Abstract
In recent studies it has been suggested that Cognitive Behavior Therapy (CBT) is beneficial to people with Autism Spectrum Disorder (ASD) but that the method needs to be modified in relation to their cognitive profile. The aim of this study is to measure the effect of modified CBT, that is, using visualized language throughout the entire session for clients with ASD and anxiety and avoidance behavior. The modification of CBT in this study consists of focusing on CBT protocols for anxiety disorders and depression, while visualizing and systematizing “the invisible” in the conversation, in order for the clients to understand the social, cognitive and emotional context of self and others and how they should interact to avoid misunderstandings. ASD clients may need help to detect the invisible code of social interaction and communication. The level of anxiety and the frequency of target behavior were measured. Four assessments were made, two at the pre-assessment, and one in mid-therapy and end of therapy respectively. Generally, results suggest no improvement during pre-treatment period but a significant improvement during treatment. The values of the clients’ psychological, social and occupational ability to function improved on the Global Function Rating scale. The preliminary conclusion of this pilot study indicates that the use of visualized language throughout the CBT therapy sessions is a promising modification of current CBT protocols for individuals with ASD. After manualization, larger studies with randomized controlled study designs can replicate or challenge these results.
Keywords: ASD, anxiety, modified CBT, visualization, mindblindness
Introduction
Autism Spectrum Disorder (ASD1) is usually described as impairment of verbal and nonverbal communication, social interaction, emotion recognition and expression, as well as restricted patterns of behavior, interests and activities, with normal to high intelligence level (Arnstein Carpenter, Soorya & Halpern, 2009; Sanders, 2009). It is suggested that ASD clients have difficulties with “theory of mind,” or with empathic abilities (Gilberg, 1993; McLeod, Wood & Klebanoff, 2015). Gray (1995, 1998) talks about their difficulties with “the sixth sense” or difficulty in understanding the unwritten rules of social conduct. Baron-Cohen (1990) refers ASD difficulties to mindblindness, which affects communication and empathic ability. ASD clients’ cognitive profile is more systematic than others, thus enhancing seeing, understanding, building systems and the ability to systemize, which is an ongoing process throughout the day. Empathy has been described as cognitive empathy and affective empathy as well as sympathy (Baron-Cohen, 2003). As described by Ramsay, Brodkin, Cohen, Listerud, Rostain and Ekman (2005, p. 484):
Affective empathy can be conceptualized as an observer’s emotional response to another’s emotional reaction (e.g., “I feel your pain”). Cognitive empathy also referred to as ‘theory-of-mind’ refers to the observer’s ability to infer another’s emotional state (e.g., “I understand why you feel the way you do”). Following this line of thinking, sympathy could be thought of as a subset of these empathy categories, reflecting an observer’s desire to do something to alleviate another person’s suffering based on her or his emotional and cognitive response to the suffering being witnessed (e.g., “I want to do something to help you”).
Baron-Cohen refers to the above as the “empathy circuit,” which is regions in the brain involved in empathy, including a region for social information processing, that is, thinking of others and of yourself (Baron-Cohen, 2012). Social psychology points to the role of the self and how this part is used to predict multidimensional perception of other people. So far the study of the theory of mind and mindblindness has focused on understanding the social cues of others but not of “self” which today is known to play an important role in mindblindness (Lombardo & Baron-Cohen, 2010).
Mindblindness, which is suggested to be the cognitive explanation of social-communicative difficulties in ASD clients (Lombardo & Baron-Cohen, 2010), has to be taken into consideration in the clinical dialog (Gaus, 2010; Sofronoff, Attwood & Hinton, 2005). The present study has a focus on the effect of modified CBT on anxiety and avoidance behavior in clients diagnosed with ASD, by using visualized language to help the client understand and follow “the invisible, i.e. the dimension of the unspoken information” in the conversation throughout the sessions (see below).
Communication
In communication, ASD clients have difficulty understanding other people’s hints and intentions and how they are expected to act. Conversation is interpreted literally and the misunderstandings become numerous and troublesome (Gaus, 2011; McLeod et al., 2015). The information that non-ASD clients take for granted and never mention (Lombardo & Baron-Cohen, 2010) and that the ASD clients miss out on social interaction needs to be visualized and systematized for the ASD client if they are to know how to cognitively process the information and be part of the dialog as well as understand the intentions. Not understanding the dialog and “the whole picture” is a common problem causing anxiety and avoidance behavior. The whole picture is the emotional, cognitive and social context of “self and others” and our experiences of the situation. This context presents itself in our mind, as we are involved in a dialog.
Most people do not reflect on the mental picture automatically visualized, while they listen or talk. The picture is often referred to as “my experience” or “I just know” (referring to a picture of memories and experience one has come across and carry around). This mental picture becomes our map, in order to orient our self in a dialog and to understand our self and others. It is “the unspoken” information in the dialog, that the ASD client does not see and therefore does not consider and understand, since it is not visual information.
The therapist, on the other hand, can in the dialog with the client use her/his own ability to visualize “the invisible” in the dialog and use it as a manual. The therapist can visualize and systematize the invisible on a paper or a whiteboard, as the dialog continues. When the client understands, the likelihood of decrease in anxiety and avoidance behavior is common (Donoghue, Stallard & Kurcia, 2011; Gaus, 2007, 2011; Gray, 1995, 1998).
The therapist and the client need to elaborate on thoughts and emotions, desires and needs as well as experiences, in order to understand the causes of the problem (i.e. the conceptualizion) as well as to be active participants in therapy. The conceptualization involves the ability to be self-referential, i.e. to see and understand “self and others” and the interaction with the surrounding environment. The conceptualization is “a bigger picture” (Lombardo & Baron-Cohen, 2010).
The “invisible” and “the whole picture” of self and others will become our map to orient our self when we need to understand our own and other peoples desires, needs thoughts and emotions as well as the social world around us. It will help us to ask necessary questions, to structure our activities and to make plans. To systemize what automatically is in our own mind by visualizing it when we communicate, helps the ASD client to understand automatically. The therapist will be the client’s eyes and help her/him see the whole mental picture.
Cognitive Behavioral Therapy (CBT)
Generally, the intervention literature on ASD is suffering from methodological limitations. Therefore, an important issue facing the field is how to develop and evaluate effective interventions (McLeod et al., 2015). Mainstream psychotherapy treatment with CBT for emotional disorders has provided increasingly positive treatment results in the past decades and are very efficacious in relieving symptoms of these conditions. Several studies have indicated these results (e.g. O’Donohue & Fischer, 2009; Roth & Fonagy, 2005). However, there are only a few studies of modified CBT treatment on ASD clients (Hesselmark, Plenty & Bejerot, 2013). Most of these are of children, individually or in groups, as well as with parental involvement. The therapeutic work is mainly based on various written manuals, visual materials and behavioral strategies, such as role play, relaxation and social skills training, involving tuition in the codes of social conduct, conflict resolution and friendship skills. Commonly used techniques are thought bubbles, toolboxes and manuals like facing your fear, as well as Multi-Component Integrated Treatment (MCIT) (Attwood, 2004; Gaus, 2011; Reaven, Blakeley-Smith, Culhane-Shelburne & Hepburn 2012; Reaven, Blakeley-Smith, Nichols, Dasari, Flanigan & Hepburn, 2009; Sofronoff, Attwood, Hinton & Levin, 2007; Sze & Wood 2007; 2008; White, Ollendick, Scahill, Oswald & Albano, 2009). Cat-kit is a pedagogic manual used to help children develop a better cognitive and emotional understanding of self (Callesen, Nielsen & Attwood, 2006).
Aim of the present study
The aim of this study is to investigate if ASD clients benefit from a modified CBT using visualization in the communication during treatment. The specific goal is to investigate any possible changes regarding anxiety level and behavioral changes in target behaviors.
Methods
This study was carried out in three different settings and cities: a private clinic, a child and adolescent psychiatric clinic and at a treatment center for youth. The therapists were proficient and experienced CBT therapists of clients with ASD and CBT. It was a quantitative study with four assessments, two at the pre-assessment stage, and one in mid-therapy and end of therapy respectively. The average time between pre-treatment and start of therapy was 1.86 months, between start of therapy and mid-therapy assessment 2.56 months and between mid-therapy and the end of therapy 2.88 months.
Participants
All clients had a diagnosis of ASD, with anxiety and avoidance behavior. Specific psychiatric diagnoses besides the ASD were not made since the treatment interventions were problem-focused because of the ASD diagnosis. The ASD diagnosis as well as the anxiety disorder were established and verified by the client’s psychiatric clinic. The anxiety diagnosis included social phobia, panic disorder, Obsessive Compulsive Disorder (OCD), and depression with anxiety. Avoidance behavior was the main reason besides the anxiety problems for seeking psychotherapeutic treatment and was established in the first interview and the assessment. Clients were recruited through advertisement on the private clinics website, on a ASD website, from the clinics’ waiting lists and from the treatment center’s waiting list, stating that free CBT psychotherapy using visualization was offered to ASD clients. Clients’ (n = 18) demographic data can be seen in Table1.
Table 1.
Client demographic and clinical data
| Variable | Treatment group (n = 18) |
|---|---|
| Gender | |
| Female adults | 4 (22.2 %) |
| Male adults | 7 (38.9%) |
| Female teens | 3 (16.7%) |
| Male teens | 4 (22.2 %) |
| Age (yrs) | |
| Adults | |
| M (SD) | 29.8 (4.4) |
| Interval | 23–36 |
| Teens | |
| M (SD) | 14.9 (1.5) |
| Interval | 13–17 |
| School/employment | |
| School 7th grade | 2 (11.1%) |
| High school | 1 (5.6%) |
| Jobs program | 3 (16.7%) |
| Employment | 2 (11.1%) |
| Special school for individuals with ASD | 4 (22.2 %) |
| Long-term sick leave | 6 (33.3%) |
| Help with homework 1–9th grade (Yes/No) | 6/12 |
| Absence from school 1–9th grade | |
| 2 days / week | 8 (44.4%) |
| 1–4 days / month | 0 (0%) |
| 1–3 times / semester | 1 (5.6%) |
| Always present in school | 9 (50%) |
| Social activity level at pre-treatment | |
| 2 days / year | 3 (16.7%) |
| 2 days / month | 6 (33.3%) |
| 2 days / week | 9 (50%) |
| Daily | 0 (0%) |
| Children (adults) | 5 (23.8%) |
| Number of months | |
| On waiting list | |
| M (SD) | 1.9 |
| Interval | 0.5–3.75 |
| In therapy | |
| M (SD) | 5.2 |
| Interval | 2–9 |
| Problem areas except ASD | |
| Social phobia | 6 (33.3%) |
| OCD | 5 (27.8%) |
| Eating disorder | 1 (5.6%) |
| Aggressive behavior, acting out | 1 (5.6%) |
| Stalker, inappropriate behavior towards women | 2 (11.1%) |
| Multiple problemsa | 3 (16.7%) |
Multiple problems can include some of the following areas: depression, anxiety, sleeping problems, eating problems.
Three therapists aged 47–60 (M = 52.3) with a mean of 6 years of experience working with CBT participated in the treatment. Two therapists were males and one female. Two therapists treated teenagers, on average 2.5 clients, ages 13–16 and one therapist treated 11 adults and 2 teenagers. The prerequisites for carrying out the therapy sessions were qualifications as CBT therapist, several years of CBT experience in a clinical setting as well as experience of working with ASD clients. In the private clinic there were four adult women (mean age of 33) and 7 adult men (mean age of 31), one teenage boy aged 14 and one teenage girl aged 17. In the treatment center for youth, there was one girl aged 14 and two boys aged 16. In the child and adolescent psychiatric clinic, there was one teenage girl aged 14 and one teenage boy aged 13.
Earlier treatments for their ASD and the problems given as target behaviors were identified: seven had mainstream CBT treatment without visualization, two had other treatment and three had no earlier treatment. Eighteen clients started treatment (11 clients over the age of 18) and all completed the treatment.
Design
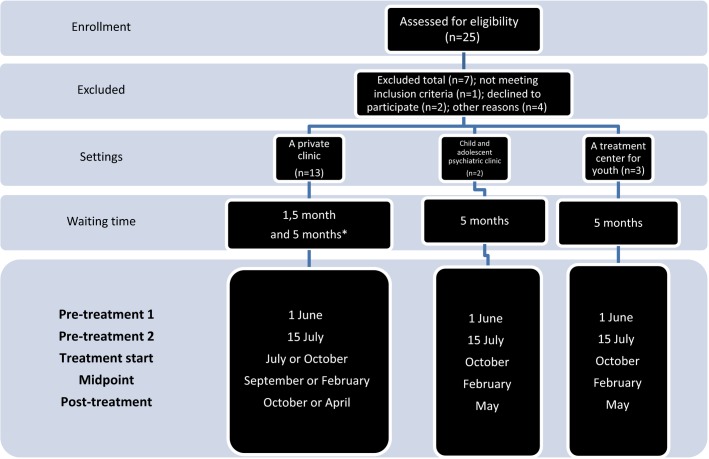
The clients were on a waiting list before the start of the therapy, and thereafter they were subjected to treatment (see Fig.1). The therapy was based on target behaviors, set by the therapists and client in consultation with their supervisor. Visualization was introduced from session one and throughout every session. The therapy was conducted individually for 15 sessions, every second week or at the client’s convenience. Each session generally lasted for approximately 45–60 minutes. Participation was without charge and neither the clients nor the therapists were given any economic compensation. Each therapist was supervised by a qualified psychotherapist who was a trained supervisor with several years of experience as a CBT supervisor and as a therapist working with CBT and patients with ASD. Supervision was provided every fourth week. The CBT treatment was not manual-based. Supervision focused on visualization, the behavioral analysis, rational and treatment methods. The therapy was performed with visualized language on a whiteboard, which was photographed and saved in a folder, which the client had constant access to for the purpose of using the worksheets in- between sessions and for homework.
Figure 1.
Flow diagram depicting the recruitment process. *Randomization between conditions.
Assessments were made at pre-treatment with a minimum of one and a half month to five months prior to treatment, during treatment twice a week, as well at the end of therapy, for the entire group. The therapist was included in the assessments to help the client assess target behavior and make sure that the assessments were made whenever clients had difficulties in performing the assessments (see the Appendix for the Assessment Schedule).
Instrument
Within the framework of this study, the clients and the therapists in conjunction set the target behavior for excessive and avoidance behaviors, measured in terms of frequency and/or intensity of the specific behavior. The objectives were to reduce excessive behaviors and increase avoidance behaviors. Behavioral excess is, for example, “excessive and unnecessary control and safety behaviors,” “impulsivity,” “sleeping,” and “inappropriate behavior.” Examples of avoidance behavior are “not starting to socialize with friends,” “not making phone calls,” “not asking for help,” “not waking up on time,” “not going to school,” and “not being able to handle changes.” Further, “worry,” “fear” and “intrusive thoughts/obsessions” are examples of cognitive excess, while cognitive avoidance is part of “the whole picture,” what others expect of you, “the unspoken,” for example reflections over getting a job, own apartment, as well as reflections over emotions and thoughts of own behavior. The clients estimated their level of anxiety and frequency of the target behaviors. The level of anxiety and the frequency of target behavior were measured on a scale from 0–3 for anxiety and 0–4 for frequency. Target behaviors are relatively concrete and with ASD clients, it is preferable to use more concrete and pictorial representation of registration and gradation (Gaus, 2007; Sze & Wood, 2008). In this study, visualized language was used to set the target behaviors and instruct on how to assess them. Background data were taken concerning earlier treatment, CBT, other or none. The clients filled in a questionnaire on how they experienced visualization in terms of making it easier to remember the conversation during the session and the use of the visual material when doing homework. The therapists used the Global Function Rating scale (GAF scale) for the pre- and post-treatment assessments (Söderberg & Tungström, 2007).
Methods of collecting data
All data were collected by the therapists and thereafter processed by the project leader (first author), however, the project leader was not one of the therapists. In the assessment, the problems caused by the ASD could as far as possible be differentiated from the symptoms of anxiety, which mainly appeared as conditioned fear of the ASD mindblindness problem of not being able to understand. This became clearer in the behavior analysis and conceptualization assessment, where the thoughts and emotions in a specific situation, and the conditioning and the maintenance were established. The behavior analysis made it easier to set and specify target behavior. Psycho education was given for anxiety and depression as well as for avoidance behavior and mindblindness in order for the client to learn to discriminate between these problems as far as possible. The CBT assessment is a therapist-client joint assessment (McLeod et al., 2015).
Baseline, i.e. measurement of pre-treatment 1 to pre-treatment 2, for all the targets behaviors was set in the first interview. The clients filled in all background data on a sheet at home and brought it to the session. The therapists collected the data in the sessions. Any questions or difficulties in monitoring the data were brought up and addressed during the sessions.
Procedure
At the first interview, the therapist informed the client about the project and when consent to participate in the study was given, the therapists interviewed the client about the target behavior that the client would be motivated to change. The pre-treatment assessment form was handed out to each client at this interview and instructions were given on how to fill in the form and what to assess. All assessment charts were handed in at the start of therapy and continuously every second week. Only data from pre-treatment (1 and 2), midpoint and post-treatment was used in the analysis. Help was given to fill in the form at every therapy session if necessary. The forms were placed in each client’s file and kept there until the end of therapy. Files were also kept at the clinics.
Intervention
Visualization in CBT
In this study, the visualization of self and how self interacts with others has been an important part of the treatment as this method not only visualizes but also systematizes emotions, abilities, actions and the conceptualizing of self and others, including intention and empathy. These aspects are usually what make us more prone to develop co-morbid anxiety, depression, anger and behavioral difficulties as well as to manage emotions and thoughts. The co-morbid problems will often lead to anxiety, depression and isolation. These are often the problems present in treatment as well as in relationships and social interactions (Gaus, 2010; Lombardo & Baron-Cohen, 2010). Generally, many ASD clients have difficulties in school and end up staying at home and do not finish school. Some have several academic degrees but still have difficulties seeking employment or keeping a job. Often they do not seek help or they leave treatment and end up in habilitation units, where they receive help, in order to get by in their daily life (Gaus, 2011).
In most studies the suggestions are that CBT is beneficial to individuals with ASD but the method needs to be modified based on their cognitive profile (Attwood & Scarpa, 2013; Gaus, 2007; 2011). The modification of CBT in this study has been to focus on CBT protocols for anxiety disorders and avoidance behavior (Roth & Fonagy, 2005), while visualizing and systematizing the invisible in the therapy conversation in order for the clients to understand the social and emotional context of self and others, of interaction, and of “the whole picture” (Lombardo & Baron-Cohen, 2010) that non ASD individuals automatically grasp. The modification was made with respect to each client’s communication style, which is more likely to yield more accurate assessment and information (Gaus, 2010), especially on what is necessary for exposure therapy and other CBT interventions (Reaven et al., 2012).
The therapist may ask the question: Why do you not go to school, work, etc.? This question derives from and involves the therapist’s mental states and pictures, which can be visualized and systematized on a whiteboard, thus helping the ASD client to understand and answer the questions. The manual, in other words, is in the therapist’s own mind and is visualized when communicated. When the therapist uses the ability to mentalize and materialize the mental states and pictures on the whiteboard while speaking, the visualized language used in the conversation serve to illustrate and systematize for the client. Other examples of such a conversation could be: What will be your problem when you start school? The question involves the therapist’s thoughts and emotional states related to different situations, such as walking to school, being in the classroom, and various social situations not mentioned but taken for granted in the therapist’s mind. Drawing “a school, pathway and the client walking” will help the client to start mentalizing in their own minds and start reflecting, answering and asking questions. The therapist’s ability to understand automatically will be the manual used to visualize the questions, “How will I know what I like and want, How do I know what friends to have?” In order to teach and help the client, the therapist needs to explain how this is usually understood by experience. Experience is the term for knowledge, skills, observations and involvement in events.
In CBT, the formulation of the problem, the rationale and the various interventions depend on the dialog between the therapist and the client. All this information is shared by the therapist and the client, thus building a relationship between them, which is important to the therapy and essential in understanding the conversation (Gaus, 2010).
The conversation may be conducted and communicated in the same way as with any other client, although adjusted to the individual client and their cognitive profile, since ASD clients often are verbal and intellectually capable (Gaus, 2010, 2011). In CBT, information is commonly visualized on the whiteboard and in therapy with the ASD client, the therapist adds “the invisible” to the visualization and takes “mindblindness” into consideration.
Statistics
The processing of data was conducted with the aid of the statistics program SPSS (IBM, Armonk, NY). A one-way repeated measures analysis of variance (ANOVA) was used (i.e. within group design). The means of baseline target behaviors for each individual at the start, the middle and the end of therapy were calculated for behavior – behavioral and cognitive excessive and avoidance behaviors. A correlation analysis was carried out to see if correlation existed between clients’ level of improvement and the number of therapy sessions attended. The Bonferroni correction was applied to prevent a mass significance problem.
Results
Global function rating
The Global Function Rating scale (GAF scale) value was estimated by the therapists at pre- and post-treatment. Pair-wise t-test showed a significant improvement from pre- (M = 55.72, SE = 2.19) to post-treatment (M = 73.17, SE = 2.71), t(17) = 7.14, p < 0.0001.
Anxiety level and frequency of behavioral excess and avoidance
Results suggest a significant improvement from pre- to post-treatment. Regarding behavioral excess and avoidance, the one-way ANOVAs showed statistically significant changes from pre- to post-treatment.
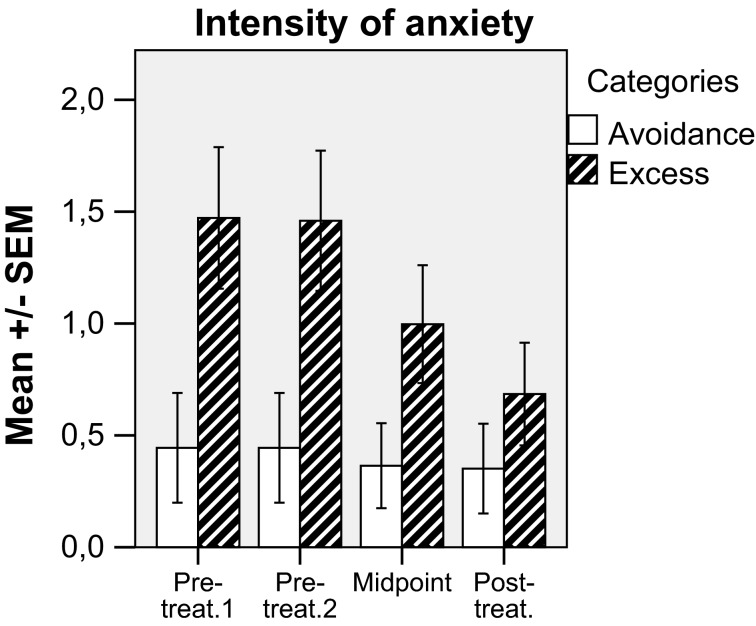
Anxiety related to behavioral excess
This showed a statistically significant level of symptom reduction F(3, 51) = 6.56, p < 0.001, ηp2 = 0.28, Cohen’s d = 0.96. In post hoc tests (Bonferroni) this was explained by a significant decrease in anxiety from both pre-measurements to post-treatment (p < 0.05) (Fig. 2).
Figure 2.
Client’s mean (+ SE) estimation for anxiety related to behavioral excess and avoidance behavior.
Anxiety related to behavioral avoidance
This showed a statistically significant level of symptom reduction F(3, 51) = 11.90, p < 0.0001, ηp2 = 0.41, Cohen’s d = 0.99. In post hoc tests (Bonferroni), this was explained by a significant decrease in anxiety from both pre-measurements to post-treatment (p < 0.005) (Fig. 2).
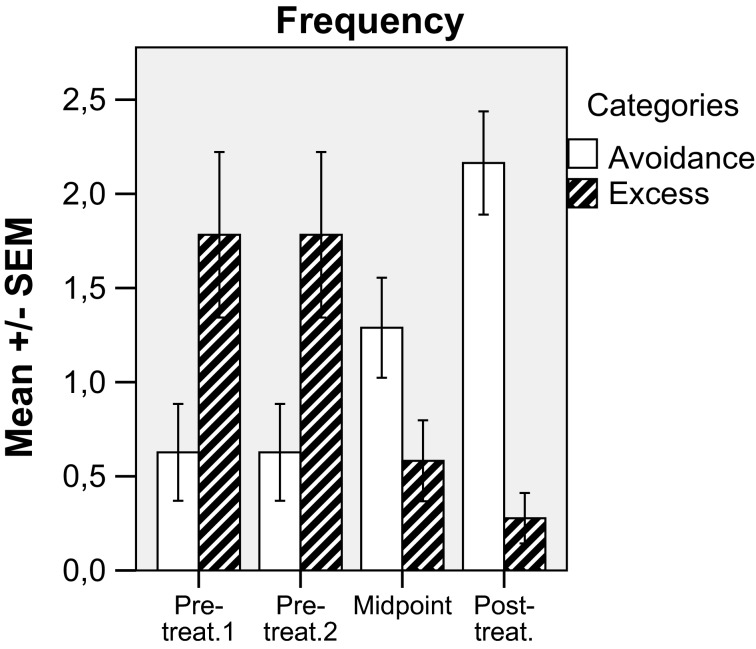
Frequency of behavioral excess
This showed statistically significant changes in frequency, F(3, 51) = 13.86, p < 0.0001, ηp2 = 0.45, Cohen’s d = 1.0. In post-hoc tests (Bonferroni), this was explained by a significant decrease in frequency from both pre-measurements to midpoint (p < 0.05) and post-treatment (p < 0.01) (Fig. 3).
Figure 3.
Client’s mean (+ SE) estimation for frequency related to behavioral excess and avoidance behavior.
Frequency of behavioral avoidance
This showed statistically significant changes in frequency F(3, 48) = 11.27, p < 0.0001, ηp2 = 0.41, Cohen’s d = 1.0. In post-hoc tests (Bonferroni), this was explained by a significant increase in frequency from both pre-measurements to post-treatment (p < 0.01). Increase from midpoint to post-treatment was also significant (p < 0.05) (Fig. 3).
Anxiety level and frequency of cognitive excess and avoidance
Anxiety related to cognitive excess
This showed a significant main term F(3, 51) = 11.57, p < 0.001, ηp2 = 0.41, Cohen’s d = 1.0. In post-hoc tests (Bonferroni), this was explained by a significant decrease in frequency from both pre-measurements to midpoint (p < 0.05) and post-treatment (p < 0.05) (Fig. 4).
Figure 4.
Client’s mean (+ SE) estimation for anxiety related to cognitive excess and avoidance behavior.
Anxiety related to cognitive avoidance, frequency of cognitive excess as well as frequency of cognitive avoidance
Anxiety related to cognitive avoidance behavior (Fig. 4) showed no significant differences (NS). Frequency of cognitive avoidance and excess behavior (not shown in any figure) showed no significant differences in either one.
Effects of visualization
All clients were asked two questions about visualized language, (i) does the visual language make it easier to remember the conversation with the therapist in the session, and (ii) was the visualized material useful when you did your homework. As shown in Table2, distributions of answers show that the majority of the clients were helped by visualization.
Table 2.
Frequency of the clients’ answers regarding visualization
| Yes | Not known | No | P* | |
|---|---|---|---|---|
| Help from visualization | 14 | 1 | 3 | 0.001 |
| Visualization useful in homework’s | 13 | 2 | 3 | 0.005 |
One-sample Chi-Square test.
Discussion
In most studies of ASD and CBT, suggestions are made to use modified CBT adapted to client profile (Attwood & Scarpa, 2013; Gaus 2007, 2011; Sofronoff et al., 2005). There are numerous studies using materials and manuals which include various visualizations for specific situations in the modification (Attwood, 2004; Callesen et al., 2006; Gaus, 2011; Moree and Davis, 2010; Reaven et al., 2009; 2012; Sofronoff et al., 2007; Sze & Wood, 2007; 2008; White et al., 2009) Visualizing the language in ongoing conversation makes it easy for both parties to follow and use the conversation as it is used in conversation with any client. CBT combined with visualized language may therefore complement earlier studies on ASD and CBT modification.
The purpose of this study was to measure the effect of modified cognitive behavioral therapy (CBT) using visualized language throughout the entire session with clients diagnosed with ASD, and anxiety and avoidance behavior. The results show a significant change in behavioral excess and avoidance behavior, for anxiety level and frequency and cognitive excess behaviors for anxiety level. There was no significant change in cognitive excess behaviors for frequency and cognitive avoidance behavior for anxiety level and frequency.
In exposure therapy, it is common for the frequency level of cognitive excess behavior, such as intrusive thoughts, to increase at the beginning of treatment and decrease at a later time when the anxiety level has decreased and maintenance is abandon. In this study the cognitive excess behaviors showed this pattern for anxiety but showed no significant change in frequency. Several reasons for this can be discussed. One reason might be that a longer treatment period or more sessions than this study allowed for may be needed in order to see the effect on frequency. Another reason might be the sample size. It may also be due to the systematic thinking of ASD clients, who might be more prone to observe and estimate concrete thoughts even without anxiety.
The cognitive avoidance behavior for anxiety and frequency showed no significant change. It can be argued that this may be due to their cognitive profile. Mindblindness involves difficulties to observe and “see” what is not “obvious” and not evident or literally visible in the mind. Cognitive avoidance is part of “the whole picture.” It has to be visualized and presented to the ASD client before it can be observed, allowing for estimating frequency and anxiety. It is tantamount to asking; “Do you not have … ” or asking if something is not present … etc. This usually results in ASD clients commenting, “you can’t see NOT.”
The analysis of the clients’ psychological, social and occupational functioning ability on the Global Function Rating scale, which measures quality of life and functioning in daily life, showed improvement. These were also concretized target behaviors for the clients. However, since the global function rating was made by the therapists, a possible bias could have affected this measurement.
CBT modification using visualized language throughout the entire sessions makes the conversation systematic and concrete and can make it easier for ASD clients to follow a conversation and be part of it, thus avoiding misunderstandings and confusions. “Ordinary conversation” in social interaction may contribute to ASD clients’ confusion and may increase the level of anxiety. A shared language and understanding with less discomfort and anxiety are important parts in building a relationship, making an assessment and engaging in treatment interventions. From the personal assessment charts, a pattern of sudden change in target behavior can be seen in several cases rather then gradual progress over a longer time. In the work and journal notes, it is noticeable that the change occurs in relation to the understanding of the intervention and the rationale. One hypothesis drawn from this may be that once the problem is resolved and ASD clients understand, their actions will be different.
An increasing number of adults as well as children and teenagers are seeking psychotherapeutic help in the ASD population and their communication problems are becoming more known to schools and other public institutions. ASD clients and many others will integrate more easily if communication generally is made more understandable. Using visualized language in schools and daily life, as well as in therapy, can help ASD clients understand “the spoken words” and take part in communication activities more easily. It is handy, inexpensive and always available and can always be adjusted to whoever the client is. To prevent ASD clients developing co-morbid problems we need to develop a more empathetic view of their profile. Referring to ASD as a profile rather than a disorder, as Baron-Cohen and co-workers do, might be part of this change (Lombardo and Baron-Cohen, 2010).
In this study there is no control group for CBT without visualization. This limitation of the study makes it impossible to compare the effectiveness of CBT with visualization with CBT without visualization. This was excluded for ethical reasons since studies show that ASD clients are in need of information about the ‘unwritten rules’ of social conduct (Gaus, 2011) and benefit from the use of pictures in sessions (Ramsay et al., 2005).
The results above should be replicated and generalized through further studies. Additional research needs to be done with a manual for visualized language in various settings. After manualization, larger studies with randomized controlled study designs and assessment of treatment fidelity, can be conducted. Until that, the results of current study should be considered preliminary. In both groups, target behaviors could be more specified for easier measuring and fewer in number for the individual ASD client, which would increase the client’s ability to make the assessment. The difficulty in specifying the target behaviors is the ASD client’s communication impairment and mindblindness. Setting targets for behavior must therefore be part of the treatment with visualization, which possibly deserves a study of its own.
Part of these data was presented at the 44th EABCT Congress, 10–13 September 2014, The Hague (Ekman, E and Hiltunen, A. Abstract nr. A-617-0000-00286).
Appendix Assessment schedule
In the first meeting, you and your therapist will assess your target behavior. The therapist will guide you and help you to formulate these behaviors. She/he will ask you questions about the behaviors in order to understand what they are and get them right.
Write down the behavior or a situation in which you get anxiety, you avoid or want to change.
These are behaviors you want to be able to do, get help for or get rid of.
These behaviors/situation are called “Target behaviors.” These can be behaviors or cognitions.
Write down each one of them.
Each time you have this behavior:
Write down the date, how frequent you estimate its occurrence and if you feel anxious, estimate the level of anxiety for this behavior or situation.
In the column for comments you may write down any comment in relation to this behavior/situation.
You will take this form with you and continue to fill it at home. You may ask your therapist for help if there is something you do not understand about how to fill in this form.
| Target behavior /target cognition | Date | Frequency* | Anxiety (0–3) | Comment |
|---|---|---|---|---|
Frequency: 4 = always, 3 = almost always, 2 = sometimes, 1 = a little, 0 = never/nothing
Note
The term ASD is used in this study, according to DSM–V, formerly called Asperger’s Syndrome, and also recognized as High Functioning Autism Spectrum Disorder.
References
- Arnstein Carpenter L, Soorya L. Halpern D. Asperger’s Syndrome and high-functioning Autism. Pediatric Annals. 2009;38:30–35. doi: 10.3928/00904481-20090101-01. [DOI] [PubMed] [Google Scholar]
- Attwood T. Cognitive behaviour therapy for children and adults with Asperger’s Syndrome. Behaviour Change. 2004;21:147–161. [Google Scholar]
- Attwood T. Scarpa A. CBT for children and adolescents with high-functioning autism spectrum disorder. New York: Guilford Press; 2013. pp. 27–44. [Google Scholar]
- Baron-Cohen S. Autism: A specific cognitive disorder of mind-blindness. International Reveiw of Psychiatry. 1990;2:81–90. [Google Scholar]
- Baron-Cohen S. Mindblindness: An essay on autism and theory of mind. Cambridge, MA: MIT Press; 1995. [Google Scholar]
- Baron-Cohen S. The essential difference, the truth about the male and the female brain. New York: Guilford Press; 2003. [Google Scholar]
- Baron-Cohen S. Zero degrees of empathy. Harmondsworth: Penguin Books; 2012. [Google Scholar]
- Callesen K, Nielsen AM. Attwood T. Cat-kit: Cognitive affective training, CAT-kit.com ApS. (original edition. 2005. Journal of Norwegian Psychological Association. 2006;8:69–74. [Google Scholar]
- Donoghue K, Stallard P. Kurcia J. The clinical practice of Cognitive Behavioural Therapy for children and young people with a diagnosis of Asperger’s Syndrome. Clinical Child Psychology and Psychiatry. 2011;16(1):89–102. doi: 10.1177/1359104509355019. [DOI] [PubMed] [Google Scholar]
- Gaus VL. Cognitive-behavioral therapy for adult Asperger syndrome. New York: Guilford Press; 2007. [Google Scholar]
- Gaus VL. Adult asperger syndrome and the utility of cognitive-behavioral therapy. Journal of Contemporary Psychotherapy. 2010;41:47–56. [Google Scholar]
- Gaus VL. Cognitive behavioural therapy for adults with autism spectrum disorder. Advances in Mental Health and Intellectual Disabilities. 2011;5:15–25. [Google Scholar]
- Gilberg C. Empatistörningar, Grundläggande vid flera svåra psykiatriska handikapptillstånd? [Empathy Disorders, Basic at several severe psychiatric disabilities?] Läkartidningen. 1993;90:467–470. [PubMed] [Google Scholar]
- Gray C. The original social story book. Arlington, TX: Future Horizon; 1995. [Google Scholar]
- Gray C. Social stories and comic strip conversation with students with Aspergers syndrom and high-functioning Autism. In: Kunce LJ, editor; Schopler IE, Mesibov G, editors. Asperger’s Syndrome or high functioning Autism? New York: Plenum Press; 1998. pp. 167–168. [Google Scholar]
- Hesselmark E, Plenty S. Bejerot S. Group cognitive behavioural therapy and group recreational activity for adults with autism spectrum disorders: A preliminary randomized controlled trial. Autism. 2013;18:672–683. doi: 10.1177/1362361313493681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lombardo MV. Baron-Cohen S. The role of the self in mindblindness in autism. Consciousness and Cognition. 2010;20:130–140. doi: 10.1016/j.concog.2010.09.006. [DOI] [PubMed] [Google Scholar]
- McLeod BD, Wood JJ. Klebanoff S. Advances in evidence-based intervention and assessment practices for youth with an Autism Spectrum Disorder. Behavior Therapy. 2015;46:1–6. doi: 10.1016/j.beth.2014.07.004. [DOI] [PubMed] [Google Scholar]
- Moree BN. Davis TE., III Cognitive-behavioral therapy for anxiety in children diagnosed with autism spectrum disorders: Modification trends. Research in Autism Spectrum Disorder. 2010;4:346–354. [Google Scholar]
- O’Donohue W, editor; Fischer JE, editor. Cognitive Behavior Therapy, applying empirically supported techniques in your practice. 2nd edn. Hoboken, NJ: John Wiley & Sons; 2009. [Google Scholar]
- Ramsay RJ, Brodkin ES, Cohen MR, Listerud J, Rostain AL. Ekman E. “Better Strangers”: Using the relationship in psychotherapy for adult patients with Asperger Syndroms. Psychotherapy: Theory. Research, Pratice, Training. 2005;42:483–493. [Google Scholar]
- Reaven J, Blakeley-Smith A, Culhane-Shelburne K. Hepburn S. Group cognitive behavior therapy for children with high-functioning autism spectrum disorders and anxiety: A randomized trial. Journal of Child Psychology and Psychiatry. 2012;53:410–419. doi: 10.1111/j.1469-7610.2011.02486.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reaven JA, Blakeley-Smith A, Nichols S, Dasari M, Flanigan E. Hepburn S. Cognitive-behavioral group treatment for anxiety symptoms in children with high-functioning autism spectrum disorders. Focus on Autism and Other Developmental Disabilities. 2009;24:27–37. [Google Scholar]
- Roth A. Fonagy P. What works for whom? A critical rewiew of psychotherapy research. 2nd edn. New York: The Guilford Press; 2005. [Google Scholar]
- Sanders JL. Qualitative or quantitative differences between Asperger’s Disorder and Autism? Historical considerations. Journal of Autism and Developmental Disorders. 2009;39:1560–1567. doi: 10.1007/s10803-009-0798-0. [DOI] [PubMed] [Google Scholar]
- Sofronoff K, Attwood T. Hinton S. A randomized controlled trial of a CBT interventions for anxiety in children with Asperger syndrome. Journal of Child Psychology and Psychiatry. 2005;46:1152–1160. doi: 10.1111/j.1469-7610.2005.00411.x. [DOI] [PubMed] [Google Scholar]
- Sofronoff K, Attwood T, Hinton S. Levin I. A randomized controlled trial of a cognitive behavioural intervention for Anger Management in children diagnosed with Asperger Syndrome. Journal of Autism Developmental Disorders. 2007;37:1203–1214. doi: 10.1007/s10803-006-0262-3. [DOI] [PubMed] [Google Scholar]
- Sze KM. Wood JJ. Cognitive behavioral treatment of comorbid anxiety disorders and social difficulties in children with high – functioning autism: A case report. Journal of Contemporary Psychotherapy. 2007;37:133–143. [Google Scholar]
- Sze KM. Wood JJ. Enhancing CBT for treatment of Autism Spectrum Disorder and Concurrent Anxiety. Behavioral and Cognitive Psychotherapy. 2008;36:403–409. [Google Scholar]
- Söderberg P. Tungström S. 2007. Outcome in psychiatric outpatient service: Reliability, validity and outcome based on routine assessments with the GAF scale. Doctoral dissertation, Department of Psychology, Umeå University.
- White SW, Ollendick T, Scahill L, Oswald D. Albano AM. Preliminary efficacy of a cognitive-behavioral treatment program for anxious youth with Autism Spectrum Disorders. Journal of Autism Developmental Disorders. 2009;39:1652–1662. doi: 10.1007/s10803-009-0801-9. [DOI] [PMC free article] [PubMed] [Google Scholar]