Abstract
Background:
The major objectives of this study were to evaluate the existing primary health care service provisions in the public and private sector and utilization of the services, and to assess the existing manpower and material resources.
Methods:
Data were collected through interviews with the primary health care providers. Data were also collected from the records maintained at the polyclinics and the Ministry of Health Statistics. An analysis and discussion of all the available data was conducted to develop a comprehensive primary health care service utilization and resources inventory at the polyclinics. Similar data were collected from the primary care providers in the private sector.
Results:
In the public sector, there are 8 polyclinics that provide primary health care to the children. All the polyclinics have immunization services and curative acute care. Some of the polyclinics have a range of services, including dental care, eye care, and rehabilitative care services that common to both adults and children. In the private sector, primary health care is delivered through the 76 private office and of the individual physicians and 11 grouped private practices. All of the private offices and group practices have curative acute care for children and some of the offices have immunization services. Over all 87.5% of all the immunizations were done at the polyclinics. Over all 60.1% of acute care visits were to the private sector and 39.9% to the public sector. In the public sector, 59.5% were under 5 years children while 40.5% were 5 years or older. The corresponding figures in the private care settings were 80.9% and 11.9%.
Conclusions:
The findings demonstrate the complimentary role of the public and the private sector in the primary health care of children in this country. While the private sector has a major role in the curative acute care of children, the public sector plays a pivotal role in the immunization services.
Keywords: Children, pluralistic health care setting, primary health care
INTRODUCTION
Barbados, one of the English speaking Caribbean countries, has both public and private facilities providing health care to its population. There is a comprehensive publicly funded (tax-funded) and delivered health care, including the primary health care and tertiary health care at the hospital, prescription drugs and some dental care.[1] A range of primary health care services including both the curative care and preventative care are delivered through a chain of tax-funded polyclinics across the country and are free of any charges for all of its citizens at the point of delivery.[2,3] There is a single tax-funded tertiary care hospital in this country which provided the entire range of free inpatient care including investigations and medications to all its citizens. Barbadians also have a choice of availing private health care services, on payment, available through the individual physicians’ private office or group private offices spread over the entire country.[4]
An accumulating literature documents the importance of a strong primary care infrastructure within a health services system especially in the context of the changing health care needs of children.[5,6,7,8] Health systems that are better organized around a primary care base achieve better health outcomes and greater population satisfaction at lower costs than health systems more focused on specialty services.[5] In the United States, areas with more primary care physicians have lower rates of hospitalization for conditions that are sensitive to primary care interventions,[6] lower death rates from major causes,[7] and lower infant mortality.[7] A recent report by the Institute of Medicine, USA, reinforces the importance of strong primary care as a critical feature of the health services system.[8,9,10,11,12,13,14]
Commitment by the government of Barbados for ensuring equitable distribution and continuous improvement in the quality affordable primary health care to all its citizens in the face of economic constrains is an ongoing policy concern. The relative role of the public and the private health care providers in the primary health care of children in this country has never been explored. In this operational research study, we critically examine the available resources in the public and the private primary health facilities in this country. We describe the utilization of the public and the private facilities by the children of this country including the demographics of the children utilizing the public primary health care facilities as well as the profile of the presenting illnesses. The report highlights the strength and challenges of public funded and the private health care provisions. These information will be necessary for making any policy decisions for further strengthen the public primary pediatric care in this country.
METHODS
The majority of the data for this paper was drawn from the reports of a professional consultancy service commissioned by the Ministry of Health (MOH), Government of Barbados to strengthen the primary health care for the children at its health centers – the polyclinics. As a part of this initiative, a need assessment survey of all the polyclinics across this country was undertaken. The major objectives of this need assessment were to evaluate the existing health care service provisions and its utilization and to assess the existing manpower and material resources at these Polyclinics. Data were also collected from the private sector primary care setting which included private offices of individual or group of doctors. Data from emergency care settings of both the public sector and the private sector were excluded.
All of data pertained to the year 2012. Data collection involved multiple methods and used multiple sources. The lead consultant visited all of the polyclinics and met individually as well as collectively with the medical and the nursing staff at the polyclinics. The Medical Officer of Health and the Senior Public Health Nurse, who are responsible for the overall management of the 8 polyclinics in this country were interviewed using a semi-structured questionnaire. Several open ended questions were used to facilitate open discussions on the various issues in the context of pediatric services at these polyclinics. Interviews covered all aspects of the pediatric primary care delivery and the existing infrastructure for the delivery. A total of 36 physicians and 41 nurses were interviewed in 8 sessions. Data on service utilization was collected form the annual reports form the polyclinics. Doctors engaged in private practice and who provided primary care were identified form the listing of the registered medical practitioners in this country. Data form the private sector primary care providers were collected by telephonic call to the offices.
The data collected from the polyclinics included the data on the available resources such as the number of physicians and nurses attending to children, availability of other support medical team such as nutritionist, physiotherapist, speech therapist, psychologist, and medical social workers. Data were also collected on the available services in term or curative care services, preventative care services, and rehabilitative services. A number of available hours available for these services were also collected. A third category of collected data included service utilizations such as number and demographics of children attending the well-baby and immunization clinic, acute care clinic and any follow-up clinics. Profile of the diagnosis for the children attending the polyclinics was also collected. Similar data were collected from the private office of the general practitioner's (GP's) (doctors with MBBS as their highest medical degree) and the pediatricians who provided primary care to children in the private settings.
An analysis and discussion on all the available data was conducted to develop a comprehensive community health care service utilization and resources inventory, to identify the needs in the priority area for improving and strengthening the primary pediatric care at the polyclinics.
Total available professional manpower hours were calculated using the following formulae:
Total available physician hours = P × 5 × 7× 0.85
P = Number of persons available for professional duties
(MOH were counted as 0.5 due to the fact that they have administrative duties assigned to them, which takes up nearly half of their working time)
Working days a week = 5 days.
Daily work time of 8 h a day − 1 h breaks for lunch = 7 h.
Effective work time factor = 0.85 (The proportion of working time actually spent at work after subtracting the 0.15 or 15% of the time is lost to vacation 6 weeks a year and sick leave 2 weeks a year for each of the physicians at the polyclinics).
Data were stored in a password protected Microsoft® access database and were analyzed using Microsoft Excel for generation of tables and graphs. Proportion and 95% confidence interval (CI) were calculated using binomial distribution and results were corrected for continuity. Crude odds ratios and their cornfield 95% CIs were calculated. Associations between categorical variables will be assessed for statistical significance by Chi-square test. A P value of 0.05 will be considered to be statistically significant.
RESULTS
The total population of Barbados is 287,733 with an under 16 year's population of 58,455, according to the 2012 census. In the public sector, there are 8 polyclinics and 2 satellite health centers spread across the length and breadth of this island state that provide primary health care to the children as well as the adults of this country. The polyclinics have a range of services including well child health clinic, antenatal clinic, and the general practice clinics (for both the children and the adults), whereas the satellite centers only have general practice clinics with limited services (for both the children and the adults). In the private sector, primary health care is delivered through the 76 private office (57 GPs and 19 pediatricians) of the individual physicians and 11 (9 GPs and 3 pediatricians) grouped private practices.
Table 1 shows the range and the quantity of primary health care services for children that are available in the public sector (at the polyclinics and the satellite centers) and in the private sector in Barbados. All 8 polyclinics have immunization/well children clinic which is the only service entirely dedicated to child health. These clinics are managed by the Public Health Nurses and provide immunizations covered under the expanded immunization program as well routine growth and development assessment for children under 5 years. Each of the polyclinics and the satellite centers have daily GP Clinics, where children of all ages are attended to by GP's. Although, the GP clinics attend to both adults and children, there is a dedicated physician for children. Nutritionist's services are available at all of the 8 polyclinics but 1; however, there is no dedicated nutritionist service for children and the nutritionists attend to both the adults and children when referred to that service. Analysis of their attendance register revealed that 20% of the clients were children. Other services include dental services and eye care services that also serves all ages. Rehabilitative services such as physiotherapy, occupational therapy, and speech therapy are available at two of the polyclinics on three-half days a week at each. Children from other polyclinics are referred to a centralized children's development center. There are no dedicated follow-up clinics for chronic diseases in children except for an asthma clinic at one of the polyclinics. There is no pediatric/specialist service of any kind (except the basic general nutritional, dental, and eye services mentioned above) available at any of the polyclinics. Where a specialist consultation is necessary, patients are referred to the Pediatric Department at Queen Elizabeth Hospital (QEH) for appointment. There is provision for home visits at all of the polyclinics; however, most of these polyclinics are able to provide only 48% (2464 requests in 2011, 1173 visits made) of the desired home visits for newborns. All of the polyclinics have a public pharmacy for dispensing medications prescribed by the physicians at the polyclinics free of any charges. None of the polyclinics have laboratory support for routine investigations. Whenever an investigation is necessary on a patient attending the polyclinics, then sample is collected and sent to the laboratory attached to the publicly funded QEH.
Table 1.
Primary care services for children in the public and the private sector in Barbados
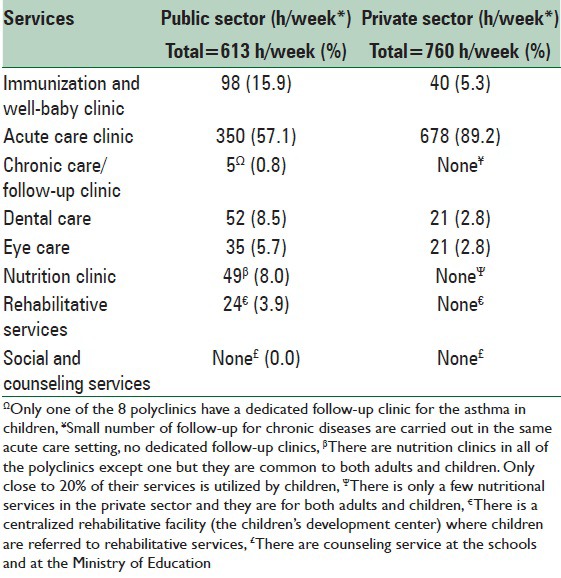
In the private sector, all GP's in addition to the pediatricians provide primary care to the children. In all of the GP's practice, both individual and group practice, both the adult and pediatric services are clubbed together and no separate records are maintained. Analysis of the records showed that on an average 21.2% (range: 11.4–30.7%) of the services were utilized by children. Only 51.9% of GP's provided immunization services while all of them provide acute care services to children and none provided any other services for children. In case of the pediatricians, all of them provided immunization/well child services, acute care services and follow-up services for chronic diseases; however, there were no dedicated time slot for these different services except for a dedicated immunization clinic at 4 of the pediatrics private offices. No other primary care services for children such as nutrition, rehabilitation, eyes, or dental services were available through any of the pediatrician's offices, although the nutritional, eye, and dental services could be obtained in the private offices of dentists and ophthalmologists on referral.
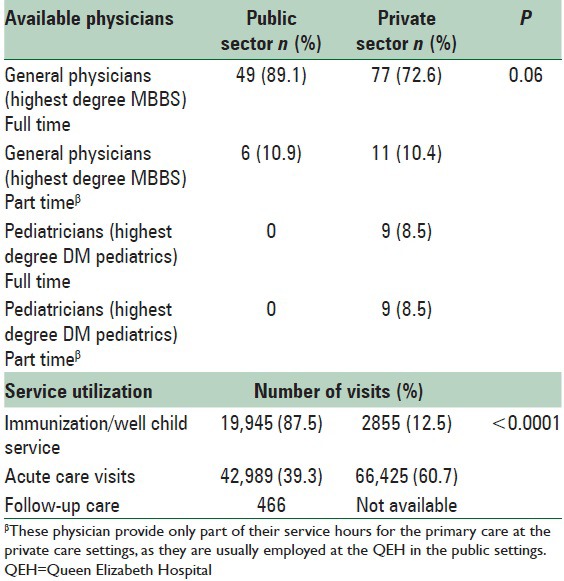
Available physicians and service utilization for the primary health care of children in the public sector and the private sector in Barbados is shown in Table 2. Of the 322 medical doctors providing direct clinical care in the community in this country, 144 (44.72%) are GPs (with their highest medical degree being MBBS). While in the public sector all of the GP's are assigned to see children from time to time, only 88 of the GP's in the private see children in their practice. The majority (49/55 = 89.1%) of the physicians in the public sector working at the polyclinics are full time (they do not hold any other employment). Many of the physicians (29/106 = 27.4%) especially the pediatricians (9/18 = 50%) in the private sector are part time in that they are also employed in the public sector health care settings (mainly at the QEH) in some capacity. Over all 87.5% (95% CI = 87.0%, 87.9%) of all the immunizations were done at the polyclinics in the public sector. Of the 109,414 estimated acute care visits from children to the primary care settings in Barbados, 60.7% (95% CI = 60.4%, 61.0%) were to the private office of the physicians in the private sector. Only follow-up service available and utilized in the primary care settings were those for asthma at one of the polyclinics in the public sector and amounted to 466 visits for the year 2011.
Table 2.
Available physicians and primary care service utilization in the public and the private sector in Barbados
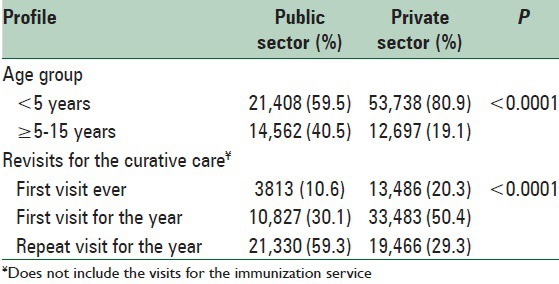
Profile of the clients visiting the primary care settings of the public sector and the private sector is shown in Table 3. In the public sector, 21,408 (59.5%; 95% CI = 59.0%, 60.0%) were under 5 years children while 14,562 (40.5%; 95% CI = 40%, 41%) were 5 years or older. The corresponding figures in the private care settings were 53738 (80.9%; 95% CI = 80.6%, 81.2%) and 12697 (19.1%; 95% CI = 18.8%, 19.4%). These differences were statistically significant (P < 0.0001). While 21,333 (59.3%; 95% CI = 58.8%, 59.8%) children in the public sector were repeat visitors for the year, 19,465 (29.3%; 95% CI = 28.9%, 29.6%) of those visiting the private sector were repeat visitors for the year. Once again these differences in the proportion of visits that were repeat visits for that year were statistically significant (P < 0.0001). In the private sector, 31.4% of children attending for care had a health insurance. In all these cases, the health insurance to pay for the care by assigning the benefits to the physician at the time of the care and just paying the 20% of the total cost upfront or they paid the whole cost upfront and then the insurance reimbursed 80% of the approved cost. Similar data were available from the public sector.
Table 3.
Profile of clients visiting the primary health care settings of the public sector and the private sector in Barbados
The diagnoses profile for the children seen at the primary care setting of the public and the primary sector is shown in Figure 1. Upper respiratory tract infection was the commonest over all diagnosis (31% among <5 children and 20% in children aged 5 or more) for children visiting the polyclinics. The second commonest (18% in <5 children and 8% in children aged 5 or more) reason for visit to the Polyclinics was for issue of health certificates for healthy children going back to day care centers, preschool and schools. Although the asthma (4.8%) and other allergic disorders such as the atopic dermatitis (4.6%) and allergic rhinitis (2.4%; clubbed in the “others” category) accounted for just 11.8%, 80.2% were revisits for the year and 47.3% had more than 2 visits for the year.
Figure 1.
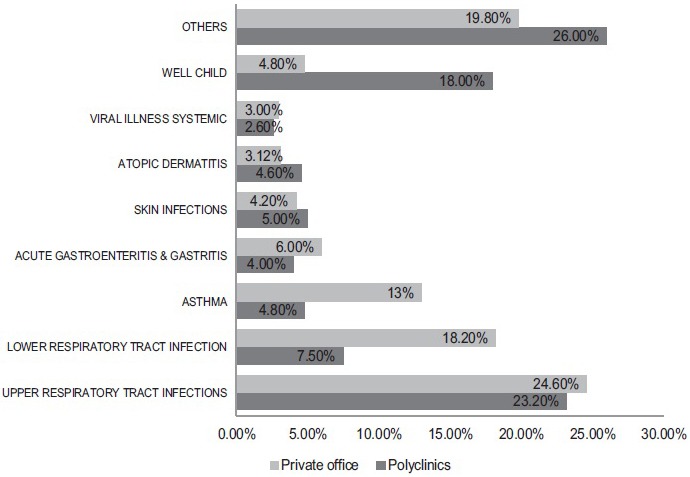
Diagnosis profile of children attending the primary health care setting of the private and the public sector in Barbados, year 2012
DISCUSSION
The most easterly Island in the Caribbean, Barbados, is a small, densely populated, English speaking country, with an estimated 287,733 people (2012 estimated) inhabiting its 431 km2.[15] Its Gross National Income per capita is US$ 25670 (2012) and its total expenditure on health as a percentage of GDP stands at 6.3% (2012). In 2011, Barbados was designated as a developed country by the United Nations Development Program, with a Human Development Index score of 0.793.[16] Very recent estimates place life expectancy at birth as 75 male/81 female years, and the infant mortality rate as 13.3/1000 live births.[15] Under-five mortality sits at 14/1000 live births for both sexes.[15] Barbados has a pluralistic health care system whereby people have a choice to utilize the health services in the public sector free of charges at the point of delivery or in the private sector at a fee that is out of pocket or through a number of the health care insurance schemes available. Less than a fourth of Barbadians have private health insurance coverage.[4] The insurance payment can be assigned to the insurance company at the time of service or paid upfront by the client who later get it reimbursed from their insurance. The public health care system has historically been the largest providers of primary health care in this country.[17,18,19] All of the physicians in the public sector have MBBS degree (addressed as GP's in this country), some of these physicians also have additional degree in public health. There is almost a parallel system of primary health care for children being provided by the physician in the private medical sector which includes GP's (physicians with MBBS degree and a further degree in General Practice or Family Medicine), pediatricians (physicians with MBBS degree and a further degree in pediatrics) and the physicians with just the basic MBBS degree who are addressed as GP's as well.[17,18,19]
The available total number of hours of primary care services (including both the public sector and the primary sector) for children in Barbados stands at 1171 h/week or 5074.3 h/month [Table 1]. This figure translates into 15,223 consultation visits given a consultation time of 20 min/month.[20,21] Utilization of health services as most papers define it, visits/1000 children per month. Given the under 16 population of Barbados at 58,455, the available services for primary care for children can accommodate 260.4 visits/1000 children. Japan with a socialized system is the utilization of primary health services is at 167/1000 children,[22] same figure as reported in the US.[23] Based on the published literature the round figure of 185 visits/month/1000 children could be considered as a reasonable “standard” demand.[22,23] When these figures on primary care utilization by children is applied to Barbados with <16 years population of 58,455, this country has a monthly demand of 10,822 visits from children. Therefore, the available service resources (15,223 consultation visits/month) exceed the projected service demand (10,822 consultation visits/month).
The proportion (144/322 = 44.7%) of all registered physicians who provide primary health care in this country is higher than 32% reported from the North America[24] and the Organization for Economic Cooperation and Development average of 26.9%.[25] This imbalance between the available physicians for primary care and specialty care will have to be address in order to strengthen the primary health care in this country. While none of the physicians in the public sector providing the primary care to the children are pediatrician, only one-sixth of the physicians in the private sector providing primary care to children are pediatrician. Therefore, the majority of the primary health care for children is provided by the GP's. The research on the need and the role of pediatrician in primary health care of children have been inconsistent.[26,27,28,29,30,31,32] Research seems to suggest that additional specialization by pediatricians translates into a unique practice style that may ultimately result in more efficient or effective care under certain circumstances.[31,33] However, it is unclear whether the exclusive focus on children, rather than families, causes pediatricians to offer less holistic or comprehensive services than those provided by family practitioners. What is obvious from this audit is that despite the lack of qualified pediatrician's service at the primary care level, the child health indicators such as the infant mortality rate and the under-five mortality rate in this country compares well with those of developed countries in the Americas.[15]
The majority of the available primary care services, however, are for the immunization and acute curative care. There is gross deficiency of other preventative services in terms of nutritional services, rehabilitative, and follow-up services for chronic disorders of childhood in both the public and the private sector especially so in the private sector. There is a need to urgently address the imbalance or inequality in the service provisions both in the private sector and the public sector for any strengthening and further improvement in the overall primary health care of children in this country.[34,35] It is also noteworthy, that while the private sector has nearly twice the amount of available services and service utilization for acute curative care, there is lack of both the preventative and rehabilitative services and utilization in this sector too. Affordability of these services in the private sector may also be factor in its uptake by the persons in the lower socioeconomic strata. These differences in the primary care in the public and the private sector points to the fact that the public sector is critical to the overall availability holistic primary health care to this population as a whole and its affordability of the underprivileged section of the society in this country which forms a significant proportion of the population. This has been observed in other studies too.[36,37] Therefore, it is even more imperative that the public sector needs to take lead in addressing these discrepancies.
This study shows that, while under-five children accounted for the majority of visits in both the public and private sector, there was a significantly greater proportion of visits from under-five children in the private sector compared to the public sector [Table 3]. This is noteworthy especially since a large proportion of the under-five children visits to the public sector would have been for the immunizations as public sector is the provider for most of the immunization services. A possible explanation for the age distribution could be the higher trust, convenience and the quality of care in the private sector when it comes to the health issues of younger children. Another notable finding from this study was a significantly higher proportion of revisits in a given year in the public sector compared to the private sector. The majority of these revisits both in the public and the private sector were for the asthma and other allergic disorders such as atopic dermatitis and allergic rhinitis. These findings strongly support the need for dedicated follow-up clinics in the public and the private sector. In this regards, having locally developed rational and relevant guidelines and standard procedure manual would ensure uniform standard of care to these children. All these could be achieved at no additional cost of care, as these children are already utilizing the health care services at these polyclinics, and would be economically beneficial in the long-term.
Therefore, it would appear that when it comes to the question of seeing a physician for their illnesses, it seems that the parents choose the health care providers in the private sector which is perceived to provide better facility/expertise/accessibility and this could explain why less than a third of the total expected number of visits from children take place at the polyclinics. However, it is well established that immunization is one of the most cost effective intervention in health care system.[38] Therefore, form the public health perspective this is advantageous for the government in ensuring high coverage of vaccination in this country without having to bear the burden of entire health care cost. Once again from the public health perspective, this is a pivotal role played by the primary care set in the public sector. Inadvertently, it ensures a healthy private public partnership in the health sector.
The major limitation of this report is the inadequate rigor of the assessment of the resources and the health care utilization parameters. This was mainly due to the lack of availability of comprehensive record and statistics from both the public and the private sector. Although, not a limitation directly linked to the design or methods of this study, lack of published operational research studies in the primary care setting such as the optimum number for physicians, need and number of pediatricians, nursing resources need and optimum number of visits in children for primary care of children in a given population was a major limitation for making useful and meaning full comparison in this report.
CONCLUSIONS
Available resources in terms of physicians and the preventative (immunization) and curative service provisions are more than adequate for the given population in this country. The primary health care service provisions and their utilization in the public and the private settings are complimentary. However, the rehabilitative and other health promotion services such as nutritionist is inadequate in both the public and private sector. The findings from this study support strong need for dedicated follow-up clinics for the common childhood diseases such as asthma and other allergic disorders in this country. Also, these findings demonstrate the complimentary role of the public and the private sector in the primary health care of children in this country.
There is a need for increased rehabilitative, health promotion and support services in both the public and the private sector, and the government should take the lead in strengthening these services in the public sector. The regular periodic audit would help to make its services client friendly, more efficient and economical. Future research is needed for better characterization of clients in the public and the private sector. These will be useful in continuously updating policy and better planning of targeted primary health care provisions in this country.
ACKNOWLEDGEMENTS
The authors wish to thank all the medical officers of health, public health nurses, and the record clerks for their assistance in the data collection for this project. We thank the senior medical officers at the MOH for their comments on the data analysis. We also thank Mr. Pranav Singh for proof reading the manuscript for English.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Pan American Health Organization. Health Systems Profile Barbados: Monitoring and Analyzing Health Systems Change/Reform. [Last accessed on 2015 Jan 24]. Available from: http://www.new.paho.org/hq/dmdocuments/2010/Health-System-Profile-Barbados-2008.pdf .
- 2.Rodney P. Trenton, NJ: Africa World Press; 1998. The Caribbean State, Health Care and Women: An Analysis of Barbados and Grenada during the 1979–1983 Period; p. 126. [Google Scholar]
- 3.Hennis A, Hambleton I, Broome H, Crichlow S, Fraser H. Washington, DC: Pan American Health Organization; 2005. Health Welfare and Aging in Bridgetown, Barbados. Sabe 2000; pp. 9–63. [Google Scholar]
- 4.UNICEF Barbados-European Commission: Country Strategy Paper and National Indicative Program for the Period; 2002-2007. [Last accessed on 2015 Jan 24]. Available from: http://www.unicef.org/easterncaribbean/spmapping/Planning/national/Barbados/EU_bb_csp_en.pdf .
- 5.Starfield B. Is primary care essential? Lancet. 1994;344:1129–33. doi: 10.1016/s0140-6736(94)90634-3. [DOI] [PubMed] [Google Scholar]
- 6.Parchman ML, Culler S. Primary care physicians and avoidable hospitalizations. J Fam Pract. 1994;39:123–8. [PubMed] [Google Scholar]
- 7.Shi L. Primary care, specialty care, and life chances. Int J Health Serv. 1994;24:431–58. doi: 10.2190/BDUU-J0JD-BVEX-N90B. [DOI] [PubMed] [Google Scholar]
- 8.Shi L. The impact of primary care: A focused review. Scientifica (Cairo) 2012. 2012:432892. doi: 10.6064/2012/432892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lawn JE, Rohde J, Rifkin S, Were M, Paul VK, Chopra M. Alma-Ata 30 years on: Revolutionary, relevant, and time to revitalise. Lancet. 2008;372:917–27. doi: 10.1016/S0140-6736(08)61402-6. [DOI] [PubMed] [Google Scholar]
- 10.Hall JJ, Taylor R. Health for all beyond 2000: The demise of the Alma-Ata Declaration and primary health care in developing countries. Med J Aust. 2003;178:17–20. doi: 10.5694/j.1326-5377.2003.tb05033.x. [DOI] [PubMed] [Google Scholar]
- 11.Macinko J, Starfield B, Shi L. The contribution of primary care systems to health outcomes within Organization for Economic Cooperation and Development (OECD) countries, 1970-1998. Health Serv Res. 2003;38:831–65. doi: 10.1111/1475-6773.00149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Macinko J, Starfield B, Erinosho T. The impact of primary healthcare on population health in low- and middle-income countries. J Ambul Care Manage. 2009;32:150–71. doi: 10.1097/JAC.0b013e3181994221. [DOI] [PubMed] [Google Scholar]
- 13.Niti M, Ng TP. Avoidable hospitalisation rates in Singapore, 1991-1998: Assessing trends and inequities of quality in primary care. J Epidemiol Community Health. 2003;57:17–22. doi: 10.1136/jech.57.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kruk ME, Porignon D, Rockers PC, Van Lerberghe W. The contribution of primary care to health and health systems in low- and middle-income countries: A critical review of major primary care initiatives. Soc Sci Med. 2010;70:904–11. doi: 10.1016/j.socscimed.2009.11.025. [DOI] [PubMed] [Google Scholar]
- 15.WHO WHO. Country – Barbados, Statistics – Basic and Health Indicators 2012. [Last accessed on 2014 Jun 27]. Available from: http://www.who.int/countries/brb/en/
- 16.Explanatory Note on 2011 HDR Composite Indices: Barbados. In Human Development Report 2011 – Sustainability and Equity: A Better Future for All. 2011. [Last accessed on 2012 Aug 27]. Available from: http://www.hdrstats.undp.org/images/explanations/BRB.pdf .
- 17.Health Systems Profile Barbados: Monitoring and Analyzing Health Systems Change/Reform. 2008. [Last accessed on 2010 Jul 21]. Available from: http://www.new.paho.org/
- 18.Kumar A, Nielsen AL. Washington DC, USA: Ministry of Health, Government of Barbados Publication; 2014. Report: Strengthening Primary Health Care in Pediatrics. [Google Scholar]
- 19.PAHO/WHO. Health in the Americas, Country Profile – Barbados. 2013. [Last accessed on 2015 Jan 24]. Available from: http://www.paho.org/saludenlasamericas/indexphp?id=23 &option=com_content and Itemid=0 and lang=en .
- 20.Deveugele M, Derese A, van den Brink-Muinen A, Bensing J, De Maeseneer J. Consultation length in general practice: Cross sectional study in six European countries. BMJ. 2002;325:472. doi: 10.1136/bmj.325.7362.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mechanic D. How should hamsters run?. Some observations about sufficient patient time in primary care. BMJ. 2001;323:266–8. doi: 10.1136/bmj.323.7307.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ishida Y, Ohde S, Takahashi O, Deshpande GA, Shimbo T, Hinohara S, et al. Factors affecting health care utilization for children in Japan. Pediatrics. 2012;129:e113–9. doi: 10.1542/peds.2011-1321. [DOI] [PubMed] [Google Scholar]
- 23.Dovey S, Weitzman M, Fryer G, Green L, Yawn B, Lanier D, et al. The ecology of medical care for children in the United States. Pediatrics. 2003;111(5 Pt 1):1024–9. doi: 10.1542/peds.111.5.1024. [DOI] [PubMed] [Google Scholar]
- 24.U.S. Department of Health and Human Services. Health Resources and Services Administration (HRSA). About Health Centers: Program Requirements. 2011. [Last accessed on 2015 Jan 24]. Available from: http://www.bphc.hrsa.gov/about/requirements/index.html .
- 25.Paris: OECD; 2012. OECD. US Health Care System from an International Perspective. [Google Scholar]
- 26.Kohler PO. Specialists/primary care professionals: Striking a balance. Inquiry. 1994;31:289–95. [PubMed] [Google Scholar]
- 27.Cooper JG, Claudi T, Jenum AK, Thue G, Hausken MF, Ingskog W, et al. Quality of care for patients with type 2 diabetes in primary care in Norway is improving: Results of cross-sectional surveys of 33 general practices in 1995 and 2005. Diabetes Care. 2009;32:81–3. doi: 10.2337/dc08-0605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tsai J, Shi L, Yu WL, Hung LM, Lebrun LA. Physician specialty and the quality of medical care experiences in the context of the Taiwan national health insurance system. J Am Board Fam Med. 2010;23:402–12. doi: 10.3122/jabfm.2010.03.090222. [DOI] [PubMed] [Google Scholar]
- 29.Tsai J, Shi L, Yu WL, Lebrun LA. Usual source of care and the quality of medical care experiences: A cross-sectional survey of patients from a Taiwanese community. Med Care. 2010;48:628–34. doi: 10.1097/MLR.0b013e3181dbdf76. [DOI] [PubMed] [Google Scholar]
- 30.Ismail H, Wright J, Rhodes P, Scally A. Quality of care in diabetic patients attending routine primary care clinics compared with those attending GP specialist clinics. Diabet Med. 2006;23:851–6. doi: 10.1111/j.1464-5491.2006.01900.x. [DOI] [PubMed] [Google Scholar]
- 31.Backer V, Nepper-Christensen S, Nolte H. Quality of care in patients with asthma and rhinitis treated by respiratory specialists and primary care physicians: A 3-year randomized and prospective follow-up study. Ann Allergy Asthma Immunol. 2006;97:490–6. doi: 10.1016/S1081-1206(10)60940-4. [DOI] [PubMed] [Google Scholar]
- 32.Sin DD, Bell NR, Man SF. Effects of increased primary care access on process of care and health outcomes among patients with asthma who frequent emergency departments. Am J Med. 2004;117:479–83. doi: 10.1016/j.amjmed.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 33.Boulis AK, Long J. Variation in the treatment of children by primary care physician specialty. Arch Pediatr Adolesc Med. 2002;156:1210–5. doi: 10.1001/archpedi.156.12.1210. [DOI] [PubMed] [Google Scholar]
- 34.Grumbach K, Bodenheimer T. Can health care teams improve primary care practice? JAMA. 2004;291:1246–51. doi: 10.1001/jama.291.10.1246. [DOI] [PubMed] [Google Scholar]
- 35.Dudley L, Garner P. Strategies for integrating primary health services in low- and middle-income countries at the point of delivery. Cochrane Database Syst Rev. 2011;2:CD003318. doi: 10.1002/14651858.CD003318.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shi L, Lebrun LA, Tsai J, Zhu J. Characteristics of ambulatory care patients and services: A comparison of community health centers and physicians’ offices. J Health Care Poor Underserved. 2010;21:1169–83. doi: 10.1353/hpu.2010.0928. [DOI] [PubMed] [Google Scholar]
- 37.Hing E, Hooker RS, Ashman JJ. Primary health care in community health centers and comparison with office-based practice. J Community Health. 2011;36:406–13. doi: 10.1007/s10900-010-9322-x. [DOI] [PubMed] [Google Scholar]
- 38.Laxminarayan R, Chow J, Shahid-Salles SA. Intervention Cost-effectiveness: Overview of Main Messages. Disease Control Priorities in Developing Countries. 2nd ed. [Last accessed on 2015 Jan 24]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK11784/


