Abstract
Aims
To determine the proportion of patients who achieved blood pressure (BP) control during the 2 years following new diabetes (DM) diagnosis.
Methods
A retrospective cohort of veterans ≥18 years with hypertension who initiated a DM medication 2000 through 2007 in the Veterans Administration Mid-South Network was assembled. BP control at DM treatment initiation (baseline) was compared to BP control 6, 12, 18, and 24 months later. The VA and American Diabetes Association (ADA) definitions of control, ≤140/90 and ≤130/80 mm/Hg, respectively were primary and secondary outcomes.
Results
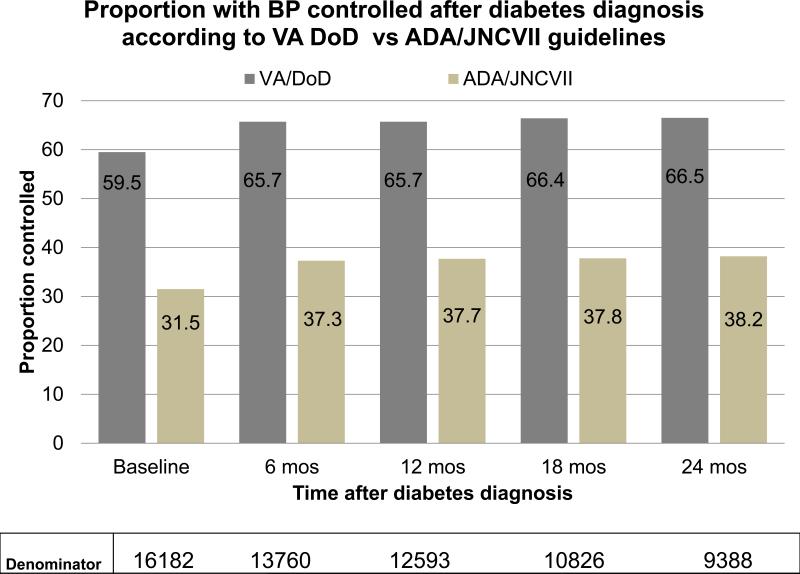
At baseline, 59.5% of 16182 patients had controlled BP according to the VA guideline (31.5% using ADA definition). Six months following initiation of DM treatment 65.7% had their blood pressure controlled (p<0.001). BP control was sustained but not further improved between 6 months and 2 years, with 66.5% controlled at 2 years following baseline. Higher initial systolic BP, black race, and hospitalization in the prior year were associated with higher likelihood of uncontrolled BP at 6 months; whereas, baseline cardiovascular disease, baseline dementia, and later year of cohort entry were associated with lower likelihood of uncontrolled BP.
Conclusion
We found an increase in BP control in the 6 months following initiation of DM treatment. However, overall BP control remained suboptimal, and with no further improvement over the next 18 months.
Keywords: Hypertension, Diabetes, Cardiovascular Disease, Guidelines
INTRODUCTION
Diabetes mellitus (DM) is an independent risk factor for cardiovascular disease (CVD) and approximately seventy percent of all deaths in patients with DM are due to CVD.[1, 2] A new diagnosis of DM signals the importance of reassessing risk factors for CVD, and achieving blood pressure (BP) control. Patients with both hypertension and DM have four times the CVD risk compared to patients without either of these conditions.[3] In recognition of this enhanced risk, the American Diabetes Association (ADA) has set a lower target BP for patients with DM.[4, 5]
There is little information on population factors associated with uncontrolled BP in patients with DM. In a retrospective cohort of 1231 patients with diabetes and isolated systolic hypertension, uncontrolled BP at follow up was associated with multiple risk factors including: baseline uncontrolled BP, use of oral hypoglycemics (compared to insulin or diet and exercise), use of three or more antihypertensive agents, and older age.[6] Among patients with diabetes surveyed through National Health and Nutrition Examination Survey (NHANES III) between 1988 and 1994, BP control was greatest among people aged 18 to 44 years and it decreased with age. Among those 65 and older, control was greater among men than women (46% vs. 28% using 140/90 mmHg as threshold). BP control was also suboptimal among non-Hispanic blacks compared to non-Hispanic whites (39% vs. 44%).[7] Other reported factors associated with uncontrolled BP included history of CVD, and congestive heart failure.[8]
Patients with newly diagnosed DM represent a target population for whom BP control may produce significant improvement in health related outcomes. Our primary aim was to determine the proportion of patients with hypertension and a new diagnosis of DM who achieve BP control during the following 2 years. Our secondary aim was to describe patient factors associated with poor BP control following a DM diagnosis. Our hypothesis was that less effort would be made to establish BP control among older versus younger age patients after the new diagnosis of DM.
PATIENTS AND METHODS
Study Design, Setting and Data Sources
A retrospective cohort study of veterans seen in the Veterans Affairs (VA) Mid South Healthcare Network (VISN 9) for care between January 1, 2000 and June 30, 2008 was assembled. This Network includes facilities in Huntington, West Virginia, Lexington and Louisville in Kentucky, Mountain Home, Memphis, Murfreesboro and Nashville in Tennessee. The institutional review board of the VA Tennessee Valley Healthcare System and the Research and Development Committee approved this study. None of the authors have noted any conflicts of interest.
The cohort was constructed from network administrative and pharmacy databases that contain electronically captured data including patient demographics, vital signs, laboratory results, and coded diagnostic (International Classification of Diseases, Ninth Revision; Clinical Modification [ICD9-CM]) and procedure information from inpatient and outpatient encounters.[9] The pharmacy files contain data from each prescription filled through the VA pharmacy including mail order prescriptions. Information included medication name, date filled, days supplied, pill number and dosage. For veterans who were also Medicare eligible, Medicare data were obtained (through 2004) through the VA Information Resource Center (VIReC) and merged with the analytical database to obtain supplemental information on race and co morbidities.[10]
Study Population
The source population was veterans aged 18 years or older who received their care at one of the healthcare systems in the VA Mid-South Network, filled any glucose lowering medication from January 1, 2000 to December 31, 2007 (including all classes of oral or injectable hypoglycemics) and had at least 1 outpatient medical encounter or filled at least 1 prescription medication in each of the 2 years prior to cohort entry. Using these criteria the source population consisted of 84,360 diabetic patients and from these persons incident users of an oral anti-diabetic drug (OAD) were delineated. Incident prescriptions were defined as the first OAD prescription filled after at least 365 days of active use of the VA pharmacy services without any glucose lowering agent (baseline period). The cohort was further restricted to patients who had date of birth and gender on file and carried a diagnosis of hypertension at baseline. Hypertension was defined as one of the following in the 365 day baseline period: 1) Prescription hypertension medication on file and ICD-9 code for hypertension (401.xx-405.99) on one outpatient visit, 2) ICD-9 codes for hypertension on two outpatient visits, or 3) ICD-9 code for hypertension on one inpatient encounter.
To examine trends in BP control, all patients who had baseline and at least one follow-up BP measurement available were included to conduct pair wise analyses. To determine factors associated with BP control at 6 months, patients missing baseline or 6 month BP outcome data were excluded along with those with a serious medical conditions identified during the baseline period which could have influenced BP treatment or control (HIV/AIDS, cancer except for nonmelanoma skin cancer, end stage liver or kidney disease, respiratory failure or organ transplant). Patients missing baseline covariate information (glycosylated hemoglobin, body mass index, serum creatinine, or demographics) were also excluded from the regression analysis. A person could re-enter the study cohort more than once if criteria were satisfied.
Study Outcome
Trends in BP control
The outcome of interest was BP control, defined according to 2 major guidelines. The VA/Department of Defense (DOD) definition for BP control is <140/90 mmHg. The American Diabetes Association (ADA) [4, 5] and the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) [11] suggests a goal for BP control among most patients with DM of <130/80 mm/Hg. BP was compared at cohort entry to 6, 12, 18, and 24 months after cohort entry. Only BPs obtained in the outpatient setting were used. If more than one value was available at the time point (± 3 months) then the measurement closest to the specific time point was used.
Factors associated with uncontrolled BP at 6 months
Uncontrolled BP was defined according to the VA/DoD national guidelines (<140/90 mmHg). For both analyses, out-of-range values were filtered and rejected (systolic BP values < 60 and > 250 mmHg, and diastolic BP values <30 and > 130 mmHg) along with probable data entry errors, including all BPs in which systolic minus diastolic BP was less than 10 mmHg. Filtered and excluded BP values were 0.2% of all BP values in the dataset. Important co-morbidities were selected a priori for inclusion in the model to predict uncontrolled BP at 6 months. Many of these covariates have been described as important determinants of BP control.
Covariates
Covariates were determined using visit codes, demographic data, and prescriptions filled in the 365 day baseline period prior to cohort entry. Study covariates included demographics [age categories (<65, 65-74, and >75 years), gender, race (white, black, other), marital status (single, married, divorced/separated)], year of cohort entry, physiologic variables collected closest to cohort entry and within the 365 day baseline period including [body mass index (BMI), glycosylated hemoglobin (HbA1c), serum creatinine, systolic BP and diastolic BP], measures of healthcare utilization in the prior year [number of outpatient visits, presence/absence of a hospitalization, and unique number of prescription medications], incident OAD prescribed and the presence/absence of important co-morbidities which may influence both the decision to treat BP and/or adherence to BP medications (cardiovascular disease, depression, and dementia, see appendix 1).
Statistical Analysis
BP control was determined according to 2 guideline cutoffs (VA /DoD <140/90 mmHg and ADA/JNC7 <130/80 mmHg). Analysis was done comparing control of BP at baseline to control at 6, 12, 18, and 24 months post DM diagnosis using a McNemar's matched-pairs analysis. All patients with available BPs at both baseline and at the time point of interest were included to prevent bias caused by differential dropout or testing.
Descriptive statistics compared patient characteristics at the time of cohort entry by age group. Relative risks (RR) with 95% Confidence intervals (CI) were calculated using Poisson regression with robust standard errors, with uncontrolled BP (≥140/90 [yes/no]) as the outcome of interest and age as the primary exposure. The unit of analysis was each episode of OAD use. Adjustment for clustering of episodes within patients and calculation of robust standard errors based on the sandwich variance estimator was preformed and adjusted for all above mentioned covariates.[12] All analyses were conducted using Stata 10.0 (Stata Corp, College Station, TX).
RESULTS
Trends in BP control
We identified 16,182 new users of OADs with baseline hypertension from 22,594 new OAD users after excluding 6412 (28.4%) without hypertension at baseline (n=6035), missing gender or date of birth (n=11), or missing a baseline BP measurement (n=366)(Figure 1). For the pairwise comparison of baseline and follow-up BP, we included 13760 at 6 months; 12593 at 12 months; 10826 at 18 months and 9388 at 2 years post DM treatment initiation.
Figure 1.
Flow of patients and prescriptions included in analysis of patients with hypertension who initate treatment for diabetes
At 6 months after new DM treatment, 65.7% of 13760 patients had BP controlled according to VA/DoD guidelines compared to 59.5% at baseline (absolute improvement 6% p<0.0001) (figure 2). Similar improvement in BP control was observed using the ADA/JNC 7 threshold (31.5% to 37% BP control at 6 months). The proportion controlled did not increase further and remained similar to the 6 month time point at 2 years (66.5% VA/DOD, 38% ADA/JNC7).
Figure 2.
Proportion who achieve BP control in the 2 years after initiating diabetes treatment according to VA/DoD guidelines and ADA/JNC 7 guidelines
Factors associated with Uncontrolled BP
The final sample for analysis of predictors of uncontrolled BP at 6 months was 8196 incident OAD users. This analysis excluded those missing covariates or with serious medical illness (Figure 1).
The study population was predominately white (85.2%) male (96.8%) and married (70%); 56% were less than 65 years of age and 16% were 75 years or older; 28% had a history of CVD. Patients were on a median of 5 (Interquartile range [IQR] 3, 9) outpatient medications, and had a median of 6 outpatient visits (IQR 3, 10) in the prior year. Baseline median BMI was 31.5 kg/m2 (IQR 28.1, 35.5), HgbA1c was 54 mmol/mol(IQR 48, 63) [7.1% (IQR 6.5, 7.9)], and median serum creatinine was 97.2 μmol/L(IQR 79.6,114.9) [1.1 mg/dL (IQR 0.9, 1.3)]. Baseline median systolic BP was 136 mmHg (IQR 126, 148 Mean137.4 standard deviation [SD] ±18.3). Median diastolic BP at baseline was 77 mmHg (IQR 69, 84 Mean 76.5 SD ±11.4). Metformin and sulfonylurea were the two most common incident OADs (53.8% and 39.7% respectively). Metformin was the most prescribed initial OAD for patients less than 65 (60.3%) whereas sulfonylurea was the most prescribed OAD for patients 75 or older (59.5%) (Table 1).
Table 1.
Characteristics of patient episodes at cohort entry
| Characteristic | Total N=8196 | Age <65 N=4797 | Age 65-74 N=2120 | Age ≥75 N=1279 |
|---|---|---|---|---|
| Gender (% Male) | 96.8 | 95% | 98.9% | 99.3% |
| Race (%) | ||||
| White | 85.2 | 80.7 | 91.7 | 91.2 |
| Black | 13.7 | 17.8 | 7.7 | 8.4 |
| Other | 1.1 | 1.5 | 0.6 | 0.3 |
| Cardiovascular Disease (%) | 28.5 | 24.1 | 32.0 | 38.9 |
| Depression (%) | 10.6 | 14.0 | 5.6 | 5.9 |
| Dementia (%) | 1.5 | 0.8 | 1.4 | 4.6 |
| Hospitalized in prior year (%) | 16.1 | 17.6 | 12.6 | 16.3 |
| Incident agent (%) | ||||
| Metformin | 53.8 | 60.3 | 50.0 | 35.9 |
| Sulfonylurea | 39.7 | 32.5 | 43.9 | 59.5 |
| Metformin+Sulfonylurea | 5.7 | 6.7 | 5.1 | 3.0 |
| Thiazolidendione | 0.8 | 0.5 | 1.0 | 1.6 |
| Marital Status (%) | ||||
| Single | 5.4 | 7.1 | 3.3 | 2.4 |
| Married | 70.0 | 63.4 | 76.7 | 83.9 |
| Divorced/Separated | 24.6 | 29.5 | 20.0 | 13.7 |
| Systolic BP (mm/Hg) Median (IQR) | 136 (126, 148) | 136(125,147) | 137(126,148) | 137(126,150) |
| Diastolic BP (mm/Hg) Median (IQR) | 77 (69, 84) | 80(72,86) | 74(67,82) | 70(62,78) |
| Outpatient Medications Median (IQR) | 5 (3,9) | 5(3,9) | 5(3,8) | 6(3,9) |
| Outpatient Visits Median (IQR) | 6(3,10) | 6(4,10) | 5(3,9) | 5(3,10) |
| Body mass index (kg/m2) Median (IQR) | 31.5 (28.1, 35.5) | 33.1(29.6,37.2) | 30.4(27.8,34.1) | 28.2(25.5,31.1) |
| HbA1c %Median (IQR) | 7.1 (6.5, 7.9) | 7.2 (6.5,8.1) | 7.1 (6.5,7.8) | 7.0 (6.4,7.6) |
| HbA1c mmol/mol Median (IQR) | 54 (48, 63) | 55 (48, 65) | 54 (48, 62) | 53 (46, 60) |
| Creatinine (mg/ dL) Median (IQR) | 1.1 (0.9, 1.3) | 1.0(0.9,1.2) | 1.1(1,1.3) | 1.2(1.1,1.4) |
| Creatinine (μmol/L) Median (IQR) | 97.2 (79.6,114.9) | 88.4(79.6,106.1) | 97.2 (88.4,114.9) | 106.1(97.2,123.8) |
Black race (adjusted RR 1.22 [95% CI 1.13, 1.32]), prior hospitalization (aRR 1.15 [95% CI 1.06, 1.25]) and baseline systolic BP (aRR 1.02 [95% CI 1.02, 1.02]) significantly increased the risk associated with uncontrolled BP at 6 months. CVD and dementia were both associated with a decreased risk of uncontrolled BP (aRR 0.90 [95% CI 0.84, 0.97] and aRR 0.73 [95% CI 0.55, 0.97], respectively). Later year of entry into the cohort was also associated with a significant increase in BP control, aRR 0.72 (95% CI 0.64, 0.81) for entering the cohort in 2007 compared to 2001.
DISCUSSION
We found that 65% of veterans had their BP controlled 6 months and 2 years following the initiation of treatment for DM when using BP threshold of <140/90 mmHg. This represents an absolute change of about 6% from baseline. Trends in BP control were similar using the ADA/JNC7 guideline of <130/80, but the proportion controlled was substantially lower. Our data demonstrate that after initiating treatment for DM, BP control improved in the immediate 6 month period but then plateaued. This suggests that providers and/or patients engage in efforts to improve control of BP in the immediate period after a new DM diagnosis. However, we found no further improvements after the initial 6 months. The reasons for this are beyond the scope of our research but could be due to decreased effort on part of providers and patients, or factors that may make blood pressure harder to control, such as weight gain secondary to DM treatment or poorer medication adherence.
The VA guidelines differ from those of the ADA and JNC 7 which recommend lower BP targets based on clinical epidemiologic data demonstrating that lower BP levels are associated with risk reduction for adverse outcomes. The VA/DoD hypertension guideline recommends a minimal target threshold based on evidence derived from randomized clinical trials (UK Prospective Diabetes Study [UKPDS] [13] and Hypertension Optimal Treatment [HOT] trial).[14] Both guidelines encourage clinicians to set target values for each patient based upon their individual circumstances, including tolerance of medications.
Two recent BP trials have demonstrated that BP thresholds of 140/90 mmHg may be preferred. Our results suggest this threshold is more achievable among patients with DM. The Action to Control Cardiovascular Risk in Diabetes (ACCORD) BP trial [15] aimed to determine the effect on CVD outcomes of lowering systolic BP to <120 mmHg. Patients with high BP and diabetes (N = 4,733) were randomized to intensive BP control (systolic BP <120 mmHg) or standard BP control (<140 mmHg). After approximately 5 years of follow-up, no statistically significant differences were noted in the primary outcome (nonfatal MI, nonfatal stroke, or cardiovascular death) between the intensive and standard BP control groups. There were numerically fewer cardiovascular events (N = 208) in the intensive group compared to the standard group (N = 237), and patients in the intensive group had fewer strokes than those assigned to the standard group (36 vs. 62 strokes). The intensive blood pressure group, however, had more adverse events, such as syncope, arrhythmias, and potassium problems, compared to the standard group (77 vs. 30 events). An observational analysis of the subgroup of 6400 patients with DM and coronary artery disease of the 22 576 participants in the International Verapamil SR-Trandolapril Study (INVEST) was also recently reported.[16] Patients were categorized by level of systolic BP control achieved. During 16 893 patient-years of follow-up, 12.7% in the tight control (systolic BP <130 mmHg) vs. 12.6% in the usual control (systolic BP 130-140 mmHg) vs. 19.8% in the uncontrolled systolic BP (systolic BP>140 mmHg) experienced the primary outcome (all cause mortality, nonfatal AMI or stroke). Both the ACCORD and the INVEST groups found that systolic BP lower than 130 mm Hg in patients with diabetes was not associated with further reduction in morbidity beyond that associated with systolic BP less than 140 mmHg. Although, these trials did not demonstrate benefits for a lower BP threshold, the study patients had mean ages of 62 and 66 years, respectively, and findings may not be applicable to younger patients.
The new diagnosis of DM is a critical time for patients and providers to re-evaluate CVD risk factors. Our findings suggest that increased efforts are needed to improve BP control among the population to at least the minimal thresholds of <140/90 mmHg. Improvement efforts should also focus on high risk populations who may be more likely to benefit from BP control. We hypothesized that age would be a predictor of uncontrolled BP. Our unadjusted analysis showed that older age was associated with poor BP control at 6 months; however, when adjusted for covariates particularly systolic BP at baseline, age was not an independent predictor of poor BP control. Thus, systolic BP at baseline plays a more important role in BP control at 6 months than age alone. Our adjusted analyses also demonstrated that black race is associated with higher risk of poor BP control. We found that dementia, CVD history, and later year of cohort entry reduced the risk of poor control. This may respectively reflect the effect of care takers who adherently provide medications to patients with dementia, or providers attentive to BP thresholds among the sickest patients (actually coded for dementia). It may also reflect additional provider and patient attention to BP control in the face of a historical CVD event, and the extra attention providers and patients gave to BP control with the publicity of newer, stricter guidelines.
Our study does have some limitations. There may be misclassification of patients with hypertension. About 25% of patients without a history of hypertension were excluded from all analyses. This is within accepted range of patients who have DM but no hypertension. In addition, some classified as having hypertension based on coding and/or drugs may also have been misclassified. This was an observational study and although we included several confounders in our model, unmeasured confounders such as the duration of hypertension and adherence to antihypertensive medications may have accounted for some of the findings. We observed significant time trends in BP control among patients in our cohort. We did adjust for year of cohort entry in our analysis, however, despite the temporal association of BP control, patients continued to have the largest gain in BP control in the first 6 months after their DM diagnosis—If trends in BP control accounted for these findings then we would have expect that BP control would continue to increase as patients remained in the cohort for up to 2 years. This did not occur, rather the proportion achieving BP control leveled off at 6 months after their DM diagnosis. Finally, our study is applicable to veteran patients from the southeast region of the United States, predominantly white and male. Data on women and minorities is limited but reflective of the VA population.
We found that for patients with hypertension, the initiation of medical treatment for DM appears to trigger attempts to improve BP control. However, among our population, BP control improvement was limited to the first 6 months after diagnosis and no further improvement occurred in the following 6 months to 2 years. We also demonstrated that the BP thresholds of <140/90 mmHg were more easily achieved than the ADA/JNC 7 threshold of 130/80 mmHg. Efforts to improve blood pressure control to at least less than 140/90 mmHg should continue after the 6 month mark and among those patients at highest risk for cardiovascular outcomes, including those who are older, black and have higher baseline blood pressure.
Supplementary Material
Table 2.
Patients with uncontrolled BP at 6 months and relative risk (RR) of uncontrolled BP
| Covariates | % Uncontrolled BP (N=2742) | % Controlled BP (N=5454) | RR (95%CI) | Adjusted RR* (95%CI) |
|---|---|---|---|---|
| Age | ||||
| <65 | 57.4 | 59.1 | Ref | Ref |
| 65-74 | 25.9 | 25.8 | 1.02 (0.96, 1.08) | 1.03 (0.95, 1.11) |
| >=75 | 16.6 | 15.1 | 1.07 (1.00, 1.13) | 1.08 (0.98, 1.18) |
| Gender | ||||
| Female | 3.5 | 2.9 | Ref | Ref |
| Male | 96.5 | 97.1 | 0.88 (0.75, 1.03) | 0.91 (0.78, 1.06) |
| Race | ||||
| White | 81.3 | 87.2 | Ref | Ref |
| Black | 17.7 | 11.7 | 1.35 (1.25, 1.45) | 1.22 (1.13, 1.32) |
| Other | 1.0 | 1.1 | 0.99 (0.73, 1.37) | 1.00 (0.73, 1.36) |
| Cardiovascular Disease | 26.1 | 29.7 | 0.89 (0.82, 0.95) | 0.90 (0.84, 0.97) |
| Depression | 9.7 | 11.0 | 0.91 (0.81, 1.00) | 0.96 (0.86, 1.07) |
| Dementia | 1.1 | 1.7 | 0.73 (0.54, .99) | 0.73 (0.55, 0.97) |
| % Hospitalized | 17.4 | 15.4 | 1.10 (1.01, 1.20) | 1.15 (1.06, 1.25) |
| Marital Status | ||||
| Single | 6.3 | 5.0 | Ref | Ref |
| Married | 67.1 | 71.4 | 0.83 (0.73, 0.93) | 0.91 (0.81, 1.03) |
| Divorced/ Separated | 26.6 | 23.6 | 0.93 (0.82, 1.06) | 0.99 (0.88, 1.13) |
| Systolic BP (mm/Hg) Median (IQR) | 144 (132,157) | 135(122,143) | 1.02(1.02,1.02) | 1.02 (1.02, 1.02) |
| Diastolic BP (mm/Hg) Median (IQR) | 79(71,87) | 76(68,82) | 1.02 (1.02,1.02) | 0.99 (0.99, 1.00) |
| Medications Median (IQR) | 5 (3,9) | 6(3,9) | 0.99 (.98,.99) | 1.00 (0.99-1.01) |
| Outpatient Visits Median (IQR) | 6 (3,10) | 6(3,10) | 0.99 (.99, 1.00) | 1.00 (0.99, 1.01) |
| Body mass index Median (IQR) | 31.4 (28.0,35.6) | 31.6 (28.2,35.5) | 0.99 (.99, 1.00) | 1.00 (0.99-1.00) |
| HgbA1c mmol/mol Median (IQR) | 55 (48,64) | 54 (48, 62) | 1.03 (1.02, 1.05) | 1.01 (0.99, 1.03) |
| Creatinine μmol/L Median (IQR) | 97.2 (79.6,114.9) | 97.2(79.6,106.1) | 1.12 (1.04,1.21) | 1.04 (0.97, 1.11) |
| Year of Cohort entry | ||||
| 2001 | 12.1 | 7.1 | Ref | Ref |
| 2002 | 14.6 | 9.4 | 0.95 (0.86, 1.06) | 0.97 (0.88, 1.08) |
| 2003 | 13.3 | 11.9 | 0.78 (0.70, 0.87) | 0.82 (0.74, 0.92) |
| 2004 | 15.8 | 15.5 | 0.73 (0.66, 0.82) | 0.81 (0.73, 0.90) |
| 2005 | 15.7 | 18.0 | 0.66 (0.59, 0.74) | 0.77 (0.69, 0.85) |
| 2006 | 14.4 | 19.1 | 0.59 (0.53, 0.67) | 0.68 (0.61, 0.76) |
| 2007 | 14.1 | 19.0 | 0.59 (0.53, 0.66) | 0.72 (0.64, 0.81) |
Uncontrolled BP defined using VA/DoD guideline threshold of <140/90 mmHg. Model adjusted for age (<65 years 65-74 years and >75 years), gender, race (white, black, other), marital status (single, married, divorced/separated)], BMI, HbA1c, serum creatinine, systolic BP and diastolic BP, number of outpatient visits, presence/absence of a hospitalization, number of prescription medications, presence/absence of cardiovascular disease, depression, and dementia and incident OAD initiated.
Acknowledgements
This project was funded in part by Contract No. 290-05-0042 from the Agency for Healthcare Research and Quality, US Department of Health and Human Services as part of the Developing Evidence to Inform Decisions about Effectiveness (DEcIDE) program. The authors of this report are responsible for its content. Statements in the report should not be construed as endorsement by the Agency for Healthcare Research and Quality or the US Department of Health and Human Services or the Veterans Health Administration. The funding sources did not participate in the planning, collection, analysis or interpretation of data or in the decision to submit for publication. The investigators had full access to the data and were responsible for the study protocol, statistical analysis plan, progress of the study, analysis, reporting of the study and the decision to publish. Dr. Roumie (04-342) was supported by a VA Career Development Awards.
References
- 1.Gilmer TP, O'Connor PJ, Manning WG, Rush WA. The cost to health plans of poor glycemic control. Diabetes Care. 1997 Dec;20(12):1847–53. doi: 10.2337/diacare.20.12.1847. [DOI] [PubMed] [Google Scholar]
- 2.Gilmer TP, O'Connor PJ, Rush WA, Crain AL, Whitebird RR, Hanson AM, et al. Predictors of health care costs in adults with diabetes. Diabetes Care. 2005 Jan;28(1):59–64. doi: 10.2337/diacare.28.1.59. [DOI] [PubMed] [Google Scholar]
- 3. [2007 August 24];Complications of Diabetes in the United States. Available from: http://www.diabetes.org/diabetes-statistics/complications.jsp.
- 4.Executive summary: Standards of medical care in diabetes--2010. Diabetes Care. Jan;33(Suppl 1):S4–10. doi: 10.2337/dc10-S004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Standards of medical care in diabetes--2010. Diabetes Care. Jan;33(Suppl 1):S11–61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duggirala MK, Cuddihy RM, Cuddihy MT, Naessens JM, Cha SS, Mandrekar JN, et al. Predictors of blood pressure control in patients with diabetes and hypertension seen in primary care clinics. Am J Hypertens. 2005 Jun;18(6):833–8. doi: 10.1016/j.amjhyper.2004.12.016. [DOI] [PubMed] [Google Scholar]
- 7.Geiss LS, Rolka DB, Engelgau MM. Elevated blood pressure among U.S. adults with diabetes, 1988-1994. Am J Prev Med. 2002 Jan;22(1):42–8. doi: 10.1016/s0749-3797(01)00399-3. [DOI] [PubMed] [Google Scholar]
- 8.Greenberg JD, Tiwari A, Rajan M, Miller D, Natarajan S, Pogach L. Determinants of sustained uncontrolled blood pressure in a national cohort of persons with diabetes. Am J Hypertens. 2006 Feb;19(2):161–9. doi: 10.1016/j.amjhyper.2005.06.032. [DOI] [PubMed] [Google Scholar]
- 9.International Classification of Diseases, Ninth Revision, Clinical Modification. Public Health Service, US Dept of Health and Human Services; Washington, DC: 1988. [Google Scholar]
- 10.Hynes DM, Koelling K, Stroupe K, Arnold N, Mallin K, Sohn MW, et al. Veterans’ access to and use of Medicare and Veterans Affairs health care. Med Care. 2007 Mar;45(3):214–23. doi: 10.1097/01.mlr.0000244657.90074.b7. [DOI] [PubMed] [Google Scholar]
- 11.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr., et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003 May 21;289(19):2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 12.Lin D, Wei L. The Robust Inference for the Cox Proportional Hazards Model. Journal of the American Statistical Association. 1989 Dec;84(408):1074–8. 1989. [Google Scholar]
- 13.Holman RR, Paul SK, Bethel MA, Neil HA, Matthews DR. Long-term follow-up after tight control of blood pressure in type 2 diabetes. N Engl J Med. 2008 Oct 9;359(15):1565–76. doi: 10.1056/NEJMoa0806359. [DOI] [PubMed] [Google Scholar]
- 14.Hansson L. The Hypertension Optimal Treatment study and the importance of lowering blood pressure. J Hypertens Suppl. 1999 Feb;17(1):S9–13. [PubMed] [Google Scholar]
- 15.Cushman WC, Evans GW, Byington RP, Goff DC, Jr., Grimm RH, Jr., Cutler JA, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. Apr 29;362(17):1575–85. doi: 10.1056/NEJMoa1001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cooper-DeHoff RM, Gong Y, Handberg EM, Bavry AA, Denardo SJ, Bakris GL, et al. Tight blood pressure control and cardiovascular outcomes among hypertensive patients with diabetes and coronary artery disease. JAMA. Jul 7;304(1):61–8. doi: 10.1001/jama.2010.884. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.