Abstract
Objective
Treatment and control of hypertension (HTN) is a challenging issue as undiagnosed HTN prevalence seems to be high among certain ethnic groups, such as African-descendant populations. The current study attempted to measure HTN prevalence, awareness and control levels among Ghawarna, an African-descendant ethnic group living in the Jordan Valley (Al-Ghawr).
Design, Setting and Participants
A cross-sectional study was conducted in a community of Ghawarna between March and June 2013 in Ghawr Al-Mazraa Village in the southern part of the Jordan Valley. A total of 517 participants, aged >25 years, were randomly selected using cluster random sampling technique.
Main Measures
Data were collected using an interviewer-administrated questionnaire and on-location measurement of blood pressure (BP), height, and weight. Prevalence rates were compared by sex and age groups using chi-square test while backward selection logistic regression analysis was used to identify predictors of HTN.
Results
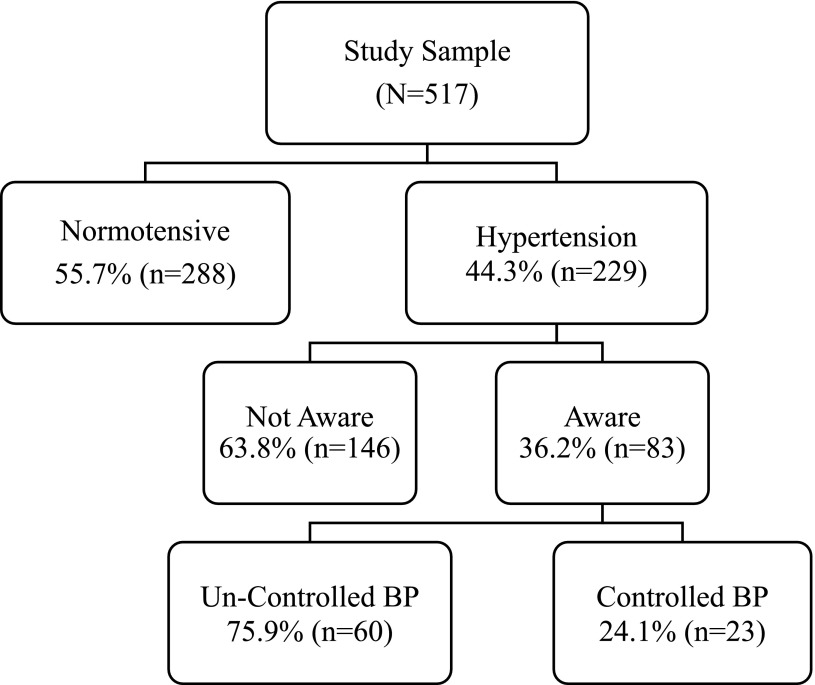
We found 229 (44.3%) of the 517 participants had HTN. Of those 229 hypertensives, 146 (28.2%) participants were discovered to have HTN for the “first time.” Only 23 of the 83 who were aware of their hypertension had their BP controlled. When we added the undiagnosed HTN (n=146) to the uncontrolled HTN (n=60), the prevalence of uncontrolled HTN became 90% (206/229). Older age, higher BMI, diabetes mellitus, and dyslipidemia were associated with having HTN.
Conclusions
HTN prevalence, awareness and control levels are alarming among Ghawarna.
Keywords: Ethnic Groups, Hypertension, Jordan
Introduction
In Jordan, the population composition includes mainly Arabs along with three major ethnic minorities. The former represents the original inhabitants in the region, and the latter includes Circassian, Chechen, and Ghawarna who originated from Cocas, Chechnya and Africa, respectively. Ghawarna are part of the African-descended Muslims1 brought to work the sugar plantations that spread in the Jordan Valley (Al-Ghawr) between 1015 and 1468.2 Since then, they resided in Al-Ghawr and were referred to as Ghawarna, in referral to the African-descendant Blacks, or brown-skinned, who are, today, the original inhabitants of the Valley.3-7
Ghawarna self-identify themselves as Jordanian Arabs, not as “Africans” or “Blacks,” and do not imagine their connection to Africa as they have adopted the Arabic identity without any identifiable African folk tradition.1 This is in contrast to the Circassian and Chechen minorities who remain endogamous and relatively isolated in terms of culture and tradition.8 Genetically, however, Ghawarna,8-11 along with Circassian and Chechen,12 represent a distinct population subgroup in Jordan. The former have a ‘genetic isolate’ that is clearly tied to Africa, but not the Eastern Mediterranean region,10 and a “high level of [genetic] homogeneity” not found among other African communities around the world11 especially sub-Saharan Africa.9 Ghawarna live in scattered rural areas (villages) in the Jordan valley and around the Dead Sea area, which is about 400 meters below sea level. Some of these villages are considered Jordanian poverty pockets13 where differences in the lifestyle and socioeconomic status compared with urban areas are evident. The term Ghawarna, therefore, encapsulates one self-defined homogenous ethnic group that shares origin, socioeconomic background, and environmental factors.
Excess burden of diseases in African-descent populations has been reported. The burden of hypertension (HTN), the most important risk factor for cardiovascular diseases (CVD),14,15 is more evident when addressing African-descent groups. HTN is the single initiating cause of death that contributes the most to the ethnic disparity in potential life-years lost between African Americans and Caucasians16 and the single disease with the greatest burden of premature death and disability among African American men.17 In part, this is because African-descent populations have the highest prevalence of HTN yet the poorest blood pressure (BP) control levels compared with all other minorities.14,18,19
Among Jordanians, where CVDs are the leading cause of adult mortality,20 national estimates of HTN among adults is high (32.3%). Awareness, treatment, and control rates are also alarming: 56.1%, 63.3% and 39.6%, respectively.21 However, reports from the Chechen and Circassian ethnic groups indicated a lower prevalence rate (23.9%).22
Lack of data on the health status of Ghawarna is not surprising given Afro-minorities’ underrepresentation in modern literature.23 This contributes to widening the recognition, management and prevention gaps between Ghawarna and other population groups. It is essential to guide public health interventions on local evidence by establishing baseline indicators on the prevalence, awareness and control levels of HTN among Ghawarna. Further, investigating HTN among this ethnic group represents a unique opportunity given their distinct genetic background and adaptation of the Arabic identity.
Methods
A cross-sectional study was conducted between March and June of 2013 in the village of Ghawr Al-Mazraa in the southern part of Al-Ghawr (Jordan Valley), which is a low-lying strip on the western border of Jordan; the climate of the area is several degrees warmer than the rest of the country. The village is around 110 km south of the capital city of Amman, is around 212 meters below sea level, and has an estimated population of more than 14,600 residents, the majority of whom are Ghawarna.1
Target Population
Ghawr Al-Mazraa residents who were aged >25 years and who self-defined as Ghawarna, ie, Blacks or Afro-Jordanians, were eligible to participate. Pregnant women were excluded.
Sampling
A detailed household map of the village was obtained from the Jordan Department of Statistics. The map divided the village into 14 census blocks; all blocks were included in the cluster random sampling procedure. Households within each block were numbered and a simple random sample of households was selected. The number of selected households was proportional to the size of the population in the block. The head of the randomly selected household was asked to participate in the study and, once consented, was asked to list the names of all adults, aged >25 years, who slept at the house on the night preceding the interview. The list was documented on the questionnaire sheet and used to randomly select one male and one female participant. Selected participants consented to participate in the study. A maximum of three visit attempts to each randomly selected individual were conducted.
Measures
Using an interviewer-administrated questionnaire, a trained researcher gathered information on socio-demographic characteristics, and history of selected behaviors (regular exercise, salt intake, smoking) and conditions (HTN, diabetes mellitus [DM], lipids, CVD). Weight and height were measured by a trained local nurse who visited the participants’ households. All anthropometric measurements were recorded by this nurse according to the latest standards of the anthropometry procedures manual of the National Health and Nutrition Examination Survey.24 A standardized method was used to measure sitting BP25 using standardized mercury sphygmomanometer with the appropriate cuff covering two-thirds of the upper left arm, at the heart level, after a 5-minute rest following the completion of the interview. The cuff was inflated at a rate of 2 to 3 mm Hg per second. Systolic and diastolic BP measures were recorded upon hearing the first sound and upon complete disappearance of Korotkoffsounds, respectively. The mean of two BP measures was computed and recorded on the data collection form.
Definitions
According to the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) guidelines,15 participants who had BP measures of ≥140 mm Hg systolic and/or ≥80 mm Hg diastolic, or reported being on anti-hypertensives, were considered as hypertensives. Participants who had been told by a physician or a health care worker that they had HTN or reported taking anti-hypertensive medication were considered to be aware of their hypertension. Participants were considered to be treated for HTN when they reported using antihypertensive medication. BP was considered controlled if systolic and diastolic BP measures were <140 and <90 mm Hg, respectively. Body mass index (BMI) was calculated as weight (kg) / (height)(m)2. Participants with calculated BMI values of ≥25 kg/m2, ≥ 30 kg/m2, or ≥40 kg/m2 were classified as overweight, obese, or morbidly obese, respectively, as per the WHO classification guidelines.26
Ethical Considerations
Our study was approved by the Institutional Review Boards (IRB) of Jordan University of Science and Technology and King Abdulla University Hospital. Written informed consent was obtained from all participants at the time of the interview. Data collection tools did not include any identifying information.
Statistical Analysis
Statistical Package for Social Science (SPSS Version 20) software was used to analyze the data. Proportions and means (SD) were reported as appropriate. Bivariate analyses were used to test the independent distribution of participants’ characteristics by HTN status using chi-square test. Multivariate logistic regression analysis was used to calculate the adjusted effect of study variables on HTN status. P <.05 were considered statistically significant. Only variables that were significantly associated with HTN at the bivariate level were included in the logistic regression model. Backwards conditional logistic regression method (entry/exit P=.05/.2) was used to identify the most significant predictors. Adjusted odds ratio (OR) and 95% confidence intervals (95% CI) were reported.
Results
Of the 511 randomly selected households, only 347 (68%) included eligible participants, and from these households, we collected data from 517 (75%) participants. Mean (SD) age and BMI were 42.9 (12.4) years and 31.4 (6.5) kg/m2, respectively. More than half of participants were aged >40 years (53.6%), 37.3% were males, 75.3% had elementary education or less and 53.6% were obese or morbidly obese. The majority of participants (96.7%) reported having health insurance. Ever cigarette smoking was reported by 31.8% of participants. Among males, 76.2% reported ever smoking compared to 5.2% among females. The most common self-reported co-morbidities were DM (11.6%) and dyslipidemia (5.0%). Only 26% and 19.3% of participants self-reported to regularly exercise and to limit their salt intake, respectively (Table 1).
Table 1. Sociodemographic and health characteristics of study participants, n=517.
| Variable | N | % |
| Age, years, n=515 | ||
| 25 to 39 | 239 | 46.4 |
| 40 to 49 | 135 | 26.2 |
| ≥50 | 141 | 27.4 |
| Males | 193 | 37.3 |
| Education level, n=515 | ||
| Illiterate | 121 | 23.5 |
| Elementary | 267 | 51.8 |
| High school | 99 | 19.2 |
| Higher Education | 28 | 5.4 |
| BMI, n=515 | ||
| Normal | 85 | 16.5 |
| Overweight | 154 | 29.9 |
| Obese | 224 | 43.5 |
| Morbidly obese | 52 | 10.1 |
| Co-morbiditiesa | ||
| Diabetes mellitus | 60 | 11.6 |
| Dyslipidemia | 26 | 5.0 |
| Coronary artery diseases | 17 | 3.3 |
| Cerebrovascular diseases | 11 | 2.1 |
| Ever smoked, n=516 | 164 | 31.8 |
| Exercise, n=516 | 134 | 26.0 |
| Limit salt intake | 100 | 19.3 |
a. Participants could have more than one co-morbidity and 429 participants did not report any.
Overall, 22% of study participants had normal blood pressure and 37% were pre-hypertensive. Blood pressure levels were categorized as stage 1 and stage 2 in 21.5% and 19.0% of participants, respectively (Table 2). The distribution of participants by HTN status, awareness and control status is shown in Figure 1. Of the total 517 participants, 229 were hypertensives. The prevalence of HTN was 44.3%, with no significant differences between males (45.6%) and females (43.5%) (P>.05). Among hypertensives (n=229), 146 participant (63.8%) had HTN for the first time, giving an overall prevalence of undiagnosed HTN of 28.2% (146/517). Awareness, among hypertensives (n=229), was 36.2%, with no significant differences between females (37.6%) and males (34.1%) (P>.05). Among aware hypertensives (n=83), the majority (91.5%, n=76) reported being treated for HTN and only 27.7% (n=23), of those who were aware, had their BP controlled. Among treated participants (n=76), BP was considered controlled in 23.7% of participants. Controlled BP status was almost equally distributed between males (23.3%) and females (24.5%) (P>.05). When undiagnosed HTN cases (n=146) were added to uncontrolled HTN cases (n=60), the prevalence of uncontrolled HTN was 90% (206/229).
Table 2. Distribution of participants by blood pressure levela, n=517.
| Blood pressure level | n | % |
| Normal blood pressure, systolic 90-119 and diastolic 60-79 mm Hg | 115 | 22.2 |
| Pre-hypertension, systolic 120-139 or diastolic 80-89 mm Hg | 193 | 37.3 |
| Stage 1 hypertension, systolic 140-159 or diastolic 90-99 mm Hg | 111 | 21.5 |
| Stage 2 hypertension, systolic ≥ 160 or diastolic ≥ 100 mm Hg | 98 | 19.0 |
a. According to the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) guidelines,15 and regardless of the use of antihypertensive medications.
Figure 1. Distribution of participants by hypertension status, awareness and controlled BP levels.
Factors that were significantly associated with HTN status (P<.05) at the bi-variate level were included in the multi-variate analysis. These included age groups, BMI, educational level, salt intake, DM, and dyslipidemia. The results of the backward conditional logistic regression analysis are presented in Table 3. Increasing age and BMI and the presence of diabetes and dyslipidemia were significantly associated with HTN. The likelihood of having HTN was significantly higher in the 40 to 49 age group (OR=2.1, 95% CI=1.3-3.4) and those aged ≥50 years (OR=8.1, 95% CI= 4.8-13.8) compared with those aged <40 years. Overweight (OR=2.3, 95% CI= 1.1 – 4.7), obese (OR=3.4, 95% CI= 1.7-6.8) and morbidly obese (OR=5.8, 95% CI= 2.4-13.8) participants were significantly more likely to be hypertensives, compared with normal weight participants. Diabetics (OR= 2.8, 95% CI=1.3-6.0) and participants with dyslipidemia were also more likely to have HTN compared with their counterparts.
Table 3. Adjusted effect of study variables on hypertension statusa.
| Variable | Adjusted OR | 95% CI |
| Age, years | ||
| <40 | Reference | -- |
| 40 to 49 | 2.1 | 1.3 - 3.4 |
| ≥ 50 | 8.1 | 4.8 - 13.8 |
| BMI | ||
| Normal, <25 | Reference | -- |
| Overweight, 25 to 29.9 | 2.3 | 1.1 - 4.7 |
| Obese, 30 to 39.9 | 3.4 | 1.7 - 6.8 |
| Morbidly obese, ≥40 | 5.8 | 2.4 - 13.8 |
| Diabetes | ||
| No | Reference | -- |
| Yes | 2.8 | 1.3 - 6.0 |
| Dyslipidemia | ||
| No | Reference | -- |
| Yes | 11.5 | 1.4 - 92.7 |
a. Backward conditional logistic regression model included the following variables: age groups, BMI, educational level, salt intake, DM, and dyslipidemia.
Discussion
Because of the Arabic identity assigned to Ghawarna, little attention has been paid to their health status. Regardless, epidemiological evidence confirms that HTN is more prevalent among African-descendant populations compared with other population subgroups,18 with low levels of detection, treatment, and control of HTN measured among Blacks27 and Afro-minorities.14 To our knowledge, our study is the first to report HTN status of an Afro-minority in the Eastern Mediterranean Region (EMR). The prevalence, awareness and control levels of HTN were investigated among Ghawarna in Ghawr Al-Mazraa village in the Jordan valley. Our findings revealed that about half (4 in 10 or 44.3%) of Ghawarna had HTN, about two thirds of hypertensives (6 in 10 or 63.8%) were not aware of their disease status, about three quarters of those aware of being hypertensive (7 in 10 or 72.3%) had uncontrolled BP levels, and that 90% of the total hypertensives, regardless of awareness status, had uncontrolled BP levels (9 in 10). These findings highlight the need for immediate public health interventions to evaluate and control BP levels among Ghawarna.
Aside from the alarming HTN prevalence, awareness and BP control levels, Ghawarna seem to have high rates of other CVD risk factors, such as obesity (53.6%) and cigarette smoking (31.8%) especially among males (76.2%). While DM and dyslipidemia seem to have low self-reported rates, the actual rates are better assessed by measuring glucose and lipid levels as the awareness rates of these conditions may mirror that of HTN. Future research should properly assess these indicators among Ghawarna, as they are crucial for a comprehensive understanding of CVD risk factors.
High HTN prevalence, awareness and control rates among Ghawarna could be attributed to the complex socio-geographic composition of the village. First, Ghawarna have a distinct genetic background that is similar to that of Africans.1,9,11 Epidemiological evidence confirms that HTN is more prevalent among Black populations compared with other population subgroups,18,28 with low levels of detection, treatment, and control of HTN measured among Blacks.14,19,27,29 This is also consistent with other studies that reported higher HTN prevalence, and poor awareness, treatment, and control rates among Afro-minorities in other parts of the world.28-30 Second, the village is one of the poverty pockets in Jordan,13 where differences in the lifestyle and socioeconomic status compared with urban areas are evident. Limited access to health care services and lack of preventive care, coupled with the silent symptoms of HTN, were reported to contribute to the lack of HTN awareness and inadequate HTN control rates in the Arab states.31
Overall, the racial, ethnic and socioeconomic characteristics of Ghawarna seem to considerably contribute to their high prevalence of HTN as well as poor awareness and control levels. Ghawarna’s overall suboptimal HTN status may be attributed to the fact that they are high-risk individuals who live in a poor health care setting. For example, heath care services provided to Ghawarna seem to have a low impact as treatment of HTN (91.5%) was not converted to BP control (23.7%). Improving HTN control rates requires an understanding of barriers to control BP. Public health interventions should incorporate individual risk assessment components and addresses inefficient health care settings.
HTN prevalence among Ghawarna was higher than that reported among Arab Jordanians (32.2%) in 200921 and among Circassian and Chechen minorities between 2008 and 2009 (23.9%).22 The reported HTN awareness rate (36.2%) was lower than the nationally reported rate (56.1%). The reported HTN treatment rate (91.5%) was higher than nationally reported (63.3%), however, BP control rate among treated patients was nationally higher (39.6% compared with 23.7%). These findings highlight the inability of local health care settings in Al-Ghawr area to effectively address HTN among Ghawarna. Inconsistencies with the national prevalence rates of HTN may be attributed to the socio-ethnic characteristics stated earlier.
Older age, higher BMI, DM, and dyslipidemia were identified as predictors for HTN among Ghawarna. These findings mirrored national studies, where older age, obesity and diabetes were significant predictors of HTN,21 as well as minority studies where older age and dyslipidemia significantly predicted having HTN.22 Such factors seem to increase the likelihood of having HTN among Jordanians regardless of their socio-ethnic differences.
Sex, in our study, was not a predictor of HTN among Ghawarna. This contradicts the reported results of the national study, where males were more likely to have HTN,21 and results of the Circassians and Chechens study, where females were more likely to have HTN.22 These contradictory findings may be attributed to the already elevated HTN rates among Ghawarna (44.3%), which could dissolve sex differences. Further, while sex differences may be due to ethnic or social differences, our study has been restricted to a single ethnic group living in one of Jordan’s poverty pockets. This created a homogeneous group in terms of social class and ethnicity where differences by sex were not evident. Still, lack of sex differences in HTN prevalence are in agreement with reports from Sub-Saharan Africa where HTN differences by sex were minimal.27
Our study has some limitations. Hypertension treatment was based only on medication use, not accounting for participants’ lifestyle activities or dietary restrictions aimed to reduce BP, which might have resulted in an underestimation of proportion of adults with HTN who received “treatment.” While generalization of results to Ghawarna may be limited, it is worth mentioning that the majority of Ghawarna actually live in scattered villages around the geographical area under study. Therefore, discrepancies in the reported prevalence rates are believed to be minimal. Regardless of the limitations, our results report for the first time findings related to one of Jordan’s ethnic groups living in a poverty pocket area.
The recognition and treatment of HTN among Ghawarna, despite known effective drug therapy and lifestyle modification programs, are suboptimal. High uncontrolled BP rates put them at higher risk of coronary heart disease, congestive heart failure, stroke, and renal failure. Simple public health interventions such as screening, early detection, and control of HTN, are critical for this population. This is especially important when considering that the risk of CVD doubles for each 20 mm Hg increase in systolic BP or 10 mm Hg increase in diastolic BP above 115/ 75 mm Hg.15 Such interventions have great potential to reduce morbidity and mortality from potentially preventable complications of HTN. Efforts to raise awareness of HTN should also stress the importance of health promotion and disease prevention as important arenas to improve the quality of life and to reduce the cost of health care among Ghawarna.
In conclusion, the current results revealed that HTN prevalence, awareness and control levels among Afro-Jordanians in Ghawr Al-Mazraa is alarming. This highlights concerns regarding HTN status of this community, and calls to increase public health efforts on prevention, diagnosis and control of HTN and its risk factors, in order to have a better health status for this important community.
Acknowledgments
Our study was funded by Jordan University of Science of Technology (JUST) grant number 92/2013.
References
- 1. Curtis EE., IV The Ghawarna of Jordan: race and religion in the Jordan Valley. Journal of Islamic Law and Culture. 2011;13(2-3):193-209. 10.1080/1528817X.2012.733136 [DOI] [Google Scholar]
- 2. Albright WF. The Jordan Valley in the Bronze Age. Annu Am Sch Orient Res. 1924;6:13-74. 10.2307/3768510 [DOI] [Google Scholar]
- 3. Shryock AJ. Popular genealogical nationalism: history writing and identity among the Balqa Tribes of Jordan. Comp Stud Soc Hist. 1995;37(02):325-357. 10.1017/S001041750001968X [DOI] [Google Scholar]
- 4. Shryock A. Tribes and the Print Trade: Notes from the Margins of Literate Culture in Jordan. AA. 1996; 98(1):26-40.
- 5. Shryock A. Nationalism and the Genealogical Imagination: Oral History and Textual Authority in Tribal Jordan. Berkeley, CA: University of California Press; 1997. [Google Scholar]
- 6. Strange GL. Palestine under the Moslems. A description of Syria and the Holy Land from A.D. 650 to 1500. 8th ed Beirut: Khayats; 1965. [Google Scholar]
- 7. Smith GA. The Historical Geography of the Holy Land: Especially in Relation to the History of Israel and of the Early Church. London: A. C. Armstrong and Son; 1902. [Google Scholar]
- 8. Dajani R, Khader YS, Hakooz N, Fatahalla R, Quadan F. Metabolic syndrome between two ethnic minority groups (Circassians and Chechens) and the original inhabitants of Jordan. Endocrine. 2013;43(1):112-119. 10.1007/s12020-012-9723-y [DOI] [PubMed] [Google Scholar]
- 9. Flores C, Maca-Meyer N, Larruga JM, Cabrera VM, Karadsheh N, Gonzalez AM. Isolates in a corridor of migrations: a high-resolution analysis of Y-chromosome variation in Jordan. J Hum Genet. 2005;50(9):435-441. 10.1007/s10038-005-0274-4 [DOI] [PubMed] [Google Scholar]
- 10. González AM, Karadsheh N, Maca-Meyer N, Flores C, Cabrera VM, Larruga JM. Mitochondrial DNA variation in Jordanians and their genetic relationship to other Middle East populations. Ann Hum Biol. 2008;35(2):212-231. 10.1080/03014460801946538 [DOI] [PubMed] [Google Scholar]
- 11. Yasin SR, Hamad MM, Elkarmi AZ, Jaran AS. African Jordanian population genetic database on fifteen short tandem repeat genetic loci. Croat Med J. 2005;46(4):587-592. [PubMed] [Google Scholar]
- 12. Barbujani G, Nasidze IS, Whitehead GN. Genetic diversity in the Caucasus. Hum Biol. 1994;66(4):639-668. [PubMed] [Google Scholar]
- 13. Jordan Department of Statistics (DOS) Report of Jordan Poverty Situation. Amman, Jordan: Department of Statistics; 2012. [Google Scholar]
- 14. Glover M, Greenlund K, Ayala C, Croft J. Racial/ethnic disparities in prevalence, treatment, and control of hypertension—United States, 1999-2002. JAMA. 2005;293(8):923-925. 10.1001/jama.293.8.923 [DOI] [Google Scholar]
- 15. Chobanian AV, Bakris GL, Black HR, et al. ; National High Blood Pressure Education Program Coordinating Committee . The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560-2572. 10.1001/jama.289.19.2560 [DOI] [PubMed] [Google Scholar]
- 16. Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. N Engl J Med. 2002;347(20):1585-1592. 10.1056/NEJMsa012979 [DOI] [PubMed] [Google Scholar]
- 17. Mensah GA, Dunbar SB. A framework for addressing disparities in cardiovascular health. J Cardiovasc Nurs. 2006;21(6):451-456. 10.1097/00005082-200611000-00007 [DOI] [PubMed] [Google Scholar]
- 18. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988-2008. JAMA. 2010;303(20):2043-2050. 10.1001/jama.2010.650 [DOI] [PubMed] [Google Scholar]
- 19. Frohlich ED. Epidemiological issues are not simply black and white. Hypertension. 2011;58(4):546-547. 10.1161/HYPERTENSIONAHA.111.178541 [DOI] [PubMed] [Google Scholar]
- 20. Centers for Disease Control and Prevention (CDC) . Assessing risk factors for chronic disease--Jordan, 2004. MMWR Morb Mortal Wkly Rep. 2006;55(23):653-655. [PubMed] [Google Scholar]
- 21. Jaddou HY, Batieha AM, Khader YS, Kanaan AH, El-Khateeb MS, Ajlouni KM Hypertension prevalence, awareness, treatment and control, and associated factors: results from a national survey, Jordan. Int J Hypertens. 2011;2011: 828-836. [DOI] [PMC free article] [PubMed]
- 22. Shishani K, Dajani R, Khader Y. Hypertension risk assessment in the largest ethnic groups in Jordan. J Immigr Minor Health. 2013;15(1):43-48. 10.1007/s10903-011-9533-y [DOI] [PubMed] [Google Scholar]
- 23. Rencher WC, Wolf LE. Redressing past wrongs: changing the common rule to increase minority voices in research. Am J Public Health. 2013;103(12):2136-2140. 10.2105/AJPH.2013.301356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. McDowell MA, Fryar CD, Ogden CL Anthropometric reference data for children and adults: United States, 1988-1994. Vital Health Stat. 2009;(249):1-68. [PubMed]
- 25. Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111(5):697-716. 10.1161/01.CIR.0000154900.76284.F6 [DOI] [PubMed] [Google Scholar]
- 26. Obesity WHO.: Preventing and Managing the Global Epidemic: Report of a WHO Consultation. WHO Technical Report Series 894. Geneva: World Health Organization, 2000. [PubMed]
- 27. Addo J, Smeeth L, Leon DA. Hypertension in sub-saharan Africa: a systematic review. Hypertension. 2007;50(6):1012-1018. 10.1161/HYPERTENSIONAHA.107.093336 [DOI] [PubMed] [Google Scholar]
- 28. Kurian AK, Cardarelli KM. Racial and ethnic differences in cardiovascular disease risk factors: a systematic review. Ethn Dis. 2007;17(1):143-152. [PubMed] [Google Scholar]
- 29. Giles T, Aranda JM Jr, Suh DC, et al. Ethnic/racial variations in blood pressure awareness, treatment, and control. J Clin Hypertens (Greenwich). 2007;9(5):345-354. 10.1111/j.1524-6175.2007.06432.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Centers for Disease Control and Prevention (CDC) . Racial/Ethnic disparities in the awareness, treatment, and control of hypertension - United States, 2003-2010. MMWR Morb Mortal Wkly Rep. 2013;62(18):351-355. [PMC free article] [PubMed] [Google Scholar]
- 31. Tailakh A, Evangelista LS, Mentes JC, Pike NA, Phillips LR, Morisky DE. Hypertension prevalence, awareness, and control in Arab countries: a systematic review. Nurs Health Sci. 2014;16(1):126-130. 10.1111/nhs.12060 [DOI] [PMC free article] [PubMed] [Google Scholar]