Key Points
Ten of 36 patients (28%) achieved an OS ≥30 months in a blinatumomab study in relapsed/refractory acute lymphoblastic leukemia.
Long-term survival may be associated with T-cell expansion, B-cell depletion, and a minimal residual disease response.
Abstract
This long-term follow-up analysis evaluated overall survival (OS) and relapse-free survival (RFS) in a phase 2 study of the bispecific T-cell engager antibody construct blinatumomab in 36 adults with relapsed/refractory B-precursor acute lymphoblastic leukemia (ALL). In the primary analysis, 25 (69%) patients with relapsed/refractory ALL achieved complete remission with full (CR) or partial (CRh) hematologic recovery of peripheral blood counts within the first 2 cycles. Twenty-five patients (69%) had a minimal residual disease (MRD) response (<10−4 blasts), including 22 CR/CRh responders, 2 patients with hypocellular bone marrow, and 1 patient with normocellular bone marrow but low peripheral counts. Ten of the 36 patients (28%) were long-term survivors (OS ≥30 months). Median OS was 13.0 months (median follow-up, 32.6 months). MRD response was associated with significantly longer OS (Mantel-Byar P = .009). All 10 long-term survivors had an MRD response. Median RFS was 8.8 months (median follow-up, 28.9 months). A plateau for RFS was reached after ∼18 months. Six of the 10 long-term survivors remained relapse-free, including 4 who received allogeneic stem cell transplantation (allo-SCT) as consolidation for blinatumomab and 2 who received 3 additional cycles of blinatumomab instead of allo-SCT. Three long-term survivors had neurologic events or cytokine release syndrome, resulting in temporary blinatumomab discontinuation; all restarted blinatumomab successfully. Long-term survivors had more pronounced T-cell expansion than patients with OS <30 months.
Introduction
The prognosis is poor for adult patients with relapsed/refractory (r/r) B-precursor acute lymphoblastic leukemia (ALL). Treatment with chemotherapy has been reported to result in median overall survival (OS) from 4.5 to 8.4 months.1-5 Five-year OS rates with chemotherapy are only 7% to 10%.1,2 Median OS is 5.8 months among patients who relapse after allogeneic stem cell transplantation (allo-SCT) and 10 months among patients who relapse after chemotherapy only (without prior allo-SCT).5
Blinatumomab, a CD19/CD3 bispecific T-cell engager (BiTE) antibody construct, leads to redirected lysis of CD19-positive (CD19+) target B cells by inducing a transient cytolytic synapse between the target cells and T cells.6 In an exploratory dose-finding phase 2 study in adult patients with r/r B-precursor ALL (including patients in late first relapse >12 months), 69% of patients achieved complete remission with full hematologic recovery (CR) or complete remission with partial hematologic recovery (CRh), and 88% of responders achieved a minimal residual disease (MRD) response within the first 2 treatment cycles.7 In addition, an MRD response was seen in 2 patients with hypocellular bone marrow and in 1 patient with partial response (normocellular bone marrow but low peripheral counts). The study explored constant dosing as well as single-step and double-step dosing to prevent severe cytokine release syndrome (CRS). In a confirmatory phase 2 study of 189 patients with r/r B-precursor ALL, including those with early relapse (<12 months) after first remission, 43% achieved CR or CRh after 2 cycles of treatment with blinatumomab.8 Median relapse-free survival (RFS) was 5.9 months; median OS was 6.1 months.
The first analysis of the phase 2 dose-finding study analyzed OS with a median follow-up of 12.1 months.7 The long-term follow-up analysis, presented here, evaluated OS at a median follow-up of 32.6 months. We evaluated clinical characteristics, including disease-related medical history before blinatumomab treatment; outcomes of blinatumomab treatment, including hematologic and MRD responses to blinatumomab, adverse events, consolidation with allo-SCT, and relapses; and T-cell and B-cell kinetics during treatment.
Patients and methods
Study design
This report describes a follow-up analysis of relapse and OS; the methods of the primary analysis are described elsewhere.7 This was an open-label, multicenter, exploratory, single-arm phase 2 study in adult patients with r/r B-precursor ALL conducted in collaboration with the German Study Group for Adult Acute Lymphoblastic Leukemia. The target population was Philadelphia chromosome (Ph)-negative and Ph-positive patients with primary refractory disease or relapse. Key exclusion criteria were Ph-positive ALL eligible for dasatinib or imatinib treatment; autologous stem cell transplantation within 6 weeks or allo-SCT within 3 months before the start of blinatumomab treatment; or history or presence of clinically relevant central nervous system (CNS) pathology, active CNS leukemia, active graft-versus-host disease and/or immunosuppressive therapy for graft-versus-host disease within 1 week of blinatumomab treatment start, or active infections.7 The study protocol was approved by the Paul Ehrlich Institute and by each study site’s independent ethics committee, and written informed consent was obtained from each patient in accordance with the Declaration of Helsinki. Toxicity and efficacy data were reviewed by an independent data monitoring committee. This trial is registered at www.clinicaltrials.gov as #NCT01209286.
Study procedures
The first 2 cycles of blinatumomab were administered to induce remissions. A bone marrow aspirate or biopsy sample was obtained before the first blinatumomab cycle and on day 29 of each cycle; cytomorphology and MRD were assessed in central reference laboratories. CR was defined by ≤5% blasts in the bone marrow, no evidence of circulating blasts or extramedullary disease, platelets >100 000/μL, hemoglobin ≥11 g/dL, and absolute neutrophil count >1500/μL. CRh was defined by the same criteria but with a lower minimum of peripheral blood counts (platelets >50 000/μL, hemoglobin ≥7 g/dL, and absolute neutrophil count >500/μL). An MRD response was defined as MRD <10−4 by allele-specific real-time quantitative polymerase chain reaction for clonally rearranged immunoglobulin and/or T-cell receptor genes (sensitivity ≥10−4).9
Each treatment cycle was 6 weeks, including 4 weeks of continuous IV infusion and a 2-week treatment-free interval. The dose-finding stage used the following dosing schedules: cohort 1 (n = 7) received blinatumomab 15 μg/m2 per day; cohort 2a (n = 5) received 5 μg/m2 per day in week 1 and then 15 μg/m2 per day; cohort 2b (n = 6) received blinatumomab 5 μg/m2 per day in week 1, 15 μg/m2 per day in week 2, and then 30 μg/m2 per day. In the extension stage, cohort 3 (n = 18) used the dosing schedule from cohort 2a. In the case of CR or CRh, consolidation treatment with up to 3 additional cycles of blinatumomab and/or allo-SCT was permitted. After 1 incidence of grade 4 CRS, prephase treatment with dexamethasone (≤24 mg per day for 1-5 days) and/or cyclophosphamide (200 mg/m2 per day for 1-4 days) was allowed. Each patient had mandatory intrathecal CNS prophylaxis with methotrexate (15 mg), cytarabine (40 mg), and dexamethasone (4 mg) administered by a spinal tap during screening and on day 29 of each cycle. IV dexamethasone (16 mg) or equivalent was given within 1 hour of treatment start. Adverse events were collected throughout the study and graded by the Common Terminology Criteria for Adverse Events (Version 4.0).10
Analysis of lymphocyte subpopulations
T-cell and B-cell kinetics were assessed in each patient. Using methods that were described previously,11 peripheral blood mononuclear cells were isolated at various time points before and throughout the first and second cycle of blinatumomab treatment and stained with fluorescent-labeled antibodies against the following cell surface markers: CD3+/CD13−/CD14− or CD3+/CD45+ (T cells); CD3+/CD45RA−/CD197− (effector memory T [TEM] cells); and CD19+/CD13−/CD14− or CD19+/CD45+ (B cells). Flow cytometry data were collected on a FACSCanto II (Becton Dickinson, Heidelberg, Germany), or Navios 10/3 instrument (Beckman Coulter, Krefeld, Germany). Statistics were analyzed by the software FCS Express (De Novo Software, Glendale, CA) or Kaluza (Beckman Coulter). Percentages of lymphocyte subpopulations were multiplied by absolute lymphocyte numbers from a differential blood count to calculate absolute cell numbers for each lymphocyte subpopulation. The analysis set included all available and/or evaluable data points (T and TEM cells, before blinatumomab infusion [on day 1 (baseline)] and on days 8, 15, 22, and 29 of each cycle; B cells, same schedule but also on day 3 of each cycle), regardless of blinatumomab dosing regimen.
Statistical analysis
RFS was measured from the time of first CR or CRh to hematologic or extramedullary relapse or death resulting from any cause. Patients still in remission at data lock were censored at the time of last remission status assessment. OS was measured from the time of first blinatumomab dose to death resulting from any cause. Kaplan-Meier methods were used to estimate the probability of RFS and OS over time, providing median and 95% confidence intervals (CIs). A Mantel-Byar test was conducted to evaluate the OS benefit associated with achieving an MRD response vs not achieving an MRD response, and Simon-Makuch plots12 were used to visualize the survival estimates over time between those who did and did not achieve an MRD response at each event time. A log-rank test was conducted to compare OS between patients with prior allo-SCT vs those without prior allo-SCT.
Long-term survivors were defined as patients with OS ≥30 months. This definition of long-term OS is based on published data, which show that most events occur within the first 24 months.5 Patients were grouped by MRD response and by OS duration (<30 months or ≥30 months). Summary statistics were provided for each subgroup, including clinical characteristics before blinatumomab treatment, use of allo-SCT before or after blinatumomab treatment, treatment response and relapse, and adverse events.
Results
Treatment response
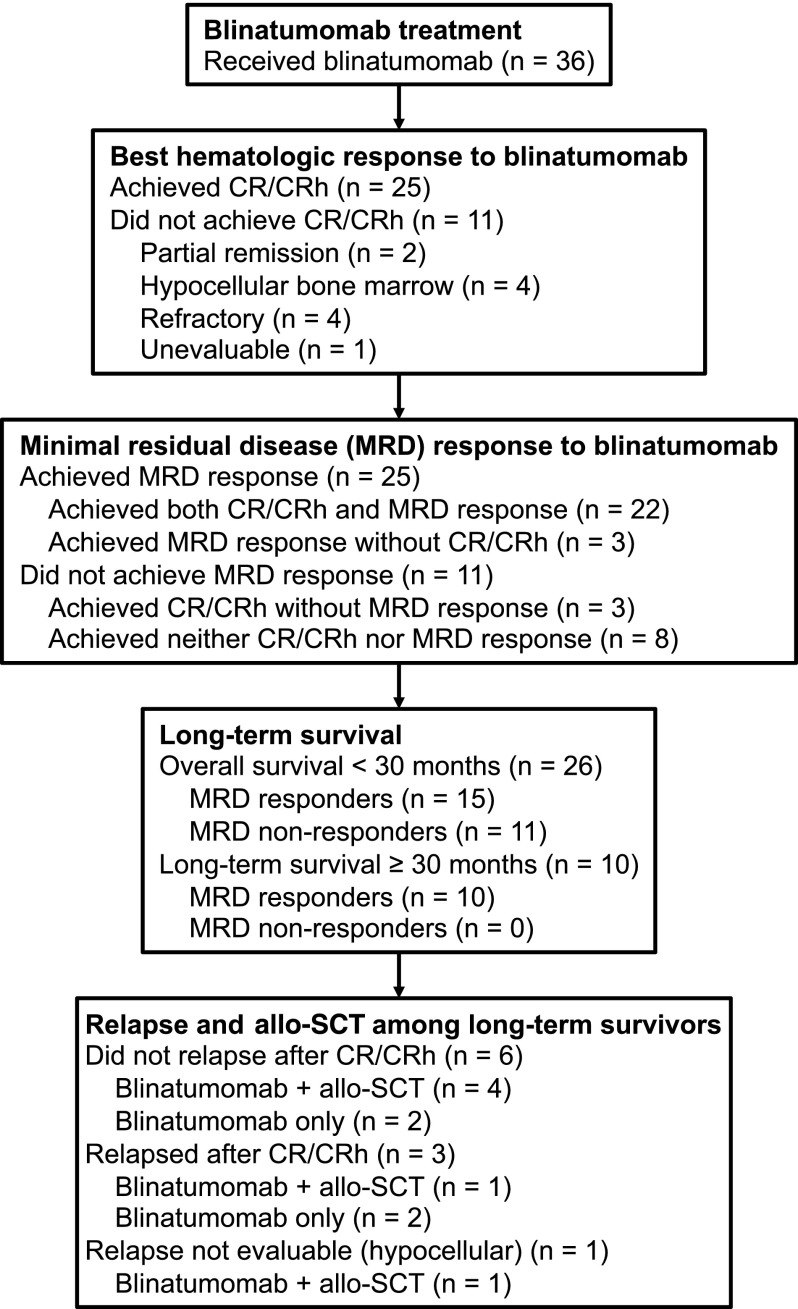
Thirty-six patients (Table 1) were treated at 9 centers in Germany between October 6, 2010, and June 19, 2012, with follow-up ongoing. Patient disposition according to treatment response is shown in Figure 1. As described previously for the primary analysis,7 the rate of CR/CRh was 69% (25/36 patients). Seventeen patients (47%) achieved CR, and 8 patients (22%) achieved CRh as a best response during the treatment period (Table 2). The other patients had partial remission (n = 2) or hypocellular bone marrow (n = 4), or were refractory to treatment (n = 4) or unevaluable (n = 1). Twenty-two of 25 patients with CR/CRh (88%) had an MRD response (3 responders did not achieve an MRD response). An additional 3 patients with bone marrow that did not fulfill the criteria for CRh had an MRD response. Thus, 25 of 36 patients (69%) who were treated with blinatumomab had an MRD response.
Table 1.
Clinical characteristics
| MRD responders | MRD nonresponders |
|||
|---|---|---|---|---|
| OS ≥30 mo (n = 10) | OS <30 mo (n = 15) | Total (N = 25) | OS <30 mo* (N = 11) | |
| Age, y | ||||
| Median | 35 | 37 | 37 | 27 |
| Range | (21–72) | (23–77) | (21–77) | (18–66) |
| Prior therapy/disease status, n (%) | ||||
| Prior allo-SCT | 4 (40) | 5 (33) | 9 (36) | 6 (55) |
| No prior allo-SCT | 6 (60) | 10 (67) | 16 (64) | 5 (45) |
| Primary refractory | 2 (20) | 0 (0) | 2 (8) | 1 (9) |
| Salvage 1 after first CR | 4 (40) | 6 (40) | 10 (40) | 1 (9) |
| ≤12 mo after initial diagnosis | 2 (20) | 3 (20) | 5 (20) | 0 (0) |
| >12 mo after initial diagnosis | 2 (20) | 3 (20) | 5 (20) | 1 (9) |
| ≥Second salvage | 0 (0) | 4 (27) | 4 (16) | 3 (27) |
| Bone marrow blasts at screening, % | ||||
| Median | 56 | 73 | 61 | 83 |
| Range | (8–97) | (9–93) | (8–97) | (6–96) |
| Prephase treatment, n (%) | ||||
| Dexamethasone | 8 (80) | 6 (40) | 14 (56) | 6 (55) |
| Cyclophosphamide | 4 (40) | 3 (20) | 7 (28) | 5 (46) |
All of the MRD nonresponders had an OS <30 mo.
Figure 1.
Patient disposition. Of the 36 patients in the study, 25 achieved CR or CRh and 11 patients did not achieve CR/CRh. Furthermore, 25 patients achieved an MRD response and 11 patients did not achieve an MRD response. Although numerically identical, the MRD response subgroups overlapped but were not the same as the CR/CRh response subgroups.
Table 2.
Summary of response, follow-up treatment, and relapse
| Outcome, n (%) | MRD responders | MRD nonresponders |
||
|---|---|---|---|---|
| OS ≥30 mo (n = 10) | OS <30 mo (n = 15) | Total (N = 25) | OS <30 mo* (N = 11) | |
| Best response† | ||||
| CR | 7 (70) | 8 (53) | 15 (60) | 2 (18) |
| CRh | 2 (20) | 5 (33) | 7 (28) | 1 (9) |
| Hypocellular bone marrow | 1 (10) | 1 (7) | 2 (8) | 2 (18) |
| Partial remission | 0 (0) | 1 (7) | 1 (4) | 1 (9) |
| Allo-SCT after CR/CRh‡ | 5 (50) | 8 (53) | 13 (52) | 0 (0) |
| Allo-SCT after hypocellular bone marrow | 1 (10) | 1 (7) | 2 (8) | 1 (9) |
| Retreatment with blinatumomab | 1 (10) | 2 (13) | 3 (12) | 2 (18) |
| Relapse-free after blinatumomab | 6 (60) | 0 (0) | 6 (24) | 0 (0) |
| Blinatumomab treatment only | 2 (20) | 0 (0) | 2 (8) | 0 (0) |
| Blinatumomab and allo-SCT | 4 (40) | 0 (0) | 4 (16) | 0 (0) |
All of the MRD nonresponders had an OS <30 mo.
Best response during the treatment period.
Excludes patients who relapsed and received chemotherapy before allo-SCT.
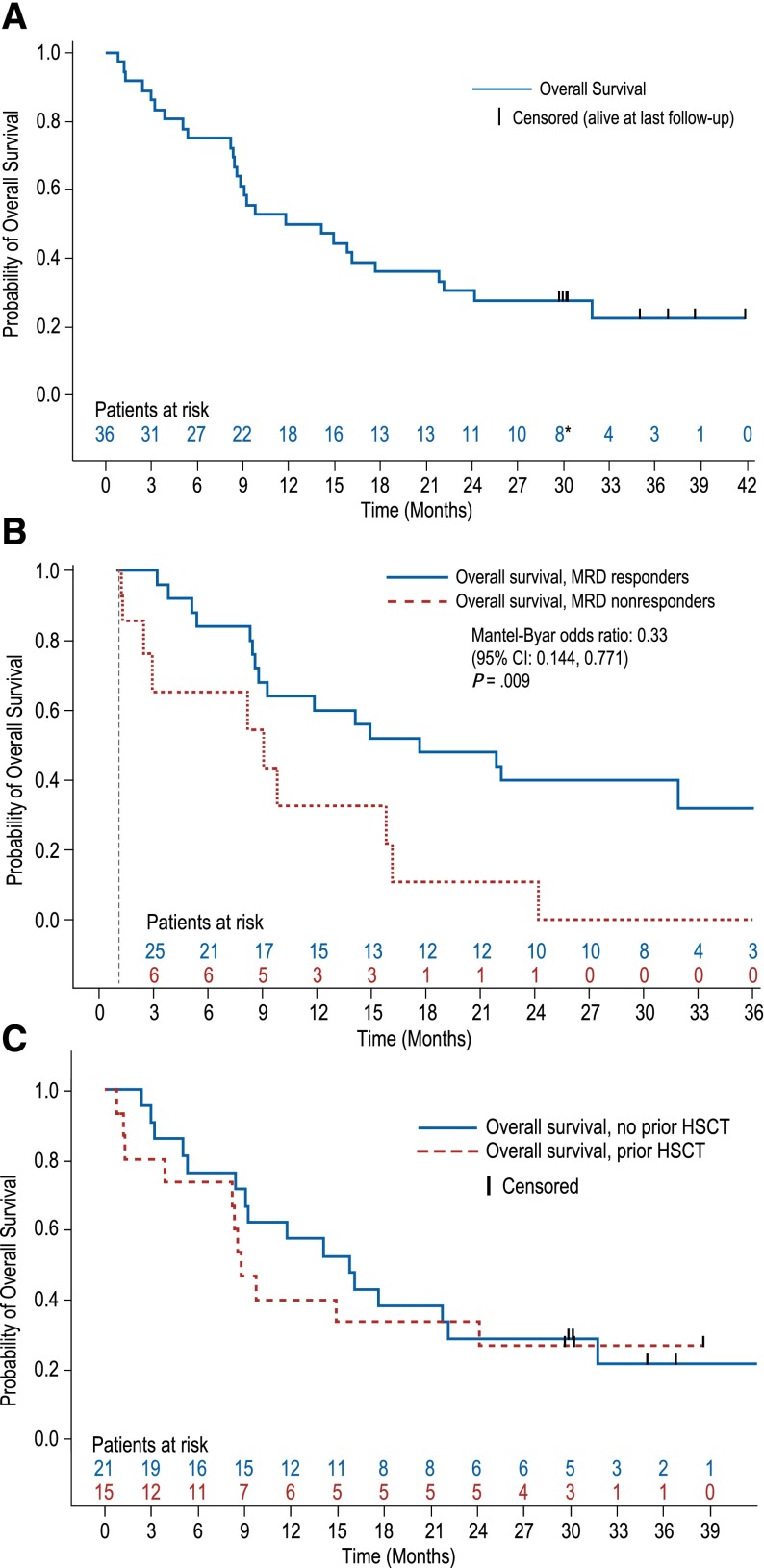
OS
At a median follow-up time of 32.6 months (range, 0.8-41.9 months), median OS was 13.0 months (95% CI, 8.5-21.9 months) (Figure 2A). A plateau was reached for OS after ∼33 months. The Mantel-Byar odds ratio was 0.33 (P = .009), indicating a 67% risk reduction associated with an MRD response (Figure 2B). A difference in OS between patients with and without prior allo-SCT was not detected (log-rank P = .640; Figure 2C).
Figure 2.
Probability of OS. (A) OS in the entire patient population (N = 36) at a median follow-up of 32.6 months. *Two patients who were alive at the last follow-up at 29.7 and >29.9 months were censored at these visits and were considered to have an OS of ≥30 months after rounding to the nearest whole number. (B) Simon-Makuch analysis of OS in patients with and without MRD response. (C) OS with and without prior allo-SCT in the entire patient population (N = 36) at a median follow-up of 32.6 months. HSCT, hematopoietic stem cell transplantation.
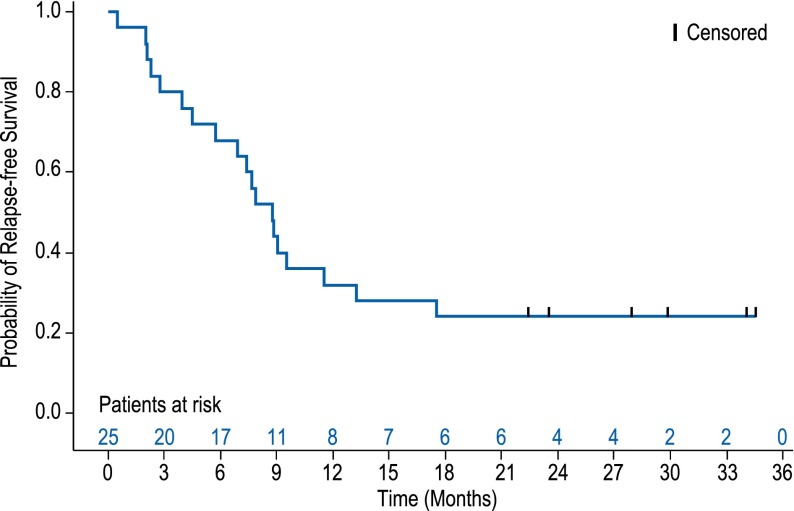
RFS
At a median follow-up time of 28.9 months (range, 0.5-34.5 months), median RFS was 8.8 months (95% CI, 5.7-13.2 months) among all 25 patients with CR/CRh. At ∼18 months, a plateau was reached for RFS, with 6 patients not having a documented relapse after this time (Figure 3). Of the 6 patients with long-term RFS, 4 patients underwent allo-SCT as consolidation for blinatumomab and 2 patients received 3 additional cycles of blinatumomab instead of allo-SCT. The 3 patients with CR/CRh and no MRD response had relapses after 0.5, 2.0, and 9.0 months, respectively.
Figure 3.
Probability of RFS. RFS among responders (n = 25) at a median follow-up of 28.9 months.
Clinical characteristics
Patients were divided into 3 groups. The first group included the 10 patients who were long-term survivors, defined as OS ≥30 months after the start of blinatumomab treatment, all of whom achieved an MRD response. The second group included the 15 patients with an MRD response who were not long-term survivors. The third group included the 11 MRD nonresponders, none of whom were long-term survivors. The main clinical characteristics for each subgroup are summarized in Table 1. A detailed listing of clinical characteristics for all 36 patients in the study is provided in supplemental Table 1, available on the Blood Web site. Based on individual patient–level data, the 3 patient groups had a similar number of prior salvage treatments, prior allo-SCT, prephase treatment with dexamethasone and/or cyclophosphamide, and administration of immunoglobulins. Median blast count was numerically lowest in the long-term survivors and highest in patients with no MRD response, but these differences were not statistically significant. Treatment responses, follow-up treatment, and relapses are summarized by MRD response and duration of survival categories in Table 2. A detailed listing for all 36 patients in the study is provided in supplemental Table 2. Seven of the long-term survivors achieved a CR (70%), but 2 patients with CRh (20%) and 1 patient with hypocellular bone marrow (10%) were also among the long-term survivors. None of the 11 patients without an MRD response was a long-term survivor. Best response to blinatumomab, follow-up treatment, and relapse for individual long-term survivors are shown in Table 3.
Table 3.
Best response to blinatumomab, follow-up treatment, and relapse for individual long-term survivors
| Patient No.* | Cohort | Best response† | MRD response | Allo-SCT after blinatumomab | RFS duration (mo) | Blinatumomab retreatment after relapse | OS duration (mo) |
|---|---|---|---|---|---|---|---|
| 5 | 2b | CR | Yes | No | 17.5 | Yes | 38.6 |
| 8 | 3 | CR | Yes | Yes | 34.5‡ | No | 35.0 |
| 10 | 3 | CRh | Yes | No | 22.4‡ | No | 30.0§ |
| 20 | 2b | CR | Yes | No | 34.1‡ | No | 36.9 |
| 23 | 3 | Hypocellular | Yes | Yes | N/A | No | 29.7§ |
| 26 | 3 | CR | Yes | Yes | 11.5 | No | 31.9‖ |
| 27 | 3 | CR | Yes | Yes | 23.5‡ | No | 30.3 |
| 29 | 2a | CR | Yes | No¶ | 2.8 | No | 41.9 |
| 31 | 3 | CRh | Yes | Yes | 27.9‡ | No | 30.2 |
| 32 | 3 | CR | Yes | Yes | 29.9‡ | No | 30.3 |
N/A, not applicable.
Patient No. refers to patients listed in supplemental Table 1.
Best response during the treatment period.
Patient was still relapse-free at the time of the analysis.
Patient had an OS of ≥30 mo after rounding to the nearest whole value.
Death.
Chemotherapy was administered after blinatumomab and before allo-SCT.
Long-term survivors with allo-SCT as consolidation for blinatumomab
Six of the 10 long-term survivors underwent allo-SCT as consolidation for blinatumomab (Table 2). Three of 6 patients previously received allo-SCT before blinatumomab treatment. Five of 6 patients were still alive at the last follow-up for this analysis, including the 3 patients who received allo-SCT before blinatumomab. One of the 3 patients achieved hypocellular bone marrow as treatment response to blinatumomab; the other patients achieved a CR or CRh as the best response to blinatumomab treatment.
Long-term survivors without allo-SCT as consolidation for blinatumomab
Four of the 10 long-term survivors did not undergo allo-SCT as consolidation for blinatumomab. All 4 achieved a CR or CRh as the best response to blinatumomab treatment. One of these 4 patients received 2 prior allo-SCTs. All 4 patients were still alive at the last follow-up for this analysis. Two of these 4 patients are in ongoing remission without further treatment. One patient has been alive for 30.0 months since the start of blinatumomab treatment (the patient had a reversible grade 4 CRS). The other patient has been alive for 36.9 months since the start of blinatumomab treatment (the patient had a reversible grade 3 neurologic event). The other 2 patients relapsed after blinatumomab treatment. One of these patients had 2 CD19+ relapses >12 months after having received 5 cycles of blinatumomab but responded to blinatumomab after each relapse with an MRD-negative remission (3 cycles of retreatment each time). The other patient had a CD19-negative relapse during the third cycle of blinatumomab. This patient achieved another remission after chemotherapy with fludarabine, cytarabine, idarubicin, and filgrastim and received allo-SCT as consolidation for the chemotherapy. The patient was still alive at a follow-up of 41.9 months. Relapses in the CNS were not reported.
Adverse events in long-term survivors
Adverse events associated with blinatumomab treatment have been previously described in detail for all 36 patients enrolled in the study.7 Among the long-term survivors, 3 had treatment-related adverse events (neurologic events or CRS) that resulted in treatment interruption (Table 4). All 3 patients received no treatment other than blinatumomab. Two of the 3 patients are still in remission; 1 patient had a CD19+ relapse that was successfully retreated with blinatumomab.
Table 4.
Neurologic events and CRS leading to treatment interruption in long-term survivors
| Patient No.* | Blinatumomab dose (μg/m2/d) | Cycle | Adverse event, CTCAE grade | Blinatumomab dose at restart of treatment (μg/m2/d) | Prophylaxis | Response, RFS, OS | Alive/In remission |
|---|---|---|---|---|---|---|---|
| 5 | 15 | 1 | Convulsion, grade 2 | 5 | Clobazam | CRh, | Yes/No (relapse) |
| RFS 17.5 mo, | |||||||
| OS 38.6 mo | |||||||
| 20 | 30 | 2 | Encephalopathy, grade 3 | 5 | No | CR, | Yes/Yes |
| RFS 34.1 mo, | |||||||
| OS 36.9 mo | |||||||
| 10 | 5 | 1 | CRS, grade 4 | 5 | Prephase dexamethasone† | CRh, | Yes/Yes |
| RFS 22.4 mo, | |||||||
| OS 30.0 mo‡ |
Long-term survivors were defined as patients with an OS ≥30 mo.
CTCAE, Common Terminology Criteria for Adverse Events (Version 4.0).
Patient No. refers to patients listed in supplemental Table 1.
Up to 24 mg/d dexamethasone for up to 5 d and/or 200 mg/m2/d cyclophosphamide for up to 4 d before blinatumomab infusion.
Patient first achieved remission on study day 99 and had to restart cycle 1 after interruptions.
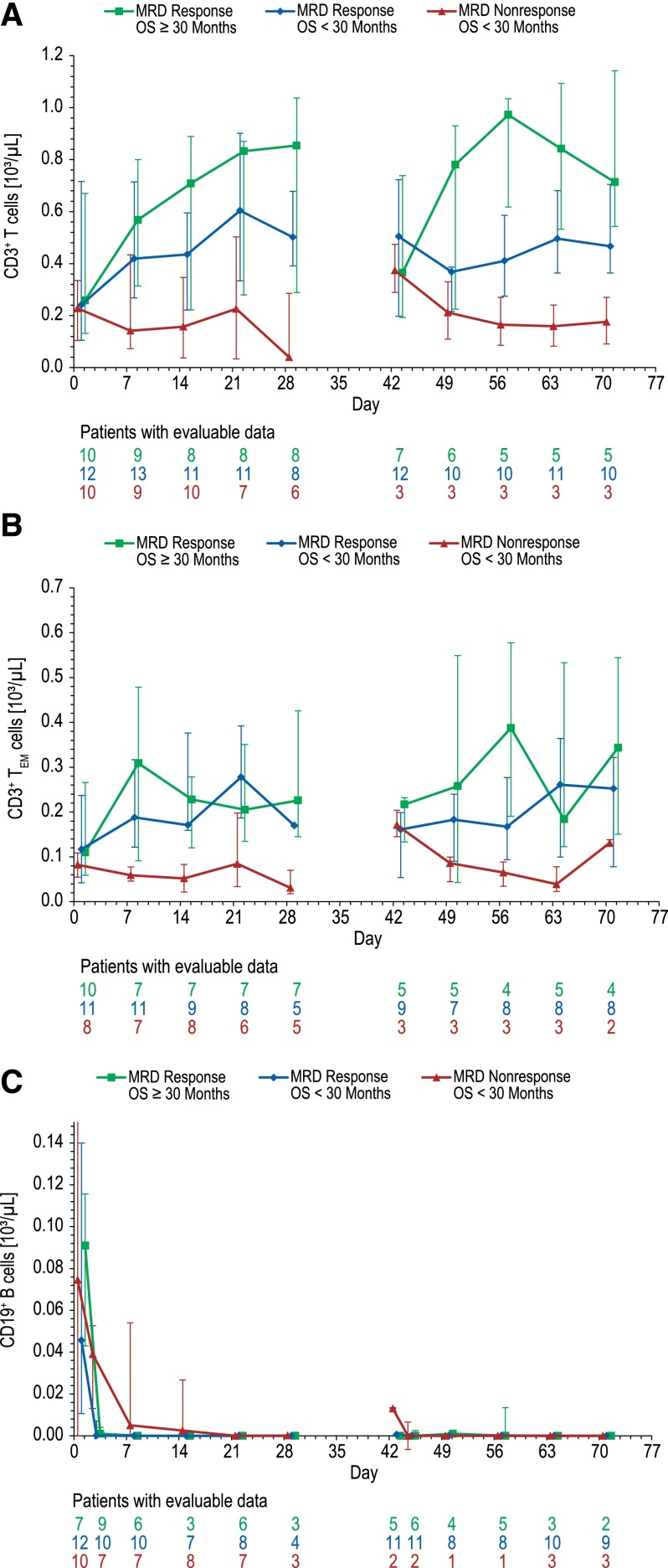
T-cell and B-cell kinetics
Expansion of CD3+ T cells, which was analyzed by kinetics of median cell counts during treatment cycles 1 and 2, was predominantly observed in MRD responders who had OS ≥30 months, in both cycle 1 and cycle 2 (Figure 4A). Increased T-cell numbers appeared to contract toward baseline during the 2-week treatment-free interval between cycles 1 and 2, mimicking a naturally occurring T-cell response also consisting of a T-cell activation, expansion, and contraction phase. MRD responders with OS <30 months showed some T-cell expansion in cycle 1, but not in cycle 2, whereas T-cell expansion was absent in MRD nonresponders in both cycles. Of note, the most pronounced CD3+ T-cell expansion was observed in a long-term survivor with an MRD response who experienced a grade 3 neurologic adverse event but did not receive any treatment other than 5 cycles of blinatumomab (data not shown).
Figure 4.
T-cell and B-cell kinetics during cycle 1 (day 1 to 29) and cycle 2 (day 43 to 71) of blinatumomab treatment. (A) CD3+ T-cell expansion. (B) CD3+ TEM-cell expansion. (C) CD19+ B-cell depletion. Patients were grouped according to MRD response and duration of OS (<30 vs ≥30 months). Data shown are median cell values (interquartile range) with numbers of evaluable data points per patient subgroup at each time point given below. For clarity, initial T-cell redistribution during the first treatment week of cycles 1 and 2 is not shown.
CD3+ T-cell expansion was associated with increasing numbers of CD3+ TEM cells, which play an important role in blinatumomab-induced apoptosis of target B cells due to their large cytotoxic potential (Figure 4B). Other memory T-cell subsets like CD8+ TEM cells with reacquired CD45RA or CD4+ central memory T cells also added to overall CD3+ T-cell expansion (data not shown). Of note, MRD nonresponders not only showed no CD3+ T-cell and CD3+ TEM-cell expansion, but also had the lowest absolute cell counts of these important T-cell populations.
In addition, the kinetics of CD19+ B-cell depletion differed between MRD responders and nonresponders (Figure 4C). Median B-cell depletion was ≤1 cell/μL at day 3, complete at day 8, and sustained throughout treatment cycles 1 and 2 in MRD responders regardless of OS duration. In contrast, in patients without an MRD response, median duration of B-cell depletion lasted 22 days, with detectable return of peripheral B cells before the start of treatment cycle 2 at day 43.
Discussion
This long-term follow-up analysis to the primary analysis of the first phase 2 study of blinatumomab in 36 adult patients with r/r B-precursor ALL demonstrated a median OS of 13.0 months with 32.6 months of follow-up, and a median RFS of 8.8 months with 28.9 months of follow-up. Previous studies have reported that chemotherapy treatment of patients with r/r ALL results in median OS ranging from 4.5 to 8.4 months.1-5 Recently published results for treatment in r/r ALL with inotuzumab ozogamicin, an anti-CD22 monoclonal antibody drug conjugate, showed a median OS of 7.3 months with a weekly dosing schedule.13 Furthermore, a previous study reported that OS with salvage chemotherapy in relapsed ALL is shorter among patients who relapse after allo-SCT.5 Many of the patients in the present study relapsed after allo-SCT before they received blinatumomab, but there was no difference in OS between patients with and without prior allo-SCT.
In this follow-up analysis, 10 of the 36 patients initially treated with blinatumomab were long-term survivors, defined by an OS of ≥30 months, and 6 of the 25 patients who achieved CR/CRh had long-term RFS. Although our results are preliminary and collection of larger data sets is warranted, the analysis points to some factors that may have influenced long-term outcomes after blinatumomab treatment. All long-term survivors previously achieved an MRD response. These results suggest that achievement of an MRD response with blinatumomab treatment in r/r B-precursor ALL may translate into clinical benefit in terms of long-term survival. Of the 6 long-term survivors who remained relapse-free after blinatumomab treatment, 2 received blinatumomab only, and 4 received blinatumomab followed by allo-SCT. These data suggest that the use of allo-SCT as consolidation for blinatumomab is a feasible treatment concept that warrants testing in larger trials. Based on individual patient–level data, prephase treatment with dexamethasone or cyclophosphamide did not have a negative impact on long-term survival. This finding is in line with previous observations from the large confirmatory phase 2 study of 189 patients in which a multivariate analysis showed no effect of dexamethasone prephase treatment on response.8
We also examined the outcome of patients who either received blinatumomab as their only therapy or who received retreatment with blinatumomab after relapse. Three long-term survivors received no other treatment after blinatumomab infusion. All 3 patients experienced neurologic adverse events or CRS that resulted in temporary interruption of blinatumomab treatment. Similar toxicities were reported in a phase 1 study of autologous T cells expressing the 19-28z chimeric antigen receptor specific for the CD19 antigen,14 suggesting that toxicities associated with agents that target CD19-expressing cells may be similar and possibly independent of the mechanism of T-cell activation. The long-term outcomes of these 3 patients illustrate that long-term survival after blinatumomab treatment may be achieved with no other subsequent treatment, even in relapsed ALL. One long-term survivor in this study who relapsed twice responded to retreatment with blinatumomab both times, suggesting that blinatumomab might be an alternative to chemotherapy for treatment of relapses in patients with r/r ALL after blinatumomab-induced CR followed by blinatumomab maintenance treatment.15 Additional research is required to confirm the activity and tolerability of blinatumomab retreatment in this setting. One patient without allo-SCT as consolidation for blinatumomab had a CD19-negative relapse and achieved another remission after chemotherapy. Blinatumomab might have prolonged the interval between chemotherapy regimens, thus possibly enhancing sensitivity to the subsequent chemotherapy. Larger data sets are needed to confirm this observation.
Long-term survivors (ie, MRD responders with OS ≥30 months) showed a higher degree of T-cell and TEM-cell expansion during treatment cycles 1 and 2. The data suggest that T-cell expansion might be a key factor for survival in the setting of r/r ALL. This is the first, albeit limited, data set to support this hypothesis; additional studies are needed to verify the observation. Prior blinatumomab data in patients with relapsed non-Hodgkin lymphoma have indicated dose-dependent effects mainly on peripheral blood, bone marrow, and lymph node B cell, whereas T-cell kinetics seemed less affected by blinatumomab dose.11 The onset of antileukemia responses after blinatumomab infusion occurs early during treatment, in most cases at the first assessment at the end of cycle 1. For nonresponders, additional cycles of treatment or an increased blinatumomab dose in the second cycle had little effect on improvement of antileukemia activity.9 In the current study, a dose increase to 30 µg/m2 per day at day 15 of the first cycle did not result in a higher CR rate (data not shown). These results suggest that although kinetics of peripheral B-cell depletion seem to be associated with achieving a complete molecular response (ie, MRD negativity), the degree of T-cell expansion might be important not only for remission but also for long-term OS. Long-term survival (OS ≥30 months) was associated with a larger and repeated T-cell expansion, as compared to only minor or even absent T-cell expansion with OS <30 months.
In conclusion, in this long-term follow-up analysis of an exploratory, dose-escalation phase 2 study of blinatumomab in adult patients with r/r B-precursor ALL, an MRD response to blinatumomab treatment was associated with significantly longer OS compared to OS in patients who did not achieve an MRD response. All of the long-term survivors had an MRD response. Long-term survivors also had greater T-cell expansion. The data suggest that long-term survival after blinatumomab treatment may be associated with an MRD response and potentially with a higher degree of T-cell expansion.
Acknowledgments
The authors thank Jonathan Latham (PharmaScribe), whose work was funded by Amgen; and Beate D. Quednau (Amgen) for editorial assistance in the preparation of this manuscript.
Footnotes
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: M.S.T., N.G., R.C.B., G.Z., and M.K. designed the research; N.G., M.K., A.V., M. Stelljes, S.N., H.-A.H., R.M., C.F., H.D., A.R., M.B., M. Schmidt, and M.S.T. performed the research; G.Z., H.-A.H., M.B., C.H., H.E., and R.C.B. analyzed the data; G.Z. and M.K. wrote the first draft of the paper; and all authors reviewed and contributed to the final paper.
Conflict-of-interest disclosure: N.G., M.B., and H.-A.H. have received research funding from Amgen. N.G., M.B., and R.C.B. have consulted for Amgen. N.G., H.-A.H., R.C.B., and M.S.T. have received honoraria from Amgen. A.V. and M.S.T. have served on advisory boards for Amgen. G.Z., M. Schmidt, and M.K. are employees of Amgen Research (Munich). C.H. is an employee of Amgen. G.Z., M. Schmidt, M.K., and C.H. are shareholders in Amgen. A.V. has served in advisory boards for Roche, Janssen, and Gilead; received honoraria from Pfizer and Roche; and received travel support from Roche, Pfizer, and Amgen. M. Stelljes, S.N., A.R., R.M., C.F., H.D., and H.E. declare no competing financial interests.
Correspondence: Gerhard Zugmaier, Amgen Research (Munich) GmbH, Staffelseestrasse 2, 81477 Munich, Germany; e-mail: gerhardz@amgen.com.
References
- 1.Tavernier E, Boiron JM, Huguet F, et al. GET-LALA Group; Swiss Group for Clinical Cancer Research SAKK; Australasian Leukaemia and Lymphoma Group. Outcome of treatment after first relapse in adults with acute lymphoblastic leukemia initially treated by the LALA-94 trial. Leukemia. 2007;21(9):1907–1914. doi: 10.1038/sj.leu.2404824. [DOI] [PubMed] [Google Scholar]
- 2.Oriol A, Vives S, Hernández-Rivas JM, et al. Programa Español de Tratamiento en Hematologia Group. Outcome after relapse of acute lymphoblastic leukemia in adult patients included in four consecutive risk-adapted trials by the PETHEMA Study Group. Haematologica. 2010;95(4):589–596. doi: 10.3324/haematol.2009.014274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fielding AK, Richards SM, Chopra R, et al. Medical Research Council of the United Kingdom Adult ALL Working Party; Eastern Cooperative Oncology Group. Outcome of 609 adults after relapse of acute lymphoblastic leukemia (ALL); an MRC UKALL12/ECOG 2993 study. Blood. 2007;109(3):944–950. doi: 10.1182/blood-2006-05-018192. [DOI] [PubMed] [Google Scholar]
- 4.Kantarjian HM, Thomas D, Ravandi F, et al. Defining the course and prognosis of adults with acute lymphocytic leukemia in first salvage after induction failure or short first remission duration. Cancer. 2010;116(24):5568–5574. doi: 10.1002/cncr.25354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gökbuget N, Stanze D, Beck J, et al. German Multicenter Study Group for Adult Acute Lymphoblastic Leukemia. Outcome of relapsed adult lymphoblastic leukemia depends on response to salvage chemotherapy, prognostic factors, and performance of stem cell transplantation. Blood. 2012;120(10):2032–2041. doi: 10.1182/blood-2011-12-399287. [DOI] [PubMed] [Google Scholar]
- 6.Nagorsen D, Baeuerle PA. Immunomodulatory therapy of cancer with T cell-engaging BiTE antibody blinatumomab. Exp Cell Res. 2011;317(9):1255–1260. doi: 10.1016/j.yexcr.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 7.Topp MS, Gökbuget N, Zugmaier G, et al. Phase II trial of the anti-CD19 bispecific T cell-engager blinatumomab shows hematologic and molecular remissions in patients with relapsed or refractory B-precursor acute lymphoblastic leukemia. J Clin Oncol. 2014;32(36):4134–4140. doi: 10.1200/JCO.2014.56.3247. [DOI] [PubMed] [Google Scholar]
- 8.Topp MS, Gökbuget N, Stein AS, et al. Safety and activity of blinatumomab for adult patients with relapsed or refractory B-precursor acute lymphoblastic leukaemia: a multicentre, single-arm, phase 2 study. Lancet Oncol. 2015;16(1):57–66. doi: 10.1016/S1470-2045(14)71170-2. [DOI] [PubMed] [Google Scholar]
- 9.Topp MS, Kufer P, Gökbuget N, et al. Targeted therapy with the T-cell-engaging antibody blinatumomab of chemotherapy-refractory minimal residual disease in B-lineage acute lymphoblastic leukemia patients results in high response rate and prolonged leukemia-free survival. J Clin Oncol. 2011;29(18):2493–2498. doi: 10.1200/JCO.2010.32.7270. [DOI] [PubMed] [Google Scholar]
- 10.National Cancer Institute. NCI common terminology criteria for adverse events (CTCAE) v4.0. Bethesda, MD: National Cancer Institute; 2010. NIH publication no. 09-5. [Google Scholar]
- 11.Bargou R, Leo E, Zugmaier G, et al. Tumor regression in cancer patients by very low doses of a T cell-engaging antibody. Science. 2008;321(5891):974–977. doi: 10.1126/science.1158545. [DOI] [PubMed] [Google Scholar]
- 12.Simon R, Makuch RW. A non-parametric graphical representation of the relationship between survival and the occurrence of an event: application to responder versus non-responder bias. Stat Med. 1984;3(1):35–44. doi: 10.1002/sim.4780030106. [DOI] [PubMed] [Google Scholar]
- 13.Kantarjian H, Thomas D, Jorgensen J, et al. Results of inotuzumab ozogamicin, a CD22 monoclonal antibody, in refractory and relapsed acute lymphocytic leukemia. Cancer. 2013;119(15):2728–2736. doi: 10.1002/cncr.28136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davila ML, Riviere I, Wang X, et al. Efficacy and toxicity management of 19-28z CAR T cell therapy in B cell acute lymphoblastic leukemia. Sci Transl Med. 2014;6(224):224ra25. doi: 10.1126/scitranslmed.3008226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Topp MS, Stelljes M, Zugmaier G, et al. Re-exposure to blinatumomab after CD19-positive relapse: experience from three trials in patients (pts) with relapsed/refractory B-precursor acute lymphoblastic leukemia (R/R ALL) [abstract]. J Clin Oncol. 2015:33. (Suppl). Abstract 7051. [Google Scholar]