Abstract
Background
Cancer represents a substantial hardship for patients and their families in multiple domains beyond health and survival. Relatively little is known about the economic impact of cancer. We present estimates of the aggregate effects of a cancer diagnosis on employment and income in a prospective, nationally representative sample of US adults.
Methods
We used data from the 1990–2009 waves of the Panel Study of Income Dynamics (PSID), a nationally-representative, prospective population-based observational study with high-quality individual and family level economic information. We estimated age-adjusted gender-stratified individual fixed-effects regression models to derive estimates of the impact of cancer on employment, hours worked, individual income, and total family income.
Results
We found significant effects of cancer on all four outcomes. The probability of a cancer patient being employed dropped by almost 10% and hours worked declined by up to 200 hours in the first year after diagnosis. Annual labor market earnings dropped almost 40 percent within two years after diagnosis and remained low while total family income declined by 20 percent although it recovered within 4 years after the diagnosis. These economic impacts were driven by effects among male survivors; the effects among women were largely not statistically significant.
Conclusions
A cancer diagnosis has substantial effects on the economic well-being of affected adults and their families. With the increasing number of cancer survivors in the US population, there is a growing need for examining the long-term implications for economic well-being and ways to mitigate the economic hardship associated with cancer.
Keywords: Economic wellbeing, Cancer, Survivors, Prospective Study, US adults, Fixed-effects approach
Cancer remains one of the most prominent public health concerns in the US and around the world. A recent study estimated the annual loss of productivity due to cancer between $9.6 and $16 billion among working-age adults in the US.1 The number of adult cancer survivors in the US population exceeds 13 million.2 Cancer survivors report difficulties in multiple domains, from health-related quality of life3 to psychological problems such as depression and anxiety.4, 5 In contrast, relatively little is known about the impact of a cancer diagnosis on economic outcomes at the individual and family levels.6
One way for a cancer diagnosis to impact economic circumstances is through reduced or discontinued employment. In a review of 64 studies of employment among cancer survivors, 63% of survivors continued working or returned to work after treatment. However, the estimates ranged from 24% to 94% depending on the sample demographics, cancer type and stage, time since diagnosis, and other factors.7 In some studies, the decline in employment or work hours was negligible8–10 although most described detrimental effects on employment.11, 12 The relatively few number of studies that have examined the effects on income tend to find that the cancer has a negative impact. For instance, convenience samples of cancer survivors from New Zealand,13 Ireland,14 and Canada15 found a 30–37% decline in income two years after diagnosis. Among low-income Hispanic women with breast cancer in the U.S., about half reported “income concerns” and “financial stress.”16
While studies have described the negative associations between cancer and economic circumstances, they have two important limitations. First, they typically used small convenience samples found through cancer registries or from oncology clinics or they focused on a specific group of patients such as terminal patients or long-term survivors. Convenience samples may suffer from selection bias and thus not generalize to the overall population of cancer survivors. A second limitation is the lack of objective measures of economic well-being. Most studies were based on retrospective reports of subjective measures such as financial stress or hardship,17, 18 however, the retrospective economic information is subject to substantial recall bias.
The current study is based on the Panel Study of Income Dynamics (PSID), the leading national longitudinal survey of economic circumstances of American families.19 The PSID is unique in the high quality of its economic data and generalizability to the US population. The data include detailed prospective employment and income data collected on an annual or bi-annual basis before and after a cancer diagnosis, allowing us to identify economic changes attributable to the cancer diagnosis. To our knowledge, this is the first study to use a quasi-random design to estimate the impact of a cancer diagnosis on key dimensions of economic wellbeing among US adults.
DATA AND METHODS
Data
The PSID is an ongoing longitudinal survey of a nationally representative sample of American families conducted continuously since 1968 (annually until 1997 and every other year since 1999).20 The primary aim has been to study economic behavior of US families. The survey has collected detailed information about employment, earnings, income, and other economic and socio-demographic characteristics, using mostly telephone interviews lasting about 80 minutes each. Reports of the survey design21 and data quality have been published elsewhere.22–25 The PSID data and documentation are available at http://psidonline.isr.umich.edu/.
Sample
The analytic sample included respondents who participated in at least one interview between 1999 and 2009, the years when cancer information was collected. Out of 17,262 individuals in that group, 1,406 reported they had previously been diagnosed with cancer. We excluded 70 respondents who did not report the year of diagnosis and 35 who had childhood cancers (occurring prior to age 18). We excluded an additional 184 respondents whose cancer occurred prior to 1990 because of potential differences over time with regard to cancer screening, types and costs of treatment, access to health insurance, and labor market conditions. The final sample thus included 1,117 persons diagnosed with cancer and 15,856 respondents who never had cancer.
The study uses publicly available de-identified data; as such it classifies as IRB-exempt.
Variables
Cancer diagnosis
In each wave from 1999 to 2009, respondents were asked a retrospective question: “Has a doctor ever told you that you have or had cancer or a malignant tumor?” A positive answer elicited a follow-up question about the age or year their diagnosis occurred. For respondents who provided cancer reports during multiple interviews, we used the first available report as the one that occurred closest in time to the diagnosis.
Economic outcomes
Economic information was collected prospectively at each wave between 1990 and 2009. Employment status was ascertained by asking whether a respondent is “working now, looking for work, retired, keeping house, a student, or what?” Employment status was dichotomized as employed versus not employed. Hours worked measured the total number of hours a respondent had worked in all jobs, including overtime, during the previous calendar year (1989–2008). Earnings included the respondent’s labor market earnings during the previous calendar year. Finally, total family income comprised the incomes of all family members living in the household, including the respondent. About 0.2% of family incomes were negative and recoded to zero. Earnings and total family income were adjusted for inflation to 2000 dollars and natural-logged due to their skewed distribution.
All models also included age (as continuous and centered at 50) and calendar year (as dummies for each calendar year from 1990 to 2009 for employment status and 1989–2008 for the other three outcomes). Earnings and income models for adults 18 and older also include age squared to capture the typical quadratic profiles of earnings.26
Analysis
The primary challenge to estimating the economic effects of a cancer diagnosis from observational data is that those who get cancer may be systematically different from those who don’t, confounding the relationship between the cancer and outcomes. To overcome this challenge, we use individual fixed-effects regression models with dummy variables capturing time before, at, and after diagnosis that isolate the within-individual changes in outcomes as a function of the diagnosis.27, 28 The fixed effect captures the permanent differences among respondents in observed and unobserved characteristics. We estimated the model:
| (1) |
The yit is the outcome for individual i at time period t, where t captures calendar years from 1990 to 2009 for employment and 1989 to 2008 for hours worked, earnings, and total family income. The αi is the within-individual intercept, Xit. is a vector of time-varying variables comprising age and age squared where appropriate, and are the indicators of the years before/since diagnosis where p = 0 is the year of diagnosis. We restricted the indicators to 5 years around the diagnosis year, −5 ≤ p ≤5. Using this approach, we capture the change in outcomes as a function of the change in the predictor dummies . Employment, a dichotomous outcome, was modeled using linear probability FE models regressions. Hours worked and log-transformed earnings and income outcomes were modeled using linear FE models. We interpolated data points for calendar years 1998, 2000, …, 2008 when no interviews were conducted by imputing the mean of prior and successive year. Results are summarized in line plots that show the year-specific effects δp on each outcome and their 95% confidence intervals. The models include respondents who never had cancer, which improves the precision of estimates without contributing to the point estimates of the cancer diagnosis δp since all their time dummies .27 Respondents missing information for any reason (question nonresponse or survey nonresponse) from one or more waves are retained in the analysis; they simply do not contribute to the estimates for those waves.
We estimated separate models for adults in prime working ages 25–64 and all adults aged 18 and above; we also stratified models by gender because men and women have distinct labor market experiences and thus cancer may affect them differently. All analyses were conducted using Stata 13.0.29
We conducted extensive sensitivity analyses for different model specifications. These included models with and without controlling for the calendar year, the squared age term, without log-transforming earnings and income, as well as with and without interpolating outcomes for the even years 1998 to 2008 when PSID did not conduct interviews. We also examined different specifications of the time before/after diagnosis dummies, including different range of years before and after diagnosis and specifying the time dummies time intervals longer than one year, changing both their length and their thresholds. We estimated models where zero earnings and income reports were considered as missing. The specific results differed across these specifications but the pattern of coefficients remained substantively similar to those shown here, with significant effects of diagnosis on the observed economic outcomes.
RESULTS
The descriptive characteristics of the sample are shown in Table 1. For adults who had cancer, there is a decline in employment and earnings from 2 years before to 2 years after the diagnosis. The group without cancer had higher employment and income levels overall.
Table 1.
Characteristics of the analytic sample (Panel Study of Income Dynamics, 1989–2009).
| All adults who reported cancer |
All adults who reported no cancer |
||
|---|---|---|---|
| Year of diagnosis1 | 2001.0 (5.2) | ||
| Age at diagnosis | 52.5 (17.3) | ||
| Demographics in 2001 | |||
| Age | 52.4 (17.2) | 37.1 (15.9) | |
| Female (%) | 58.6% | 52.5% | |
| Economic circumstances | 2 years before diagnosis3 | 2 years after diagnosis3 | In 2001 |
| Employed (%) | 56.2% | 50.8% | 72.4% |
| Hours worked | 1,172.4 (1,067.5) | 1,038.6 (1,062.2) | 1,609 (934) |
| Own earnings (median)2 | $9,552 | $5,090 | $21,980 |
| Own earnings (mean) | $20,127 (29,579) | $19,137 (28,150) | $28,066 (41,927) |
| Total family income (median)2 | $31,800 | $27,470 | $40,560 |
| Total family income (mean) | $46,530 (55,717) | $47,408 (91,098) | $54,144 (70,434) |
| N | 1,117 | 15,856 | |
Mean and standard error in parentheses are shown unless indicated otherwise.
Earnings and total family income are highly skewed; we therefore report the median values in addition to the mean (s.d.).
Since the year of diagnosis varies across individuals, the calendar year of the 2 years before and after diagnosis time accordingly across individuals.
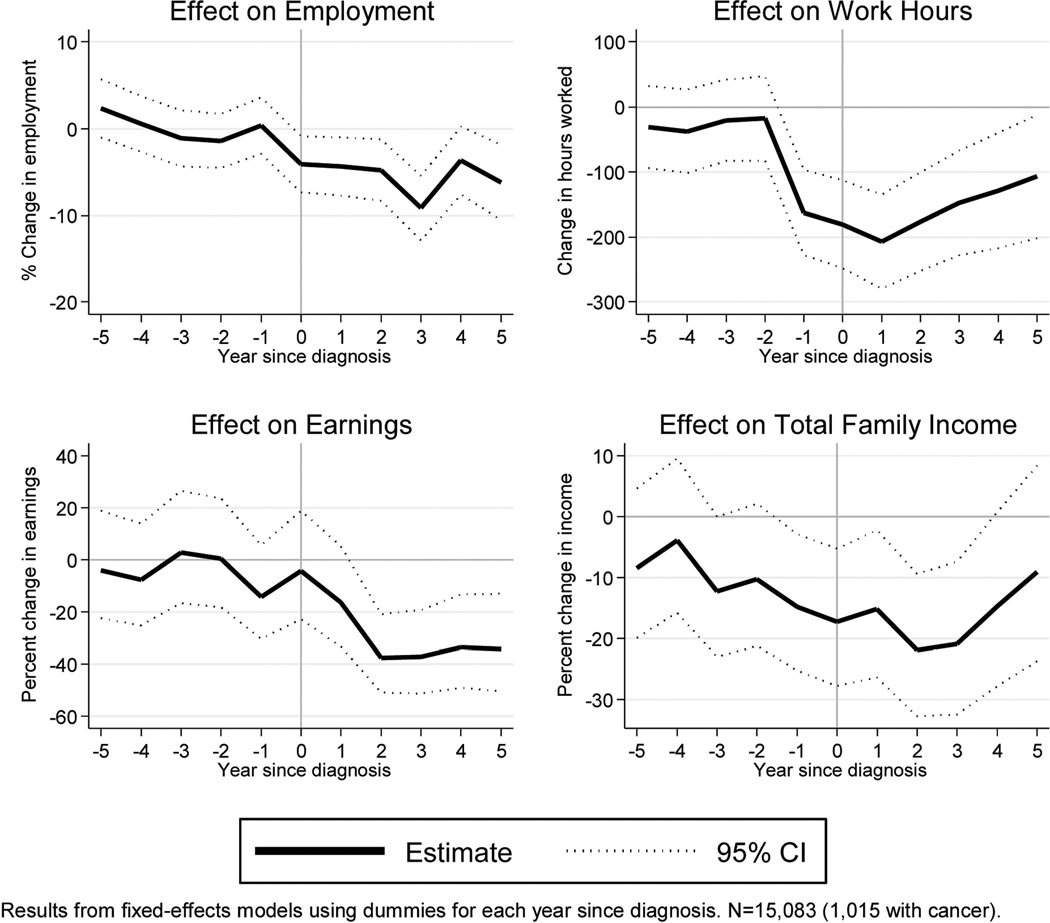
Figures 1 to 3 show the changes in economic outcomes following a cancer diagnosis based on estimates from model (1). Figure 1 displays aggregate estimates for adults age 25–64. Prior to the diagnosis, the effect of the time dummies was largely not significant (with the exception of a negative effect in year 1 before diagnosis for work hours and total family income) – that is, employment status, hours worked, labor market earnings, and total family income were only slightly negatively affected by the impending diagnosis. For all outcomes, there was a significant negative effect of most year dummies in the year of diagnosis and later. The probability of being employed decreased by up to 9 percentage points by year 3 after diagnosis, with evidence of recovery for survivors in years 4 and 5. Annual work hours decreased by up to 200 hours, or 5 weeks of lost work time, in the first year after diagnosis and then appeared to recover. Survivors’ labor market earnings dropped by up to 40 percent by the second year and remained low through years 4–5. Total family income was reduced by over 20 percent in years 2 and 3 years following the diagnosis but recovered in years 4 and 5 (the effect of dime dummies was not significant).
Figure 1.
Effect of Cancer Diagnosis on Economic Outcomes, Ages 25–64.
Figure 3.
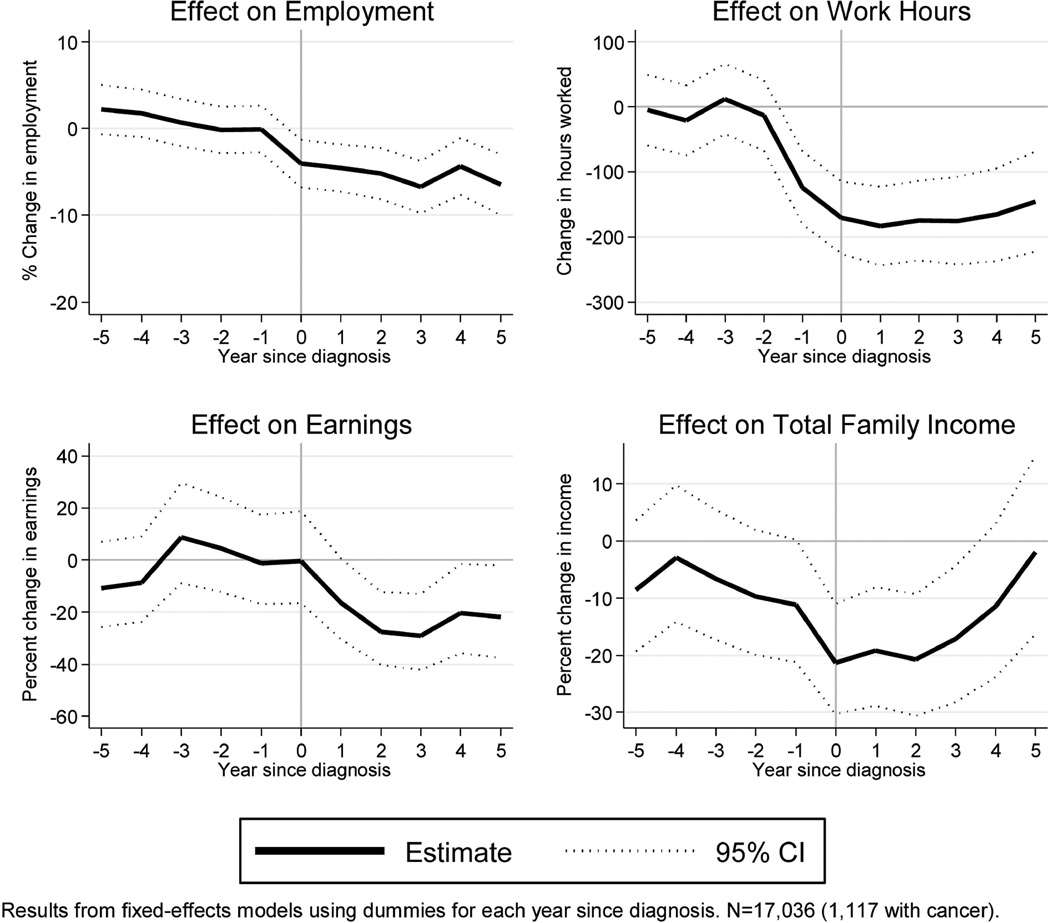
Effect of Cancer Diagnosis on Economic Outcomes, Adults Age 18 and Above.
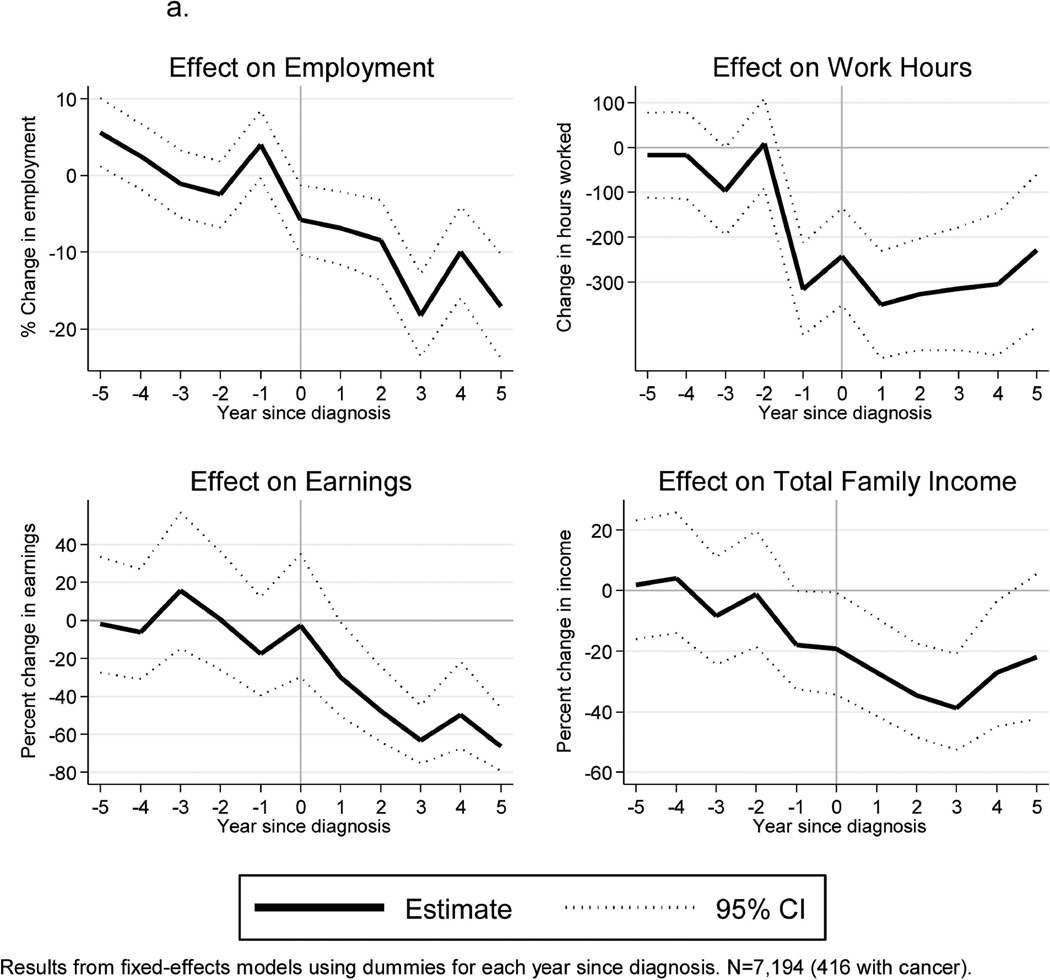
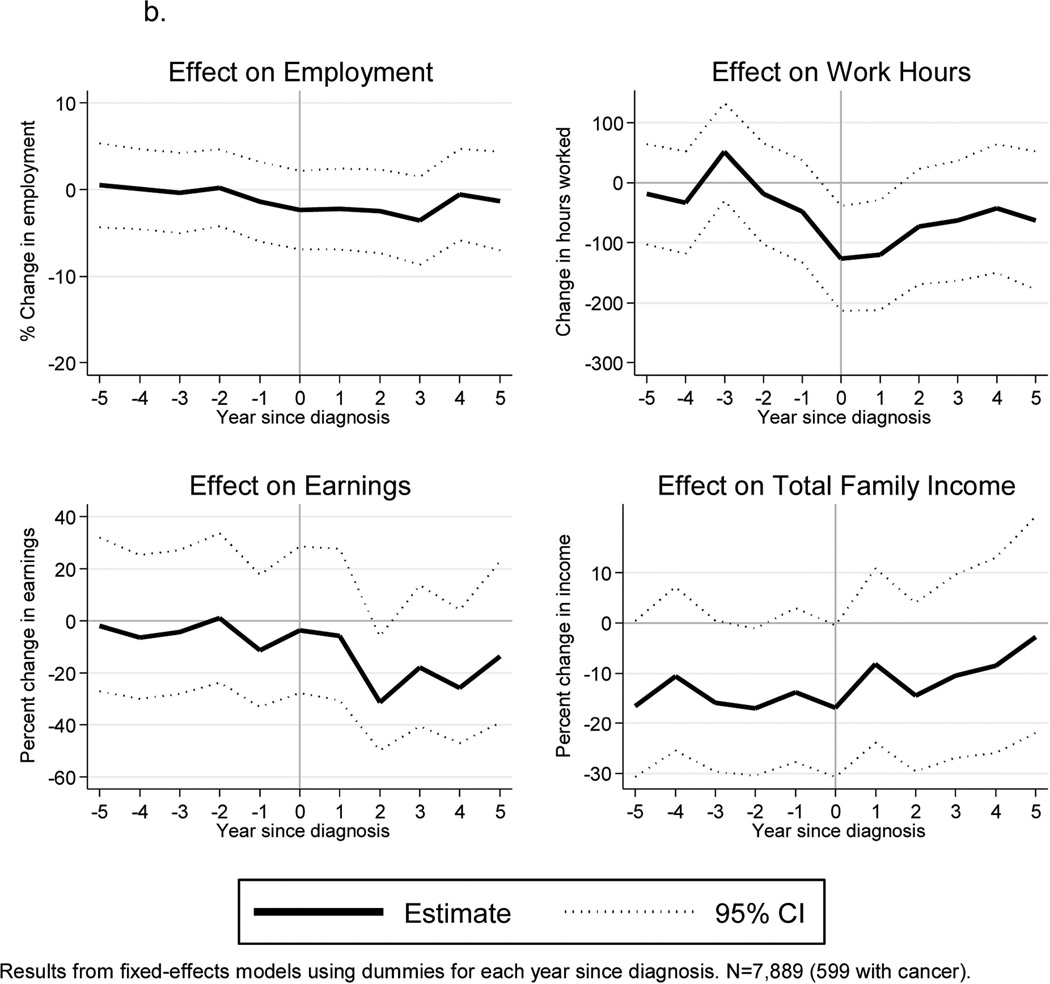
Figures 2a and 2b stratify the results by gender. These estimates are less precise due to the reduced sample sizes so we interpret the findings with caution. However, the results suggest that the economic losses were greater for male than female survivors. Among male cancer survivors age 25–64, the probability of being employed was reduced by nearly 20 percentage points and their annual hours were reduced by over 300 hours (or about 7–8 weeks of full-time employment). Correspondingly, their labor market earnings and total family income dropped significantly; earnings declined by 60% in years 3–5 and total family income declined by over 40 percent although it recovered somewhat by year 5 after diagnosis. In contrast, the losses were much smaller for female survivors (Figure 2b), with most time period effects not reaching statistical significance.
Figure 2.
a. Effect of Cancer Diagnosis on Economic Outcomes, Men 25–64.
b. Effect of Cancer Diagnosis on Economic Outcomes, Women 25–64.
Finally, Figure 3 shows the outcomes for the whole adult sample, ages 18 and above. The time profile of the diagnosis effect was generally similar to that of working-age adults but the magnitude of the time dummy effects was somewhat smaller than for working-age adults 25–64. Additional findings for the entire age range (not shown but available on request) revealed patterns by gender similar to those 25–64: the losses were more pronounced among men than among women.
DISCUSSION
Within a decade, the number of cancer survivors in the U.S. will reach 18 million.2 As cancer increasingly changes from a terminal illness to a chronic disease, it becomes increasingly important to understand how its diagnosis and treatment affect the economic well-being of cancer patients and their families.
We found significant effects of a cancer diagnosis on all examined economic outcomes. Among adults in prime working ages 25–64, the probability of being employed fell by almost 10 percentage points in the 5 years after diagnosis. Hours worked per year dropped around the diagnosis year, with average working-age cancer survivors losing about 200 hours, or about 5 weeks of full-time work. Correspondingly, annual labor market earnings dropped nearly 40 percent within two years after diagnosis. The survivor’s spouse or other adults in the household may have compensated for this loss: the total family income dropped about 20 percent in years 2 and 3 after diagnosis, but recovered by year 5. The recovery may be the result of the cancer survivor’s or their spouses’ increased labor-market participation, disability benefits d or possibly other relatives such as adult children moving into the household and contributing their income to the family total.
Interestingly, the economic losses were only modestly smaller in the total sample, which included adults 18 and older, than for adults 25–64. Given the lower labor-market participation of older respondents (as well as those 18–24), we expected that the cancer losses would be muted in this group; on the other hand adults still working in their late 60s and 70s may be more likely to exit the labor force following the diagnosis compared to younger workers, which could accentuate the effects in this age group, balancing the weaker affects among the retired.
The observed effects were primarily driven by losses among male survivors. For women who were diagnosed with cancer, the losses were largely not statistically significant. This gender difference may be a result of the lower overall labor-market participation of women, which would attenuate the average effects of cancer. It is also possible that the economic impacts may be greater for men if they suffer from types of cancer or treatments that have greater effects on their ability to work, or if their jobs are more physically demanding and less compatible with the rigors of treatment. Future studies should continue to give attention to gender differences in the economic impact of cancer.
These results generally corroborate previous studies that reported lower labor-market participation among cancer survivors,5, 7, 12 as well as significant income losses that are partially compensated by other family members.13–15, 30 There may be several reasons for income losses in families with a cancer patient, including changing attitudes toward work by the patient, increased caregiver burden for other family members, ongoing cancer treatments including long-term adjuvant chemotherapy, or residual physical problems from successful treatments such as radiation damage. Alternatively, a survivor may choose a less demanding job or go back to school as a result of a diagnosis because of necessary work modifications due to cancer, its treatment, or a change in motivation after diagnosis.
An important characteristic of these economic changes is the decline prior to the year of diagnosis. This pattern could reflect prodromal symptoms that led individuals to work less prior to diagnoses. Alternatively, it could reflect imprecise reporting of the year of cancer diagnosis. A previous study of cancer reporting among PSID respondents showed a substantial amount of reporting error that might attenuate the associations between cancer and economic loss, suggesting that our findings may be underestimates of the true effects.31 Even over-reporting (i.e., reporting non-malignant lesions as cancer) could contribute to underestimates of ‘true’ cancer diagnoses because in such cases the effect of the diagnosis would be relatively minimal. The reporting issues could be addressed in future studies by linking prospective surveys like the PSID to cancer registries or medical records. Finally, our estimates represent the average effects of cancer that necessarily vary across different cancer types and by respondent characteristics. Unfortunately our sample sizes of cancer survivors were too small for precise estimates by key individual and cancer characteristics.
The strengths of the present study include the data source and the analytic approach. The PSID is the world’s longest-running nationally representative household panel survey and widely regarded as the leading source of information about the economic and social dynamics of American families. The fixed-effects approach is a unique research design within this literature that takes advantage of prospectively-reported economic data before and after cancer diagnosis. This approach allows us to identify the effect of cancer on economic circumstances free of potential bias due to unobserved confounding by individual characteristics.
Future research should examine the effects of a cancer diagnosis across different population groups, such as by race, marital status, and family composition. Additionally, the impact of different types of cancer and treatment protocols needs to be disaggregated. Another promising avenue for future research as more data become available is to condition analyses on working outside of the home prior to diagnosis -- as many women are homemakers, including them in the analysis may blunt the estimated impact of cancer on employed women.
Our findings represent an important contribution to the literature on economic losses to cancer survivors and their families. To our knowledge, these are the first estimates of economic impact of cancer based on prospective economic survey data from a nationally-representative sample of American adults using a quasi-random design. Our estimates suggest that for the cohorts under consideration, a cancer diagnoses has serious implications for employment and labor market earnings for many years, and for the most part these economic outcomes do not return to their pre-diagnosis levels. Cancer history thus plays an important role in the economic well-being of millions Americans, and workplace or other policies should be considered to help buffer the impact of this serious but common health shock.
Acknowledgments
Funding: This work was supported by the National Institutes of Health: the National Cancer Institute (R03 CA149072 to A.Z.), the Eunice Kennedy Shriver National Institute of Child Health & Human Development (R24 HD041028) and the National Institute on Aging (P30 AG012846-14) to the Population Studies Center, University of Michigan. The funding for the source data was provided by the National Science Foundation, National Institute on Aging, National Institute of Child Health and Human Development, and additional funding agencies.
Footnotes
Financial disclosures: no disclosures.
Contributor Information
A. Zajacova, University of Wyoming.
J.B. Dowd, CUNY School of Public Health, Hunter College, City University of New York.
R.F. Schoeni, University of Michigan.
R.B. Wallace, University of Iowa.
REFERENCES
- 1.Guy GP, Ekwueme DU, Yabroff KR, et al. Economic Burden of Cancer Survivorship Among Adults in the United States. Journal of Clinical Oncology. 2013 doi: 10.1200/JCO.2013.49.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Moor JS, Mariotto AB, Parry C, et al. Cancer Survivors in the United States: Prevalence across the Survivorship Trajectory and Implications for Care. Cancer Epidemiology Biomarkers & Prevention. 2013 doi: 10.1158/1055-9965.EPI-12-1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown ML, Lipscomb J, Snyder C. The Burden of Illness of Cancer: Economic Cost and Quality of Life. Annual Review of Public Health. 2001;22:91–113. doi: 10.1146/annurev.publhealth.22.1.91. [DOI] [PubMed] [Google Scholar]
- 4.Baker F, Denniston M, Smith T, West MM. Adult Cancer Survivors: How Are They Faring? Cancer. 2005;104:2565–2576. doi: 10.1002/cncr.21488. [DOI] [PubMed] [Google Scholar]
- 5.Hewitt M, Rowland JH, Yancik R. Cancer Survivors in the United States: Age, Health, and Disability. Journal of Gerontology: Biological Sciences and Medical Sciences. 2003;58:82–91. doi: 10.1093/gerona/58.1.m82. [DOI] [PubMed] [Google Scholar]
- 6.Steiner JF, Cavender TA, Main DS, Bradley CJ. Assessing the Impact of Cancer on Work Outcomes. Cancer. 2004;101:1703–1711. doi: 10.1002/cncr.20564. [DOI] [PubMed] [Google Scholar]
- 7.Mehnert A. Employment and work-related issues in cancer survivors. Critical Reviews in Oncology/Hematology. 2011;77:109–130. doi: 10.1016/j.critrevonc.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 8.Bradley CJ, Neumark D, Luo Z, Bednarek H, Schenk M. Employment Outcomes of Men Treated for Prostate Cancer. Journal of the National Cancer Institute. 2005;97:958–965. doi: 10.1093/jnci/dji171. [DOI] [PubMed] [Google Scholar]
- 9.Hensley ML, Dowell J, Herndon JE, et al. Economic outcomes of breast cancer survivorship: CALGB study 79804. Breast Cancer Research and Treatment. 2005;91:153–161. doi: 10.1007/s10549-004-6497-9. [DOI] [PubMed] [Google Scholar]
- 10.Torp S, Nielsen RA, Fosså SD, Gudbergsson SB, Dahl AA. Change in employment status of 5-year cancer survivors. The European Journal of Public Health. 2013;23:116–122. doi: 10.1093/eurpub/ckr192. [DOI] [PubMed] [Google Scholar]
- 11.Earle CC, Chretien Y, Morris C, et al. Employment Among Survivors of Lung Cancer and Colorectal Cancer. Journal of Clinical Oncology. 2010;28:1700–1705. doi: 10.1200/JCO.2009.24.7411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moran JR, Short PF, Hollenbeak CS. Long-term employment effects of surviving cancer. Journal of health economics. 2011;30:505–514. doi: 10.1016/j.jhealeco.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bennett JA, Brown P, Cameron L, Whitehead LC, Porter D, McPherson KM. Changes in Employment and Household Income During the 24 Months Following a Cancer Diagnosis. Supportive Care in Cancer. 2009;17:1057–1064. doi: 10.1007/s00520-008-0540-z. [DOI] [PubMed] [Google Scholar]
- 14.Sharp L, Timmons A. The financial impact of a cancer diagnosis. Dublin, Ireland: National Cancer Registry/Irish Cancer Society; 2010. [Google Scholar]
- 15.Lauzier S, Maunsell E, Drolet M, Coyle D, Hebert-Croteau N, et al. Wage Losses in the Year After Breast Cancer: Extent and Determinants Among Canadian Women. Journal of the National Cancer Institute. 2008;100:321–332. doi: 10.1093/jnci/djn028. [DOI] [PubMed] [Google Scholar]
- 16.Ell K, Xie B, Wells A, Nedjat-Haiem F, Lee P-J, Vourlekis B. Economic stress among low-income women with cancer. Cancer. 2008;112:616–625. doi: 10.1002/cncr.23203. [DOI] [PubMed] [Google Scholar]
- 17.Hanratty B, Holland P, Jacoby A, Whitehead M. Financial Stress and Strain Associated with Terminal Cancer: A Review of the Evidence. Palliative Medicine. 2007;21:595–607. doi: 10.1177/0269216307082476. [DOI] [PubMed] [Google Scholar]
- 18.Covinsky KE, Goldman L, Cook EF, et al. The Impact of Serious Illness on Patients' Families. JAMA. 1994;272:1839–1844. doi: 10.1001/jama.272.23.1839. [DOI] [PubMed] [Google Scholar]
- 19.McGonagle KA, Schoeni RF, Sastry N, Freedman VA. The Panel Study of Income Dynamics: Overview, recent renovations, and potential for life course research. Longitudinal and Life Course Studies. 2012;3:268–284. doi: 10.14301/llcs.v3i2.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Institute for Social Research. Panel Study of Income Dynamics. 2013. [Google Scholar]
- 21.Hill MS. The Panel Study of Income Dynamics: A User's Guide. Beverly Hills: CA Sage; 1992. [Google Scholar]
- 22.Kim Y-S, Stafford FP. Technical Series Paper. Ann Arbor, MI: University of Michigan; 2000. The Quality of PSID Income Data in the 1990's and Beyond. [Google Scholar]
- 23.Andreski P, Gouskova E, McGonagle K, Schoeni RF. An Analysis of the Quality of the Health Data in the Panel Study or Income Dynamics. Ann Arbor, MI: University of Michigan; 2005. [Google Scholar]
- 24.Wilhelm MO. New Data on Charitable Giving in the PSID. Economics Letters. 2006;92:26–31. [Google Scholar]
- 25.Gouskova E, Schoeni RF. Comparing Estimates of Family Income in the Panel Study of Income Dynamics and the March Current Population Survey, 1968–2005. Ann Arbor, MI: Institute for Social Research, University of Michigan; 2007. [Google Scholar]
- 26.Haider S, Solon G. Life-cycle variation in the association between current and lifetime earnings. American Economic Review. 2006;96:1308–1320. [Google Scholar]
- 27.Jacobson LS, LaLonde RJ, Sullivan DG. Earning Losses of Displaced Workers. The American Economic Review. 1993;83:685–709. [Google Scholar]
- 28.Reville RT, Schoeni RF. Labor and Population Program Working Paper Series 01–08. Santa Monica, CA: RAND; 2001. Disability from Injuries at Work: The Effects on Earnings and Employment. [Google Scholar]
- 29.StataCorp. Stata Statistical Software: Release 11.0. College Station, TX: StataCorp, LP; 2009. College Station, TX. [Google Scholar]
- 30.Céilleachair AÓ, Costello L, Finn C, et al. Inter-relationships between the economic and emotional consequences of colorectal cancer for patients and their families: a qualitative study. BMC gastroenterology. 2012;12:62–71. doi: 10.1186/1471-230X-12-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zajacova A, Dowd JB, Schoeni RF, Wallace RB. Consistency and precision of cancer reporting in a multiwave national panel survey. Population Health Metrics. 2010;8:1–11. doi: 10.1186/1478-7954-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]