Abstract
Background
Evidence is accumulating that mindfulness training has favorable effects on psychological outcomes, but studies on physiological outcomes are limited. Patients with heart disease have a high incidence of physiological and psychological problems and may benefit from mindfulness training. Our aim was to determine the beneficial physiological and psychological effects of online mindfulness training in patients with heart disease.
Methods
The study was a pragmatic randomized controlled single-blind trial. Between June 2012 and April 2014 we randomized 324 patients (mean age 43.2 years, 53.7% male) with heart disease in a 2:1 ratio (n = 215 versus n = 109) to a 12-week online mindfulness training in addition to usual care (UC) compared to UC alone. The primary outcome was exercise capacity measured with the 6 minute walk test (6MWT). Secondary outcomes were other physiological parameters (heart rate, blood pressure, respiratory rate, and NT-proBNP), subjective health status (SF-36), perceived stress (PSS), psychological well-being (HADS), social support (PSSS12) and a composite endpoint (all-cause mortality, heart failure, symptomatic arrhythmia, cardiac surgery, and percutaneous cardiac intervention). Linear mixed models were used to evaluate differences between groups on the repeated outcome measures.
Results
Compared to UC, mindfulness showed a borderline significant improved 6MWT (effect size, meters: 13.2, 95%CI: -0.02; 26.4, p = 0.050). There was also a significant lower heart rate in favor of the mindfulness group (effect size, beats per minute: -2.8, 95%CI: -5.4;-0.2, p = 0.033). No significant differences were seen on other outcomes.
Conclusions
Mindfulness training showed positive effects on the physiological parameters exercise capacity and heart rate and it might therefore be a useful adjunct to current clinical therapy in patients with heart disease.
Trial Registration
Dutch Trial Register 3453
Introduction
In recent decades, cardiovascular disease (CVD) has become the foremost cause of health burden worldwide.[1] Especially the group of adults with congenital heart disease has increased over the last decades. While cardiovascular disease cause significant stress,[2] chronic stressors such as anxiety and depression are themselves independent risk factors for cardiovascular morbidity and mortality.[3, 4] Chronic stress can negatively affect not only quality of life, but also physiological parameters such as respiration rate, heart rate, blood pressure, inflammatory markers and brain activity.[5]
As heart rate is associated with long-term survival, patients are recommended to try reducing heart rate in the management and prevention of CVD.[6] Often medication, such as betablockers, is prescribed for this goal. Stress reduction in itself may also have a beneficial effect on heart rate and physical fitness. While the best approach to stress management is unclear, increased attention is now being paid to lifestyle interventions such as mindfulness therapy.[7, 8] Mindfulness is described as the capacity to live with open and non-judgmental awareness towards all experiences within the present moment.[9, 10] Several core features, such as meditation, yoga, and cognitive assignments, can increase the ability to accept negative experience or emotions.[11] Mindfulness therapy has been found to positively affect psychological outcomes in patients with chronic pain, obesity, hypertension, depression, anxiety and cardiovascular disease.[12–16]
We hypothesized that, besides these psychological effects, mindfulness therapy may influence heart rate, breathing patterns and blood pressure through a favorable effect on the autonomic nervous system and therefore may positively affect exercise capacity and thus long-term outcome[17]. In a randomized controlled trial (RCT), we therefore investigated the effectiveness of online mindfulness training on exercise capacity in patients with heart disease.
Methods
Study design
The current study is a single blinded, pragmatic RCT performed at the outpatient cardiology clinic of the Erasmus MC, Rotterdam, The Netherlands. Ethical approval was obtained from the Medical Ethics Committee (METC) of the Erasmus Medical Center and the study complied with the Declaration of Helsinki (S1 and S2 Texts). The study was registered at the Dutch trial register, 3453, http://www.trialregister.nl. Patients received written information about the study at home, 2–4 weeks prior to their scheduled visit to the cardiologist at the outpatient clinic. Full disclosure was given about the nature of the intervention. The current study reports the results of 3 month follow-up, which ended in July 2014, whereas the 12-month follow-up is still ongoing.
Participants
Adult patients, between 18 and 65 years of age, with diagnosed heart disease (ischemic, valvular, congenital heart disease, or cardiomyopathy) were eligible for inclusion between June 2012 and April 2014. Patients were excluded based on the following criteria: (1) planned operation or percutaneous intervention within the upcoming year; (2) inability or unwillingness to give informed consent; (3) inability to understand Dutch, inability to read or write Dutch; (4) no internet access, email, or cell phone; (5) patients who did not fill out the baseline questionnaires or did not show up for the scheduled baseline tests. All participants provided written informed consent.
Intervention
The active intervention was mindfulness training which consisted of a 12-week structured standardized online program. The training was offered in addition to usual care (UC) as provided by the treating cardiologist. All patients received a book about mindfulness by a renowned author to support the 12-week training[18]. The training was designed to be self-directed and to be easily accessible and engaging to a wide audience by keeping practice sessions and lessons short. The program teaches different meditations, self-reflection, and yoga. Furthermore, it includes practical assignments and suggestions for mindfulness in day-to-day life. The use of breath as a reminder for present moment awareness is emphasized in all meditations. The program was divided into four components (S1 Table). During the course participants also received biweekly reminders by e-mail and standardized text messages. Adherence to the intervention was monitored by whether the questions of the online program were completed. For privacy reasons, the content of the answers remained undisclosed. Both the program and the book were provided free of charge to participating patients.
Control
The control group received UC by their treating cardiologist. Treatment and frequency differs between patients, but general components are regular outpatient visits, lifestyle advice regarding nutrition, smoking, exercise, stress reduction, medication and other procedures if indicated. We chose for a pragmatic study design without a placebo online training in order to measure effectiveness rather than efficacy. This choice is justified by the likelihood of a partial placebo effect that is part-and-parcel of the training as it would be implemented in future practice.
Randomization
After a patient’s eligibility was established by one of the study investigators, written informed consent was obtained and baseline measurements were performed. Subsequently, patients were randomized according to a 2:1 ratio via dedicated computer software (ALEA®) with a block size of 12 to receive the online Mindfulness training or UC.[19] The investigator entered the patients into the computer software, but did not receive the result of the allocation. The result of the randomization procedure was sent to an independent employee (medical secretary) of the outpatient clinic, who was not involved in establishing eligibility, outcome assessment, or data analyses. Subsequently, this employee contacted the participant with the result and provided instructions on how to access the web-based training.
Blinding
Due to the nature of the intervention, blinding of patients was not feasible. The intervention started as soon as patients logged on to the mindfulness training website. The outcome assessors (investigators) were unaware of patients’ treatment allocation. Therefore, the design of this study can be considered as a single-blinded randomized controlled trial in which the investigators remained blinded throughout the duration of the study. Additionally, patients were instructed not to say anything about their treatment allocation, neither to study investigators nor to their cardiologist.
Outcome measures
Outcomes were measured in all patients pre- (T0) and post-intervention (12 weeks, T1).
We were interested in evaluating the physical effects of mindfulness and thus chose as primary outcome measure the 6MWT, which is an overall measure of exercise tolerance, has reproducible results, and has shown to be an independent predictor of long term outcome.[20–22] The 6MWT was performed in a 20-meter-long corridor at the outpatient clinic.[23] The corridor had well-indicated ‘start’ and ‘finish’ marks with colored pawns.
Secondary outcome measures
Physical parameters
Weight, blood pressure, respiratory rate and heart rate. BMI was calculated by weight in kilograms divided by height in meters squared. Blood pressure was measured using an automated non-invasive monitor (Mindray Datascope Duo) after the participant had rested for 5 minutes in the sitting position. This monitor also reports the heart rate. Respiratory rate was measured in rest within a set amount of 30 seconds.
Blood sampling laboratory tests
N-terminal pro-brain natriuretic peptide (NT-proBNP, Elecsys system, Roche Diagnostics, Basel, Switzerland: normal values ≤ 14pmol/L) and creatinin were measured from peripheral venous blood samples.
Subjective health status
The Short-Form Health survey 36 (SF-36) was used to evaluate subjective health status. For each of the 8 subdomains a transformed score is generated, ranging from 0 to 100,[24] with a higher score indicating better health.[25] The subdomains were used to construct the mental component summary (MCS) measure, which consists of the subdomains vitality, social functioning, role-emotional functioning and mental health, and the physical component summary (PCS) measure, which consists of the subdomains physical functioning, role physical functioning, bodily pain and general health.[26]
A Visual Analogue Scale (VAS) was used to assess subjective perceived QoL (“Indicate on the line above where you would situate yourself in terms of your overall quality of life”, ranging from 0 to 100, with a higher score indicating better QoL.[27]
Psychological well-being
To assess symptoms of anxiety and depression, the Hospital Anxiety and Depression scale was used. The questionnaire contains 14 items on depression and anxiety with a higher score on the 3 point Likert scale indicating a greater level of emotional distress.[28]
Stress
The Dutch version of the Perceived Stress Scale (PSS) was used to evaluate perceived stress. The scale consists of fourteen 5-point Likert scales, with a higher score indicating a higher level of stress (0 = never, 4 = very often). A total perceived stress score is made by summing all individual items.[29]
Social support
To evaluate perceived social support, the Dutch version of the Perceived Social Support Scale 12 Blumenthal (PSSS12) was used. The PSSS12 has 12 items with a 7-point Likert scale addressing the degree of perceived social support with a higher score indicating a greater feeling of support (1 = very strongly disagree, 7 = very strongly agree).[30] For the purpose of this study we used the total score.
Adverse events
Adverse events were defined as all-cause mortality, heart failure, symptomatic arrhythmia, cardiac surgery, and percutaneous cardiac intervention. Arrhythmias were defined as symptomatic if antiarrhythmic medication was prescribed, cardioversion or ablation had been applied, or a pacemaker or intracardiac defibrillator (ICD) was implanted. Heart failure was defined as an event when either medication or hospitalization was necessary.
Other study parameters
In order to document baseline risk levels, traditional cardiovascular risk factors and demographics were determined: age, sex, length, weight, smoking, type of heart disease, and employment status. Additionally participation in other mindfulness-based exercises and the use of other complementary care was monitored with a questionnaire (type, frequency, and intensity).
Quality control and audit
The digitalization of the paper case record forms (CRFs) in the database was independently performed by 2 persons (JY and MW). After digitalization, an error rate of <0.5% was observed between JY and MW. An independent audit was performed and the study was found to comply with Good Clinical Practice and Scientific Integrity standards.
Sample size justification
To demonstrate an improvement of 5% in the intervention group vs 1% in the control group on the 6MWT, this study required 99 patients in the control group and 198 in the active intervention group (SD10%, alpha = 0.05, power = 0.90, ratio experimental to controls = 2). Even if only 50% of patients in the experimental group adhered to the training, this would give us a power of 0.80 in the as-treated analysis. To account for non-adherence and loss to follow-up our aim was to randomize at least 300 patients. This number of patients is sufficient to demonstrate a smaller difference (5% in the intervention group vs 2% in the control group) in a repeated measurements analysis with a power of 75% (2 follow-up measurements, correlation between follow up measurements = 0.70, correlation between baseline & follow-up = 0.50).
Statistical analysis
Descriptive analyses were performed to describe the baseline characteristics of demographic and clinical variables stratified by treatment group. Changes in outcomes at 12 weeks compared with baseline (intragroup effect) and differences between treatment groups (difference in delta’s, intergroup effect) on physiological and psychological outcomes were calculated. To simultaneously account for the correlation between the multiple measurements of each patient and dropout, a repeated measurements analysis was performed using a multivariate linear regression mixed model to determine intergroup effects. In the mean structure of the mixed model we included the time effect, the intervention effect and their interaction, while a fully unstructured variance-covariance matrix was assumed for the error terms. Due to randomization only p-values for the interaction effect are reported.
An intention-to-treat (ITT) analysis was performed to address whether offering a mindfulness training was effective compared to UC. An as-treated (AT) analysis was performed to address whether the mindfulness training was beneficial if actually performed. In the AT analysis, patients were considered adherent if they completed 50% or more of the exercises. Patients allocated to the UC group who sought mindfulness training on their own were excluded from the AT analysis.
For both ITT and AT, Cohen’s D was calculated to enable comparison of effect sizes. This calculation was performed based on the results of the mixed model.
A p-value less than 0.05 was considered to be indicative of statistical significance. All data were analyzed with IBM SPSS Statistics version 21.0 (IBM Corp., Somers, NY).
Results
Patient recruitment and characteristics
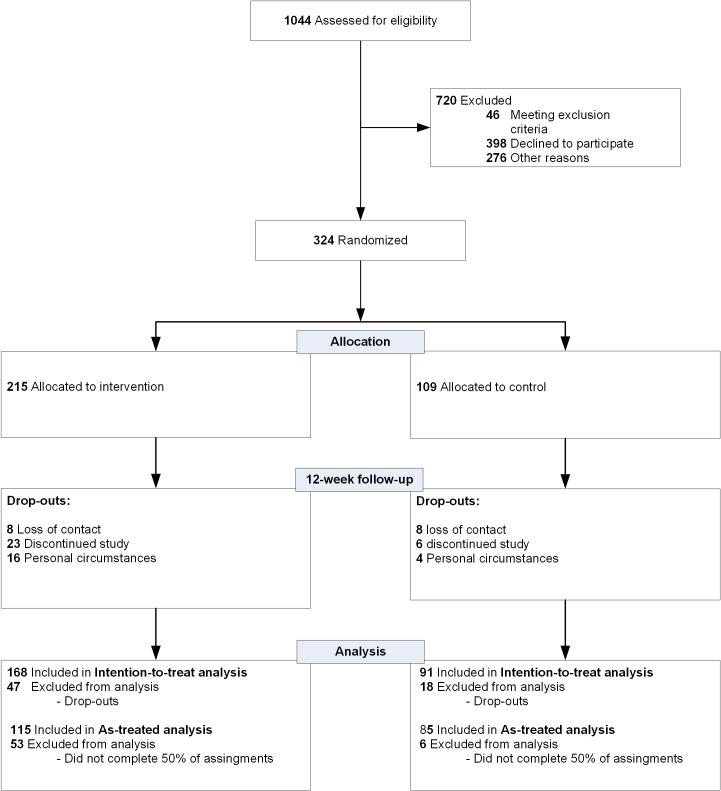
A flowchart of the patients’ recruitment is shown in Fig 1. Patients’ baseline characteristics (Table 1) demonstrated no significant differences between the intervention and control group which confirmed a successful randomization, also on important characteristics such as: age (p = 0.98) and, gender (p = 0.28). In total, 5 patients did not complete any assignment of the mindfulness training whereas 115 patients completed at least 50% of the assignments (as-treated analysis) with a mean (SD) 53% (34).
Fig 1. Flowchart of mindfulness training and control group.
Table 1. Baseline characteristics of study participants.
| Mindfulness Group N = 215 | Control Group N = 109 | ||
|---|---|---|---|
| Demographics | |||
| Age (years), mean (SD) | 43.2 (14.1) | 43.2 (13.7) | |
| Female (%) | 44.2 | 50.5 | |
| Physiological parameters | |||
| Heart rate (beats/min), mean (SD) | 68 (12) | 69 (11) | |
| Systolic blood pressure (mm Hg), mean (SD) | 128 (16) | 125 (15) | |
| Diastolic blood pressure (mm Hg), mean (SD) | 78 (11) | 80 (10) | |
| Resting respiratory rate (breaths/min), median (IQR) | 15 (2) | 15 (3) | |
| Body mass index (kg/m2), mean (SD) | 25.9 (4.6) | 25.7 (4.7) | |
| Obesity* (%) | 16.7 | 15.6 | |
| Psychological parameters | |||
| PCS, mean (SD) | 46.6 (9.6) | 45.3 (10.3) | |
| MCS, mean (SD) | 50.2 (10.6) | 50.8 (9.6) | |
| HADS Anxiety, mean (SD) | 8.2 (3.6) | 9.0 (3.4) | |
| HADS Depression, mean (SD) | 3.8 (2.9) | 3.8 (2.9) | |
| VAS, mean (SD) | 75.0 (13.2) | 72.7 (13.2) | |
| PSS, mean (SD) | 22.4 (7.8) | 22.0 (7.5) | |
| PSSS12, mean (SD) | 69.5 (11.6) | 71.5 (12.3) | |
| Exercise tolerance | |||
| 6 minute walk test distance (meters), mean (SD) | 537.5 (77.0) | 539.3 (67.3) | |
| Laboratory works | |||
| NT-proBNP, median (IQR), pmol/L | 16.7 (28.5) | 18.3 (33.9) | |
| Creatinine, median (IQR), μmol/L | 79.0 (21.0) | 77.0 (21.0) | |
| Cardiac history, type of heart disease, (%) | |||
| Congenital heart disease | 41.9 | 42.2 | |
| Cardiomyopathy | 39.5 | 29.4 | |
| Valvular heart disease | 18.6 | 28.4 | |
| Other comorbidity, (%) | |||
| Diabetes Mellitus** | 3.2 | 3.7 | |
| Number of interventions in life***, mean (SD) | 1.4 (1.4) | 1.4 (1.2) | |
| Time since first intervention (years), mean (SD) | 19.1 (14.0) | 15.9 (11.7) | |
| ICD, (%) | 5.9 | 4.3 | |
| PM, (%) | 9.3 | 5.2 | |
| Current medication (%) | 70.2 | 72.5 | |
| Beta-blocker | 43.2 | 36.7 | |
| Statin | 18.6 | 13.8 | |
| Aspirin | 16.3 | 14.7 | |
| Ace-inhibitor | 23.3 | 22.0 | |
| Angiotensin II antagonist | 8.8 | 11.9 | |
| Calcium channel blocker | 9.8 | 6.4 | |
| Nitroglycerin | 2.3 | 0.0 | |
| Cardiac glycoside | 2.3 | 2.8 | |
| Diuretic | 16.8 | 19.3 | |
| Anticoagulant | 24.6 | 33.9 | |
| Antidepressant | 5.1 | 2.8 | |
| Tranquilizer | 1.9 | 1.8 | |
| Other | 43.3 | 57.8 | |
| Intoxication, (%) | |||
| Current smoking | 14.4 | 18.3 | |
| Current alcohol use | 62.1 | 55.0 | |
| Current drugs use | 3.3 | 2.8 | |
| Work status | |||
| Employed, (%) | 68.7 | 67.9 | |
| Prior use of complementary therapies****, (%) | 14.4 | 12.8 | |
* Obesity was defined when the BMI was ≥30 kg/m2.
** Diabetes was defined when a patient reported use of anti-diabetes medication.
*** Include both surgical and percutaneous interventions.
**** Contains yoga, meditation, mindfulness, tai chi, Qigong and acupuncture.
SD, standard deviation; PCS, physical component summary measure; MCS, mental component summary measure; VAS, visual analogue scale; HADS, hospital anxiety and depression scale; PSS, perceived stress score; PSSS12, perceived social support; NT-proBNP, N-terminal pro-Brain Natriuretic Peptide; IQR, interquartile range; ICD, implantable cardioverter-defibrillator; PM, pacemaker.
Safety/side effects
No major side effects were reported during the follow-up period. In 7 patients (5 mindfulness (2.3%), 2 control (1.8%)) at baseline and 13 patients (8 mindfulness (4.8%), 5 control (5.5%)) at follow-up, fatigue, dizziness, shortness of breath, or pain due to pre-existing conditions were described while performing the 6MWT.
Outcome analysis
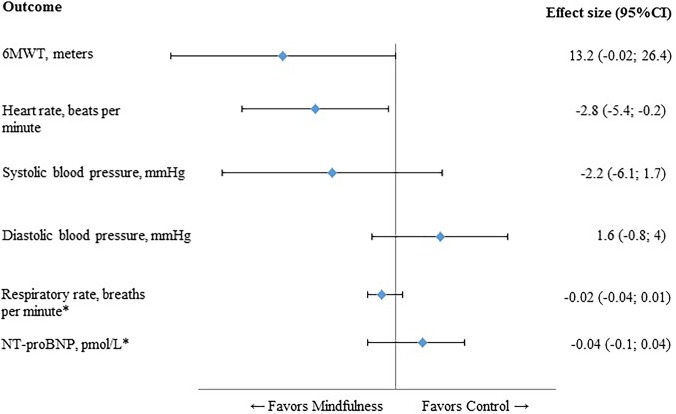
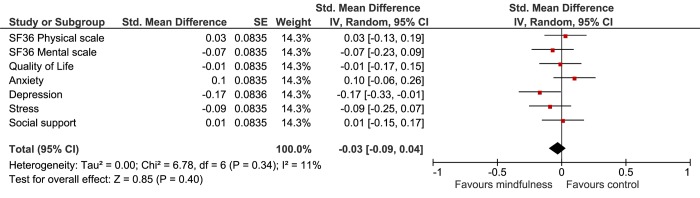
At 12 weeks, the mindfulness group showed a notable improvement on their mean 6MWT, which was borderline significantly different compared with UC (p = 0.050) (Table 2). The intergroup comparison showed that heart rate was significantly lower in the mindfulness group (p = 0.033) (Table 2). Mean systolic and mean diastolic blood pressure decreased in the mindfulness and UC group, but no significant differences were found in the intergroup comparison (Table 2). The results of the physiological outcomes are summarized in Fig 2.
Table 2. Changes in outcomes at 12 weeks compared with baseline (intragroup effect) and differences between treatment groups (difference in delta’s, intergroup effect) on physiological and psychological outcomes.
Intention-to-treat analyses.
| Physiological outcomes | Treatment group | Delta 12-weeks vs baseline (intragroup) a (mean, SD) | Effect Estimate (intergroup) b | 95% CI | p-value |
|---|---|---|---|---|---|
| 6MWT, meters | Mindfulness | 10.42 (49.0) | 13.2 | -0.02; 26.4 | 0.050 |
| UC | -4.0 (55.6) | ||||
| Heart rate, beats/min | Mindfulness | -2 (10.9) | -2.8 | -5.4; -0.2 | 0.033 |
| UC | 0.5 (9.0) | ||||
| SBP, mmHg | Mindfulness | -4.2 (15.4) | -2.2 | -6.1; 1.7 | 0.268 |
| UC | -1.9 (15.5) | ||||
| DBP, mmHg | Mindfulness | -1.9 (8.9) | 1.6 | -0.8; 4.0 | 0.186 |
| UC | -3.4 (10.1) | ||||
| Respiratory rate, breaths/minute * | Mindfulness | -0.5 (3.6) | -0.02 | -0.04; 0.01 | 0.189 |
| UC | -0.1 (4.0) | ||||
| NT-proBNP, pmol/L * | Mindfulness | 0.3 (9.7) | -0.04 | -0.1; 0.04 | 0.333 |
| UC | 0.0 (11.10) | ||||
| Psychological outcomes | |||||
| SF-36 PCS | Mindfulness | 0.5 (6.3) | -0.4 | -2.0; 1.3 | 0.668 |
| UC | 0.7 (6.7) | ||||
| SF-36 MCS | Mindfulness | 0.2 (7.4) | 0.74 | -1.4; 2.8 | 0.489 |
| UC | 1.2 (8.8) | ||||
| VAS | Mindfulness | 0.4 (10.4) | -0.4 | -3.0; 2.1 | 0.745 |
| UC | 0.7 (9.3) | ||||
| HADS Anxiety | Mindfulness | -0.5 (3.2) | 0.6 | -0.2; 1.4 | 0.145 |
| UC | -0.9 (3.0) | ||||
| HADS Depression | Mindfulness | -0.5 (2.9) | -0.4 | -1.1; 0.2 | 0.203 |
| UC | 0.0 (2.3) | ||||
| PSS | Mindfulness | -2.4 (6.3) | -1.0 | -2.7; 0.6 | 0.226 |
| UC | -0.9 (6.8) | ||||
| PSSS12 | Mindfulness | 0.6 (7.4) | 0.4 | -1.6: 2.4 | 0.685 |
| UC | 0.1 (8.0) | ||||
SD, standard deviation; SE, standard error; 6MWT, six-minute walk test; UC, usual care; SBP, systolic blood pressure; DBP, diastolic blood pressure; NT-proBNP, N-terminal pro-brain natriuretic peptide; SF-36, Short Form Health survey; PCS, physical component summary measure; MCS, mental component summary measure; VAS, visual analogue scale; HADS, hospital anxiety and depression scale; PSS, perceived stress score; PSSS12, perceived social support.
* Effect estimates are calculated from log-transformed scores.
a Delta value (follow-up measurement minus baseline, intragroup effect) was calculated for those who attended the 12-week follow-up.
b Linear mixed model analyses for repeated measurements for differences between treatment groups (intergroup effect) on the dependent variables (time X intervention effect).
Fig 2. Forest plot of physiological outcomes.
All values on the left of the Y-axis indicate a difference in favour of the mindfulness group. 6MWT, six-minute walk test; IC, confidence interval, NT-proBNP, N-terminal pro-brain natriuretic peptide; * Log-transformed scores.
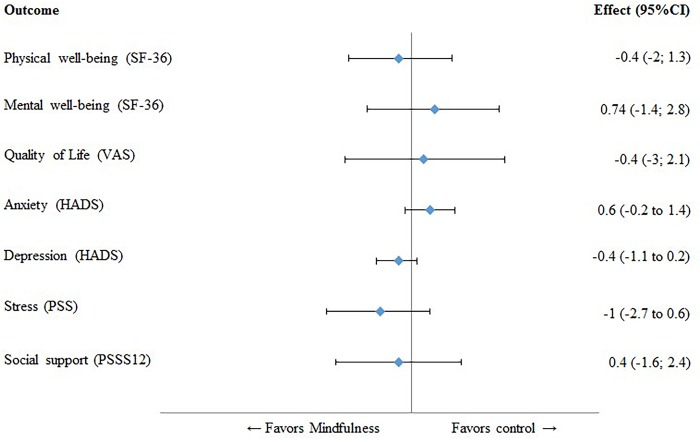
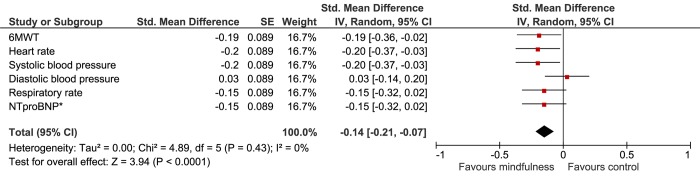
Analyses showed no significant differences between the groups on the PCS and MCS of the SF-36 (Table 2). At 12 weeks, anxiety levels were lower than baseline scores in both the mindfulness and the UC group, but no significant differences were found in the intergroup comparison (Table 2).
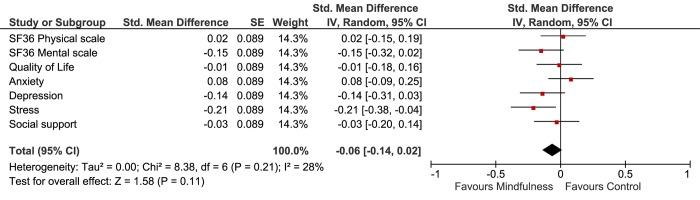
Depressive symptoms decreased at 12 weeks, but did not significantly differ between the groups. Neither perceived stress scores nor perceived social support were statistically significant different in the intergroup comparison (Table 2). No significant differences were found on adverse events. The results of the psychological outcomes are summarized in Fig 3.
Fig 3. Forest plot of psychological outcomes.
All values on the left of the Y-axis indicate a difference in favour of the mindfulness group. CI, confidence interval; SF-36, Short Form Health survey; VAS, visual analogue scale; HADS, hospital anxiety and depression scale; PSS, perceived stress score; PSSS12, perceived social support.
The results of AT-analyses were comparable with the ITT analyses (Table 3).
Table 3. Changes in outcomes at 12 weeks compared with baseline (intragroup effect) and differences between treatment groups (intergroup effect) on physiological and psychological outcomes, as-treated analyses.
| Physiological outcomes | Treatment group | Delta 12-weeks* (mean, SD) | Estimate† | 95% CI | p |
|---|---|---|---|---|---|
| 6MWT, meters | Mindfulness | 9.36 (35.9) | 10.6 | -1.7; 23.0 | 0.091 |
| UC | -1.92 (51.7) | ||||
| Heart rate, beats/min | Mindfulness | -3.07 (11.7) | -3.4 | -6.3; 0.4 | 0.027 |
| UC | 0.47 (9.2) | ||||
| SBP, mmHg | Mindfulness | -5.17 (14.5) | -3.8 | -8.0; 0.3 | 0.072 |
| UC | -1.50 (15.5) | ||||
| DBP, mmHg | Mindfulness | -2.34 (8.9) | 0.8 | -1.8; 3.5 | 0.524 |
| UC | -3.39 (10.1) | ||||
| Respiratory rate, breaths/minute | Mindfulness | -0.67 (3.5) | -0.7 | -1.8; 0.3 | 0.170 |
| UC | -0.11 (4.1) | ||||
| NT-proBNP, pmol/L ‡ | Mindfulness | 1.03 (28.7) | -0.04 | -0.2; 0.09 | 0.540 |
| UC | 4.73 (21.7) | ||||
| Psychological outcomes | |||||
| SF-36 PCS | Mindfulness | 0.7 (6.4) | 0.13 | -1.7; 2.0 | 0.893 |
| UC | 0.4 (6.8) | ||||
| SF-36 MCS | Mindfulness | -0.05 (7.5) | 1.2 | -1.1; 3.5 | 0.302 |
| UC | 1.5 (8.9) | ||||
| VAS | Mindfulness | 0.4 (10.4) | -0.2 | -3.0; 2.6 | 0.878 |
| UC | 0.7 (9.3) | ||||
| HADS Anxiety | Mindfulness | -0.5 (3.2) | 0.5 | -0.4; 1.4 | 0.267 |
| UC | -0.9 (3.0) | ||||
| HADS Depression | Mindfulness | -0.5 (2.9) | -0.4 | -1.2; 0.3 | 0.267 |
| UC | 0.0 (2.3) | ||||
| PSS | Mindfulness | -2.4 (6.3) | -1.1 | -3.0; 0.8 | 0.244 |
| UC | -0.9 (6.8) | ||||
| PSSS12 | Mindfulness | 0.6 (7.4) | 0.5 | -1.7; 2.6 | 0.670 |
| UC | 0.1 (8.0) | ||||
SD, standard deviation; SE, standard error; 6MWT, six-minute walk test; UC, usual care; SBP, systolic blood pressure; DBP, diastolic blood pressure; IQR, interquartile range; SE, standard error, NT.
proBNP, N-terminal pro-brain natriuretic peptide; SF-36, Short Form Health survey; VAS, visual analogue scale; HADS, hospital anxiety and depression scale; PSS, perceived stress score; PSSS12, perceived social support.
* Delta value (follow-up measurement minus baseline, intragroup effect) was calculated for those who attended the 12-week follow-up.
† Linear mixed model analyses for repeated measurements for differences between treatment groups on the dependent variables (time X intervention effect).
‡ Effect estimates are calculated from log-transformed scores.
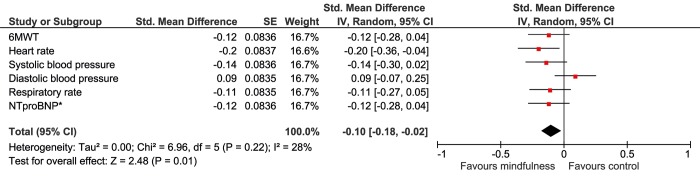
Cohen’s D
In order to compare different outcome measures, Cohen’s D effect sizes were calculated. In the intention-to-treat analyses (Figs 4 and 5), heart rate and depression showed, small, but significant improvement (D = 0.20, 95%CI 0.04 to 0.36 and d = 0.17, 95%CI 0.01 to 0.33 respectively). In the As-Treated analysis, exercise capacity, heart rate, systolic blood pressure and stress improved significantly, with small effect sizes ranging from D = 0.19 to D = 0.21 (Figs 6 and 7).
Fig 4. Forest plot showing the Intention-to-Treat Cohen’s D results of the effectiveness of the mindfulness intervention compared with usual care on the physiological outcomes.
The width of the line indicates the 95%CI. All values lower than 0 indicate a significant difference in favour of the mindfulness group.
Fig 5. Forest plot showing the Intention-to-Treat Cohen’s D results of the effectiveness of the mindfulness intervention compared with usual care on the psychological outcomes.
The width of the line indicates the 95%CI. All values lower than 0 indicate a significant difference in favour of the mindfulness group.
Fig 6. Forest plot showing the As-Treated Cohen’s D results of the effectiveness of the mindfulness intervention compared with usual care on the physiological outcomes.
The width of the line indicates the 95%CI. All values lower than 0 indicate a significant difference in favour of the mindfulness group.
Fig 7. Forest plot showing the As-Treated Cohen’s D results of the effectiveness of the mindfulness intervention compared with usual care on the psychological outcomes.
The width of the line indicates the 95%CI. All values lower than 0 indicate a significant difference in favour of the mindfulness group.
Discussion
To our knowledge, this is the first randomized trial to evaluate the effectiveness of mindfulness training in patients with heart disease. By taking physiological parameters as its main outcome parameter, it is also an innovative study. On the primary endpoint–exercise capacity–we found a borderline significant but clinically small effect in favor of mindfulness. Heart rate also decreased significantly more with mindfulness training. Remarkably, no significant improvements were found on subjective outcome measures, although anxiety and depressive symptoms did decrease.
Limited exercise capacity is an important predictor for outcome for cardiac disease, and several studies have reported an association with survival.[17, 31–33] Since a decrease in physical performance is also an important predictor of adverse outcomes in patients with congenital heart disease, improving physical performance may be an important target of treatment. In recent years, cardiac rehabilitation programs, many of them conducted in patients with post-myocardial infarction, have had good results on total and cardiovascular mortality.[34, 35] Our results indicate that mindfulness training could be part of future treatment modalities intended to improve physical performance in heart disease patients. It remains to be shown whether this will also affect long-term outcome. Several epidemiological studies in patients with hypertension, acute coronary syndromes,[36] stable coronary heart disease[37] and heart failure[38] have shown that resting heart rate is a risk factor for cardiovascular and all-cause mortality. These epidemiological results suggest that the beneficial effect of mindfulness on heart rate demonstrated in our study is clinically meaningful.
To date, very few studies have evaluated mindfulness training in patients with cardiac disease. A pilot study that offered a brief mindfulness-based stress-reduction program to patients with, or at risk of, coronary artery disease[16] showed significant but moderate reductions on two psychological outcomes, depression (Cohen’s d = 0.54) and perceived stress (d = 0.68). Unlike in our study, the participants were not randomized and the intervention was fairly short (4-weeks). Two reports of the same study population showed that mindfulness-based stress-reduction mainly improved anxiety, emotional control and coping, rather than resting-stress hormones or physical functioning.[39, 40] Recently, a brief group-MBSR intervention in patients undergoing a percutaneous coronary intervention showed favorable effects on quality of life.[41] Additionally, anxiety, depression, and stress appeared to be influenced positively but only in the younger age group (<60 years).[41] Lastly, an individual MBSR training in patients with coronary heart disease showed significant reductions in anxiety, depression, perceived stress and the physiological parameters BP and BMI.[42] However, this study had limited power and was only performed in males. In contrast to previous reports, in our study psychological outcomes did not significantly improve by mindfulness training. Whereas in previous studies patients were often selected on the basis of reduced psychological well-being, in our study they were not. In fact, baseline psychological scores were similar to scores in the general population[43–47] implying that improvement was hardly possible (a ceiling effect). Also, our training was online without any personal contact, which probably resulted in smaller effects. There is increased interest in the effect of acceptance and commitment therapy, which has similarities with mindfulness training, focusing on the relationship between persons’ own thoughts and feelings that could potentially have a positive effect on several modifiable CVD risk factors.[48]
Similar to the ceiling effect for psychological outcomes, we observed a floor effect for blood pressure, as our patients had regular blood pressure monitoring and (extra) medication was given when necessary. Previous studies, some of which showed potential benefits on blood pressure, investigated populations whose blood pressures at baseline were higher than average.[7, 49]
Accumulating evidence suggests that mind and body do indeed show an interaction and that physiological changes are underlain by several neuro-humoral mechanisms. For example, in an extensive study of a framework in mind-body medicine, Benson and colleagues focused on the relaxation response as a core component in autonomic function and physical changes.[50, 51] It has been shown that, through emotions and thoughts, the autonomic nervous system is key in the brain-heart connection.[52] By working through the autonomic nervous system, mind-body practices can also benefit endothelial, neuroendocrine and immune function.[53–55] However, the mechanism between the mind and body is not merely unidirectional: several levels of the neuro-axis have been found to contribute to the “top-down and bottom-up mechanisms” in mind-body practices.[56]
To date, web-based mindfulness training studies have been limited to small studies on stress reduction. A study by Gluck et al.[57] reported a trend towards lower levels of stress. Two other studies on online mindfulness training showed not only that it was feasible to conduct online mindfulness training, but also that it was effective in reducing stress.[58, 59] It is important to emphasize that their study populations consisted of mainly females recruited from the healthy general population, and in one, no randomization was performed.
Limitations of the current study must be addressed. Our own study used neither a placebo nor a waiting list for the control group. We considered the placebo effect of the online training to be inherent to the active intervention: we evaluated the training and the control as they would be implemented in real-world practice and measured effectiveness rather than efficacy. We acknowledge that by doing so our study is pragmatic rather than explanatory. Our inclusion of the placebo effect as part of the mindfulness intervention compared with UC without placebo in the control group is further justified by the fact that no competing therapy exists. Every placebo online training similar to the intervention we could think of would likely have an unwanted beneficial effect in the control group.
Another limitation is that only 80.6% (n = 261) of the patients returned for follow-up. Reasons for trial discontinuation were not reported due to recommendations from the local ethics committee. A possible explanation for the follow-up rate is the fact that the intervention was not offered in a group-based setting. The impact of online training may be lower than that of personal or group training. While this would mean that the results of mindfulness therapy may therefore be even stronger in other settings, the easy accessibility of online training may have allowed better generalizability of the results, as patients could do the training in their own environment and fit it into a busy schedule. Although we monitored participants’ training activity, detailed adherence was difficult to assess and control for. Furthermore, ethical considerations prevented us from blinding patients to the nature of the intervention during the informed consent procedure and patients’ expectation of the interventions was not addressed. The control group was therefore aware that the online mindfulness training was available and that they were not receiving it. This could have led to selective follow-up but we found no significant difference between the groups at follow-up with regard to demographic and clinical variables. A placebo lifestyle intervention in the control group could underestimate the effectiveness of the active intervention compared to what can be expected in real-world practice. Thus, rather than comparing to a unrealistic placebo intervention, we considered the placebo effect as part-and-parcel of the procedure. In addition, we did not assess maintenance of blinding, but the inability to blind patients could have potentially led to unblinding of the investigators (outcome assessors), even though extensive precautions were made to limit this bias.
Conclusions
Online mindfulness training is feasible in patients with heart disease and shows a small positive effect on exercise capacity and heart rate. The current study found no significant effect on psychological outcomes.
Supporting Information
(DOC)
(DOC)
(DOCX)
Acknowledgments
The authors thank the patients, secretary Celeste Manley for her fantastic administrative support, and students Esther van der Woude and Maud Hendriksen for their assistance.
The online mindfulness training was originally developed and provided by Psychology Magazine. This program is also available to clients in the general Dutch population as an 8 weeks training. For the current study the training was extended to12 weeks. In particular we would like to thank Peggy van der Lee from Psychology Magazine for her support in the design of the mindfulness training for this study.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
JOY, RAG, MGMH, and JWR received an internal grant from the Erasmus MC. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Murray CJL, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2197–223. 10.1016/S0140-6736(12)61689-4 [DOI] [PubMed] [Google Scholar]
- 2. Richardson S, Shaffer JA, Falzon L, Krupka D, Davidson KW, Edmondson D. Meta-analysis of perceived stress and its association with incident coronary heart disease. Am J Cardiol. 2012;110(12):1711–6. Epub 2012/09/15. 10.1016/j.amjcard.2012.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rosengren A, Hawken S, Ounpuu S, Sliwa K, Zubaid M, Almahmeed WA, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):953–62. Epub 2004/09/15. 10.1016/S0140-6736(04)17019-0S0140-6736(04)17019-0 [pii]. . [DOI] [PubMed] [Google Scholar]
- 4. Richardson S, Shaffer JA, Falzon L, Krupka D, Davidson KW, Edmondson D. Meta-analysis of perceived stress and its association with incident coronary heart disease. Am J Cardiol. 2012;110(12):1711–6. Epub 2012/09/15. doi: S0002-9149(12)01929-7 [pii] 10.1016/j.amjcard.2012.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Custodis F, Gertz K, Balkaya M, Prinz V, Mathar I, Stamm C, et al. Heart rate contributes to the vascular effects of chronic mental stress: effects on endothelial function and ischemic brain injury in mice. Stroke. 2011;42(6):1742–9. Epub 2011/04/30. doi: STROKEAHA.110.598607 [pii] 10.1161/STROKEAHA.110.598607 . [DOI] [PubMed] [Google Scholar]
- 6. Perk J, De Backer G, Gohlke H, Graham I, Reiner Z, Verschuren M, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts). Eur Heart J. 2012;33(13):1635–701. Epub 2012/05/05. doi: ehs092 [pii] 10.1093/eurheartj/ehs092 . [DOI] [PubMed] [Google Scholar]
- 7. Abbott RA, Whear R, Rodgers LR, Bethel A, Thompson Coon J, Kuyken W, et al. Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: A systematic review and meta-analysis of randomised controlled trials. Journal of psychosomatic research. 2014;76(5):341–51. 10.1016/j.jpsychores.2014.02.012 . [DOI] [PubMed] [Google Scholar]
- 8. Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med. 2014;174(3):357–68. Epub 2014/01/08. doi: 1809754 [pii] 10.1001/jamainternmed.2013.13018 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kabatzinn J. An Outpatient Program in Behavioral Medicine for Chronic Pain Patients Based on the Practice of Mindfulness Meditation—Theoretical Considerations and Preliminary-Results. Gen Hosp Psychiat. 1982;4(1):33–47. 10.1016/0163-8343(82)90026-3 . [DOI] [PubMed] [Google Scholar]
- 10. Segal ZVW, J.M.G.; Teasdale J.D. Mindfulness-based Cognitive Therapy for Depression: A New Approach to Preventing Relapse. New York: Guilford Press; 2002. 351 p. [Google Scholar]
- 11. Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, et al. Mindfulness: A proposed operational definition. Clin Psychol-Sci Pr. 2004;11(3):230–41. 10.1093/clipsy/bph077 . [DOI] [Google Scholar]
- 12. Hofmann SG, Sawyer AT, Witt AA, Oh D. The Effect of Mindfulness-Based Therapy on Anxiety and Depression: A Meta-Analytic Review. J Consult Clin Psych. 2010;78(2):169–83. 10.1037/A0018555 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zeidan F, Johnson SK, Gordon NS, Goolkasian P. Effects of Brief and Sham Mindfulness Meditation on Mood and Cardiovascular Variables. J Altern Complem Med. 2010;16(8):867–73. 10.1089/acm.2009.0321 . [DOI] [PubMed] [Google Scholar]
- 14. Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clin Psychol-Sci Pr. 2003;10(2):125–43. 10.1093/clipsy/bpg015 . [DOI] [Google Scholar]
- 15. Ospina MB, Bond K, Karkhaneh M, Tjosvold L, Vandermeer B, Liang Y, et al. Meditation practices for health: state of the research. Evid Rep Technol Assess (Full Rep). 2007;(155):1–263. Epub 2007/09/04. . [PMC free article] [PubMed] [Google Scholar]
- 16. Olivo EL, Dodson-Lavelle B, Wren A, Fang Y, Oz MC. Feasibility and effectiveness of a brief meditation-based stress management intervention for patients diagnosed with or at risk for coronary heart disease: a pilot study. Psychology Health & Medicine. 2009;14(5):513–23. Epub 2009/10/22. doi: 915988873 [pii] 10.1080/13548500902890087 . [DOI] [PubMed] [Google Scholar]
- 17. Diller GP, Dimopoulos K, Okonko D, Li W, Babu-Narayan SV, Broberg CS, et al. Exercise intolerance in adult congenital heart disease: comparative severity, correlates, and prognostic implication. Circulation. 2005;112(6):828–35. Epub 2005/08/03. doi: CIRCULATIONAHA.104.529800 [pii] 10.1161/CIRCULATIONAHA.104.529800 . [DOI] [PubMed] [Google Scholar]
- 18. Maex E. Mindfulness 'in de maalstroom van je leven': Lannoo; 2006. [Google Scholar]
- 19.Formsvision. [updated 24/10/2014]. Available: www.formsvision.com.
- 20. Van De Bruaene A, De Meester P, Voigt JU, Delcroix M, Pasquet A, De Backer J, et al. Worsening in oxygen saturation and exercise capacity predict adverse outcome in patients with Eisenmenger syndrome. International journal of cardiology. 2013;168(2):1386–92. 10.1016/j.ijcard.2012.12.021 . [DOI] [PubMed] [Google Scholar]
- 21. Rostagno C, Olivo G, Comeglio M, Boddi V, Banchelli M, Galanti G, et al. Prognostic value of 6-minute walk corridor test in patients with mild to moderate heart failure: comparison with other methods of functional evaluation. European journal of heart failure. 2003;5(3):247–52. . [DOI] [PubMed] [Google Scholar]
- 22. Manzano L, Babalis D, Roughton M, Shibata M, Anker SD, Ghio S, et al. Predictors of clinical outcomes in elderly patients with heart failure. European journal of heart failure. 2011;13(5):528–36. 10.1093/eurjhf/hfr030 . [DOI] [PubMed] [Google Scholar]
- 23. Laboratories ATSCoPSfCPF. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–7. Epub 2002/07/02. 10.1164/ajrccm.166.1.at1102 . [DOI] [PubMed] [Google Scholar]
- 24. Ware JE Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83. Epub 1992/06/11. . [PubMed] [Google Scholar]
- 25. Lane DA, Lip GY, Millane TA. Quality of life in adults with congenital heart disease. Heart. 2002;88(1):71–5. Epub 2002/06/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. McHorney CA, Ware JE Jr., Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31(3):247–63. . [DOI] [PubMed] [Google Scholar]
- 27. Moons P, Van Deyk K, De Bleser L, Marquet K, Raes E, De Geest S, et al. Quality of life and health status in adults with congenital heart disease: a direct comparison with healthy counterparts. Eur J Cardiovasc Prev Rehabil. 2006;13(3):407–13. Epub 2006/08/24. doi: 00149831-200606000-00017 [pii]. . [DOI] [PubMed] [Google Scholar]
- 28. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70. Epub 1983/06/01. . [DOI] [PubMed] [Google Scholar]
- 29. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96. Epub 1983/12/01. . [PubMed] [Google Scholar]
- 30. Pedersen SS, Spinder H, Erdman RA, Denollet J. Poor perceived social support in implantable cardioverter defibrillator (ICD) patients and their partners: cross-validation of the multidimensional scale of perceived social support. Psychosomatics. 2009;50(5):461–7. Epub 2009/10/27. doi: 50/5/461 [pii] 10.1176/appi.psy.50.5.461 . [DOI] [PubMed] [Google Scholar]
- 31. Dimopoulos K, Okonko DO, Diller GP, Broberg CS, Salukhe TV, Babu-Narayan SV, et al. Abnormal ventilatory response to exercise in adults with congenital heart disease relates to cyanosis and predicts survival. Circulation. 2006;113(24):2796–802. Epub 2006/06/14. doi: CIRCULATIONAHA.105.594218 [pii] 10.1161/CIRCULATIONAHA.105.594218 . [DOI] [PubMed] [Google Scholar]
- 32. Inuzuka R, Diller GP, Borgia F, Benson L, Tay EL, Alonso-Gonzalez R, et al. Comprehensive use of cardiopulmonary exercise testing identifies adults with congenital heart disease at increased mortality risk in the medium term. Circulation. 2012;125(2):250–9. Epub 2011/12/08. doi: CIRCULATIONAHA.111.058719 [pii] 10.1161/CIRCULATIONAHA.111.058719 . [DOI] [PubMed] [Google Scholar]
- 33. Kempny A, Dimopoulos K, Alonso-Gonzalez R, Alvarez-Barredo M, Tutarel O, Uebing A, et al. Six-minute walk test distance and resting oxygen saturations but not functional class predict outcome in adult patients with Eisenmenger syndrome. International journal of cardiology. 2013;168(5):4784–9. Epub 2013/08/22. doi: S0167-5273(13)01452-6 [pii] 10.1016/j.ijcard.2013.07.227 . [DOI] [PubMed] [Google Scholar]
- 34. Heran BS, Chen JM, Ebrahim S, Moxham T, Oldridge N, Rees K, et al. Exercise-based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2011;(7):CD001800 Epub 2011/07/08. 10.1002/14651858.CD001800.pub2 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Clark AM, Hartling L, Vandermeer B, McAlister FA. Meta-analysis: secondary prevention programs for patients with coronary artery disease. Ann Intern Med. 2005;143(9):659–72. Epub 2005/11/03. doi: 143/9/659 [pii]. . [DOI] [PubMed] [Google Scholar]
- 36. Hjalmarson A, Gilpin EA, Kjekshus J, Schieman G, Nicod P, Henning H, et al. Influence of heart rate on mortality after acute myocardial infarction. Am J Cardiol. 1990;65(9):547–53. Epub 1990/03/11. doi: 0002-9149(90)91029-6 [pii]. . [DOI] [PubMed] [Google Scholar]
- 37. Diaz A, Bourassa MG, Guertin MC, Tardif JC. Long-term prognostic value of resting heart rate in patients with suspected or proven coronary artery disease. Eur Heart J. 2005;26(10):967–74. Epub 2005/03/19. doi: ehi190 [pii] 10.1093/eurheartj/ehi190 . [DOI] [PubMed] [Google Scholar]
- 38. Gullestad L, Wikstrand J, Deedwania P, Hjalmarson A, Egstrup K, Elkayam U, et al. What resting heart rate should one aim for when treating patients with heart failure with a beta-blocker? Experiences from the Metoprolol Controlled Release/Extended Release Randomized Intervention Trial in Chronic Heart Failure (MERIT-HF). J Am Coll Cardiol. 2005;45(2):252–9. Epub 2005/01/18. doi: S0735-1097(04)02063-7 [pii] 10.1016/j.jacc.2004.10.032 . [DOI] [PubMed] [Google Scholar]
- 39. Robert McComb JJ, Tacon A, Randolph P, Caldera Y. A pilot study to examine the effects of a mindfulness-based stress-reduction and relaxation program on levels of stress hormones, physical functioning, and submaximal exercise responses. J Altern Complement Med. 2004;10(5):819–27. Epub 2005/01/15. 10.1089/acm.2004.10.819 . [DOI] [PubMed] [Google Scholar]
- 40. Tacon AM, McComb J, Caldera Y, Randolph P. Mindfulness meditation, anxiety reduction, and heart disease: a pilot study. Fam Community Health. 2003;26(1):25–33. Epub 2003/06/13. . [DOI] [PubMed] [Google Scholar]
- 41. Nyklicek I, Dijksman SC, Lenders PJ, Fonteijn WA, Koolen JJ. A brief mindfulness based intervention for increase in emotional well-being and quality of life in percutaneous coronary intervention (PCI) patients: the MindfulHeart randomized controlled trial. J Behav Med. 2014;37(1):135–44. Epub 2012/11/28. 10.1007/s10865-012-9475-4 . [DOI] [PubMed] [Google Scholar]
- 42. Parswani MJ, Sharma MP, Iyengar S. Mindfulness-based stress reduction program in coronary heart disease: A randomized control trial. International journal of yoga. 2013;6(2):111–7. 10.4103/0973-6131.113405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Aaronson NK, Muller M, Cohen PD, Essink-Bot ML, Fekkes M, Sanderman R, et al. Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol. 1998;51(11):1055–68. Epub 1998/11/17. doi: S0895-4356(98)00097-3 [pii]. . [DOI] [PubMed] [Google Scholar]
- 44.Cohen SW, G. Perceived stress in a probability sample of the United States. In: Oskamp ISSS, editor. The social psychology of health: Claremont Symposium on applied social psychology. Newbury Park, CA: Sage; 1988.
- 45. Crawford JR, Henry JD, Crombie C, Taylor EP. Normative data for the HADS from a large non-clinical sample. Br J Clin Psychol. 2001;40(Pt 4):429–34. Epub 2002/01/05. . [DOI] [PubMed] [Google Scholar]
- 46. Kind P, Dolan P, Gudex C, Williams A. Variations in population health status: results from a United Kingdom national questionnaire survey. BMJ. 1998;316(7133):736–41. Epub 1998/04/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. J Pers Assess. 1988;52(1):30–41. 10.1207/s15327752jpa5201_2 . [DOI] [PubMed] [Google Scholar]
- 48. Spatola CA, Manzoni GM, Castelnuovo G, Malfatto G, Facchini M, Goodwin CL, et al. The ACTonHEART study: rationale and design of a randomized controlled clinical trial comparing a brief intervention based on Acceptance and Commitment Therapy to usual secondary prevention care of coronary heart disease. Health and quality of life outcomes. 2014;12:22 10.1186/1477-7525-12-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Younge JO, Gotink RA, Baena CP, Roos-Hesselink JW, Hunink MM. Mind-body practices for patients with cardiac disease: a systematic review and meta-analysis. Eur J Prev Cardiol. 2014. Epub 2014/09/18. doi: 2047487314549927 [pii] 10.1177/2047487314549927 . [DOI] [PubMed] [Google Scholar]
- 50. Benson H, Beary JF, Carol MP. The relaxation response. Psychiatry. 1974;37(1):37–46. Epub 1974/02/01. . [DOI] [PubMed] [Google Scholar]
- 51. Benson H. The relaxation gesponse: its subjective and objective historical precendents and physiology. Trends Neurosci. 1983;6:281–4. [Google Scholar]
- 52. Emani S, Binkley PF. Mind-body medicine in chronic heart failure: a translational science challenge. Circ Heart Fail. 2010;3(6):715–25. Epub 2010/11/18. doi: 3/6/715 [pii] 10.1161/CIRCHEARTFAILURE.110.951509 . [DOI] [PubMed] [Google Scholar]
- 53. Ditto B, Eclache M, Goldman N. Short-term autonomic and cardiovascular effects of mindfulness body scan meditation. Ann Behav Med. 2006;32(3):227–34. Epub 2006/11/17. 10.1207/s15324796abm3203_9 . [DOI] [PubMed] [Google Scholar]
- 54. Dod HS, Bhardwaj R, Sajja V, Weidner G, Hobbs GR, Konat GW, et al. Effect of intensive lifestyle changes on endothelial function and on inflammatory markers of atherosclerosis. Am J Cardiol. 2010;105(3):362–7. Epub 2010/01/28. doi: S0002-9149(09)02409-6 [pii] 10.1016/j.amjcard.2009.09.038 . [DOI] [PubMed] [Google Scholar]
- 55. Greeson JM. Mindfulness Research Update: 2008. Complement Health Pract Rev. 2009;14(1):10–8. Epub 2010/01/05. 10.1177/1533210108329862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Taylor AG, Goehler LE, Galper DI, Innes KE, Bourguignon C. Top-down and bottom-up mechanisms in mind-body medicine: development of an integrative framework for psychophysiological research. Explore (NY). 2010;6(1):29–41. Epub 2010/02/05. doi: S1550-8307(09)00343-7 [pii] 10.1016/j.explore.2009.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Gluck TM, Maercker A. A randomized controlled pilot study of a brief web-based mindfulness training. BMC Psychiatry. 2011;11:175. Epub 2011/11/10. doi: 1471-244X-11-175 [pii] 10.1186/1471-244X-11-175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Krusche A, Cyhlarova E, King S, Williams JM. Mindfulness online: a preliminary evaluation of the feasibility of a web-based mindfulness course and the impact on stress. BMJ Open. 2012;2(3). Epub 2012/05/23. doi: bmjopen-2011-000803 [pii] 10.1136/bmjopen-2011-000803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Morledge TJ, Allexandre D, Fox E, Fu AZ, Higashi MK, Kruzikas DT, et al. Feasibility of an online mindfulness program for stress management—a randomized, controlled trial. Ann Behav Med. 2013;46(2):137–48. Epub 2013/05/02. 10.1007/s12160-013-9490-x [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOC)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.