Abstract
Objective
To examine life-space mobility over 8.5 years among older Black and White male veterans and non-veterans in the Deep South.
Design
A prospective longitudinal study of community-dwelling Black and White male adults aged >65 years (N=501; mean age=74.9; 50% Black and 50% White) enrolled in the University of Alabama at Birmingham (UAB) Study of Aging. Data from baseline in-home assessments with follow-up telephone assessments of life-space mobility completed every 6 months were used in linear mixed-effects modeling analyses to examine life-space mobility trajectories.
Main Outcome Measures
Life-space mobility.
Results
In comparison to veterans, non-veterans were more likely to be Black, single, and live in rural areas. They also reported lower income and education. Veterans had higher baseline life-space (73.7 vs 64.9 for non-veterans; P<.001). Race-veteran subgroup analyses revealed significant differences in demographics, comorbidity, cognition, and physical function. Relative to Black veterans, there were significantly greater declines in life-space trajectories for White non-veterans (P=.009), but not for White veterans (P=.807) nor Black non-veterans (P=.633). Mortality at 8.5 years was 43.5% for veterans and 49.5% for non-veterans (P=.190) with no significant differences by race-veteran status.
Conclusions
Veterans had significantly higher baseline life-space mobility. There were significantly greater declines in life-space trajectories for White non-veterans in comparison to other race-veteran subgroups. Black veterans and non-veterans did not have significantly different trajectories.
Keywords: Life-space Mobility, Older Veterans, Cumulative Inequality
Introduction
In the United States, racial disparities abound in practically every facet of society, including education, income, employment, housing, and most importantly, health.1 Racial disparities in health are prominent in advanced age, particularly between Blacks and Whites.2 Racial differences in life-space, a measure of mobility incorporating distance traveled, frequency of travel, and independence of movement, have been documented among older Blacks and Whites;3,4 less is known about racial differences in life-space mobility of older veterans.
Theoretical approaches to understand racial disparities in health, in particular the life-course perspective, have included life course epidemiology,5 cumulative advantage theory,6 and cumulative disadvantage theory.7,8 Cumulative disadvantage theory has been used extensively to examine racial health inequalities over the life course. Ferraro and colleagues used cumulative disadvantage theory to examine racial health disparities in hospital admissions and discharges.8 They found Black adults were less likely than Whites to be admitted to the hospital, had longer length of stays, and Black men aged >70 years were more likely to die within two weeks of a hospital stay.
In recent years, Ferraro and Shippee9 have advanced the discussion on cumulative advantage/disadvantage and life course health by introducing cumulative inequality theory (CIT), an integrative life course perspective that builds on the work of others, such as Dannefer10 and O’Rand.11 CIT postulates that “social systems generate inequality, which is manifested over the life course via demographic and developmental processes, and that personal trajectories are shaped by the accumulation of risk, available resources, perceived trajectories, and human agency.”9 CIT incorporates the potential for events throughout the life course to mitigate or interrupt the cumulative effects of early life course disadvantage. An exemplar in this growing area of research was the study conducted by Shippee and colleagues12 in their longitudinal examination showing the effects of accumulated financial strain on women’s health trajectories.
Although racial disparities in health have been explored over the life course, the benefits of military service on the life-space of older veterans have not been determined. First discussed by Brotz and Wilson13 and later by Sampson and Laub,14 military service results in a “knifing-off” of previous experience, including past indiscretions such as juvenile delinquency. Thus, military service erases negative life events that would most likely result in limited opportunities for advancement in civilian life. In addition to knifing-off, Elder examined the benefits of military service on the life course of WWII veterans.15, 16 He found that military service represented a “turning point” in the lives of veterans who were inducted at younger ages, compared with veterans who were inducted in their third decade of life.
To expand the theoretical understanding about the benefits of military service on life-space mobility over the life course, our approach to this study is through the theoretical lens of CIT.9 While in agreement with Ferraro and colleagues about the inherent inequality within social structures, we propose that military service would mitigate the childhood and adolescence disadvantages to Black males, such as socio-economic disadvantage, racism and discrimination, through knifing–off and turning points.
The purpose of these analyses was to examine life-space mobility of older Black and White male veterans and non-veterans who participated in the University of Alabama at Birmingham (UAB) Study of Aging.17 First, we hypothesized that life-space mobility trajectories would demonstrate that both Black and White male veterans would have higher baseline life-space and slower declines than non-veterans. Second, we hypothesized that Black veterans would have lower life-space mobility in comparison with White veterans. Third, we hypothesized that in comparison with Black male veterans, Black non-veterans would demonstrate lower baseline life-space mobility scores and steeper decline in life-space trajectories.
Methods
Participants
The UAB Study of Aging was a longitudinal investigation of mobility designed to examine racial differences in mobility and changes in mobility associated with aging.17 Participants (N=1,000) were a stratified random sample, balanced in terms of race, sex, and rural/urban residence. Participants were recruited from a list of community-dwelling Medicare beneficiaries aged >65 years from five central Alabama counties. Baseline in-home interviews were conducted between November 1999 and February 2001 by trained interviewers after obtaining informed consent. Follow-up telephone interviews to assess life-space mobility and vital status were conducted at six-month intervals over the next 8.5 years. The UAB Institutional Review Board approved the study protocol. Detailed study methods have been described elsewhere.17,18 Our analyses used data from male participants of the UAB Study of Aging since the focus of this study was a comparison of male veterans and non-veterans.
Measures
Life-space
The primary outcome measure was the UAB Life-Space Assessment (LSA), a validated patient-reported outcome that measures community mobility and also reflects social participation17-19 and quality of life.20 LSA incorporates the distance traveled in terms of life-space levels (ranging from within one’s bedroom to out of town), frequency with which the life-space level is attained, and degree of independence, based on the reported use of assistive equipment or help from another person during the past four weeks. Scores range from 0-120, with higher scores reflecting greater mobility.
Military Service
Veteran status was self-reported without the determination of branch of service, the number of years served or designation of the nature of the service.
Demographic and Economic Factors
Demographic factors were self-reported and included age, sex, race, and marital status. Locale was defined as urban or rural based on county population.21 Income, education, and marital status variables were used as dichotomous measures. Income was categorized into <$12,000 and >$12,000, which was based on poverty guidelines at the time of the initial study.22 Education was categorized into <7th grade education based on the high number of participants without a 7th grade education.17 Marital status was categorized as married vs not married. Participants provided birthdates, state of birth, and time living in their current communities. Transportation resources were assessed by asking participants questions about transportation difficulty.
Comorbidity and Medications
During the baseline interview, participants were asked if a physician had ever told them they had diseases contained in the Charlson Comorbidity Index,23 such as congestive heart failure, hypertension, and diabetes mellitus. Participants showed all prescriptions, OTC, and supplements to the interviewer. Verified diagnoses by a physician, hospital record, or medication for the condition were used for analyses.
Geriatric Depression Scale
The short form of the Geriatric Depression Scale (GDS) was used to assess depressive symptoms.24 Scores range from 0 to 15; a score of 6 or higher suggests possible depression.
Mental Status
The Mini-Mental Status Exam (MMSE) was used to assess cognition.25 Scores range from 0-30; lower scores indicate poorer performance.
Physical Function
During the baseline in-home assessment, the short physical performance battery (SPPB) was performed.26 Scores were calculated by summing results from tests of walking speed, balance, and timed chair stands, based on values established by the SPPB. Scores for individual tasks range from 0 to 4 with a score of 4 representing better performance. Composite scores range from 0-12.
Vital Status
Mortality was determined from the follow-up interviews and confirmed using the National Death Index.27 Time to death and length of follow-up were calculated in half-year increments.
Statistical Analysis
Summary data consisted of frequencies (percentages) for categorical variables and means and standard deviations for continuous variables. Independent sample t-tests compared continuous variables (age, life-space, mental status, depression, comorbidity, number of medications, length of follow-up in years, and time to death in years). Chi-square tests of independence examined the relationship between categorical variables (veteran status, race, rural residence, education, income, marital status, transportation difficulty, and mortality). The primary analysis examined the rate of change (slope) and baseline scores (intercept) for LSA using linear mixed effects models (random coefficients models). The mixed effects model incorporates all data from dropouts collected prior to attrition into the trajectories (rather than restricting to complete cases) and minimizes bias and better controls for Type I error in the presence of missing data.28 Previous research has shown that the LSA follows an approximately linear trajectory in the absence of acute events, such as hospitalization.29 Models were constructed with group effect (race, veteran status, or both), time, and group by time interaction.
Thus, for participant
i=1,2,…,n at visit j=1,2,…,ni the model was LSAi,j = intercepti + groupi + timei,j + groupi • time i,j + ε i,j
which included fixed effects of time at the group level, and random effects of time at the individual level to account for subject-specific variation from the group mean. An unstructured covariance matrix was used to model the independence of the slope and intercept parameters. Parameters were estimated using restricted maximum likelihood (REML). The primary test of interest was the group by time interaction, indicating that slopes (life-space trajectories) differed by race and/or veteran category. Secondary analyses examined the effect of race only and veteran status only. Sensitivity analyses included covariates of demographics, Charlson comorbidity score,23 GDS,24 MMSE,25 and SPPB26 in the above models.
Results
Five hundred-one males (mean age=74.9; 50% Black and 50% White) were assessed at baseline. Sixty percent (n=301) reported being a veteran. Four hundred and fifty-three (90.4%) participants were born in the Deep South (Alabama, Georgia, and Mississippi) between 1909 and 1936. In comparison to veterans, non-veterans were more likely to report their birthplace as the Deep South (94.5% vs 87.7%).
Non-veterans were more likely to be older, Black, single, and living in rural areas. They also reported lower income, education, and difficulty with transportation. Veterans had significantly higher baseline life-space (73.7 vs 64.9 for non-veterans), lower scores on geriatric depression, higher cognitive scores, and higher scores on function, as measured by SPPB.26 Additional characteristics are displayed in Table 1.
Table 1. Characteristics of male participants in the UAB Study of Aging based on veteran status.
| Non-Veterans (n=200) | Veterans (n=301) | ||||
| n | Mean (SD) or % | n | Mean (SD) or % | P | |
| Mean age | 200 | 76.3 (7.5) | 301 | 74.0 (5.5) | <.001a |
| Black | 141 | 70.5% | 110 | 36.5% | <.001a |
| Rural | 116 | 58.0% | 141 | 46.8% | .014a |
| ≤7th Education | 87 | 43.5% | 33 | 10.9% | <.001a |
| Income <$12,000 | 104 | 52.0% | 62 | 20.6% | <.001a |
| Married | 124 | 62.0% | 223 | 74.0% | .004a |
| Transportation difficulty | 29 | 14.5% | 26 | 8.6% | .040a |
| Baseline life-space | 200 | 64.9 (24.6) | 301 | 73.7 (24.2) | <.001a |
| Comorbidity | 200 | 2.5 (1.7) | 301 | 2.6 (1.7) | .690 |
| # Medications | 200 | 3.8 (3.2) | 301 | 4.5 (3.7) | .030a |
| GDS | 200 | 2.5 (2.4) | 301 | 2.0 (2.1) | .013a |
| MMSE | 200 | 21.8 (5.7) | 301 | 26.4 (3.5) | <.001a |
| SPPB | 200 | 6.4 (3.4) | 301 | 7.7 (3.1) | <.001a |
| Follow-up, years | 200 | 5.8 (2.7) | 301 | 6.0 (2.8) | .381 |
| Time to death, years | 99 | 3.7 (2.0) | 131 | 3.5 (2.3) | .410 |
| Mortality | 99 | 49.5% | 131 | 43.5% | .190 |
a. Psignificant at .05 level (2-tailed).
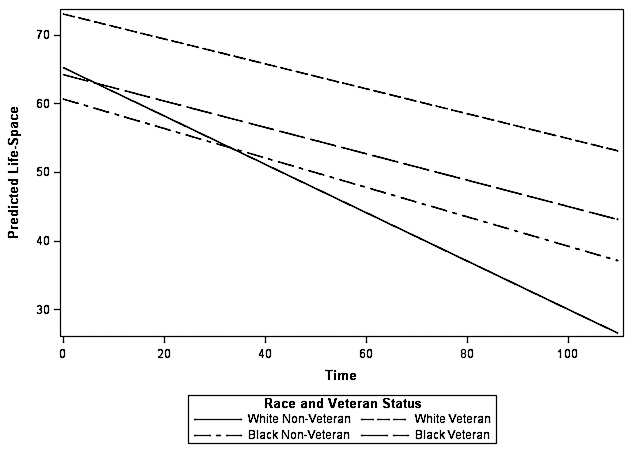
There were significant differences in race-veteran subgroups at 8.5 years (Table 2). Relative to Black veterans, there were significantly greater declines in life-space trajectories for White non-veterans (P=.009), but not for White veterans (P=.807) or Black non-veterans (P=.633). Baseline differences in life-space persisted over 8.5 years. Relative to Black veterans, White veterans had a significantly higher baseline life-space (P<.001), compared with Black non-veterans (P=.177), and White non-veterans (P=.758). Figure 1 shows the slower decline in life-space trajectory for White veterans, compared to the other race-veteran subgroups.
Table 2. UAB Study of Aging Change in life-space of male participants over time by race and veteran status .
| Effect | Estimate | Standard Error | DF | t-value | P |
| Intercept | 64.170 | 1.971 | 481 | 32.56 | <.000a |
| Time | -.192 | .035 | 286 | -5.49 | <.000a |
| Race/veteran status | |||||
| White/non-veterans | 1.033 | 3.349 | 488 | .31 | .758 |
| White veteran | 8.829 | 2.474 | 480 | 3.57 | <.001a |
| Black/non-veteran | -3.555 | 2.630 | 481 | -1.35 | .177 |
| Black/veteran | (Reference) | --- | --- | --- | --- |
| Time x race/veteran interaction | |||||
| Time x White/non-veteran | -.160 | .061 | 314 | -2.64 | .009a |
| Time x White/veteran | .011 | .043 | 282 | .24 | .807 |
| Time x Black/non-veteran | -.022 | .046 | 290 | -.48 | .633 |
| Time x Black/veteran | (Reference) | --- | --- | --- | --- |
a. P significant at .05 level (2-tailed)
Figure 1. UAB Study of Aging. Predicted Life-space by Race and Veteran Status over the course of 8.5 years. Rates of change (slope) and baseline scores (intercepts) were estimated using mixed effects models with random slope and intercept.
We found no significant differences in time to death in years across the four groups. Time to death in years for Black veterans (n=45) was 3.1 (SD=2.1) and 3.8 (SD =2.2) for Black non-veterans (n=66), compared to 3.6 (SD =2.4) for White veterans (n=86) and 3.3 (SD =1.8) for White non-veterans (n=33) (all P>.05) (data not shown). Mortality was not significant at 8.5 years between veterans and non-veterans. For veterans, mortality was 43.5%, compared to 49.5% for non-veterans (P=.189). There were also no significant differences in mortality based on race-veteran status (all P>.05). Mortality for Black veterans and Black non-veterans was 40.9% and 46.8%. For White veterans and White non-veterans, mortality was 45.0% and 55.9% (data not shown).
Discussion
Our primary objective was to examine life-space mobility of older Black and White male veterans and non-veterans in the context of CIT9 to determine the benefits of military service for older Black male veterans born in the Deep South. These men came of age during a period of intense racism and discrimination that limited opportunities for social and economic mobility over their life courses. Military service offered benefits, such as access to mortgages, educational benefits, health and disability benefits, which theoretically should have increased opportunities for better health and life-space in older age.
Our first hypothesis was supported because veterans demonstrated higher baseline life-space and slower declines than non-veterans. This finding contributes to the life-space literature because the influence of military service has not been examined in previous research. Our findings also indicated that White male veterans benefited from military service more than Black male veterans. These findings reflect CIT Axiom 2: “Disadvantage increases exposure to risk, but advantage increases exposure to opportunity.” 9 Although previous life course research found military service influenced adult achievement among WWII veterans who were young inductees, racial group differences were not examined.16 Historical data note that even though the GI Bill included the benefits noted above, the majority of Black male veterans returning from WWII to the segregated Deep South were unable to benefit from the GI Bill, primarily because of racism and discrimination.30
Regardless of the era in which Black veterans served, findings support our second hypothesis and previous research that older Blacks demonstrate lower life-space compared with older Whites,3,18 which also supports CIT Axiom 3: “Life-course trajectories are shaped by the accumulation of risk, available resources, and human agency.”9 During the lives of our participants, the United States underwent significant social changes, such as the desegregation of the Armed Forces in 1948 and the Civil Rights Movement of the 1960s. However, research indicates that Black veterans returning home from the Korean and Vietnam Wars experienced similar barriers in access to GI Bill benefits as Black WWII veterans.31 The advantage on return from the military did not result for many Black veterans. The Deep South was acutely segregated with limited opportunities for Blacks irrespective of military service. The largest difference in life-space was between White veterans and non-veterans that suggests a plausible cumulative advantage associated with being a White male veteran. White male veterans also demonstrated a slower rate of decline in their life-space than White non-veterans over 8.5 years, which further suggests a cumulative advantage.
Our second hypothesis was also supported and validated by CIT Axiom 4: “The perception of life trajectories influences subsequent trajectories.”9 Life-space can track mobility in older adults, as well as coping methods used in the maintenance of mobility in advanced age suggesting a shaping of trajectories based on “social comparisons.”18 Furthermore, because life-space reflects what people actually do, the differences in life-space scores at baseline may have been influenced by the personal expectations, “favorable life review,” as well as time and place. Compared with White veterans, Black veterans were more likely to return to adverse social conditions and were more likely to live in rural areas, which may have limited their opportunities and access to resources. The finding that Black veterans had a lower life-space than White veterans contributes to the life-space literature, especially to racial differences in life-space.
We did not find support for our third hypothesis. However, White veterans had a slower decline in life-space over time than White non-veterans. The differences in life-space trajectories between veterans and non-veterans at baseline were not sustained (accumulated) for Black male veterans compared with Black non-veterans over 8.5 years. The knifing-off and turning points that should have resulted from military service were not as beneficial to Black male veterans. This finding further supports previous research on life-space differences between Blacks and Whites.3,18 In contrast to the post-war years of Black male veterans, White male veterans returning to the Deep South were able to take full advantage of the GI Bill,31 which could have altered their life-space trajectory.
It is possible that overall findings demonstrate support for Axiom 5: “Cumulative inequality may lead to premature mortality; therefore, nonrandom selection may give the appearance of decreasing inequality in later life.”9 This could have resulted in selection bias such that Black males who participated in this study were able to participate because they were both survivors and the healthiest Blacks within the population recruited. The fact that there were no significant differences in mortality suggests that this selection bias may have occurred.
Furthermore, an examination of baseline characteristics indicates differences between Black and White males regardless of military service consistent with CIT Axiom 1: “Social systems generate inequality, which is manifested over the life course through demographic and developmental processes.” 9 These findings suggest that Black male veterans did not overcome the disadvantage experienced during the critical periods of childhood and adolescence in later life, which further suggests that the benefits of military service were influenced by not only time (pre- and post-desegregation of the Armed Forces and pre- and post-civil rights), but also place (Alabama).
Overall, these analyses provide evidence that veteran status was associated with a significantly slower decline in life-space mobility among older White male veterans in contrast to White male non-veterans. However, trajectories of life-space decline were similar for Black veterans and non-veterans. Despite inequality in factors that would have predicted more rapid declines in life-space for Black men, the life-space declines experienced by both veteran and non-veteran Black men were similar to that observed among White veterans, but significantly better than that demonstrated by White non-veterans. These data suggest that the Black men recruited for the study had factors beyond military service that protected them from showing the more rapid declines observed by White non-veteran men.
Study Limitations
There were limitations to this study. We were unable to verify military service, the number of years served, place of discharge, and the type of discharge received. Verification of place of discharge would have confirmed if a veteran returned to the Deep South immediately upon discharge. Childhood and adolescent health histories would have provided an additional perspective on the health of non-veterans, which may have limited access to the Armed Forces.
Conclusions
To the best of our knowledge, our study is the first to examine the potential benefits of military service on health and life-space mobility in late life among older Black and White veterans and non-veterans. Although military service did not lessen the effects of cumulative inequalities in the life course for Black veterans aged >65 years, it is possible that any impact on life-space and life-space trajectories based on veteran status for Blacks would have dissipated by this age. Findings demonstrated that military service has the potential to slow decline in health and mobility; however, the impact of cumulative inequality cannot be overcome by military service alone. To understand proximal and long-term effects of military service, it would be beneficial to follow life-space trajectories in a younger cohort of veterans, such as the current cohort of Afghanistan and Iraq veterans, in an era of more equitable distribution of GI benefits.
Acknowledgments
This study was supported through a Fellowship in Advanced Geriatrics, Birmingham/Atlanta Geriatric Research, Education, & Clinical Center (GRECC) and Award Numbers R01 AG15062 and P30AG031054 from the National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the US Department of Veterans Affairs or the National Institutes of Health.
Dr. McCaskill is a Fellow in Advanced Geriatrics, a Deep South Resource Center for Minority Aging Research (RCMAR) Scholar, and a John A. Hartford Veterans Affairs Social Work Scholar.
Dr. Sawyer serves as Research Advisor for Deep South RCMAR Scholars.
Dr. Kennedy is a former NIA Summer Institute Scholar and Deep South RCMAR Scholar. He has received support from the NIA (R01 AG 037561, R01 AG15062).
Ms. Williams has received funding from the NIA (R01 AG15062).
Dr. Burgio is the current Deep South RCMAR Director.
Dr. Clay is a former Deep South RCMAR Scholar and has been supported by the NIA at the National Institutes of Health (3P30AG031054-02S1), Research Supplement to Promote Diversity in Health Related Research (Supplement to the Deep South RCMAR). Dr. Clay is also the co-chair of the Deep South RCMAR Scholar Advisory Group.
Dr. Allman previously served as the Deep South RCMAR advisor.
References
- 1. Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 2. Federal Interagency Forum on Aging-Related Statistics Older Americans 2012: Key Indicators of Well-Being. Washington, DC: Federal Interagency Forum on Aging-Related Statistics; June 2012.
- 3. Allman RM, Baker PS, Maisiak RM, Sims RV, Roseman JM. Racial similarities and differences in predictors of mobility change over eighteen months. J Gen Intern Med. 2004;19(11):1118-1126. 10.1111/j.1525-1497.2004.30239.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Crowe M, Andel R, Wadley VG, Okonkwo OC, Sawyer P, Allman RM. Life-space and cognitive decline in a community-based sample of African American and Caucasian older adults. J Gerontol A Biol Sci Med Sci. 2008;63(11):1241-1245. 10.1093/gerona/63.11.1241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lynch J, Smith GD. A life course approach to chronic disease epidemiology. Annu Rev Public Health. 2005;26(1):1-35. 10.1146/annurev.publhealth.26.021304.144505 [DOI] [PubMed] [Google Scholar]
- 6. Wilson AE, Shuey KM, Elder GH Jr. Cumulative advantage processes as mechanisms of inequality in life course health. AJS. 2007;112:1886-1924. [Google Scholar]
- 7. Ferraro KF, Kelley-Moore JA. Cumulative disadvantage and health: long-term consequences of obesity? Am Sociol Rev. 2003;68(5):707-729. 10.2307/1519759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ferraro KF, Thorpe RJ Jr, McCabe GP, Kelley-Moore JA, Jiang Z. The color of hospitalization over the adult life course: cumulative disadvantage in black and white? J Gerontol B Psychol Sci Soc Sci. 2006;61(6):S299-S306. 10.1093/geronb/61.6.S299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ferraro KF, Shippee TP. Aging and cumulative inequality: how does inequality get under the skin? Gerontologist. 2009;49(3):333-343. 10.1093/geront/gnp034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dannefer D. Cumulative advantage/disadvantage and the life course: cross-fertilizing age and social science theory. J Gerontol B Psychol Sci Soc Sci. 2003;58(6):S327-S337. 10.1093/geronb/58.6.S327 [DOI] [PubMed] [Google Scholar]
- 11. O’Rand AM. The precious and the precocious: understanding cumulative disadvantage and cumulative advantage over the life course. Gerontologist. 1996;36(2):230-238. 10.1093/geront/36.2.230 [DOI] [PubMed] [Google Scholar]
- 12. Shippee TP, Wilkinson LR, Ferraro KF. Accumulated financial strain and women’s health over three decades. J Gerontol B Psychol Sci Soc Sci. 2012;67(5):585-594. 10.1093/geronb/gbs056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brotz H, Wilson E. Characteristics of military society. Am J Sociol. 1946;51(5):371-375. 10.1086/219845 [DOI] [PubMed] [Google Scholar]
- 14. Sampson RJ, Laub JH. Socioeconomic achievement in the life course of disadvantaged men: military service as a turning point, circa 1940-1965. Am Sociol Rev. 1996;61(3):347-367. 10.2307/2096353 [DOI] [Google Scholar]
- 15. Elder GH., Jr Military times and turning points in men’s lives. Dev Psychol. 1986;22(2):233-245. 10.1037/0012-1649.22.2.233 [DOI] [Google Scholar]
- 16. Elder GH Jr, Shanahan MJ, Clipp EC. When war comes to men’s lives: life-course patterns in family, work, and health. Psychol Aging. 1994;9(1):5-16. 10.1037/0882-7974.9.1.5 [DOI] [PubMed] [Google Scholar]
- 17. Baker PS, Bodner EV, Allman RM. Measuring life-space mobility in community-dwelling older adults. J Am Geriatr Soc. 2003;51(11):1610-1614. 10.1046/j.1532-5415.2003.51512.x [DOI] [PubMed] [Google Scholar]
- 18. Allman RM, Sawyer P, Roseman JM. The UAB Study of Aging: background and insights into life-space mobility among older Americans in rural and urban settings. Aging Health. 2006;2(3):417-429. 10.2217/1745509X.2.3.417 [DOI] [Google Scholar]
- 19. Sawyer P, Allman RM. Resilience in mobility in the context of chronic disease and aging: cross-sectional and prospective findings from the UAB Study of Aging. In: Fry PS, Keyes CLM, eds. New Frontiers of Resilient Aging, Life Strengths and Wellness in Late Life. New York, NY: Cambridge University Press; 310-339, 10.1017/CBO9780511763151.014. [DOI] [Google Scholar]
- 20. Bentley JP, Brown CJ, McGwin G Jr, Sawyer P, Allman RM, Roth DL. Functional status, life-space mobility, and quality of life: a longitudinal mediation analysis. Qual Life Res. 2013;22(7):1621-1632. 10.1007/s11136-012-0315-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Health Status of Rural Alabamians. Montgomery, AL: Alabama Rural Health Association; 1998. [Google Scholar]
- 22. US Census Bureau Poverty Thresholds 2000. www.census.gov/hhes/www/poverty/data/threshld/thresh00.html. Accessed March 27, 2015.
- 23. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373-383. 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 24. Sheikh J, Yesavage J. Geriatric Depression Scales: recent evidence and development of a shorter version. Clin Gerontol. 1986;5:164-174. [Google Scholar]
- 25. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189-198. 10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- 26. Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85-M94. 10.1093/geronj/49.2.M85 [DOI] [PubMed] [Google Scholar]
- 27. National Center for Health Statistics National Death Index User’s Guide. Hyattsville, MD: Centers for Disease Control and Prevention; 2000. [Google Scholar]
- 28. Brown H, Prescott R. Applied Mixed Models in Medicine. Chichester, England: Wiley; 2006, 10.1002/0470023589. [DOI] [Google Scholar]
- 29. Brown CJ, Roth DL, Allman RM, Sawyer P, Ritchie CS, Roseman JM. Trajectories of life-space mobility after hospitalization. Ann Intern Med. 2009;150(6):372-378. 10.7326/0003-4819-150-6-200903170-00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Onkst DH. “First a Negro…incidentally a veteran”: black World War Two veterans and the GI Bill of Rights in the deep south, 1944-1948. J Soc Hist. 1998;31(3):517-543. 10.1353/jsh/31.3.517 [DOI] [Google Scholar]
- 31. Herbold H. Never a level playing field: blacks and the GI Bill. J Blacks High Educ. 1994;6(6):104-108. 10.2307/2962479 [DOI] [Google Scholar]