Abstract
Objectives
Studies about racial disparities in infant mortality suggest that racial differences in socioeconomic position (SEP) and maternal risk behaviors explain some, but not all, excess infant mortality among Blacks relative to non-Hispanic Whites. We examined the contribution of these to disparities in specific causes of infant mortality.
Methods
We analyzed data about 2,087,191 mother–child dyads in Michigan between 1989 and 2005. First, we calculated crude Black–White infant mortality ratios independently and by specific cause of death. Second, we fit multivariable Poisson regression models of infant mortality, overall and by cause, adjusting for SEP and maternal risk behaviors. Third, Crude Black–White mortality ratios were compared to adjusted predicted probability ratios, overall and by specific cause.
Results
SEP and maternal risk behaviors explained nearly a third of the disparity in infant mortality overall, and over 25% of disparities in several specific causes including homicide, accident, sudden infant death syndrome, and respiratory distress syndrome. However, SEP and maternal risk behaviors had little influence on disparities in other specific causes, such as septicemia and congenital anomalies.
Conclusions
These findings help focus policy attention toward disparities in those specific causes of infant mortality most amenable to social and behavioral intervention, as well as research attention to disparities in specific causes unexplained by SEP and behavioral differences.
Keywords: Infant mortality, Health inequalities, Racial disparities
Introduction
Black infants in the United States are nearly three times more likely to die before their first birthday than are non-Hispanic White infants (Scribner, 1991; Salihu et al., 2005; Mathews and MacDorman, 2010; Lu and Halfon, 2003; Anachebe and Sutton, 2003; Anachebe, 2006). It is clear that socioeconomic position (SEP) and maternal demographic and behavioral factors, such as birth out of wedlock, maternal age <20 years, alcohol use during pregnancy, and access to prenatal care are important predictors of infant mortality (Khanani et al., 2010). Some risk factors are more prevalent among Black mothers, such as lower SEP, out-of-wedlock pregnancy, and lower access to prenatal care. However, the black–white infant mortality disparity remains substantial even upon adjusting for differences in maternal SEP and behaviors (Singleton et al., 2009; Kitsantas and Gaffney, 2010a; Hessol and Fuentes-Afflick, 2005; Byrd et al., 2007; Bureau of Health Information 2001; Alio et al., 2010).
Substantial resources have been invested in attempting to narrow Black–White gaps in infant mortality on the state and federal levels (CDC, 2013). For example, reducing such disparities remain an important aim of “Women, Infants, and Children,” a federal program to provide support and care for pregnant mothers and children. However, despite these efforts, these disparities persist and in some cases, are widening (Khanani et al., 2010; Carmichael and Iyasu, 1998; Alexander et al., 2008). Therefore, a better understanding of the mechanisms that produce racial disparities in infant mortality is needed to guide interventions that may effectively reduce these disparities.
A notable gap in the literature in this area relates to studies about specific causes of infant death. It is plausible, perhaps even likely, that SEP and maternal behavior are not comparably associated with all causes of infant mortality. To date, however, studies about the influence of SEP and maternal demographic, behavioral, and access-related risk factors have not considered the influences of these factors on specific causes of infant death, and therefore cannot clarify the particular causes of death most amenable to social and behavioral interventions (Link et al., 1998). To address this limitation in the literature we assessed the differential contribution of SEP and maternal demographic, behavioral, and health access factors to Black–White disparities across specific causes of infant mortality.
Methods
Data
We obtained data about all live singleton births from the Birth Registry of the state of Michigan between January 1989 and December 2005, as well as data about all deaths among them from the Death Registry of the state of Michigan compiled by the Michigan Department of Community Health (MDCH). Using a unique MDCH statewide identifier, data about all deaths in Michigan to infants under 1 year of age during the study period were matched to births; <1% of deaths did not have suitable matches among births and were not included in the analysis.
Our analysis was restricted to infants born to both Hispanic and non-Hispanic Black (N = 420,636) or non-Hispanic White mothers (N = 1,666,555) without missing data. Data were collected about infant mortality, defined as death prior to one completed year of life. Data were also collected about primary causes of infant death using International Classification of Disease (ICD) codes defined by the World Health Organization, and are listed in ICD10/ICD9 Comparability Ratios for 113 Selected Causes of Death (Bureau of Health Information et al.). Of the 113 Selected Causes of Death, 20 causes are used for cases of infant mortality. Note that comparability ratios were used to compare deaths coded with ICD-9 (1990–1998) and ICD-10 (1999–2007). We used the following categories (ICD-9-CM codes) for infant death: certain gastrointestinal diseases (520–579), septicemia (038), remainder of infectious and parasitic diseases (001–037, 039–139), meningitis (320–322), pneumonia and influenza (480–487), congenital anomalies (740–759), newborn affected by maternal complications of pregnancy (761), newborn affected by complications of placenta, cord and membranes (762), disorders relating to short gestation and unspecified low birthweight (765), birth trauma (767), intrauterine hypoxia and birth asphyxia (768), respiratory distress syndrome (RDS) (769), other respiratory conditions (770), infections specific to the perinatal period (771), all other and ill-defined conditions originating in the perinatal period (779), SIDS (798), accidents (E800–E869, E880–E929), homicides (E960–E969), and all other causes of infant death.
Other covariates of interest included maternal race (non-Hispanic White, Black); SEP (as measured by socioeconomic factors routinely available on birth certificate data: maternal education [<12 years vs. general equivalency diploma or higher education] and hospital payment source [private insurance vs Medicaid, self-pay or other]), maternal risk behaviors (maternal smoking and alcohol consumption during pregnancy [coded as yes vs. no]), demographic risk factors (as measured by parity [0 previous births, 1 previous births, 2 or more previous births], maternal marital status at parturition [married vs. unmarried], maternal age at parturition [<20 years, 20–35 years, >35 years], and maternal birthplace [US vs. foreign]). All covariates were derived from self-reported information from infant birth certificates. None of the covariates in which we were interested had greater than 2% missing. Therefore, observations with missing variables were ignored.
This study was reviewed and approved by the Institutional Review Board of the MDCH and the Health Science Institutional Review Board of the University of Michigan.
Statistical analyses
First, we calculated descriptive statistics for all covariates and overall infant mortality (death prior to one completed year of life) and conducted two-tailed bivariate chi-square tests between maternal race and all other covariates (α < 0.05). We also used two-tailed chi-square tests to assess bivariate relations between all explanatory covariates and infant mortality (α < 0.05). Second, we calculated overall and cause-specific infant mortality ratios among Black relative to non-Hispanic White infants using infant mortalities rates calculated over the course of our study period.
Third, we fit multivariable Poisson regression models with overall infant mortality as the outcome and SEP, maternal risk behaviors, demographic risk factors, and access to prenatal care (all described above) simultaneously entered as predictors. We also fit multivariable Poisson regression models of each specific cause of infant mortality independently and SEP, maternal risk behaviors, demographic risk factors, and access to prenatal care simultaneously entered as predictors. This allowed us to determine the disparity in infant mortality by specific cause of death when variance associated with SEP, maternal risk behaviors, demographic risk factors, and access to prenatal care was factored out of the model.
Fourth, these adjusted predicted probability ratios (from each specific multivariable Poisson model specified above) for infant mortality overall and for each specific cause of death among Black relative to non-Hispanic White infants were compared to crude rate ratios to assess the proportion of the disparities in infant mortality by cause explained by differences in SEP, maternal risk behaviors, demographic factors, and access to prenatal care.
SAS 9.3 was used to carry out all statistical analyses.
Results
There were 2,087,191 live singleton births in Michigan from 1989 to 2005 to non-Hispanic White and Black mothers. Of these, 15,826 died before one completed year of life. Table 1 shows descriptive statistics and bivariate analyses between maternal race and all explanatory covariates. All covariates of interest were associated with maternal race (p < 0.001). Blacks had a greater infant mortality rate (IMR) (15.5 vs 5.6 per 1000 live births) than non-Hispanic Whites. Black mothers were less likely than non-Hispanic Whites to receive adequate prenatal care (58.6% vs 80.5%), to be married at parturition (25.5% vs 78.0%), to refrain from alcohol use during pregnancy (97.7% vs 98.4%), or to be foreign-born (1.8% vs 5.0%). Non-Hispanic White mothers were more likely than Blacks to use tobacco during pregnancy (19.3% vs 16.6%). Black mothers were more likely to have received less than 12 years of formal education (32.0% vs. 13.5%) and to have paid for their medical services with Medicaid, self-pay or other (57.1% vs. 27.2%) relative to non-Hispanic White mothers.
Table 1.
Descriptive statistics and bivariate chi-square tests between explanatory covariates and maternal race and infant mortality among live, singleton births to Black and non-Hispanic White mothers in Michigan, 1989–2005.
| Overall
|
Non-Hispanic White
|
African–American
|
p-values | |
|---|---|---|---|---|
| (n = 2,087,191)
|
(n = 1,666,555)
|
(n = 420,636)
|
||
| % | % | % | ||
| Infant mortality rate (per 1000 live births) | 7.6 | 5.6 | 15.5 | <0.001 |
| Preterm birth | <0.001 | |||
| Yes | 7.9 | 6.6 | 13.1 | |
| No | 92.1 | 93.4 | 86.9 | |
| Prenatal care* | <0.001 | |||
| Adequate | 76.1 | 80.5 | 58.6 | |
| Inadequate | 24.0 | 19.6 | 41.4 | |
| Parity | <0.001 | |||
| 0 previous | 31.6 | 32.6 | 27.4 | |
| 1 previous | 28.8 | 30.1 | 23.6 | |
| 2+ | 39.7 | 37.3 | 49.1 | |
| Marital status | <0.001 | |||
| Unmarried | 32.6 | 22.0 | 74.5 | |
| Married | 67.5 | 78.0 | 25.5 | |
| Maternal age | <0.001 | |||
| <20 | 11.7 | 8.9 | 22.7 | |
| 20–35 | 80.4 | 82.6 | 71.6 | |
| 36+ | 8.0 | 8.6 | 5.7 | |
| Education | <0.001 | |||
| <12 years | 17.2 | 13.5 | 32.0 | |
| 12 years | 36.2 | 35.8 | 37.8 | |
| >12 years | 46.6 | 50.7 | 30.2 | |
| Payment source | <0.001 | |||
| Private insurance | 66.7 | 72.8 | 42.8 | |
| Medicaid, self-pay, other | 33.3 | 27.2 | 57.2 | |
| Mother US born | <0.001 | |||
| Yes | 95.6 | 95.0 | 98.2 | |
| No | 4.4 | 5.0 | 1.8 | |
| Alcohol use | <0.001 | |||
| None | 98.3 | 98.4 | 97.7 | |
| Yes | 1.7 | 1.6 | 2.3 | |
| Smoking | <0.001 | |||
| None | 81.3 | 80.7 | 83.4 | |
| Yes | 18.8 | 19.3 | 16.6 |
The Kessner/Institute of Medicine Adequacy of Prenatal Care Index (Kessner et al., 1973) was calculated and analyzed as a binary variable denoting adequate vs. inadequate prenatal care.
Table 2 shows infant mortality rates per 1000 live births and bivariate chi-square tests per category for all explanatory covariates among non-Hispanic White and Black infants. All explanatory covariates were significantly associated with all outcomes of interest among both Blacks and non-Hispanic Whites, as well as overall (p < 0.001). Maternal SEP, maternal demographic risk factors (including maternal parity of two or more, birth out of wedlock, maternal age less than 20 years, and maternal birthplace within the United States), and maternal behavioral factors (maternal alcohol and tobacco consumption during pregnancy) and access to prenatal care (inadequate prenatal care use) all carried higher risk for infant mortality overall and among both racial groups.
Table 2.
Descriptive statistics and bivariate chi-square tests between explanatory covariates and race and infant mortality rate (per 1000 live births) among live, singleton births to Black and Non-Hispanic White mothers in Michigan, 1989–2005.
| Overall
|
Non-Hispanic White
|
African–American
|
||||
|---|---|---|---|---|---|---|
| (n = 2,087,191)
|
(n = 9312)
|
(n = 6514)
|
||||
| IMR | p | IMR | p | IMR | p | |
| Prenatal care* | <0.001 | <0.001 | <0.001 | |||
| Adequate | 5.7 | 4.5 | 12.4 | |||
| Inadequate | 13.4 | 10 | 19.7 | |||
| Parity | <0.001 | <0.001 | <0.001 | |||
| 0 previous | 6.8 | 5.4 | 13.5 | |||
| 1 previous | 6.2 | 4.8 | 13.3 | |||
| 2+ | 9 | 6.3 | 17.1 | |||
| Marital status | <0.001 | <0.001 | <0.001 | |||
| Unmarried | 12.5 | 8.9 | 16.7 | |||
| Married | 5.2 | 4.6 | 12 | |||
| Maternal age | <0.001 | <0.001 | <0.001 | |||
| <20 | 11.7 | 9.5 | 15.2 | |||
| 20–35 | 7 | 5.2 | 15.2 | |||
| 36+ | 7.6 | 5.7 | 19.3 | |||
| Education | <0.001 | <0.001 | <0.001 | |||
| <12 years | 12.5 | 9.6 | 17.4 | |||
| 12 years | 8.1 | 6.1 | 15.3 | |||
| >12 years | 5 | 3.9 | 12 | |||
| Payment source | <0.001 | <0.001 | <0.001 | |||
| Private insurance | 5.8 | 4.6 | 13.8 | |||
| Medicaid, self-pay, other | 11.1 | 8.2 | 16.5 | |||
| Mother US born | <0.001 | <0.001 | <0.001 | |||
| Yes | 7.6 | 5.6 | 15.2 | |||
| No | 4.9 | 4.4 | 9.7 | |||
| Alcohol use | <0.001 | <0.001 | <0.001 | |||
| None | 7.2 | 5.4 | 14.7 | |||
| Yes | 16.6 | 10.5 | 33.7 | |||
| Smoking | <0.001 | <0.001 | <0.001 | |||
| None | 6.5 | 4.7 | 13.7 | |||
| Yes | 11.2 | 8.7 | 22.9 | |||
The Kessner/Institute of Medicine Adequacy of Prenatal Care Index (Kessner et al., 1973) was calculated and analyzed as a binary variable denoting adequate vs. inadequate prenatal care.
Table 3 shows the risk of infant mortality by maternal race adjusted for SEP (maternal education and payment source), maternal demographic risk factors (parity, marital status, maternal age at parturition, maternal birthplace [US vs. foreign]), maternal behavioral risk factors (maternal use of alcohol and tobacco during pregnancy), and access to prenatal care (prenatal care adequacy). After adjusting for these factors, Black infants had nearly twofold higher risk of infant mortality (RR = 1.96 [95% CI: 1.88–2.04]) than non-Hispanic Whites.
Table 3.
Multivariable Poisson regression model of infant mortality by maternal race adjusted for social and maternal behavioral mediators among live, singleton births to Black or non-Hispanic White mothers in Michigan, 1989–2005.
| Infant mortality1
|
|
|---|---|
| RR (95% CI) | |
| Race/ethnicity | |
| White | ref |
| African–American | 1.96 (1.88, 2.04) |
| Prenatal care* | |
| Adequate | ref |
| Inadequate | 1.48 (1.43, 1.54) |
| Parity | |
| 0 previous | 1.01 (0.97, 1.06) |
| 1 previous | ref |
| 2+ | 1.22 (1.17, 1.27) |
| Marital status | |
| Unmarried | 1.28 (1.22, 1.34) |
| Married | ref |
| Maternal age | |
| <20 | 1.09 (1.03, 1.15) |
| 20–35 | ref |
| 36+ | 1.21 (1.14, 1.29) |
| Education | |
| <12 years | 1.1 (1.05, 1.15) |
| 12 years | ref |
| >12 years | 0.81 (0.78, 0.85) |
| Payment source | |
| Private insurance | ref |
| Medicaid, self-pay, other | 1.11 (1.07, 1.16) |
| Mother US born | |
| Yes | ref |
| No | 0.85 (0.77, 0.94) |
| Alcohol use | |
| None | ref |
| Yes | 1.5 (1.38, 1.64) |
| Smoking | |
| None | ref |
| Yes | 1.36 (1.3, 1.41) |
The Kessner/Institute of Medicine Adequacy of Prenatal Care Index (Kessner et al., 1973) was calculated and analyzed as a binary variable denoting adequate vs. inadequate prenatal care.
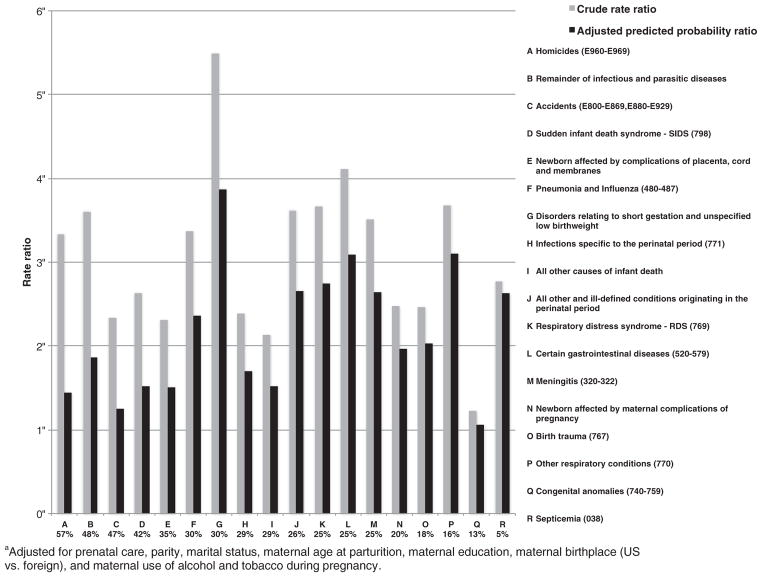
Fig. 1 shows both crude rate ratios of infant mortality by cause among Blacks relative to non-Hispanic Whites, as well as rate ratios adjusted for SEP (maternal education and payment source), maternal demographic risk factors (parity, marital status, maternal age at parturition, maternal birthplace [US vs. foreign]), maternal behavioral risk factors (maternal use of alcohol and tobacco during pregnancy), and access to prenatal care (prenatal care adequacy). Adjusted ratios were lower than crude ratios for all causes and SEP, and maternal demographic, behavioral, and health access differences explained between 57% and 5% of disparities in cause-specific mortality. Adjustment explained >30% of disparities in cause-specific mortality for seven causes, including Homicides (57%), remainder of infectious and parasitic diseases (48%), accidents (47%), SIDS (42%), newborn affected by complications of placenta, cord and membranes (35%), pneumonia and influenza (30%), and disorders related to short gestation and low birthweight (30%). SEP, and maternal demographic, behavioral, and health access differences explained between 15% and 30% of disparities in nine causes: infections specific to the perinatal period (29%), all other causes of death (29%), all other and ill-defined conditions originating in the perinatal period (26%), RDS (25%), certain gastrointestinal diseases (25%), meningitis (25%), newborn affected by maternal complications of pregnancy (20%), birth trauma (18%), and other respiratory conditions (16%). Adjustment only explained 13% of disparities in congenital anomalies, and 5% of disparities in septicemia.
Fig. 1.
Crude risk ratios and adjusted predicted probability ratiosa of infant mortality by cause as well as proportion of crude ratios explained by adjustment among Black relative to Non-Hispanic White mothers in Michigan, 1989–2005. aAdjusted for prenatal care, parity, marital status, maternal age at parturition, maternal education, maternal birthplace (US vs. foreign), and maternal use of alcohol and tobacco during pregnancy.
Discussion
In a study of all births to Black and non-Hispanic White mothers in one US state between 1989 and 2005, we found that SEP and maternal demographic, behavioral, and health access differences explained nearly a third of the Black–White disparity in infant mortality overall, as well as over 30% of the Black–White disparity in several specific causes of infant mortality including homicide, accident, SIDS, and disorders relating to short gestation and low birthweight. By contrast, SEP and maternal risk behaviors had little influence on disparities in other specific causes, such as septicemia and congenital anomalies.
Our findings build on previous studies that have documented racial disparities in specific causes of infant mortality, as well as those that have demonstrated the contributions of social factors to racial disparities in infant mortality overall (Hessol and Fuentes-Afflick, 2005; Byrd et al., 2007; Kitsantas and Gaffney, 2010b; Singleton et al., 2009; Hauck et al., 2002; Papacek et al., 2002; Collins et al., 2003). However, ours is the first study, of which we are aware, that has attempted to understand the contribution of differences in SEP and maternal demographic, behavioral, and health access factors between Blacks and non-Hispanic Whites to cause-specific disparities in infant mortality.
Our work links together two disparate literatures concerned with infant mortality. There is a sizable literature that has documented the contribution of SEP and maternal behaviors to Black–White differences in infant mortality overall (Hessol and Fuentes-Afflick, 2005; Byrd et al., 2007; Kitsantas and Gaffney, 2010b; Papacek et al., 2002; Collins et al., 2003). For example, a recent study by Elder and colleagues demonstrated that the proportion of the Black–White infant mortality disparity explained by differences in demographic, geographic, and childbearing risk factors had declined over the past two decades, even as the proportion of the disparity not explained by these factors increased over the same time period (Elder et al., 2014). A parallel stream of work has examined disparities in infant mortality by cause. For example, there are Black–White disparities in infant mortality due to SIDS, likely owing to more common parent–infant bed-sharing and use of nonstandard sleeping surfaces, such as floor mattress and couches among Blacks (Hauck et al., 2002; Joyner et al., 2010).
Our work brings together these heretofore-disparate literatures by comparing crude cause-specific rate ratios to predicted probability ratios adjusted for SEP and maternal demographic, behavioral, and health access differences. This approach has two central advantages: First, assessing differences in the contributions of these factors to specific causes of death may improve our understanding of the etiology of each of these specific causes, more broadly. Second, clarifying the particular downstream influences of these factors on infant mortality can help to improve the ways in which interventions are targeted.
In that respect, the literature has demonstrated that some specific causes of mortality may be more sensitive to social patterning than others (Galea et al., 2005; Ahern et al., 2008), providing a rational explanation for the heterogeneity in the influence of social factors across causes of death that we observed here. Borrowing from this literature about overall mortality, it is plausible that the influences of social factors on specific causes of infant mortality may also be heterogeneous, as our findings suggested that SEP and maternal risk factors, including prenatal care, parity, marital status, maternal age at parturition, maternal education, maternal birthplace (US vs. foreign), and maternal use of alcohol and tobacco during pregnancy explained different proportions of the disparity in infant mortality by cause.
SEP and maternal demographic and behavioral risk factors explained a sizable portion of the disparity in infant mortality resulting from pre-term birth or low birthweight. This is consistent with a well-developed literature that has demonstrated the social and behavioral predictors of preterm birth and low birthweight—many for which we adjusted here. For example, maternal smoking, maternal education (Luo et al., 2006; Kyrklund-Blomberg and Cnattingius, 1998), and maternal nativity have all been demonstrated to predict higher risk for preterm birth (Singh and Yu, 1996). It follows that these factors, via population-level increases in risk for preterm birth and low birthweight, would also increase risk for infant mortality to these causes.
Furthermore, differences in SEP and maternal risk factors between Black and non-Hispanic White mothers also explained a substantial proportion of the disparity in causes of death attributable to exposures occurring after birth, including accidents, homicide, perinatal infection, and SIDS. The factors for which we adjusted likely index the material well-being of homes into which infants are born and are, as such, important in shaping perinatal risk of death. Further, maternal health behaviors may be influential in child health through a variety of mechanisms and alongside other factors that shape home environments that may influence the risk of a range of causes of death. This is supported by the literature that has explored the predictors of these causes of death. For example, Black–White disparities in infant mortality to SIDS are explained by differences in parent–infant bed-sharing and use of nonstandard sleeping surfaces, such as floor mattress and couches, among Blacks relative to Whites (Hauck et al., 2002; Joyner et al., 2010). Similarly with respect to accidental death, Tomashek et al. (2003) reported that Black infants were more likely to die of unintentional injury than non-Hispanic White infants as a result of mechanical suffocation, obstructive suffocation, motor vehicle crashes, fires, drowning, falls, and poisoning (Tomashek et al., 2003). As many of these mechanisms are socioeconomically and behaviorally mediated, it follows that adjusting for SEP and maternal health behaviors would explain a sizable proportion of Black–White disparities in these causes of death.
By contrast, SEP and maternal behavioral, demographic, and health access differences had little influence on disparities in mortality resulting from septicemia or congenital anomalies. This is consistent with what is understood about the etiology of each of these outcomes. For example, sepsis is most commonly a cause of death among neonates infected with particular bacteria colonizing the maternal vagina during the course of parturition—a result of improper obstetrical management of chorioamnionitis or vaginal colonization with potential virulent microbiota (Stoll et al., 1998). Therefore, given the well-established literature demonstrating that the quality of obstetric care is driven principally by provider characteristics rather than prenatal characteristics such as those we explored here (Phibbs et al., 1996), it is plausible that disparities in neonatal sepsis should be less attributable to maternal differences in SEP, health behaviors, and health access between Black and White mothers. Similarly, congenital anomalies may be more likely to be influenced by broad environmental exposures to which Black mothers may be more likely to be exposed rather than individual-level differences in SEP, health behaviors, and health access between Black and White mothers (Dolk et al., 1998; Dolk and Vrijheid, 2003).
On this note, it is important to stress that while our covariate set included many of the most important socioeconomic and behavioral predictors of infant mortality, such as maternal age, maternal education, and maternal smoking during pregnancy, there are other important demographic and behavioral factors about which we did not have data. There remain substantial differences, for example, in the social and environmental contexts, including contextual income inequality, community disorder, and area-level SEP, within which Black and non-Hispanic White infants are born. Moreover, racial differences in social exposures not considered here, including social support, social exclusion, and discrimination may also contribute to inequalities in infant mortality. In this regard, we explicitly caution readers from concluding that residual differences in racial disparities in cause-specific infant mortality are uniquely attributable to biological or genetic differences between Black and non-Hispanic White infants or their mothers.
Rather, we suggest that a more promising mechanism to pursue for further research is the pervasive, systematic, and ongoing structural and interpersonal discrimination experienced by Blacks in the United States due to persistently marginalized social status that structures resources and opportunities and causes chronic exposure to stress. For example, Geronimus first observed that the Black–White disparity in birthweight increased with maternal age (Geronimus, 1996). Coining the “weathering” hypothesis, she reasoned that this observed effect represented the aggregate of the negative influences of discrimination-associated stress among Black relative to non-Hispanic White mothers with time—demonstrating the importance of discrimination as a contributor to the Black–White disparity in birth outcomes.
There are several limitations that must be considered when interpreting our findings. First, our sample included births from only one state in the United States. Thus, these findings may not be transportable to other states or countries. Nevertheless, as Michigan has a large Black minority with relatively poor health outcomes, findings from Michigan are likely to extend to other regions with vulnerable Black populations. Second, as discussed above, our covariate sample was limited. For example, the only SEP variables for which data were available were maternal education and payment source for obstetric services. However, SEP also includes measures of income and wealth, which were unavailable, suggesting that our analyses may not have had the capacity to fully account for the influence of SEP on disparities in cause-specific mortality. However, we were limited by the breadth of data collected in publicly available datasets, the size and quality of which were necessary to carry out the present analysis. Third, our study relied on the accuracy of data from the vital birth and death registries. While these registries provide potentially unreliable estimates of maternal tobacco and alcohol use during pregnancy, they have been shown to accurately report demographic data (Buescher, 1993; Northam, 2006).
Our work suggests several avenues for research and public health policy. First, we found that up to 30% of racial disparities in infant mortality can be explained by commonly understood differences in SEP, maternal demographics, behaviors, and access to prenatal care; this implies that a substantial proportion of these inequalities are not accounted for by the factors we considered here. There are substantial differences in the social and environmental contexts, including contextual income inequality, community disorder, and area-level SEP, within which Black and non-Hispanic White infants are born. Similarly, racial differences in other social exposures, including social support, social exclusion, and discrimination may also contribute to inequalities in infant mortality. Understanding the contributions of these contextual and social factors to the Black–White infant mortality gap is an important area of future work. With respect to health policy, addressing the upstream social predictors of infant mortality, such as SEP, maternal health risk behaviors, and differences in access to prenatal care may address a substantial proportion of inequalities overall, as well as inequalities in high burden causes of infant death, including SIDS and perinatal infections.
Acknowledgments
Funding
AME and DWF were funded, in part, by the Rhodes Trust. There was no specific support for this project. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and/or preparation, review, or approval of the manuscript.
Footnotes
Contributors
AME and DWF conceived and designed the analysis. DFW and MP conducted the analysis. AME and DWF drafted the manuscript. KMK and SG edited the manuscript for intellectual content. All authors have reviewed and approve of the final version of the manuscript and have taken due care to ensure the integrity of this work. All authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Conflict of interest
The authors declare that there are no conflicts of interest.
References
- Ahern J, Galea S, Hubbard A, Midanik L, Syme SL. “Culture of drinking” and individual problems with alcohol use. Am J Epidemiol. 2008;167:1041–1049. doi: 10.1093/aje/kwn022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander GR, Wingate MS, Bader D, Kogan MD. The increasing racial disparity in infant mortality rates: composition and contributors to recent US trends. Am J Obstet Gynecol. 2008;198:51.e1–51.e9. doi: 10.1016/j.ajog.2007.06.006. [DOI] [PubMed] [Google Scholar]
- Alio AP, Kornosky JL, Mbah AK, Marty PJ, Salihu HM. The impact of paternal involvement on feto-infant morbidity among Whites, Blacks and Hispanics. Matern Child Health J. 2010;14:735–741. doi: 10.1007/s10995-009-0482-1. [DOI] [PubMed] [Google Scholar]
- Anachebe NF. Racial and Ethnic Disparities in Infant and Maternal Mortality. 2006:16. [PubMed] [Google Scholar]
- Anachebe NF, Sutton MY. Racial disparities in reproductive health outcomes. Am J Obstet Gynecol. 2003;188:S37–S42. doi: 10.1067/mob.2003.245. [DOI] [PubMed] [Google Scholar]
- Buescher PA. The Quality of the New Birth Certificate Data: A Validation Study in North Carolina. 1993:83. doi: 10.2105/ajph.83.8.1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Health Information. ICD-10/ICD-9 Comparability Ratios for the 113 Selected Causes of Death. 2001. Division of Health Care Financing & Department of Health Family Services. [Google Scholar]
- Byrd DR, Katcher ML, Peppard P, Durkin M, Remington PL. Infant mortality: explaining black/white disparities in Wisconsin. Matern Child Health J. 2007;11:319–326. doi: 10.1007/s10995-007-0183-6. [DOI] [PubMed] [Google Scholar]
- Carmichael SL, Iyasu S. Changes in the black–white infant mortality gap from 1983 to 1991 in the United States. Am J Prev Med. 1998;15:220–227. doi: 10.1016/s0749-3797(98)00052-x. [DOI] [PubMed] [Google Scholar]
- CDC. [Accessed September 28th 2013];Infant Mortality. 2013 [Online]. Available:, http://www.cdc.gov/reproductivehealth/MaternalInfantHealth/InfantMortality.htm.
- Collins JW, David RJ, Jr, Prachand NG, Pierce ML. Low birth weight across generations. Matern Child Health J. 2003;7:229–237. doi: 10.1023/a:1027371501476. [DOI] [PubMed] [Google Scholar]
- Dolk H, Vrijheid M. The impact of environmental pollution on congenital anomalies. Br Med Bull. 2003;68:25–45. doi: 10.1093/bmb/ldg024. [DOI] [PubMed] [Google Scholar]
- Dolk H, Vrijheid M, Armstrong B, Abramsky L, Bianchi F, Garne E, Nelen V, Robert E, Scott JE, Stone D. Risk of congenital anomalies near hazardous-waste land-fill sites in Europe: the EUROHAZCON study. Lancet. 1998;352:423–427. doi: 10.1016/s0140-6736(98)01352-x. [DOI] [PubMed] [Google Scholar]
- Elder TE, Goddeeris JH, Haider SJ, Paneth N. The changing character of the black–white infant mortality gap, 1983–2004. Am J Public Health. 2014:e1–e7. doi: 10.2105/AJPH.2013.301349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Ahern J, Karpati A. A model of underlying socioeconomic vulnerability in human populations: evidence from variability in population health and implications for public health. Soc Sci Med. 2005;60:2417–2430. doi: 10.1016/j.socscimed.2004.11.028. [DOI] [PubMed] [Google Scholar]
- Geronimus AT. Black/white differences in the relationship of maternal age to birthweight: a population-based test of the weathering hypothesis. Soc Sci Med. 1996;42:589–597. doi: 10.1016/0277-9536(95)00159-x. [DOI] [PubMed] [Google Scholar]
- Hauck FR, Moore CM, Herman SM, Donovan M, Kalelkar M, Christoffel KK, Hoffman HJ, Rowley D. The contribution of prone sleeping position to the racial disparity in sudden infant death syndrome: the Chicago Infant Mortality Study. Pediatrics. 2002;110:772–780. doi: 10.1542/peds.110.4.772. [DOI] [PubMed] [Google Scholar]
- Hessol NA, Fuentes-Afflick E. Ethnic differences in neonatal and postneonatal mortality. Pediatrics. 2005;115:e44–e51. doi: 10.1542/peds.2004-0478. [DOI] [PubMed] [Google Scholar]
- Joyner BL, Oden RP, Ajao TI, Moon RY. Where should my baby sleep: a qualitative study of African American infant sleep location decisions. J Natl Med Assoc. 2010;102:881–889. doi: 10.1016/s0027-9684(15)30706-9. [DOI] [PubMed] [Google Scholar]
- Kessner DM, Singer J, Kalk CE, Schlesinger ER. Infant Death: An Analysis by Maternal Risk and Health Care. Institute of Medicine and National Academy of Sciences; Washington, DC: 1973. [Google Scholar]
- Khanani I, Elam J, Hearn R, Jones C, Maseru N. The impact of prenatal WIC participation on infant mortality and racial disparities. Am J Public Health. 2010;100:S204–S209. doi: 10.2105/AJPH.2009.168922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitsantas P, Gaffney K. Racial/ethnic disparities in infant mortality. J Perinat Med. 2010;38:87–94. doi: 10.1515/jpm.2010.014. [DOI] [PubMed] [Google Scholar]
- Kyrklund-Blomberg NB, Cnattingius S. Preterm birth and maternal smoking: risks related to gestational age and onset of delivery. Am J Obstet Gynecol. 1998;179:1051–1055. doi: 10.1016/s0002-9378(98)70214-5. [DOI] [PubMed] [Google Scholar]
- Link BG, Northridge ME, Phelan JC, Ganz ML. Social epidemiology and the fundamental cause concept: on the structuring of effective cancer screens by socioeconomic status. Milbank Q. 1998;76:375–402. doi: 10.1111/1468-0009.00096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Matern Child Health J. 2003;7:13. doi: 10.1023/a:1022537516969. [DOI] [PubMed] [Google Scholar]
- Luo Z-C, Wilkins R, Kramer MS for the Fetal Infant Health Study Group of the Canadian Perinatal Surveillance System. Effect of neighbourhood income and maternal education on birth outcomes: a population-based study. Can Med Assoc J. 2006;174:1415–1420. doi: 10.1503/cmaj.051096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathews TJ, Macdorman MF. Infant mortality statistics from the 2006 period linked birth/infant death data set. National vital statistics reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2010;58:1–31. [PubMed] [Google Scholar]
- Northam S. The Reliability and Validity of Birth Certificates. 2006:35. doi: 10.1111/j.1552-6909.2006.00016.x. [DOI] [PubMed] [Google Scholar]
- Papacek EM, Collins JW, Jr, Schulte NF, Goergen C, Drolet A. Differing postneonatal mortality rates of African–American and white infants in Chicago: an ecologic study. Matern Child Health J. 2002;6:99–105. doi: 10.1023/a:1015464207740. [DOI] [PubMed] [Google Scholar]
- Phibbs CS, Bronstein JM, Buxton E, Phibbs RH. THe effects of patient volume and level of care at the hospital of birth on neonatal mortality. J Am Med Assoc. 1996;276:1054–1059. [PubMed] [Google Scholar]
- Salihu HM, Garces IC, Sharma PP, Kristensen S, Ananth CV, Kirby RS. Stillbirth and infant mortality among Hispanic singletons, twins, and triplets in the United States. Obstet Gynecol. 2005;106:789–796. doi: 10.1097/01.AOG.0000177975.61197.ae. [DOI] [PubMed] [Google Scholar]
- Scribner RA. Infant mortality among Hispanics: the epidemiological paradox. J Am Med Assoc. 1991;265:2065–2066. [PubMed] [Google Scholar]
- Singh GK, Yu SM. Adverse pregnancy outcomes: differences between US- and foreign-born women in major US racial and ethnic groups. Am J Public Health. 1996;86:837–843. doi: 10.2105/ajph.86.6.837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singleton RJ, Wirsing EA, Haberling DL, Christensen KY, Paddock CD, Hilinski JA, Stoll BJ, Holman RC. Risk factors for lower respiratory tract infection death among infants in the United States, 1999–2004. Pediatrics. 2009;124:e768–e776. doi: 10.1542/peds.2009-0109. [DOI] [PubMed] [Google Scholar]
- Stoll BJ, Holman RC, Schuchat A. Decline in sepsis-associated neonatal and infant deaths in the United States, 1979 through 1994. Pediatrics. 1998;102:e18. doi: 10.1542/peds.102.2.e18. [DOI] [PubMed] [Google Scholar]
- Tomashek KM, Hsia J, Iyasu S. Trends in postneonatal mortality attributable to injury, United States, 1988–1998. Pediatrics. 2003;111:1219–1225. [PubMed] [Google Scholar]