children (see Johnston & Mash, 2001). Thus, the link we found between PSDI and adverse outcomes is likely to be related to the tendency for stressful interactions in the parent-child relationship to trigger less-than-optimal parenting practices (e.g., ineffective monitoring, inconsistent discipline, withdrawal of parental support).
In addition, other forms of reciprocal, transactional processes are also likely to be at play. For example, adolescent-related ADHD behavior patterns may lead youth to seek deviant peers, who also reinforce tendencies toward internalization or externalization (Marshal, Molina, & Pelham, 2003). Further research should be done to investigate the mechanisms by which other child characteristics and parental stress interact to increase the risk for adverse outcomes.
Because neither indicators of parenting stress was associated with suicide attempt count, there are doubtless other factors that may mediate the relation between early ADHD symptomatology and suicide attempts. For example, maternal depression has been associated with increased risk for depression and suicidal behaviors in children with ADHD (Chronis-Tuscano et al., 2010). Past research has also suggested that the high rate of suicidal behaviors in individuals with ADHD may be related to the presence of comorbid conditions, such as anxiety disorder, major depressive disorder, and substance abuse disorders (Balazs, Miklosi, Kereszteny, Dallos, & Gadroros, 2014). Furthermore, in Swanson et al. (2014), we found that an objective measure of response inhibition/impulsivity, as well as both externalizing and internalizing symptoms during adolescence, fell on the pathway to NSSI and suicide attempts. Thus, additional research should be done to explore other mediators in the link between ADHD and suicide attempts.
It is also important to explore why PSDI, but not parental distress, mediated the link between ADHD and internalizing and depressive symptoms. As noted earlier, parental distress focuses on the aspect of parental stress that is associated with parents’ perception of their parenting role, while PSDI focuses on parents’ perception of their parent-child interactions that may induce parental stress. Because of the dynamic nature of parent-child interactions, a child’s ADHD symptoms are likely to have more of a direct role on dysfunction and associated stress in the parent-child relationship than on a parent’s more general perception of her parenting role. Furthermore, previous research has suggested that there is an increase in the affective intensity of parent-child conflict in adolescence (Laursen, Coy, & Collins, 1998), along with an increase in the parental stress associated with such conflict (Putnick et al., 2010). Thus, PSDI may be salient during this time period and, as a result, may increase the chance that an adolescent may develop resultant internalizing and depressive symptoms—even over and above her adolescent levels of these symptoms.
Our use of an all-female sample might also account for why PSDI continues to mediate ADHD and internalizing/depressive symptoms but not externalizing symptoms when covarying adolescent behavior patterns, as increases in depressive and internalizing symptoms are normative for girls during the transition to adolescence (Nolen-Hoeksema & Girgus, 1994). Future studies should explore whether the same persistent mediational role of PSDI in the relation between ADHD and internalizing symptoms can be generalized to males with ADHD.
In addition to a lack of generalizability to males with ADHD, there are additional limitations in our investigation that should be taken into consideration when interpreting our results. First of all, we did not explore the role of other child characteristics (i.e., personality traits) in the development of their parents’ stress. Given the aforementioned bidirectional nature of parenting stress and child behaviors, a future study investigating the role of a child’s early temperament and/or personality characteristics—in addition to their ADHD symptoms—could enlighten our understanding of how parental stress develops and influences later outcomes. In addition, future research should also explore how other parent characteristics and broader family variables might affect the associations found. For example, a parent’s own ADHD status and depressive symptomology are strong predictors of their parental stress (Theule, Wiener, Rogers, & Marton, 2011; Theule, Wiener, Tannock, & Jenkins, 2013.)
We also were not able to include the girls’ own account of their experience of their parents’ stress. Such an investigation would also help us understand the mechanisms by which parental stress influences later outcomes. Furthermore, the primary reporters for parental stress in our study were mothers. Because of low participation rates and a number of single-parent families, we were not able to include the father’s report of parental stress, which might also be associated with key young-adult behavior patterns in females with ADHD.
Because the mothers’ reports were used (in addition to teacher reports) to determine the girls’ childhood diagnoses, to construct the girls’ young-adult externalizing and internalizing composites, and to assess parental stress, our investigation may be subject to shared method variance. Although we tried to mitigate this issue by including input from other sources, future investigations could be improved by including more objective measures of externalizing and internalizing symptoms.
In addition, the adjusted R2 values for the models exploring the mediating role of PSDI on depressive symptoms were low, meaning that only a small percentage of variance of this key outcome was attributable to PSDI. Furthermore, the statistical methods used in our analyses allowed us to explore only one criterion variable at a time. Because some of our criterion variables were highly correlated (e.g., girls’ internalizing symptoms and depressive symptoms), future research exploring these criteria as composites may be in order. Finally, because we did not covary baseline internalizing and externalizing symptoms, we are not able to postulate that the relations observed are specific to girls’ childhood ADHD symptoms and not their associated early internalizing/externalizing behaviors. However, our investigation is still relevant to children with ADHD, as these behavior patterns are common comorbidities (Jensen et al., 2001).
Despite these limitations, we have demonstrated the importance of dysfunctional family interactions and the stress experienced by parents of adolescent girls with ADHD in young adult development of crucial comorbidities and impairments. Interventions targeting dysfunctional parent-child interactions may help to reduce girls’ risk for internalizing, externalizing, and depressive symptoms as young adults. Such interventions would doubtless need to incorporate multimodal efforts, including enhancement of parental competence, treatments tailored to the particular challenges of adolescence for youth with ADHD, and broader provision of supports to such families.
Acknowledgments
This project was supported by National Institute of Mental Health Grant R01 MH45064 and Grant 5T32MH089919-04. We gratefully acknowledge the girls—now young women—who have participated in our ongoing investigation, along with their caregivers and our large numbers of graduate students and research assistants. Their remarkable dedication has made this research possible. We also acknowledge the great assistance of Elizabeth Owens.
Footnotes
The internal consistency for this measure is not extremely high, because this score reflects the sum of six methods endorsed. Participants tend to only endorse one method (e.g. “cutting”) and not others (e.g. “burning)”.
Some investigators argue that significant total effects are not required to test the indirect effects, suggesting quantification of the indirect the effects instead of inferring them from the significance testing of the direct and total effects (see Hayes, 2009 for a more detailed explanation).
Contributor Information
Chanelle T. Gordon, Department of Psychology, University of California, Berkeley
Stephen P. Hinshaw, Department of Psychology, University of California, Berkeley
References
- Abidin RR. The determinants of parenting behavior. Journal of Clinical Child Psychology. 1992;21(4):407–412. [Google Scholar]
- Abidin RR. Parenting Stress Index. 3rd ed. Odessa, FL: Psychological Assessment Resources; 1995. [Google Scholar]
- Abidin RR, Brunner JF. Development of a parenting alliance inventory. Journal of Clinical Child Psychology. 1995;24(1):31–40. [Google Scholar]
- Achenbach TM. Manual for the Child Behavior Checklist/4–18 and 1991 Profile. Burlington: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for the ASEBA adult forms and profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2003. [Google Scholar]
- Anderson CA, Hinshaw SP, Simmel C. Mother-child interactions in ADHD and comparison boys: Relationships with overt and covert externalizing behavior. Journal of Abnormal Child Psychology. 1994;22(2):247–265. doi: 10.1007/BF02167903. [DOI] [PubMed] [Google Scholar]
- Balazs J, Miklósi M, Keresztény Á, Dallos G, Gádoros J. Attention-deficit hyperactivity disorder and suicidality in a treatment naïve sample of children and adolescents. Journal of Affective Disorders, 152–154. 2014:282–287. doi: 10.1016/j.jad.2013.09.026. doi: http://dx.doi.org/10.1016/j.jad.2013.09.026. [DOI] [PubMed]
- Barkley RA, editor. Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment. 4th ed. New York: Guilford Press; 2015. [Google Scholar]
- Barkley RA, Murphy KR. Attention-deficit hyperactivity disorder: A clinical workbook. 3rd ed. New York: Guilford; 2006. [Google Scholar]
- Barkley RA, Karlsson J, Pollard S, Murphy JV. Developmental changes in the mother-child interactions of hyperactive boys: Effects of two dose levels of Ritalin. Child Psychology & Psychiatry & Allied Disciplines. 1985;26(5):705–715. doi: 10.1111/j.1469-7610.1985.tb00585.x. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult outcome of hyperactive children: Adaptive functioning in major life activities. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(2):192–202. doi: 10.1097/01.chi.0000189134.97436.e2. doi: http://dx.doi.org/10.1097/01.chi.0000189134.97436.e2. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Edelbrock C, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria: III. Mother-child interactions, family conflicts and maternal psychopathology. Journal of Child Psychology & Psychiatry. 1991;32(2):233–255. doi: 10.1111/j.1469-7610.1991.tb00304.x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio (TX): The Psychological Corporation; 1996. [Google Scholar]
- Bell RQ. A reinterpretation of the direction of effects in studies of socialization. Psychological Review. 1968;75:61–95. doi: 10.1037/h0025583. [DOI] [PubMed] [Google Scholar]
- Benzies KM, Harrison MJ, Magill-Evans J. Parenting stress, marital quality, and child behavior problems at age 7 years. Public Health Nursing. 2004;21(2):111–121. doi: 10.1111/j.0737-1209.2004.021204.x. doi: http://dx.doi.org/10.1111/j.0737-1209.2004.021204.x. [DOI] [PubMed] [Google Scholar]
- Biederman J, Petty CR, Fried R, Kaiser R, Dolan CR, Schoenfeld S, Faraone SV. Educational and occupational underattainment in adults with attention-deficit/hyperactivity disorder: A controlled study. Journal of Clinical Psychiatry. 2008;69(8):1217–1222. doi: 10.4088/jcp.v69n0803. doi: http://dx.doi.org/10.4088/JCP.v69n0803. [DOI] [PubMed] [Google Scholar]
- Biederman J, Monuteaux MC, Mick E, Spencer T, Wilens TE, Silva JM, Faraone SV. Young adult outcome of attention deficit hyperactivity disorder: A controlled 10-year follow-up study. Psychological Medicine. 2006;36(2):167–179. doi: 10.1017/S0033291705006410. doi: http://dx.doi.org/10.1017/S003329170500641. [DOI] [PubMed] [Google Scholar]
- Claes L, Vandereycken W. The Self-Injury Questionnaire-Treatment Related (SIQ-TR): Construction, reliability, and validity in a sample of female eating disorder patients. In: Goldfarb PM, editor. Psychological Tests and Testing Research Trends. New York: Nova Science Publishers; 2007. pp. 111–139. [Google Scholar]
- Claes L, Vandereycken W, Vertommen H. Self-injurious behaviors in eating-disordered patients. Eating Behaviors. 2001;2(3):263–272. doi: 10.1016/s1471-0153(01)00033-2. doi: http://dx.doi.org/10.1016/S1471-0153(01)00033-2. [DOI] [PubMed] [Google Scholar]
- Charach A, Yeung E, Climans T, Lillie E. Childhood attention-deficit/hyperactivity disorder and future substance use disorders: Comparative meta- analyses. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50(1):9–21. doi: 10.1016/j.jaac.2010.09.019. doi: http://dx.doi.org/10.1016/j.jaac.2010.09.019. [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Molina BSG, Pelham WE, Applegate B, Dahlke A, Overmyer M, Lahey BB. Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 2010;67(10):1044–1051. doi: 10.1001/archgenpsychiatry.2010.127. doi: http://dx.doi.org/10.1001/archgenpsychiatry.2010.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa NM, Weems CF, Pellerin K, Dalton R. Parenting stress and childhood psychopathology: An examination of specificity to internalizing and externalizing symptoms. Journal of Psychopathology and Behavioral Assessment. 2006;28(2):113–122. doi: http://dx.doi.org/10.1007/s10862-006-7489-3. [Google Scholar]
- Deater-Deckard K. Parenting stress and child adjustment: Some old hypotheses and new questions. Clinical Psychology: Science and Practice. 1998;5(3):314–332. [Google Scholar]
- DuPaul GJ, McGoey KE, Eckert TL, VanBrakle J. Preschool children with attention-deficit/hyperactivity disorder: Impairments in behavioral, social, and school functioning. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(5):508–515. doi: 10.1097/00004583-200105000-00009. doi: http://dx.doi.org/10.1097/00004583-200105000-00009. [DOI] [PubMed] [Google Scholar]
- Eccles JS. The development of children ages 6 to 14. The Future of Children. 1999;9(2):30–44. doi: http://dx.doi.org/10.2307/1602703. [PubMed] [Google Scholar]
- Graziano PA, McNamara JP, Geffken GR, Reid A. Severity of children’s ADHD symptoms and parenting stress: A multiple mediation model of self-regulation. Journal of Abnormal Child Psychology. 2011;39(7):1073–1083. doi: 10.1007/s10802-011-9528-0. doi: http://dx.doi.org/10.1007/s10802-011-9528-0. [DOI] [PubMed] [Google Scholar]
- Harold GT, Leve LD, Barrett D, Elam K, Neiderhiser JM, Natsuaki MN, Thapar A. Biological and rearing mother influences on child ADHD symptoms: Revisiting the developmental interface between nature and nurture. Journal of Child Psychology and Psychiatry. 2013;54(10):1038–1046. doi: 10.1111/jcpp.12100. doi: http://dx.doi.org/10.1111/jcpp.12100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haskett ME, Ahern LS, Ward CS, Allaire JC. Factor structure and validity of the parenting stress index-short form. Journal of Clinical Child and Adolescent Psychology. 2006;35(2):302–312. doi: 10.1207/s15374424jccp3502_14. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76(4):408–420. doi: http://dx.doi.org/10.1080/03637750903310360. [Google Scholar]
- Heller TL, Baker BL, Henker B, Hinshaw SP. Externalizing behavior and cognitive functioning from preschool to first grade: Stability and predictors. Journal of Clinical Child Psychology. 1996;25(4):376–387. [Google Scholar]
- Hinshaw SP. Preadolescent girls with attention-deficit/hyperactivity disorder: I. background characteristics, comorbidity, cognitive and social functioning, and parenting practices. Journal of Consulting and Clinical Psychology. 2002;70(5):1086–1098. doi: 10.1037//0022-006x.70.5.1086. doi: http://dx.doi.org/10.1037/0022-006X.70.5.1086. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Owens EB, Sami N, Fargeon S. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into adolescence: Evidence for continuing cross-domain impairment. Journal of Consulting and Clinical Psychology. 2006;74(3):489–499. doi: 10.1037/0022-006X.74.3.489. doi: http://dx.doi.org/10.1037/0022-006X.74.3.489. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Owens EB, Zalecki C, Huggins SP, Montenegro-Nevado A, Schrodek E, Swanson EN. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into early adulthood: Continuing impairment includes elevated risk for suicide attempts and self-injury. Journal of Consulting and Clinical Psychology. 2012;80(6):1041–1051. doi: 10.1037/a0029451. doi: http://dx.doi.org/10.1037/a0029451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinshaw SP, Scheffler RM. The ADHD explosion: Myths, medication, money, and today’s push for performance. New York: Oxford University Press; 2014. [Google Scholar]
- Jensen PS, Hinshaw SP, Kraemer HC, Lenora N, Newcorn JH, Abikoff HB, Vitiello B. ADHD comorbidity findings from the MTA study: Comparing comorbid subgroups. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(2):147–158. doi: 10.1097/00004583-200102000-00009. [DOI] [PubMed] [Google Scholar]
- Johnston C, Mash EJ. Families of children with attention-deficit/ hyperactivity disorder: Review and recommendations for future research. Clinical Child and Family Psychology Review. 2001;4(3):183–207. doi: 10.1023/a:1017592030434. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children’s Depression Inventory (CDI) manual. Toronto, Ontario, Canada: Multi-Health Systems; 1992. [Google Scholar]
- Laursen B, Coy KC, Collins WA. Reconsidering changes in parent-child conflict across adolescence: A meta-analysis. Child Development. 1998;69(3):817–832. [PMC free article] [PubMed] [Google Scholar]
- Marshal MP, Molina BSG, Pelham WE., Jr Childhood ADHD and adolescent substance use: An examination of deviant peer group affiliation as a risk factor. Psychology of Addictive Behaviors. 2003;17(4):293–302. doi: 10.1037/0893-164X.17.4.293. doi: http://dx.doi.org/10.1037/0893-164X.17.4.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meinzer MC, Lewinsohn PM, Pettit JW, Seeley JR, Gau JM, Chronis–Tuscano A, Waxmonsky JG. Attention-deficit/hyperactivity disorder in adolescence predicts onset of major depressive disorder through early adulthood. Depression and Anxiety. 2013;30(6):546–553. doi: 10.1002/da.22082. doi: http://dx.doi.org/10.1002/da.22082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modesto-Lowe V, Danforth JS, Brooks D. ADHD: Does parenting style matter? Clinical Pediatrics. 2008;47(9):865–872. doi: 10.1177/0009922808319963. doi: http://dx.doi.org/10.1177/0009922808319963. [DOI] [PubMed] [Google Scholar]
- Morgan J, Robinson D, Aldridge J. Parenting stress and externalizing child behaviour. Child & Family Social Work. 2002;7(3):219–225. doi: http://dx.doi.org/10.1046/j.1365-2206.2002.00242.x. [Google Scholar]
- Nolen-Hoeksema S, Girgus JS. The emergence of gender differences in depression during adolescence. Psychological Bulletin. 1994;115(3):424–443. doi: 10.1037/0033-2909.115.3.424. [DOI] [PubMed] [Google Scholar]
- Patterson GR. The early development of coercive family process. In: Reid JB, Patterson GR, Snyder JJ, editors. Antisocial behavior in children and adolescents: a developmental analysis and the Oregon model for intervention. Washington, DC: American Psychological Association; 2002. pp. 25–44. [Google Scholar]
- Pelham WE, Lang AR, Atkeson B, Murphy DA, Gnagy EM, Greiner AR, Greenslade KE. Effects of deviant child behavior on parental distress and alcohol consumption in laboratory interactions. Journal of Abnormal Child Psychology. 1997;25(5):413–424. doi: 10.1023/a:1025789108958. [DOI] [PubMed] [Google Scholar]
- Pettit GS, Arsiwalla DD. Commentary on special section on “bidirectional parent-child relationships”: The continuing evolution of dynamic, transactional models of parenting and youth behavior problems. Journal of Abnormal Child Psychology. 2008;36(5):711–718. doi: 10.1007/s10802-008-9242-8. doi: http://dx.doi.org/10.1007/s10802-008-9242-8. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. doi: http://dx.doi.org/10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- Putnick DL, Bornstein MH, Hendricks C, Painter KM, Suwalsky JTD, Collins WA. Stability, continuity, and similarity of parenting stress in European American mothers and fathers across their child’s transition to adolescence. Parenting: Science and Practice. 2010;10(1):60–77. doi: 10.1080/15295190903014638. doi: http://dx.doi.org/10.1080/15295190903014638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skegg K. Self-harm. The Lancet. 2005;366:1471–1483. doi: 10.1016/S0140-6736(05)67600-3. [DOI] [PubMed] [Google Scholar]
- Swanson EN, Owens EB, Hinshaw SP. Pathways to self–harmful behaviors in young women with and without ADHD: A longitudinal examination of mediating factors. Journal of Child Psychology and Psychiatry. 2014;55(5):505–515. doi: 10.1111/jcpp.12193. doi: http://dx.doi.org/10.1111/jcpp.12193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Theule J, Wiener J, Rogers MA, Marton I. Predicting parenting stress in families of children with ADHD: Parent and contextual factors. Journal of Child and Family Studies. 2011;20(5):640–647. doi: http://dx.doi.org/10.1007/s10826-010-9439-7. [Google Scholar]
- Theule J, Wiener J, Tannock R, Jenkins JM. Parenting stress in families of children with ADHD: A meta-analysis. Journal of Emotional and Behavioral Disorders. 2013;21(1):3–17. doi: http://dx.doi.org/10.1177/1063426610387433. [Google Scholar]
- Vanderlinden J, Vandereycken W. Trauma, dissociation, and impulse dyscontrol in eating disorders. Brunner/Mazel: Philadelphia, PA; 1997. [Google Scholar]
- Woodward L, Taylor E, Dowdney L. The parenting and family functioning of children with hyperactivity. Journal of Child Psychology and Psychiatry. 1998;39(2):161–169. [PubMed] [Google Scholar]