To the editor:
Infusion-related reactions (IRRs) occur commonly with rituximab administration, a type-I anti-CD20 monoclonal antibody that is routinely used in the treatment of chronic lymphocytic leukemia (CLL).1,2 The pathophysiology of these reactions has been attributed to cytokine release with patients experiencing IRR found to release greater amounts of interleukin (IL) 8, IL-6, and tumor necrosis factor α (TNF-α) than those who did not and patients with baseline absolute lymphocyte count (ALC) ≥50 × 109/L at greatest risk of developing a reaction.2-4
Obinutuzumab is a humanized glycoengineered immunoglobulin G1 type-II anti-CD20 monoclonal antibody, with enhanced antibody-dependent cell-mediated cytotoxicity and phagocytosis, increased direct cell death, and lower complement activation compared with rituximab in vitro.5-7 These properties translated into improved clinical activity as demonstrated by the results of the CLL11 trial (#NCT01010061), and obinutuzumab plus chlorambucil has approval to treat patients with CLL and comorbidities as a result.8,9 The incidence and severity of IRR in CLL patients treated with obinutuzumab appears to be greater than observed with rituximab, and we sought to investigate whether the underlying pathophysiology echoed that of rituximab.
We analyzed IRR frequency and severity in a subset of 38 patients, the entire complement with an underlying diagnosis of CLL pooled from 2 phase-1/2 trials, GAUSS (#NCT00576758),10 and GAUGUIN (#NCT00517530).11 Study methods were as previously published.10,11 Patients were universally treated with obinutuzumab monotherapy and had frequent sequential blood samples taken. This enabled us to interrogate the association of IRR with patient baseline and tumor characteristics, peripheral blood leukocyte subsets, serum cytokine release, and complement activation.
Differences in baseline laboratory values and other variables between groups (severe IRRs vs nonsevere IRRs) were evaluated for statistical significance using the Student t test or Fisher’s exact test where appropriate. In addition, patients were retrospectively stratified into 2 groups according to ALC at baseline, those considered as having “low” levels of circulating disease (<50 × 109/L) and “high” levels of circulating disease (≥50 × 109/L). All P values are 2-sided with a level of significance at <.05.
Of the 38 patients investigated, 35 (92%) developed symptoms of IRR (grade 1/2, n = 25; grade 3/4, n = 10) with the first infusion, and IRR resulted in permanent treatment discontinuation in 3 (8%) patients. The median time to onset was shorter in the group that had severe (grade 3/4) reactions (30 minutes, range 5-180 minutes) compared with those with less severe reactions (51 minutes, range 5-440 minutes). Even small doses of obinutuzumab (as little as 9 mg) had the potential to elicit symptoms. However, the majority of patients (27/35) completed their first infusion on day 1 despite developing IRR.
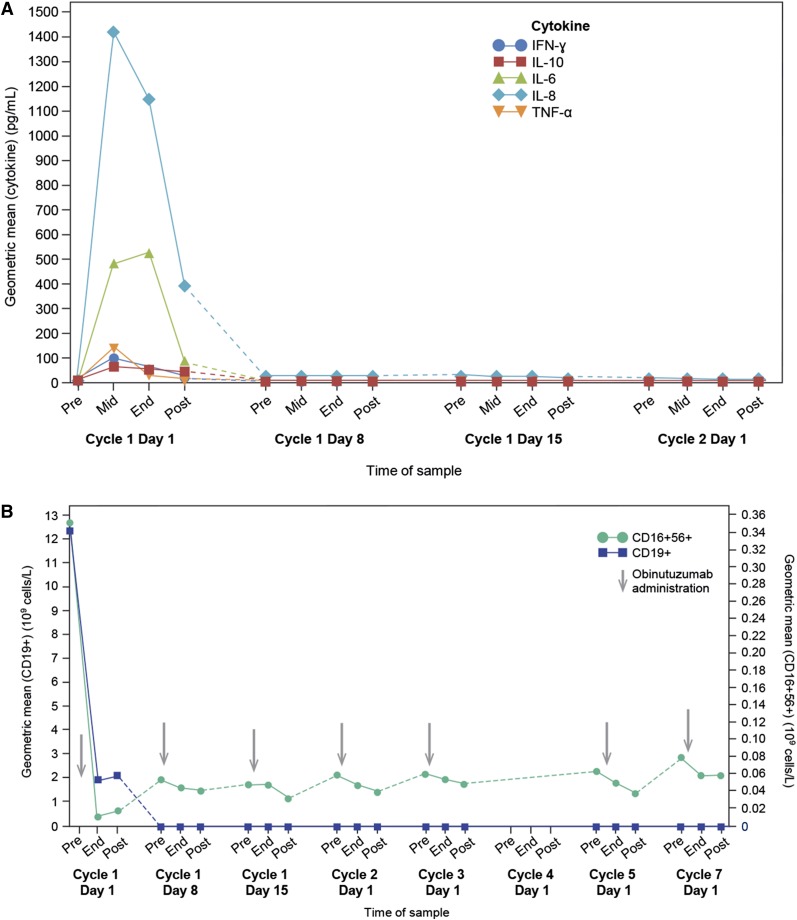
The initial obinutuzumab infusion was accompanied by a rapid decrease in circulating CD19+ B cells (−84% change from baseline to end of infusion), a decrease in the measurable circulating natural killer (NK) CD16+56+ cells (−97% change), as well as an increase of proinflammatory cytokines IL-6, IL-8, TNF-α, and interferon γ (Figure 1). Subsequent infusions of obinutuzumab did not induce significant cytokine release, nor were there any severe-grade IRRs observed beyond cycle 1.
Figure 1.
Effects of obinutuzumab administration on cytokine release patterns, ALC, and circulating NK cells. (A) Cytokine release observed pre-, mid-, end-, and postadministration of obinutuzumab observed in n = 38 CLL patients. (B) Changes in circulating CD19+ B cells (y-axis left) and CD16+56+ NK cells (y-axis right) pre-, end-, and postadministration of obinutuzumab observed in n = 38 CLL patients.
Although the number of patients studied is small, there were statistically significant differences in baseline ALC (when analyzed as a continuous variable; P = .02) and baseline thrombocytopenia (P = .02), with those patients who had a severe-grade event more likely to have higher ALC and lower platelet count compared with those patients who had a nonsevere reaction. When patients were dichotomized into those with ALC <50 × 109/L vs those with ALC ≥50 × 109/L at baseline, the resultant loss of information meant that the increased risk of severe-grade IRR for those in the high ALC group did not achieve conventional statistical significance, with a P value of .06. Patients who had grade 3 or greater reactions also appeared to have had higher baseline values in parameters of tumor burden, nodal disease, thymidine kinase, β-2 microglobulin, and splenomegaly. However, none of these differences reached statistical significance.
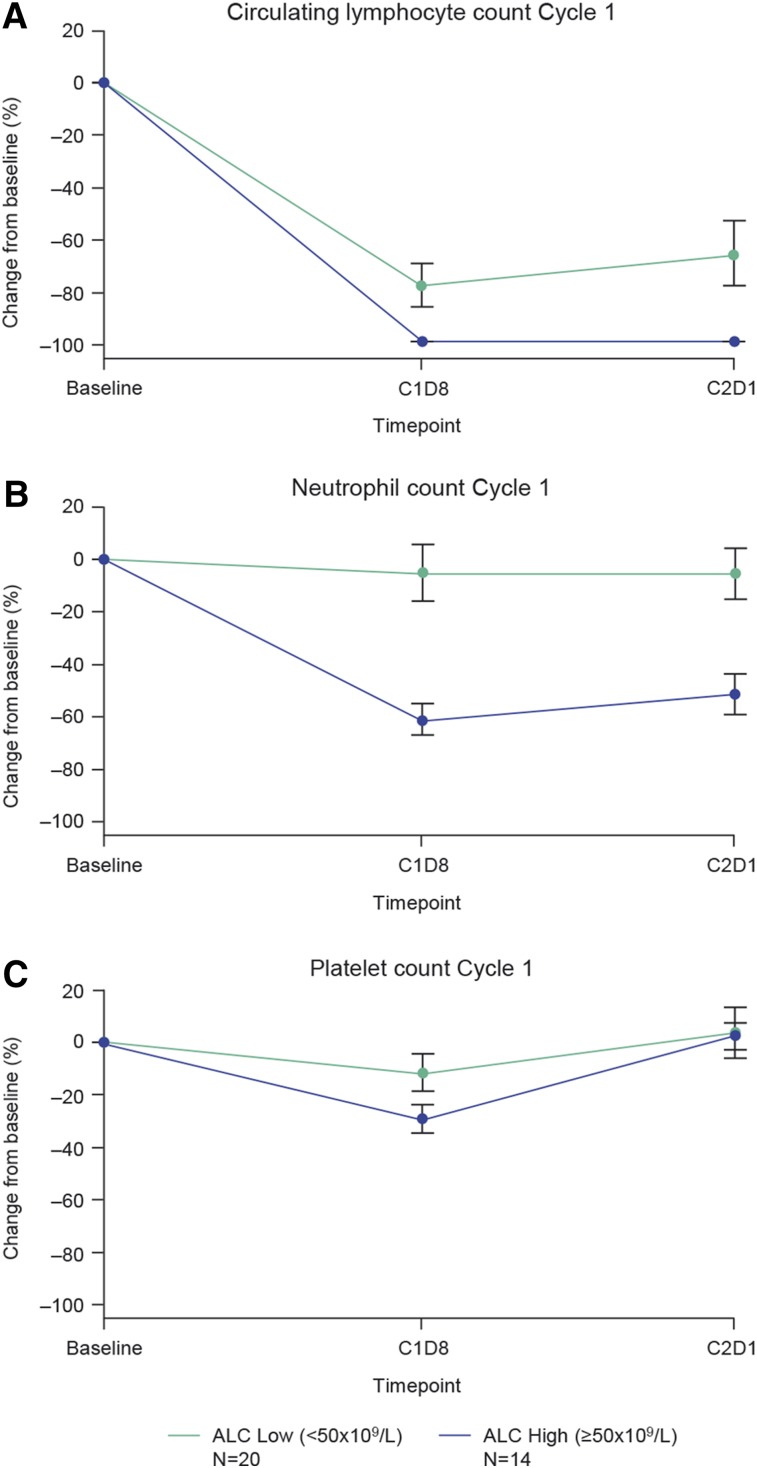
At the midinfusion time point, patients with preinfusion ALC ≥50 × 109/L released more proinflammatory cytokines, in particular IL-6 (mean IL-6 [log10] 3.16 vs 2.41) and IL-8 (mean IL-8 [log10] 3.57 vs 2.91) than those with ALC <50 × 109/L. In addition, those patients with higher pretreatment ALC developed more pronounced decreases in their neutrophil and platelet counts at day 8 when compared with those with lower levels of circulating disease (Figure 2). Markers of complement activation, C5a and C3a, did not increase nor was there consumption of C3/C4 levels.
Figure 2.
First cycle cytopenias observed in patients with high vs low ALC at baseline. Mean percentage change in circulating lymphocyte (A), neutrophil (B), and platelet (C) counts observed during cycle 1 in patients with high (≥50 × 109/L) and low (<50 × 109/L) baseline ALC values.
Do these results provide new insight into the pathophysiology and possible intervention strategies that could be exploited to prevent IRR? IL-8 is a proinflammatory chemokine that acts as a chemotactic factor for neutrophils, T cells, eosinophils, and NK cells.12 Elevated serum concentrations have been noted in CLL13 and correlate with advanced disease. However, IL-8 is required for effector cell migration and triggers several mechanisms required for phagocytosis14; thus, inhibiting this key cytokine may not be advantageous. In fact, CLL-secreted IL-8 appears to be required as a cofactor to maximize NK-mediated antibody-dependent cell-mediated cytotoxicity,15 although this effect was more pronounced for those cells treated with rituximab than obinutuzumab.
Given the known biological properties of IL-6, with elevated levels causing hypotension, vascular leakage, tissue edema, and hypoxia,16 it might prove a more appropriate target to inhibit or prevent severe IRR. Patients treated with recombinant IL-6 developed a clinical syndrome very similar to IRR, with pyrexia, headaches, flushing, and rigors.17 Dexamethasone has been shown to inhibit both IL-6 and IL-6 receptor gene expression,18 and this may explain the partial efficacy of steroid premedication in reducing the incidence and severity of IRR observed in the CLL11 trial.8 Furthermore, blockade of IL-6 receptor with tocilizumab sensitized cells in vitro to the cytotoxic action of chlorambucil19; thus, the benefits of inhibiting this pathway in CLL may not be limited to the prevention of IRR.
First-cycle thrombocytopenia attributable to rituximab has been reported in up to 30% of patients for any grade and 20% for severe grades.20 Risk factors include high levels of circulating disease, higher levels of CD20 expression, the presence of splenomegaly, and bone marrow infiltration.4,20 Many of these were also recently identified as risk factors for the development of IRR with anti-CD20 monoclonal administration in CLL.21 In our pooled cohort, cycle-1 thrombocytopenia was observed in 25/38 patients, with severe grades in 8/38 (21%). This may result from an endothelial-mediated process or margination, as both TNF-α22 and IL-623 in particular can induce expression of endothelial adhesion molecules. Acute leukopenia has also been described in response to rituximab administration, in particular in patients who experienced symptoms of cytokine release.24 Thus, the increased incidence of grade 3 or greater neutropenia (obinutuzumab 14% vs rituximab 9%) and thrombocytopenia (obinutuzumab 11% vs rituximab 3%) observed during the first cycle in the CLL11 trial may relate to the fact that the cytokine release induced by obinutuzumab appears to be quantitatively different from rituximab.5,8 This too may explain the differences in IRRs observed between the 2 arms in this trial.
In conclusion, the administration of obinutuzumab to patients with CLL triggered immediate and marked release of cytokines, in particular IL-6 and IL-8, which was limited to the first infusion and accompanied by rapid destruction of circulating B cells, by decrease in circulating NK cells, and, in the majority of patients, by signs and symptoms suggestive of IRR. Patients with higher levels of circulating disease at baseline appear more likely to develop associated cytopenias with cycle 1. Intervention strategies that target these proinflammatory cytokines may be promising to reduce the incidence and severity of IRR with obinutuzumab and are currently being explored in clinical trials (#NCT01905943 and #NCT02336048).
Authorship
Acknowledgments: This research was sponsored by F. Hoffmann-La Roche Ltd. Statistical and programming support was provided by Ute Dickschat, Renate Scheiner-Sparna, and Rosie Brown. Professor Michael Hallek is supported by the Deutsche Forschungsgemeinschaft (KFO 826, TP6). Martin Quinn (Gardiner-Caldwell Communications, Macclesfield, United Kingdom), a medical writer supported by funding from F. Hoffmann-La Roche Ltd., provided figure formatting and journal styling support only to the authors during preparation of this manuscript.
Contribution: C.L.F., G.F.-R., and M.D. designed the research; C.L.F. and M.D. performed the research; F.M., T.L., G.C., L.S., M.H., and G.S. collected the data; C.L.F., M.D., R.H., G.F.-R., E.W.-F., and J.G.G. analyzed and interpreted the data; M.D. performed the statistical analysis; C.L.F wrote the manuscript; and all authors reviewed the manuscript and approved the final version.
Conflict-of-interest disclosure: C.L.F. has received research funding from F. Hoffmann-La Roche Ltd., honoraria from F. Hoffmann-La Roche Ltd. and Gilead Sciences, and other remuneration (travel, accommodation, and expenses) from Chugai Pharmaceutical Co. Ltd., F. Hoffmann-La Roche Ltd., and NAPP Pharmaceutical Group Ltd. F.M. has received honoraria for scientific speeches (not Speaker’s Bureau) from Mundipharma, Gilead Sciences and Spectrum Pharmaceuticals; honoraria for advisory boards from Mundipharma, Gilead Sciences, Spectrum Pharmaceuticals, and Bayer; and a travel grant from Genentech Inc. L.S. has received consultancy fees and honoraria from F. Hoffmann-La Roche Ltd./Genentech Inc., Celgene Corporation, Gilead Sciences, Pfizer Inc., Amgen Inc., Janssen-Cilag Ltd., and Lundbeck Ltd., and research funding from F. Hoffmann-La Roche Ltd. M.D. and R.H. are employees of Roche Products Ltd., and G.F.-R. and E.W.-F. are employees of F. Hoffmann-La Roche Ltd. M.D. and G.F.-R. have stock ownership in Roche, which is publicly traded. J.G.G. has received honoraria from Celgene Corporation, Gilead Sciences, F. Hoffmann-La Roche Ltd., Janssen-Cilag Ltd., and Pharmacyclics LLC, and other remuneration (travel, accommodation, and expenses) from Gilead Sciences. M.H. has received consultancy fees and research funding from, and has served on a Speaker’s Bureau for, F. Hoffmann-La Roche Ltd. G.S. has received consultancy fees from F. Hoffmann-La Roche Ltd./Genentech Inc., Celgene Corporation, Gilead Sciences, Janssen-Cilag Ltd., and Mundipharma; honoraria from F. Hoffmann-La Roche Ltd./Genentech Inc., Amgen Inc., Mundipharma, and Sanofi; and research funding and other remuneration (travel and expenses) from F. Hoffmann-La Roche Ltd. G.C. has received consultancy fees from F. Hoffmann-La Roche Ltd. and honoraria from F. Hoffmann-La Roche Ltd., GlaxoSmithKline, Gilead Sciences, Jansen-Cilag Ltd., and Sanofi. T.L. declares no competing financial interests.
Correspondence: Ciara Freeman, Barts Cancer Institute, 3rd Floor John Vane Science Centre, Charterhouse Square, London, United Kingdom; e-mail: c.freeman@qmul.ac.uk.
References
- 1.Hallek M. Chronic lymphocytic leukemia: 2015 update on diagnosis, risk stratification, and treatment. Am J Hematol. 2015;90(5):446–460. doi: 10.1002/ajh.23979. [DOI] [PubMed] [Google Scholar]
- 2.Byrd JC, Murphy T, Howard RS, et al. Rituximab using a thrice weekly dosing schedule in B-cell chronic lymphocytic leukemia and small lymphocytic lymphoma demonstrates clinical activity and acceptable toxicity. J Clin Oncol. 2001;19(8):2153–2164. doi: 10.1200/JCO.2001.19.8.2153. [DOI] [PubMed] [Google Scholar]
- 3.Byrd JC, Waselenko JK, Maneatis TJ, et al. Rituximab therapy in hematologic malignancy patients with circulating blood tumor cells: association with increased infusion-related side effects and rapid blood tumor clearance. J Clin Oncol. 1999;17(3):791–795. doi: 10.1200/JCO.1999.17.3.791. [DOI] [PubMed] [Google Scholar]
- 4.Winkler U, Jensen M, Manzke O, Schulz H, Diehl V, Engert A. Cytokine-release syndrome in patients with B-cell chronic lymphocytic leukemia and high lymphocyte counts after treatment with an anti-CD20 monoclonal antibody (rituximab, IDEC-C2B8). Blood. 1999;94(7):2217–2224. [PubMed] [Google Scholar]
- 5.Golay J, Da Roit F, Bologna L, et al. Glycoengineered CD20 antibody obinutuzumab activates neutrophils and mediates phagocytosis through CD16B more efficiently than rituximab. Blood. 2013;122(20):3482–3491. doi: 10.1182/blood-2013-05-504043. [DOI] [PubMed] [Google Scholar]
- 6.Mössner E, Brünker P, Moser S, et al. Increasing the efficacy of CD20 antibody therapy through the engineering of a new type II anti-CD20 antibody with enhanced direct and immune effector cell-mediated B-cell cytotoxicity. Blood. 2010;115(22):4393–4402. doi: 10.1182/blood-2009-06-225979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patz M, Isaeva P, Forcob N, et al. Comparison of the in vitro effects of the anti-CD20 antibodies rituximab and GA101 on chronic lymphocytic leukaemia cells. Br J Haematol. 2011;152(3):295–306. doi: 10.1111/j.1365-2141.2010.08428.x. [DOI] [PubMed] [Google Scholar]
- 8.Goede V, Fischer K, Busch R, et al. Obinutuzumab plus chlorambucil in patients with CLL and coexisting conditions. N Engl J Med. 2014;370(12):1101–1110. doi: 10.1056/NEJMoa1313984. [DOI] [PubMed] [Google Scholar]
- 9.Goede V, Fischer K, Engelke A, et al. Obinutuzumab as frontline treatment of chronic lymphocytic leukemia: updated results of the CLL11 study. Leukemia. 2015;29(7):1602–1604. doi: 10.1038/leu.2015.14. [DOI] [PubMed] [Google Scholar]
- 10.Sehn LH, Assouline SE, Stewart DA, et al. A phase 1 study of obinutuzumab induction followed by 2 years of maintenance in patients with relapsed CD20-positive B-cell malignancies. Blood. 2012;119(22):5118–5125. doi: 10.1182/blood-2012-02-408773. [DOI] [PubMed] [Google Scholar]
- 11.Cartron G, de Guibert S, Dilhuydy MS, et al. Obinutuzumab (GA101) in relapsed/refractory chronic lymphocytic leukemia: final data from the phase 1/2 GAUGUIN study. Blood. 2014;124(14):2196–2202. doi: 10.1182/blood-2014-07-586610. [DOI] [PubMed] [Google Scholar]
- 12.Nyhlén K, Gautam C, Andersson R, Srinivas U. Modulation of cytokine-induced production of IL-8 in vitro by interferons and glucocorticosteroids. Inflammation. 2004;28(2):77–88. doi: 10.1023/b:ifla.0000033023.76110.51. [DOI] [PubMed] [Google Scholar]
- 13.Kara IO, Sahin B, Gunesacar R. Expression of soluble CD27 and interleukins-8 and -10 in B-cell chronic lymphocytic leukemia: correlation with disease stage and prognosis. Adv Ther. 2007;24(1):29–40. doi: 10.1007/BF02849990. [DOI] [PubMed] [Google Scholar]
- 14.Walz A, Meloni F, Clark-Lewis I, von Tscharner V, Baggiolini M. [Ca2+]i changes and respiratory burst in human neutrophils and monocytes induced by NAP-1/interleukin-8, NAP-2, and gro/MGSA. J Leukoc Biol. 1991;50(3):279–286. doi: 10.1002/jlb.50.3.279. [DOI] [PubMed] [Google Scholar]
- 15.Laprevotte E, Ysebaert L, Klein C, et al. Endogenous IL-8 acts as a CD16 co-activator for natural killer-mediated anti-CD20 B cell depletion in chronic lymphocytic leukemia. Leuk Res. 2013;37(4):440–446. doi: 10.1016/j.leukres.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 16.Krüttgen A, Rose-John S. Interleukin-6 in sepsis and capillary leakage syndrome. J Interferon Cytokine Res. 2012;32(2):60–65. doi: 10.1089/jir.2011.0062. [DOI] [PubMed] [Google Scholar]
- 17.Gordon MS, Nemunaitis J, Hoffman R, et al. A phase I trial of recombinant human interleukin-6 in patients with myelodysplastic syndromes and thrombocytopenia. Blood. 1995;85(11):3066–3076. [PubMed] [Google Scholar]
- 18.Trikha M, Corringham R, Klein B, Rossi JF. Targeted anti-interleukin-6 monoclonal antibody therapy for cancer: a review of the rationale and clinical evidence. Clin Cancer Res. 2003;9(13):4653–4665. [PMC free article] [PubMed] [Google Scholar]
- 19.Liu F, Jia L, Wang P, Farren T, Agrawal S. Tocilizumab overcomes chemo-resistance of CLL cells [abstract]. Blood. 2013;122(21) Abstract 5305. [Google Scholar]
- 20.Giezen TJ, Mantel-Teeuwisse AK, ten Berg MJ, et al. Rituximab-induced thrombocytopenia: a cohort study. Eur J Haematol. 2012;89(3):256–266. doi: 10.1111/j.1600-0609.2012.01808.x. [DOI] [PubMed] [Google Scholar]
- 21.Freeman CL, Dixon M, Houghton R, et al. Risk factors associated with the development of infusion-related reactions in patients with chronic lymphocytic leukaemia treated with anti-CD20 monoclonal antibodies: analysis of the CLL11 study dataset [abstract]. Blood. 2014;124(21) Abstract 3339. [Google Scholar]
- 22.Xia P, Gamble JR, Rye K-A, et al. Tumor necrosis factor-alpha induces adhesion molecule expression through the sphingosine kinase pathway. Proc Natl Acad Sci USA. 1998;95(24):14196–14201. doi: 10.1073/pnas.95.24.14196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mihara M, Hashizume M, Yoshida H, Suzuki M, Shiina M. IL-6/IL-6 receptor system and its role in physiological and pathological conditions. Clin Sci (Lond) 2012;122(4):143–159. doi: 10.1042/CS20110340. [DOI] [PubMed] [Google Scholar]
- 24.Ram R, Bonstein L, Gafter-Gvili A, Ben-Bassat I, Shpilberg O, Raanani P. Rituximab-associated acute thrombocytopenia: an under-diagnosed phenomenon. Am J Hematol. 2009;84(4):247–250. doi: 10.1002/ajh.21372. [DOI] [PubMed] [Google Scholar]