Abstract
Objective
To examine whether residence in ethnically segregated metropolitan areas is associated with increased diabetes risk for Latinos in the United States.
Methods
Population data from the 2005 Behavioral Risk Factor Surveillance System and the 2005 American Community Survey were used to determine whether higher levels of Latino-White segregation across metropolitan statistical areas (MSAs) in the United States is associated with increased diabetes risk among Latinos (n=7462).
Results
No significant relationship (P<.05) between levels of segregation and diabetes risk was observed.
Conclusion
The research literature examining the impact of residential segregation on health outcomes remains equivocal for Latinos.
Keywords: Segregation, Diabetes, Latinos
Introduction
Residential segregation, or the minority composition and separation of neighborhoods within a metropolitan area,1,2 may perpetuate health disparities between Latinos and Whites in the United States. Recent census data show that Latinos account for 16.9% of the nation’s population and are the second most segregated minority group.3,4 As the US Latino population grows, so too do concerns about the residential patterns of this minority group. National averages suggest that the overall segregation of Latinos over the last several decades has not changed. A review of 2010 Census data reveals that, on average, Latinos reside in metropolitan areas that are 46% Latino.5 Using common indices of segregation,6 several studies report increases in isolation for Latinos, particularly Mexicans, between 1990 and 2010.3,7 An isolation index measures the extent to which different racial/ethnic groups are exposed to each other in the same neighborhood.8 Furthermore, Latino immigrants are likely to locate in ethnic enclaves, often to ease the acculturation process.6,9-11
This spatial isolation and concentration of Latinos may have important implications for health outcomes. Specifically, segregation isolates minority groups such as African Americans and Latinos in economically disadvantaged neighborhoods.12 These areas tend to be characterized by high crime, fewer educational and employment opportunities, discriminating housing practices, and poverty.1,3,13,14 The ensuing low socioeconomic status of minorities living in these segregated areas creates racial/ethnic differences in access, quality, and utilization of health promoting resources such as healthy food or access to opportunities to engage in physical activity.1,2,14 Consequently, health outcomes are poor among low-income minority populations. Much of the literature in this area, however, focuses on Black-White segregation.
The limited research that exists on Latino segregation and health outcomes reports mixed results. Some studies indicate positive associations between Latino-White segregation and risk for obesity,15 physical inactivity,16 body mass index (BMI),17 and self-rated health.18 However, many studies show that Latinos who live in segregated areas have lower mortality rates than non-Latino Whites.19-21 This epidemiological contradiction, known as the Latino Paradox, explains the notion that Latinos have lower mortality rates than Whites,22 albeit while experiencing greater barriers to health care and higher rates of chronic conditions like diabetes.14,15,23 To this end, some studies introduce various control variables to isolate the effects of Latino status,20,24,25 and find that the apparent mortality advantage suggested by the Latino Paradox does not exist for conditions like diabetes.26
Diabetes is the fifth leading cause of death among Latinos and is 66% more likely to be diagnosed in Latinos than in Whites.27,28 Risk for diabetes is often attributed to genetics, environmental factors, and modifiable lifestyle behaviors.29,30 While these individual-level risk factors are important to our understanding of diabetes risk, population-level factors need to be explored further in order to develop policies to prevent diabetes onset. This is especially true for Latinos, as studies suggest that diabetes risk among Latinos is heavily influenced by population-level factors associated with segregation such as the availability of healthy food outlets and access to quality health care services in residential areas.27,31 For these reasons, our study examined the association between segregation and risk of diabetes among Latinos from a population perspective. Specifically, we examined individual-level characteristics thought to predispose individuals to diabetes (eg, obesity and exercise), as well as residential characteristics (eg, segregation and population size). Given the state of current research, we hypothesized both individual and residential indicators interact to produce ethnic differences in diabetes risk.
Methods
Data Sources and Sample
The 2005 Behavioral Risk Factor Surveillance System (BRFSS), supported by the Centers for Disease Control and Prevention, served as our primary data source. The BRFSS is an annual US-based telephone survey, measuring health outcomes and risk factors of the non-institutionalized population.32 The BRFSS also includes geographically referenced data for Metropolitan Statistical Areas (MSAs) with samples of 500 or more individuals to permit the assignment of segregation indices for analysis. The US Bureau of the Census defines an MSA as an area that contains a city or urbanized area with 50,000 or more inhabitants.33
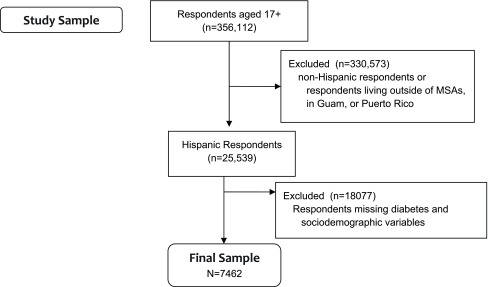
The 2005 American Community Survey (ACS), which is conducted by the US Census Bureau, was also used in our research. On a monthly basis, the ACS surveys households in areas of the US with at least 65,000 people regarding socioeconomic characteristics such as race and income. The 2005 wave yielded a response rate of 97.3% with a working sample of 1,924,527 respondents.34 The ACS was merged with the BRFSS in order to derive socioeconomic characteristics of MSAs for participants included in our sample. In addition, segregation data from the Racial Residential Project at the University of Michigan was used to assign levels of segregation to respective metropolitan areas.35 The BRFSS is administered by local governments in the 50 states, the District of Columbia, Guam and Puerto Rico, and the 2005 wave includes 356,112 respondents aged >17 years, with a median state-level response rate of 51.1%.36 After excluding non-Hispanic respondents and those living outside of MSAs or in Guam or Puerto Rico, 25,539 respondents remained. Of those, 7,462 responded to all BRFSS questions used in this study and comprise our working sample. (Figure 1)
Figure 1. Participant inclusion/exclusion criteria, Behavioral Risk Factor Surveillance Survey, 2005.
A study of non-response bias comparing data from the year 2000 BRFSS and Decennial Census revealed that racial/ethnic minorities, women, and younger people were less likely to respond to the BRFSS.37 Any over-representation of White, non-Hispanic respondents cannot influence the results here because the sample is limited to Latinos; women are in fact over-represented in our working sample (Table 1) and controlling for sex should counter any resulting biases. While the under-representation of young people favors finding diabetes in our sample given it is not a young person’s disease, that source of response bias should not bias the coefficients. The ACS was used to generate MSA-level data, so does not cause any further missing values.
Table 1. Individual and metropolitan-level descriptive statistics.
| Mean or % | SD | |
| Diabetes diagnosis | ||
| Yes | 9.1% | |
| No | 90.9% | |
| Individual SES | ||
| Education level | ||
| Less than high schoola | 27.3% | |
| High school graduate | 3.3% | |
| Some college | 23.5% | |
| Graduated college | 18.9% | |
| Household income | ||
| Less than $15,000a | 18.7% | |
| $15,000 - $25,000 | 3.5% | |
| $25,000 - $35,000 | 15.4% | |
| $35,000 - $50,000 | 13.2% | |
| > $50,000 | 22.3% | |
| Employed | 67.7% | |
| Individual Controls | ||
| Body mass index | ||
| Body mass index categories | 27.8 | 5.9 |
| Underweight | 1.4% | |
| Normal weighta | 31.6% | |
| Overweight | 38.6% | |
| Obese | 28.4% | |
| Smoker status | ||
| Current smokera | 17.7% | |
| Former smoker | 19.9% | |
| Never smoked | 62.3% | |
| Physical activity (minutes of moderate activity) | 53.3 | 73.5 |
| Insured | 69.1% | |
| Age | 41.8 | 15.01 |
| Sex | ||
| Malea | 39.6% | |
| Female | 60.4% | |
| Marital status | ||
| Never married, separated | 38.6% | |
| Married, cohabitatinga | 61.4% | |
| Fruit/Vegetable Intake | ||
| Less than 5 times per daya | 77.9% | |
| 5+ times per day | 22.1% | |
| General health | ||
| Excellent | 17.3% | |
| Very good | 23.9% | |
| Good | 34.4% | |
| Fair | 18.8% | |
| Poora | 5.7% | |
| Segregation measuresb | ||
| Nonsegregateda | 4.0% | |
| Segregated | 95.0% | |
| Hypersegregated | 1.0% | |
| Area SES | ||
| Total MSA population | .15 | .18 |
| Proportion in poverty | .14 | .049 |
| Hispanic population | 701448.8 | 806196.5 |
n=7,462.
n for MSA = 198.
a. Indicates a category used as the base category for logistic regression.
b. Summary is at MSA level.
c. .55 cutoff, Wilkes’ Index.
Outcome Measure
Diabetes risk was measured using a question from the BRFSS that asks respondents, “Have you ever been told by a doctor that you have diabetes?” (Respondents were not asked to differentiate between diabetes type, eg, type 1 vs type 2).
Exposure Measures
Segregation
According to Massey and Denton,12 there are five distinct but complimentary measures of minority residential segregation: evenness, exposure, centralization, clustering and concentration. Each measure taps into a slightly different construct of segregation, and all have been used to model diabetes care38 and other health outcomes such as obesity.11 From these measures, three distinct types of segregated environments are constructed. Hypersegregated areas correspond to MSAs that score .55 or higher on at least four of five segregation measures. Segregated areas score .55 or higher on one, two, or three of the five measures of segregation. Lastly, nonsegregated areas are those MSAs that did not score high on any of the segregation measures.
Covariates
Sociodemographic and health information served as controls in the analyses. At the individual level, socioeconomic status was captured using measures of education, employment and income from the BRFSS. Education was divided into four categories: less than high school, high school graduate, some college and graduated college. Income was constructed based on total household income, excluding income from interest, dividends, and other investments. This measure included other income for each person such as disability assistance, social security, and public assistance, which are not necessarily from earnings, but is still contributed to the household. A series of dummy variables were used with the categories less than $15,000, $15,000 to $25,000, $25,000 to $35,000, $35,000 to $50,000, and more than $50,000. Employment status was dichotomized based on whether or not respondents indicated they worked full- or part-time during the previous year.
Self-reported health measures included body mass index (BMI), smoker status, levels of physical activity, fruit and vegetable intake and insurance status. BMI, as a proxy for adiposity, is based on height and weight that applies to both adult men and women. Four categories of BMI were created using the CDC’s definition of BMI that correspond with underweight, normal weight, overweight and obese.39 Physical activity was defined as the number of days per week respondents perform at least 10 minutes of exercise excluding work- related activities. Fruit/vegetable intake was assessed using self-report by asking whether the respondent ate five or more fruit and vegetable servings per day. Insurance status assessed whether or not the respondent had any kind of public or private health insurance. Smoker status was measured with a series of dummy variables characterize respondents as current smokers, former smokers or nonsmokers at time of interview.
Demographic Controls
Age at time of survey was measured in complete years. The sex of the respondent also served as a control measure. Marital status was categorized as either currently in a relationship (ie, married, coupled with an unmarried partner) or currently not in a relationship (ie, never married, separated, divorced, widowed).
Area Controls
Metropolitan characteristics were used as control variables to examine the effect of segregation on diabetes for Latinos. These measures were linked to the MSA the respondent resided in during 2005. The first is population size, which is logged. The proportion of residents who are below the poverty line was also used as a control measure. To account for the racial composition of MSAs, the proportion of Whites in the MSA was included. These covariates were derived from the 2005 ACS estimates and were merged onto the BRFSS data file using 6-digit MSA codes that are present in both the ACS and the BRFSS.
Statistical Analysis
Multi-level linear models were constructed using the PROC GLIMMIX procedure in the SAS 9.1 statistical software program. A random intercept model with a random effect at the MSA level was used. Chi-square and t-tests were used to assess associations between ethnicity (Latino) and covariates used in the analysis.
Results
Table 1 shows the majority of individuals in the sample of Latinos (90.9%) reported that they had not been diagnosed with diabetes. The sample included 7,462 persons with an average age of 41.8 years. Of those sampled, 60.4% were female and 61.4% were currently in a relationship (married or cohabitating). While 67.7% of individuals were employed, other socioeconomic characteristics suggested that individuals from this sample came from slightly disadvantaged backgrounds. Less than half (42.4%) had any college experience, and only 22.3% earned a household income >$50,000. The percentage of households in poverty was 14% and the percentage of uninsured individuals was 30.9%. Descriptive statistics further show that nearly 95% of Latinos in the study lived in segregated communities. In terms of health behavior, the majority (77.9%) of respondents reported that they consumed <5 servings of fruits/vegetables daily. The average time spent engaging in physical activity per week was less than one hour (53.3 minutes per week), and approximately 67% were overweight or obese.
Comparative descriptive statistics and tests for differences across respondents reporting or not reporting diabetes are provided in Table 2, with Pvalues from Chi-squared tests of association for categorical variables and from t-tests for continuous variables. The average body mass index (BMI) among individuals who reported having diabetes exceeds that for non-diabetic individuals. On average, the BMI for individuals with diabetes was 4.1 units higher than the BMI for non-diabetics. Additionally, individuals reporting a diabetes diagnosis were more likely to be in fair or poor health. Of the 681 individuals in the sample diagnosed with diabetes, 34.65% were in fair health compared with 17.17% of the 6,781 individuals without diagnoses of diabetes. The percentage of people with poor health totaled 22.47% for diabetics and only 4.06% for non-diabetics respectively.
Table 2. Comparative descriptive statistics for diabetes diagnosis, Behavioral Risk Factor Surveillance System, Hispanic participants, 2005.
| No self-report of diabetes diagnosis | Self-reported diabetes diagnosis | ||
| Covariate | Mean (SD) or n (%) | Mean (SD) or n (%) | Pb |
| Diabetes | |||
| Diabetes diagnosis | 6781 (9.87%) | 681 (9.13%) | |
| Individual SES | |||
| Educational level | <.001 | ||
| Less than high schoola | 1803 (88.64%) | 231 (11.36%) | |
| High school graduate | 2049 (9.62%) | 212 (9.38%) | |
| Some college | 1608 (91.57%) | 148 (8.43%) | |
| Graduated college | 1321 (93.62%) | 90 (6.38%) | |
| Household income | <.001 | ||
| <$15,000a | 1189 (85.05%) | 209 (14.95%) | |
| $15,000 to $25,000 | 2073 (91.20%) | 200 (8.80%) | |
| $25,000 to $35,000 | 1063 (92.76%) | 83 (7.24%) | |
| $35,000 to $50,000 | 908 (92.37%) | 75 (7.63%) | |
| >$50,000 | 1548 (93.14%) | 114 (6.86%) | |
| Employed | <.001 | ||
| Yes | 4750 (93.95%) | 306 (6.05%) | |
| No | 2031 (84.41%) | 375 (15.59%) | |
| Individual Controls | |||
| Body mass index | 27.45 (5.61) | 31.55 (7.47) | <.001 |
| Body mass index categories | <.001 | ||
| Underweight | 99 (94.29%) | 5 (5.71%) | |
| Normal weighta | 2268 (96.26%) | 88 (3.74%) | |
| Overweight | 2659 (92.36%) | 220 (7.64%) | |
| Obese | 1755 (82.70%) | 367 (17.30%) | |
| Smoker Status | <.001 | ||
| Current smokera | 1216 (91.84%) | 108 (8.16%) | |
| Former smoker | 1271 (85.53%) | 215 (14.47%) | |
| Never smoked | 4294 (92.30%) | 358 (7.70%) | |
| Physical activity (minutes of moderate activity) | 53.76 (73.07) | 49.08 (77.72) | .132 |
| Insured | <.001 | ||
| Yes | 4619 (89.58%) | 537 (1.42%) | |
| No | 2162 (93.76%) | 144 (6.24%) | |
| Age | 4.53 (14.52) | 54.83 (13.62) | <.001 |
| Sex | .619 | ||
| Male | 2682 (9.67%) | 276 (9.33%) | |
| Female | 4099 (91.01%) | 405 (8.99%) | |
| Marital status | .081 | ||
| Never married, separated | 2596 (9.14%) | 284 (9.86%) | |
| Cohabiting, marrieda | 4185 (91.34%) | 397 (8.66%) | |
| Fruit and vegetable consumption | .877 | ||
| Less than 5 times per daya | 5285 (9.90%) | 529 (9.10%) | |
| 5 or more times per day | 2596 (9.14%) | 284 (9.86%) | |
| General Health | <.001 | ||
| Excellent | 1258 (97.67%) | 30 (2.33%) | |
| Very good | 1707 (95.79%) | 75 (4.21%) | |
| Good | 2377 (92.71%) | 187 (7.29%) | |
| Fair | 1164 (83.14%) | 236 (16.86%) | |
| Poora | 275 (64.25%) | 153 (35.75%) |
a. Indicates a category used as the base category for logistic regression.
b. Ps are from Chi-square test of association for categorical variables and from t-test for continuous variables.
Results from these simple tests also showed statistically significant differences in several individual-level factors between those who self-reported diabetes diagnosis and those who did not. The individuals most likely to have diabetes included a higher proportion of people who formerly smoked, had less than a high school education, and made <$15,000 annually. Those with diabetes also tended to be older than those without diabetes. Compared with people without diabetes, people diagnosed with the disease were less likely to be employed, but more likely to be insured.
Table 3 summarizes the regression analysis. Specifically, being employed and having an annual income >$15,000 had a protective effect on the risk for diabetes for Latinos. Those who were unemployed were significantly more likely to be diagnosed with diabetes. Being a female also served as a protective factor. The results further suggest that the likelihood of being diagnosed with diabetes is significantly less for uninsured individuals compared with those with insurance, while obesity was associated with increased risk. Neither higher levels of physical activity or fruit and vegetable consumption were found to be significantly associated with reduced diabetes risk. Increasing age was associated with an increase in diabetes risk (P<.05).
Table 3. Standardized regression coefficients for hierarchical linear modeling of the effects of individual and metropolitan measures on diabetes diagnosis.
| Hispanic | |
| Individual-level measures | |
| Education (<high school) | |
| High school graduate | .005 |
| Some college | .005 |
| Graduated college | -.011 |
| Annual household income (< $15,000) | |
| $15,000 - $25,000 | -.04c |
| 25,000 - $35,000 | -.05c |
| $35,000 - $50,000 | -.04c |
| > $50,000 | -.05c |
| Employed (Yes) | |
| No | .04c |
| BMI (Normal weight) | |
| Underweight | .02 |
| Overweight | .02b |
| Obese | .11c |
| Minutes of physical activity per week | -.00 |
| Fruit/vegetable intake (< 5 times per day) | |
| 5+ times per day | .003 |
| Insurance (Yes) | |
| No | -.02a |
| Smoker status (current smoker) | |
| Former smoker | -.005 |
| Never smoked | .022a |
| Age | .004c |
| Sex (Male) | |
| Female | -.014a |
| Marital status (currently in a relationship) | |
| Currently not in a relationship | -.003 |
| Metropolitan-level measures | |
| Segregation (segregated) | -.008 |
| Nonsegregated | .00 |
| Hypersegregated | |
| Log population size | .002 |
| % Households in poverty | -.007 |
| % Hispanic in MSA | .01 |
| n | 7244 |
a P<.05.
b P<.01.
c P<.001.
At the MSA level, higher levels of segregation were not significantly associated with diabetes risk, even at the P<.05 level. Nor were larger populations, a higher concentration of poverty or a larger number of Latinos in the MSA significantly related to diabetes risk.
Discussion
Previous studies of Latinos have found that higher levels of segregation confer benefits against obesity,11 and other health outcomes.18,40 Our study, on the contrary, found no significant association between residential segregation among Latinos and diabetes risk. It is possible that, while measures of segregation in the United States typically reflect isolation from resources and other racial ethnic groups, this isolation may not influence Latinos in the same way as other minority groups. Specifically, immigrants comprise a large number of Latinos in the United States who may reap benefits from being in enclaves that reinforce ethnic identity and aid the assimilation process.41,42 In conjunction with the findings reported here, a reasonable conclusion may be that, while residential segregation may be related to adverse health effects among some minority groups, such as African Americans, those adverse effects may be limited among Latinos in the United States.43
Among the significant findings, diabetes risk was positively related to unemployment and to health insurance coverage. Given that unemployment includes all respondents not employed, and that Medicare provides insurance to older respondents, it is possible that these findings are a statistical artifact of post-retirement age respondents being more likely to report diabetes. While this is possible, note that the findings hold in the regression results, which control directly for age, and that age is significantly and positively correlated with diabetes risk (Table 3). Instead, it seems likely that employed individuals enjoy greater resources and perhaps greater health in general, and that diabetes diagnoses are more likely among those with greater access to health care, as proxied by health insurance coverage.
Our study has several limitations. The BRFSS is cross-sectional, so no causal inferences can be drawn. The data were collected over the telephone, which may omit populations, such as the poor, without access to a telephone. The key dependent variable, diabetes diagnosis, is self-reported and not based on any medical records or physical examination. Also, the analysis was not able to divide the sample into individuals with type 1 or type 2 diabetes. There were a large number of uninsured in our sample, which may be related to the dependent measure because it could influence awareness of diabetes. While the focus on Latinos was intentional, the study was not able to make inter-ethnic comparisons within the Latino community, which might identify differences across Latinos with historical ties to Mexico, Puerto Rico, or other areas in Latin America and the Caribbean. Future research could expand on this work by making these distinctions and by including other races and ethnicities.
There are further limitations in terms of the spatial data. The geographic data were aggregated to the metropolitan level, but the research could have been more powerful if the spatial level was more localized, such as a community or neighborhood. While five separate measures of segregation were used, they had to be collapsed into a trichotomous variable to indicate if areas were segregated, hypersegregated or non-segregated. Because of this coding strategy, variation in segregation was compressed and, perhaps more troubling, there were few non-segregated areas identified in these data, limiting the variation available to statistically explain diabetes risk.
Conclusions
There are two important implications of this research. First, other research has indicated a strong deleterious segregation effect on health across many disadvantaged racial and ethnic groups. The fact that this research found no such relationship between segregation and health among Latinos suggests that there could be a self-segregation effect that may be protective or at least not harmful to health among this group. Second, given the high prevalence of diabetes among Latinos in the United States compared with Whites,28 future studies could either consider more finely grained geographic data or alternative socio-environmental factors to explain that difference.44,45
References
- 1. Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404-416. 10.1016/S0033-3549(04)50068-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian SV. Future directions in residential segregation and health research: a multilevel approach. Am J Public Health. 2003;93(2):215-221. 10.2105/AJPH.93.2.215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. . Iceland J, Weinberg DH, Steinmetz E Racial and Ethnic Residential Segregation in the United States: 1980-2000. Washington, DC: US Bureau of the Census, August 2002. https://www.census.gov/prod/2002pubs/censr-3.pdf. Accessed June 2, 2015.
- 4. . US Bureau of the Census State and County Quick Facts. Washington, DC: US Bureau of the Census, April 2015. http://quickfacts.census.gov/qfd/states/00000.html. Accessed June 2, 2015.
- 5. Logan JR. The persistence of segregation in the 21st century metropolis. City Community. 2013;12(2):160-168. 10.1111/cico.12021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wilkes R, Iceland J. Hypersegregation in the twenty-first century. Demography. 2004;41(1):23-36. 10.1353/dem.2004.0009 [DOI] [PubMed] [Google Scholar]
- 7. . Logan JR, Turner RN Hispanics in the United States: Not Only Mexicans. March 2013. http://www.s4.brown.edu/us2010/Data/Report/report03202013.pdf. Accessed June 2, 2015.
- 8. White K, Borrell LN. Racial/ethnic residential segregation: framing the context of health risk and health disparities. Health Place. 2011;17(2):438-448. 10.1016/j.healthplace.2010.12.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Iceland J, Scopilliti M. Immigrant residential segregation in U.S. metropolitan areas, 1990-2000. Demography. 2008;45(1):79-94. 10.1353/dem.2008.0009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Viruell-Fuentes EA, Miranda PY, Abdulrahim S. More than culture: structural racism, intersectionality theory, and immigrant health. Soc Sci Med. 2012;75(12):2099-2106. 10.1016/j.socscimed.2011.12.037 [DOI] [PubMed] [Google Scholar]
- 11. Kershaw KN, Albrecht SS, Carnethon MR. Racial and ethnic residential segregation, the neighborhood socioeconomic environment, and obesity among Blacks and Mexican Americans. Am J Epidemiol. 2013;177(4):299-309. 10.1093/aje/kws372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Massey DS, Denton NA. Hypersegregation in U.S. metropolitan areas: black and Hispanic segregation along five dimensions. Demography. 1989;26(3):373-391. 10.2307/2061599 [DOI] [PubMed] [Google Scholar]
- 13. Kramer MR, Hogue CR. Is segregation bad for your health? Epidemiol Rev. 2009;31(1):178-194. 10.1093/epirev/mxp001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. . White K, Haas JS, Williams DR Elucidating the role of place in health care disparities: the example of racial/ethnic residential segregation. Health Services Research. 2012;47(3.2): 1278-1299. [DOI] [PMC free article] [PubMed]
- 15. Wen M, Maloney TN. Latino residential isolation and the risk of obesity in Utah: the role of neighborhood socioeconomic, built-environmental, and subcultural context. J Immigr Minor Health. 2011;13(6):1134-1141. 10.1007/s10903-011-9439-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mellerson J, Landrine H, Hao Y, Corral I, Zhao L, Cooper DL. Residential segregation and exercise among a national sample of Hispanic adults. Health Place. 2010;16(3):613-615. 10.1016/j.healthplace.2009.12.013 [DOI] [PubMed] [Google Scholar]
- 17. Do DP, Dubowitz T, Bird CE, Lurie N, Escarce JJ, Finch BK. Neighborhood context and ethnicity differences in body mass index: a multilevel analysis using the NHANES III survey (1988-1994). Econ Hum Biol. 2007;5(2):179-203. 10.1016/j.ehb.2007.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lee MA, Ferraro KF. Neighborhood residential segregation and physical health among Hispanic Americans: good, bad, or benign? J Health Soc Behav. 2007;48(2):131-148. 10.1177/002214650704800203 [DOI] [PubMed] [Google Scholar]
- 19. Sorlie PD, Backlund E, Johnson NJ, Rogot E. Mortality by Hispanic status in the United States. JAMA. 1993;270(20):2464-2468. 10.1001/jama.1993.03510200070034 [DOI] [PubMed] [Google Scholar]
- 20. Abraído-Lanza AF, Dohrenwend BP, Ng-Mak DS, Turner JB. The Latino mortality paradox: a test of the “salmon bias” and healthy migrant hypotheses. Am J Public Health. 1999;89(10):1543-1548. 10.2105/AJPH.89.10.1543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Inagami S, Borrell LN, Wong MD, Fang J, Shapiro MF, Asch SM. Residential segregation and Latino, black and white mortality in New York City. J Urban Health. 2006;83(3):406-420. 10.1007/s11524-006-9035-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Markides KS, Coreil J. The health of Hispanics in the southwestern United States: an epidemiologic paradox. Public Health Rep. 1986;101(3):253-265. [PMC free article] [PubMed] [Google Scholar]
- 23. Ruiz JM, Steffen P, Smith TB. Hispanic mortality paradox: a systematic review and meta-analysis of the longitudinal literature. Am J Public Health. 2013;103(3):e52-e60. 10.2105/AJPH.2012.301103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Swenson CJ, Trepka MJ, Rewers MJ, Scarbro S, Hiatt WR, Hamman RF. Cardiovascular disease mortality in Hispanics and non-Hispanic whites. Am J Epidemiol. 2002;156(10):919-928. 10.1093/aje/kwf140 [DOI] [PubMed] [Google Scholar]
- 25. Hunt KJ, Resendez RG, Williams K, Haffner SM, Stern MP, Hazuda HP. All-cause and cardiovascular mortality among Mexican-American and non-Hispanic White older participants in the San Antonio Heart Study- evidence against the “Hispanic paradox”. Am J Epidemiol. 2003;158(11):1048-1057. 10.1093/aje/kwg249 [DOI] [PubMed] [Google Scholar]
- 26. Palloni A, Arias E. Paradox lost: explaining the Hispanic adult mortality advantage. Demography. 2004;41(3):385-415. 10.1353/dem.2004.0024 [DOI] [PubMed] [Google Scholar]
- 27. . Centers for Disease Control and Prevention National Diabetes Fact Sheet: National Estimates and General Information on Diabetes and Prediabetes in the United States. Atlanta, GA: Centers for Disease Control and Prevention, 2011. http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Accessed June 2, 2015.
- 28. . Centers for Disease Control and Prevention Fact Sheet Prevalence of Diabetes among Hispanics in Six U.S. Geographic Locations. Atlanta, GA: Centers for Disease Control and Prevention, 2009. http://www.cdc.gov/diabetes/pubs/pdf/hispanic.pdf. Accessed December 1, 2009.
- 29. Zimmet PZ, McCarty DJ, de Courten MP. The global epidemiology of non-insulin-dependent diabetes mellitus and the metabolic syndrome. J Diabetes Complications. 1997;11(2):60-68. 10.1016/S1056-8727(96)00090-6 [DOI] [PubMed] [Google Scholar]
- 30. . International Diabetes Federation IDF Diabetes Atlas (6th Edition). Brussels, Belgium: International Diabetes Federation, 2013. http://www.idf.org/sites/default/files/EN_6E_Atlas_Full_0.pdfAccessed June 2, 2015.
- 31. Chaufan C, Davis M, Constantino S. The twin epidemics of poverty and diabetes: understanding diabetes disparities in a low-income Latino and immigrant neighborhood. J Community Health. 2011;36(6):1032-1043. 10.1007/s10900-011-9406-2 [DOI] [PubMed] [Google Scholar]
- 32. Mokdad AH, Stroup DF, Giles WH; Behavioral Risk Factor Surveillance Team . Public health surveillance for behavioral risk factors in a changing environment. Recommendations from the Behavioral Risk Factor Surveillance Team. MMWR Recomm Rep. 2003;52(RR-9):1-12. [PubMed] [Google Scholar]
- 33. . US Bureau of the Census Metropolitan and Micropolitan Statistical Areas. Washington, DC: US Bureau of the Census, February 2013. http://www.census.gov/population/metro/about/. Accessed June 2, 2015.
- 34. . US Bureau of the Census American Community Survey: Survey Methodology Main. Washington, DC: US Bureau of the Census, December 2014. http://www.census.gov/acs/www/methodology/methodology_main. Accessed, June 2, 2015.
- 35. . Farley R. Racial Residential Segregation: Census 2000. Findings. Ann Arbor, MI: University of Michigan. http://enceladus.isr.umich.edu/race/racestart.asp. Accessed June 2, 2015.
- 36. . Centers for Disease Control and Prevention 2005. Behavioral Risk Factor Surveillance System: Summary Data Quality Report. Atlanta, GA: Centers for Disease Control and Prevention, August 2006. http://www.cdc.gov/brfss/annual_data/2005/pdf/2005summarydataqualityreport.pdf. Accessed June 2, 2015.
- 37. Schneider KL, Clark MA, Rakowski W, Lapane KL. Evaluating the impact of non-response bias in the Behavioral Risk Factor Surveillance System (BRFSS). J Epidemiol Community Health. 2012;66(4):290-295. 10.1136/jech.2009.103861 [DOI] [PubMed] [Google Scholar]
- 38. Chan KS, Gaskin DJ, Dinwiddie GY, McCleary R. Do diabetic patients living in racially segregated neighborhoods experience different access and quality of care? Med Care. 2012;50(8):692-699. 10.1097/MLR.0b013e318254a43c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. . NHLBI Obesity Education Initiative Expert Panel Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. Bethesda, MD: National Heart, Lung, and Blood Institute, September 1998. http://www.nhlbi.nih.gov/files/docs/guidelines/ob_gdlns.pdf. Accessed June 2, 2015.
- 40. Eschbach K, Ostir GV, Patel KV, Markides KS, Goodwin JS. Neighborhood context and mortality among older Mexican Americans: is there a barrio advantage? Am J Public Health. 2004;94(10):1807-1812. 10.2105/AJPH.94.10.1807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wen M, Lauderdale DS, Kandula NR. Ethnic neighborhoods in multi-ethnic America, 1990–2000: resurgent ethnicity in the ethnoburbs? Soc Forces. 2009;88(1):425-460. 10.1353/sof.0.0244 [DOI] [Google Scholar]
- 42. Logan JR, Zhang W, Alba RD. Immigrant enclaves and ethnic communities in New York and Los Angeles. Am Sociol Rev. 2002;67(2):299-322. 10.2307/3088897 [DOI] [Google Scholar]
- 43. Patel RC, Baek J, Smith MA, Morgenstern LB, Lisabeth LD. Residential ethnic segregation and stroke risk in Mexican Americans: the Brain Attack Surveillance in Corpus Christi project. Ethn Dis. 2015;25(1):11-18. [PMC free article] [PubMed] [Google Scholar]
- 44. Grigsby-Toussaint DS, Lipton R, Chavez N, Handler A, Johnson TP, Kubo J. Neighborhood socioeconomic change and diabetes risk: findings from the Chicago childhood diabetes registry. Diabetes Care. 2010;33(5):1065-1068. 10.2337/dc09-1894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Knip M, Simell O. Environmental triggers of type 1 diabetes. Cold Spring Harb Perspect Med. 2012;2(7):a007690. 10.1101/cshperspect.a007690 [DOI] [PMC free article] [PubMed] [Google Scholar]