Abstract
Introduction
Husbands can play a crucial role in pregnancy and childbirth, especially in patriarchal societies of developing countries. In Myanmar, despite the critical influence of husbands on the health of mothers and newborns, their roles in maternal health have not been well explored. Therefore, the aim of this study was to identify the factors associated with husbands’ involvement in maternal health in Myanmar. This study also examined the associations between husbands’ involvement and their spouses’ utilization of maternal care services during antenatal, delivery and postnatal periods.
Methods
A community-based, cross sectional study was conducted with 426 husbands in Thingangyun Township, Yangon, Myanmar. Participants were husbands aged 18 years or older who had at least one child within two years at the time of interview. Face to face interviews were conducted using a pretested structured questionnaire. Factors associated with the characteristics of husband’s involvement as well as their spouses’ utilization of maternal care services were analyzed by multivariable logistic regression models.
Results
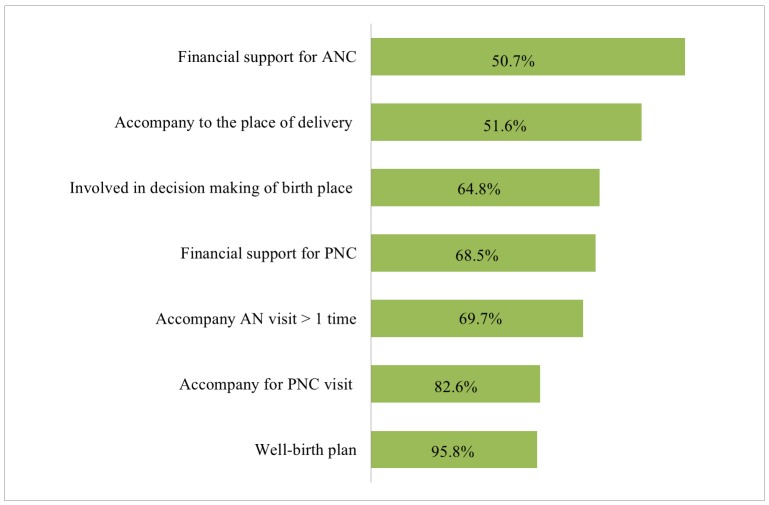
Of 426 husbands, 64.8% accompanied their spouses for an antenatal visit more than once while 51.6% accompanied them for a postnatal visit. Husbands were major financial supporters for both antenatal (95.8%) and postnatal care (68.5%). Overall, 69.7% were involved in decision making about the place of delivery. Regarding birth preparedness, the majority of husbands prepared for skilled birth attendance (91.1%), delivery place (83.6%), and money saving (81.7%) before their spouses gave birth. In contrast, fewer planned for a potential blood donor (15.5%) and a safe delivery kit (21.1%). In the context of maternal health, predictors of husband’s involvement were parity, educational level, type of marriage, decision making level in family, exposure to maternal health education and perception of risk during pregnancy and childbirth. Increased utilization of maternal health services was found among spouses of husbands who accompanied them to antenatal visits (AOR 5.82, 95% CI, 3.34–10.15) and those who had a well birth plan (AOR 2.42, 95% CI, 1.34–4.39 for antenatal visit and AOR 2.88, 95% CI, 1.52–5.47 for postnatal visit).
Conclusion
The majority of husbands supported their spouses’ maternal care services use financially; however, they were less involved in birth preparedness and postnatal care. Exposure to maternal health education and their maternal health knowledge were main predictors of their involvement. Women were more likely to use maternal care services when their husbands company them for ANC visits and had a well-birth plan in advance.
Introduction
Pregnancy and childbirth could threaten a woman’s life because of obstetric complications. Annually, worldwide maternal deaths contribute to more than half a million of deaths, and of these, 99% occur in developing countries [1, 2]. According to the World Health Organization (WHO), developing countries accounted for 286,000 of maternal deaths as a result of preventable complications in 2013 [2, 3]. Since appropriate health care services could diminish maternal morbidity and mortality, quality maternal care services should be utilized [4–7].
Husbands’ role is critical in pregnancy and childbirth of women, especially in making a decision about seeking appropriate health care services [8–12]. In patriarchal societies, pregnancy and child birth were often regarded as the women’s exclusive concern [9, 13, 14]. However, husbands are potentially involved in three levels of delays in obstetric emergencies: namely delay in awareness of emergency, delay in seeking care and delay in access to health care providers [15–18]. They are also becoming recognized as key players as their unsupportive attitude could cause a negative impact on the health of their spouses and children [15, 19, 20]. Therefore, since 2001, WHO incorporated husbands into reproductive health programs to achieve safe motherhood [20, 21].
Husbands’ involvement has so far improved the use of reproductive health services, birth preparedness and psycho-social well-being for their spouses [20, 22–24]. For example, husband participation in voluntary HIV counseling and testing was positively associated with uptake of HIV transmission prevention interventions in Kenya [23]. Similarly, in India, husband antenatal attendance was associated with increased skilled birth attendance [25]. Moreover, in Nepal, by educating both husbands and wives in couples, more wives used maternal health services, compared to educating wives alone [22].
Myanmar is still progressing towards meeting the fifth Millennium Development Goal (MDG). The maternal death rate is estimated at over 300 deaths per 100,000 live births [26–29]. Myanmar lags behind most Asian countries such as Vietnam, India and Malaysia in achieving MDG 5 [26–29]. Although the government invests more to improve maternal health services, Myanmar women continue to use these services unsatisfactorily, reflecting the insufficient progress towards MDG 5 [29–32]. In Myanmar, economic, socio-cultural and geographical factors solely or jointly determine a woman’s decision to uptake maternal health services [33, 34]. Meanwhile, husbands’ participation in maternal health also predisposes a challenge on the women’s uptake of maternal health care services in Myanmar [35].
The determinants of husbands’ involvement in maternal care have been explored. However, most of them were either qualitative or descriptive studies [8, 9, 13, 36] or included only limited characteristics of husbands’ involvement [21, 36–38]. In addition, only a few studies have examined the characteristics of husbands’ involvement in three different phases including antenatal, delivery, and postnatal periods [8, 9, 39]. Although husbands critically influence maternal health, little has been explored about the role of husbands in maternal health. Moreover, little is known about how husbands are involved in their spouses’ utilization of maternal care services in Myanmar. Therefore, this study aimed to identify the level of husbands’ involvement in maternal care services and its associated factors in Myanmar. This study also identified the associations between husbands’ involvement and their spouses’ utilization of maternal care services.
Methods
Study design and setting
A cross-sectional study was conducted in Thingangyun Township, Yangon, Myanmar in June and July 2014. Myanmar has 15 regions; a region is composed of districts, and each district is then subdivided into townships. A township is composed of village tracts in rural areas and towns or wards in urban areas [40]. Thingagyun Township consists of 38 wards, covering an estimated 14.8 square kilometer with a total population of 194,173 (5,925 children were under two years of age) in 2014.
Eligible participants were husbands aged 18 years and above who had at least one child within two years at the time of interview. A total of 433 eligible participants were recruited. For sampling, a two-staged random sampling method was adopted. In the first stage, 20 wards were randomly selected from total 38 wards. In the second stage, out of assumed 5,925 husbands, 433 eligible participants were selected from the list of fathers of children under the extended program on immunization (EPI) obtained from the township health center. This township health center manages the EPI program of all wards, including the outreach programs.
Data collection
The tool for data collection was a structured questionnaire (S1 Appendix). The questionnaire items were adapted from survey tools and indicators for maternal and newborn health developed by Jhpiego, an affiliate of Johns Hopkins University [41], Demographic Health Survey (DHS) and relevant prior studies [8, 9, 34]. It comprised four parts: covering 1) socio-demographic characteristics of participants; 2) knowledge of risk of pregnancy and childbirth; 3) assessment of husbands’ involvement in maternal care; and 4) cue for involvement in utilization of maternal care services. The questionnaire was initially prepared in English and translated into the Myanmar Language. To enhance the accuracy of the translation, it was back translated into English by two independent local medical doctors who were familiar with maternal health care. Face to face interviews were conducted by the lead researcher and four trained research assistants. Each interview took about 30 minutes on average. Before collecting the data, the lead researcher conducted a training program for the research assistants to enable them to be familiar with the concept of this study and understand the questions. The same questionnaire was also pretested among 20 participants in Mingalar Taungnyunt Township to correct inconsistencies and inappropriate questions.
Measurements
In this study, husbands’ involvement is the variable of interest. It refers to 1) antenatal care (ANC) accompaniment once or more; 2) financial support for ANC; 3) birth preparedness [saving money for delivery, purchasing a safe delivery kit, planning for a place and skilled birth attendant for delivery, arranging of transportation for delivery, planning for a potential blood donor], 4) involvement in decision making of the delivery place, 5) accompaniment to the place of delivery and 6) PNC accompaniment; and 7) financial support for PNC. The current study examined separately each variable of husband’s involvement and its associated factors.
Dichotomous questions were used to assess the antenatal, delivery and postnatal accompaniment, financial support for ANC and PNC, and the characteristics of birth preparedness. Birth preparedness was measured by scoring one point for each characteristic, and it was categorized as “well planned” or “not well planned”. The cut-off score was three in accordance with the mean score. Moreover, prior studies of birth preparedness applied this approach of categorization [18, 42, 43].
To assess the husband’s involvement in decision making about delivery place, participants were asked “Who made the final decision of where to give birth?” The responses included “yourself”, “your spouse,” “jointly with your spouse,” “other family member,” “health professional,” “friend,” and “others” [18, 41]. Responses were subdivided into two categories of husbands involved in decision making (“yourself” and “jointly with your spouse”) and others involved.
Independent variables included 1) socio-demographic characteristics including age, ethnicity, religion, education, occupation, monthly income, type of marriage, parity and spouse’s characteristics [8, 9, 21, 36]; 2) knowledge of the risk of pregnancy and childbirth accessed by their knowledge of the danger signs of pregnancy and childbirth. It was measured by using a single question with multiple danger signs. One point was scored for each danger sign and the total score was summed [41]; 3) perception of pregnancy and childbirth was accessed by whether or not they perceived pregnancy and childbirth as life-threatening conditions and maternal care as a necessity [9]; 4) cue for involvement in maternal care refers to any facilitation for husbands to be involved in maternal health. It was assessed by whether participants had ever received any maternal health education and their past experiences about pregnancy and childbirth [21, 41].
Dependent variables were the utilization of maternal care services. These included four or more antenatal visits, choice of delivery care services as home delivery (with skilled or unskilled birth attendant) or institutional delivery (public or private), and receiving PNC [21, 37]. Dichotomous questions were asked to measure the utilization of maternal care services.
Data analysis
Statistical Analysis was done by Stata 13.1. Descriptive analysis was used to summarize the socio-demographic characteristics and the level of husband’s involvement. Different multiple logistic regression models were constructed to access the factors associated with each of the characteristics of husband’s involvement. Later, three different multiple logistic regression models were run to identify the associations between husbands’ involvement and their spouses’ utilization of maternal care services. The models included the variables which have theoretical or rational associations in prior studies [8, 9, 21, 36, 37]. The significance level was set at a p-value of <0.05.
Ethical considerations
This study was approved by the Research Ethics Committee of the Graduate School of Medicine, the University of Tokyo, Japan. Ethical approval was also obtained from the Department of Medical Research (Lower Myanmar), Yangon, Myanmar. The study objectives were explained to the participants before each interview. Confidentiality was assured and written informed consent was taken from all participants.
Results
Background characteristics of participants
Of 433 husbands, 426 husbands completed the interview in this study (response rate = 98.4%). Table 1 shows the socio-demographic characteristics of husbands. Their mean age was 34.0 (Standard deviation [SD] 6.9) years while that of their spouses was 30.7 (SD 6.5) years. Of 426 husbands, 75.6% followed Buddhism and 68.3% were Bamar. More than half completed high school or higher levels of education (68.1%). The majority of them acquired monogamous marriage (95.3%). Husbands mainly decided for the health care in families (58.4%), followed by jointly with spouse (22.2%), spouse alone (13.2%) and the others (5.6%).
Table 1. Background Characteristics of Participants (n = 426).
| Characteristics | n | % | Mean | SD | |
|---|---|---|---|---|---|
| Age (years) | 426 | 34.0 | 6.9 | ||
| Religion | |||||
| Buddhist | 322 | 75.6 | |||
| Others | 104 | 24.4 | |||
| Ethnicity | |||||
| Bamar | 291 | 68.3 | |||
| National Races† | 67 | 15.7 | |||
| Others | 68 | 16.0 | |||
| Education | |||||
| Middle school or lower | 136 | 31.9 | |||
| High school or higher | 290 | 68.1 | |||
| Occupation | |||||
| Government worker | 45 | 10.6 | |||
| Private/company worker | 52 | 12.2 | |||
| Labor or driver | 144 | 33.8 | |||
| Own business | 144 | 33.8 | |||
| Unemployed or others | 41 | 9.6 | |||
| Income per month (USD)# | 426 | 236.2 | 172.9 | ||
| Income situation | |||||
| Regular | 181 | 42.5 | |||
| Non-regular | 242 | 56.8 | |||
| Missing | 3 | 0.7 | |||
| Type of marriage | |||||
| Monogamous | 406 | 95.3 | |||
| Polygamous | 20 | 4.7 | |||
| Currently living with spouse | |||||
| No | 18 | 4.2 | |||
| Yes | 408 | 95.8 | |||
| Number of children | |||||
| Only one | 193 | 45.3 | |||
| More than one | 233 | 54.7 | |||
| Spouse’s age (years) | 426 | 30.7 | 6.5 | ||
| Spouse’s education | |||||
| Middle school or lower | 164 | 38.5 | |||
| High school or higher | 262 | 61.5 | |||
| Spouse’s occupation | |||||
| Unemployed/house-wife | 300 | 70.4 | |||
| Employed | 126 | 29.6 | |||
| Decision maker regarding health care in family | |||||
| Yourself | 249 | 58.5 | |||
| Your spouse | 56 | 13.1 | |||
| Jointly with your spouse | 97 | 22.2 | |||
| Others | 24 | 5.6 | |||
†National races include Kachin, Kayar, Kayin, Chin, Mon, Yakhine and Shan.
# 1USD = 957.9 kyats, as of 1st July, 2014.
Husband’s involvement in maternal care
As shown in Fig 1, 276 husbands (64.8%) accompanied their spouses’ antenatal visit more than once while 408 (95.8%) provided money for ANC. A total of 279 (69.7%) were involved in decision making about delivery places. Regarding PNC, 51.6% accompanied their spouses and 68.5% provided financial support. Table 2 presents more insight into husbands’ involvement regarding the birth preparedness. Only small percentages of husbands prepared for a potential blood donor (15.5%) and safe delivery kit (21.1%). The majority planned for the delivery place (83.6%), skilled birth attendant (91.1%) and saved money (81.7%) before their spouses gave birth. About half of them (52.1%) planned for the transportation to the delivery place in advance.
Fig 1. Level of Husband’s Involvement in Maternal Care (n = 426).
Table 2. Characteristics of Birth Preparedness (n = 426).
| Characteristics | Number | Percentage (%) | |
|---|---|---|---|
| Arrange or save money | |||
| No | 78 | 18.3 | |
| Yes | 348 | 81.7 | |
| Plan for transportation | |||
| No | 204 | 47.9 | |
| Yes | 222 | 52.1 | |
| Plan for a delivery place | |||
| No | 70 | 16.4 | |
| Yes | 356 | 83.6 | |
| Arrange a skilled birth attendant | |||
| No | 38 | 8.9 | |
| Yes | 388 | 91.1 | |
| Purchase a safe delivery kit | |||
| No | 336 | 78.9 | |
| Yes | 90 | 21.1 | |
| Plan for a potential blood donor | |||
| No | 360 | 84.5 | |
| Yes | 66 | 15.5 | |
Table 3 presents the factors associated with husband’s involvement by the multivariable logistic regressions. Having more than one child was negatively associated with antenatal accompaniment (AOR 0.44, 95% CI 0.24–0.81, p = 0.008), having a well-birth plan (AOR 0.44, 95% CI 0.26–0.75, p = 0.003), postnatal accompaniment (AOR 0.24, 95% CI 0.13–0.43, p < 0.001) and financial support for PNC (AOR 0.20, 95% CI 0.09–0.46, p < 0.001). Likewise, polygamous marriage had a negative association with antenatal accompaniment (AOR 0.24, 95% CI 0.07–0.78, p < 0.05), delivery care accompaniment (AOR 0.34, 95% CI 0.12–0.96, p < 0.05) and postnatal care accompaniment (AOR 0.21, 95% CI 0.04–0.98, p < 0.05). Educated husbands were more likely to provide financial support for ANC (AOR 6.08, 95% CI 1.48–25.97, p = 0.012). Husbands were involved more in decision making of their spouses’ delivery place when they were the main decision maker in a family. Additionally, exposure to maternal health education was positively associated with antenatal accompaniment more than once (AOR 2.00, 95% CI 1.10–3.62, p = 0.022), having a well-birth plan (AOR 2.86, 95% CI 1.59–5.14, p < 0.001), and postnatal accompaniment (AOR 6.92, 95% CI 3.31–14.47, p < 0.001). Contrary to other studies, age, monthly income and spouse’s occupation had no significant association with husbands’ involvement in this study [8–10, 36].
Table 3. Multivariable Analysis for the Factors Associated with Husband’s Involvement in Maternal Care (n = 426).
| Variables | Antenatal | Delivery | Postnatal | |||||
|---|---|---|---|---|---|---|---|---|
| AOR A (95% CI) | AOR B (95% CI) | AOR C (95% CI) | ||||||
| Accompany ANC > one time | Financial support for ANC | Well birth-planned | Accompany to the place of delivery | Decision making of a delivery place | Accompany for PNC visit | Financial support for PNC | ||
| Age (years) | ||||||||
| ≤ 30 (ref) | 1.0 | |||||||
| >30 | 1.17(0.61–2.24) | 1.03(0.19–5.52) | 1.09(0.61–1.94) | 0.90(0.40–2.01) | 0.84(0.44–1.62) | 1.16(0.61–2.22) | 1.44(0.56–3.64) | |
| Education | ||||||||
| Middle school of lower (ref) | 1.0 | |||||||
| High school or higher | 1.32(0.76–2.28) | 6.08(1.48–25.97)* | 1.22(0.74–2.01) | 1.16(0.63–2.13) | 0.83(0.47–1.47) | 1.03(0.55–1.93) | 1.09(0.53–2.21) | |
| Spouse’s age (years) | ||||||||
| ≤ 30 (ref) | 1.0 | |||||||
| >30 | 1.37(0.77–2.41) | 0.80 (0.20–3.21) | 1.76(1.04–2.98)* | 0.82(0.43–1.59) | 1.47(0.82–2.64) | 1.34(0.74–2.43) | 0.57(0.27–1.23) | |
| Number of child/children | ||||||||
| Only one (ref) | 1.0 | |||||||
| More than one | 0.44(0.24–0.81)** | 0.34(0.54–2.16) | 0.44(0.26–0.75)** | 0.60(0.28–1.27) | 0.96(0.51–1.78) | 0.24(0.13–0.43)*** | 0.20(0.09–0.46)*** | |
| Type of marriage | ||||||||
| Monogamous (ref) | 1.0 | |||||||
| Polygamous | 0.24(0.07–0.78)* | 0.39(0.06–2.47) | 0.92(0.30–2.78) | 0.34(0.12–0.96)* | 1.44(0.46–4.53) | 0.21(0.04–0.98)* | 0.22(0.04–1.12) | |
| Decision maker regarding health care in family | ||||||||
| Yourself (ref) | 1.0 | |||||||
| Your spouse | 0.84(0.36–1.95) | 0.96(0.10–8.72) | 0.98(0.45–2.16) | 2.56(0.88–7.64) | 0.06(0.02–0.13)*** | 0.80(0.33–1.92) | 2.43(0.69–8.55) | |
| Jointly with your spouse | 0.96(0.49–1.87) | 0.95(0.17–5.39) | 1.08(0.69–2.16) | 1.43(0.61–3.37) | 1.58(0.73–3.43) | 0.46(0.24–1.03) | 0.45(0.18–1.09) | |
| Others | 0.80(0.28–2.25) | 0.18(0.03–1.14) | 0.70(0.27–1.79) | 0.56(0.19–1.66) | 0.07(0.02–0.20)*** | 0.34(0.11–1.03) | 0.42(0.11–1.53) | |
| Have you received any information regarding with maternal health? | 2.00(1.10–3.62)** | 2.05(0.57–7.42) | 2.86(1.59–5.13)*** | 3.17(1.61–6.26)** | 2.03(1.07–3.85)* | 6.92(3.31–14.47)*** | 8.39(4.06–17.38)*** | |
| No (ref) | 1.0 | |||||||
| Yes | 2.00(1.10–3.62)* | 2.05(0.57–7.42) | 2.86(1.59–5.13)*** | 3.17(1.61–6.26)** | 2.03(1.07–3.85)** | 6.92(3.31–14.47)*** | 8.39(4.06–17.38)*** | |
| Knowledge about danger signs of pregnancy, childbirth and puperium | 1.51(1.07–2.13)** | 1.16(0.37–3.65) | 2.04(1.48–2.82)*** | 1.36(0.86–2.16) | 1.16(0.83–1.61) | 1.36(0.99–1.87) | 1.57(0.94–2.62) | |
*p-value<0.05
**p-value<0.01
***p-value<0.001.
ᴬ Adjusted for age, education, occupation, income per month, spouse’s age, spouse’s occupation, number of child/children, type of marriage, currently living with a spouse, decision maker regarding health care in a family, exposure to maternal health education, perception on risk of pregnancy and childbirth, knowledge about danger signs of pregnancy and childbirth, perception on ANC.
ᴮ Adjusted for age, education, occupation, income per month, spouse’s age, spouse’s occupation, number of child/children, type of marriage, currently living with a spouse, decision maker regarding health care in a family, exposure to maternal health education, perception on risk of pregnancy and childbirth, knowledge on danger signs of pregnancy and childbirth.
ᶜ Adjusted for age, education, occupation, income per month, spouse’s age, spouse’s occupation, number of child/children, type of marriage, currently living with a spouse, decision maker regarding health care in a family, exposure to maternal health education, perception on risk of pregnancy and childbirth, knowledge on danger signs of pregnancy and childbirth, perception on ANC, perception on PNC.
According to Fig 2, of total 426, 75.8% of spouses received ANC more than four times, and the majority of them (87.8%) used institutional delivery care. However, only 68.1% of them sought PNC from health personnel. Table 4 shows the associations between husbands’ involvement and their spouses’ utilization of maternal care services. Based on the bivariate analysis, some characteristics were excluded in multivariable models due to a very small number participant. The excluded characteristics were financial support for ANC, accompaniment to the place of delivery, PNC accompaniment, and financial support for PNC. By analyzing with three different multiple logistic regressions models, it was found that husbands’ ANC accompaniment more than once was positively associated with their spouses’ ANC visits more than four times (AOR 5.82, 95% CI, 3.34–10.15). Similarly, husbands having a well-birth plan had a strong positive association with their spouses’ antenatal visits more than four times (AOR 2.42, 95% CI, 1.34–4.39) and utilization of PNC services (AOR 2.88, 95% CI, 1.52–5.47).
Fig 2. Reported Their Spouses’ Utilization of Maternal Health Care Services (n = 426).
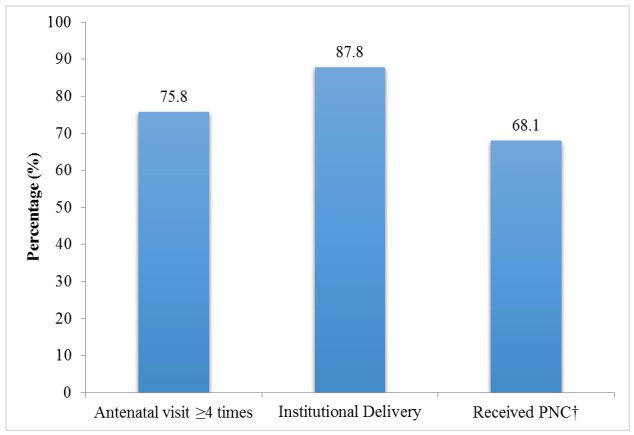
†n = 423.
Table 4. Multivariable Analysis for the Associations between Husband’s Involvement and Utilization of Maternal Care Services (n = 426).
| Variables | Antenatal visit > = 4 times (95%CI) | Institutional delivery (95%CI) | Received PNC†(95%CI) | ||||
|---|---|---|---|---|---|---|---|
| OR | AOR# | OR | AOR# | OR | AOR# | ||
| Accompany antenatal visit | |||||||
| No and < = one time (ref) | 1.0 | ||||||
| >one time | 9.47(5.69–15.77)*** | 5.82(3.34–10.15)*** | 4.64(2.50–8.62)*** | 1.93(0.92–4.04) | 4.06(2.63–6.26)*** | 1.37(0.73–2.61) | |
| Birth preparedness | |||||||
| Not well-planned (ref) | 1.0 | ||||||
| Well | 4.82(2.90–8.02)*** | 2.42(1.34–4.39)** | 5.92(2.81–12.50)*** | 2.25(0.96–5.28) | 5.94(3.72–9.47)*** | 2.88(1.52–5.47)** | |
| Decision making of delivery place | |||||||
| Others (ref) | 1.0 | ||||||
| Husbands involved | 1.77(1.11–2.81)* | 1.58(0.90–2.77) | 1.25(0.68–2.32) | 0.93(0.45–1.93) | 1.58(1.02–2.45)* | 1.23(0.64–2.53) | |
*p-value<0.05
**p-value<0.01
***p-value<0.001.
†n = 423.
#adjusted for age, education, occupation, spouse’s education, spouse’s occupation, number of child/children, type of marriage and exposure to maternal health education in addition to above mentioned variables in all three models.
Discussion
Husband involvement in maternal health was found to be off-balanced in Thingagyun Township. Specifically, their indirect involvement as financial support for maternal care (95.8% for ANC and 68.5% for PNC) was much higher compared to their direct involvement as accompaniment (64.8% for ANC and 51.6% for PNC). The regression models revealed that exposure to maternal health education and their maternal health knowledge were main predictors of their involvement in maternal care. This study also identified that women received maternal health care services more frequently when their husbands accompanied them to an antenatal visit and made a well-birth plan in advance.
As shown in Fig 1, husbands’ ANC and PNC accompaniment was relatively low, compared to their ANC and PNC financial support. The possible explanation could be due to gender norms and social discomfort in being present in a female-dominated environment [13, 36, 44]. Additionally, compared to antenatal and delivery periods, husbands involved less during the postnatal period in this study. PNC services utilization itself is comparatively lower than other periods in many developing countries including Myanmar [45–49]. Moreover, husbands may perceive that wives and children should be taken care by the female family members in the postnatal period, not by the male family members [50, 51]. They may not be aware the services available in the postnatal period or they may not perceive benefits from PNC visits [46]. Therefore, proper PNC should be encouraged with adequate consideration of socio-cultural norms.
This study showed that husbands were involved more in maternal health programs if they had higher maternal health knowledge. With respect to previous studies, lower knowledge on maternal health precluded husbands from positive participation and interest in maternal issues [19, 38, 52]. As a result, those husbands subsided their support on their spouses’ utilization of maternal care services [19, 51]. Therefore, this study highlights a call to recognize husbands as clients of maternal care services.
In this study, having more than one child and polygamous marriage were negatively associated with husband’s involvement. Husbands tend to pay more care and attention to their spouses’ maternal issues when the newborn is their first child or when they are in a monogamous marriage [9, 39]. In a polygamous society, husbands may have difficulty in changing their perception as they do not need to be involved in maternal issues [50]. Moreover, both having more than one child and polygamous marriage were known to be associated with lower utilization of maternal care services in many studies [37, 39, 53]. Thus, husbands’ involvement should be enhanced to mitigate barriers against maternal care services utilization.
Regarding the birth preparedness, husband’s involvement was notably low for some characteristics. For example, less husbands’ involvement was found in planning for transportation to the delivery place (52.1%), purchasing a safe delivery kit (21.1%), and arranging for a potential blood donor (15.5%). Husbands tend to expect that health centers are liable to provide necessary delivery materials. Consequently, this could contribute to low birth-preparedness for some characteristics. Birth preparedness packages have been proven to be an effective strategy in obstetric emergencies to reduce maternal mortality [41–43]. However, the characteristics of birth preparedness are not yet familiar among Myanmar husbands, and awareness should be raised not only for women but also for their partners.
In consistence with previous studies [34, 54], reported utilization of ANC services was 75.8% in this study. Institutional deliveries (87.8%) was much higher than the national 2010 UNFPA report in which 76.4% of deliveries took place at home [54]. These differing results could possibly be due to the peri-urban study setting and easy accessibility to health facilities [6, 34, 49]. This study reinforces how geological distance and proximity to health facilities determines the utilization of health care services.
In Table 4, having more than four skilled antenatal visits was positively associated with husbands’ antenatal accompaniment more than once. Furthermore, spouses were more likely to use skilled ANC when their husbands had well-birth plans. Women’s utilization of safe delivery care was considerably influenced by their husbands’ concern about pregnancy and childbirth in physical, psychological, or social context [5–7, 14]. In the prior studies, husbands’ antenatal accompaniment was considered as their direct involvement, and women had better birth outcomes when their husbands accompanied them to antenatal visits [6, 18]. Therefore, to achieve safe motherhood, one of the critical factors is to encourage husbands to be involved in maternal health.
This study had some limitations. First, this study setting was peri-urban; therefore, the findings could not be generalizable in large cities and rural areas. Second, eligible participants were selected from the list of fathers in the immunization program of children. Therefore, it is possible that some of the eligible participants may not have been in this list. Nevertheless, it may contribute only a small fraction since the immunization coverage is more than 95% in Yangon, Myanmar [30]. Third, recall bias could be present although the study included fathers of children less than two years. Lastly, in this study, the underlying reasons for their less involvement were not assessed in detail.
Conclusion
In Myanmar, although husbands’ involvement was high for financial support, they were less involved in birth preparedness and PNC as compared to ANC. More husbands’ involvement was found among higher educated husbands and husbands of primigravide. Exposure to maternal health education and their maternal health knowledge could increase their involvement. Husbands’ antenatal accompaniment and having a well birth plan enhanced their spouses’ utilization of maternal care services.
To strengthen husband encouragement, maternal health interventions should target husbands as consumers of maternal health services, hear more on postnatal issues, and raise their awareness about birth preparedness. Further qualitative studies are also recommended to address the underlying reasons of their less involvement and design effective interventions to improve their involvement.
Supporting Information
(DOCX)
Acknowledgments
First of all, the authors wish to express their deepest gratitude to all the respondents in this study. We would like to show our humble gratitude to Professor Dr. Khin Thet Wai (Department of Medical Research (Lower Myanmar)) for her expert advice and technical inputs in this study. We also would like to acknowledge all the Ethical Board members of Department of Medical Research (Lower Myanmar), all the officials and staff from Thingangyun Township Health Center for their support during my field visit.
Data Availability
Data are available upon request as a requirement of the Research Ethics Committee of the Graduate School of Medicine, the University of Tokyo, Japan. Ethical approval was also obtained from the Department of Medical Research (Lower Myanmar), Yangon, Myanmar. The authors agree to share the data set upon request considering the ethical issues from Department of Medical Research, Myanmar. Interested researchers may submit requests for data to the Corresponding Author.
Funding Statement
The data collection of this study was supported by Asian Development Bank Japan Scholarship Program’s research grant (http://www.adb.org/site/careers/japan-scholarship-program/main).
References
- 1. World Health Organization. Maternal death surveillence and response: Technical guidance information for action to prevent maternal dealth Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 2. WHO, UNICEF, UNFPA, the World Bank, the United Nations Population Division. Trends in Maternal Mortality: 1990 to 2013. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- 3. World Health Organization. Women and Health: Today's Evidence, Tomorrow's Agenda. Geneva, Switzerland: World Health Organization; 2009. [Google Scholar]
- 4. Ronsmans C, Graham WJ. Maternal mortality: who, when, where, and why. Lancet. 2006;368(9542):1189–200. [DOI] [PubMed] [Google Scholar]
- 5. Yanagisawa S, Oum S, Wakai S. Determinants of skilled birth attendance in rural Cambodia. Trop Med Int Health. 2006;11(2):238–51. [DOI] [PubMed] [Google Scholar]
- 6. Story WT, Burgard SA, Lori JR, Taleb F, Ali NA, Hoque DM. Husbands' involvement in delivery care utilization in rural Bangladesh: A qualitative study. BMC Pregnancy Childbirth. 2012;12:28 10.1186/1471-2393-12-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Agha S, Carton TW. Determinants of institutional delivery in rural Jhang, Pakistan. Int J Equity Health. 2011;10:31 10.1186/1475-9276-10-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bhatta DN. Involvement of males in antenatal care, birth preparedness, exclusive breast feeding and immunizations for children in Kathmandu, Nepal. BMC pregnancy and childbirth. 2013;13:14 10.1186/1471-2393-13-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Iliyasu Z, Abubakar IS, Galadanci HS, Aliyu MH. Birth preparedness, complication readiness and fathers' participation in maternity care in a northern Nigerian community. African journal of reproductive health. 2010;14(1):21–32. [PubMed] [Google Scholar]
- 10. Kakaire O, Kaye DK, Osinde MO. Male involvement in birth preparedness and complication readiness for emergency obstetric referrals in rural Uganda. Reproductive health. 2011;8:12 10.1186/1742-4755-8-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mullany BC, Hindin MJ, Becker S. Can women's autonomy impede male involvement in pregnancy health in Katmandu, Nepal? Soc Sci Med. 2005;61(9):1993–2006. [DOI] [PubMed] [Google Scholar]
- 12. Jennings L, Na M, Cherewick M, Hindin M, Mullany B, Ahmed S. Women's empowerment and male involvement in antenatal care: analyses of Demographic and Health Surveys (DHS) in selected African countries. BMC pregnancy and childbirth. 2014;14:297 10.1186/1471-2393-14-297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kululanga LI, Sundby J, Malata A, Chirwa E. Male involvement in maternity health care in Malawi. African journal of reproductive health. 2012;16(1):145–57. [PubMed] [Google Scholar]
- 14. Carter M. Husbands and maternal health matters in rural Guatemala: wives' reports on their spouses' involvement in pregnancy and birth. Soc Sci Med. 2002;55(3):437–50. [DOI] [PubMed] [Google Scholar]
- 15. Dudgeon MR, Inhorn MC. Men's influences on women's reproductive health: medical anthropological perspectives. Soc Sci Med. 2004;59(7):1379–95. [DOI] [PubMed] [Google Scholar]
- 16. Barnes-Josiah D, Myntti C, Augustin A. The "three delays" as a framework for examining maternal mortality in Haiti. Soc Sci Med. 1998;46(8):981–93. [DOI] [PubMed] [Google Scholar]
- 17. Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med. 1994;38(8):1091–110. [DOI] [PubMed] [Google Scholar]
- 18. Kabakyenga JK, Ostergren PO, Turyakira E, Pettersson KO. Influence of birth preparedness, decision-making on location of birth and assistance by skilled birth attendants among women in south-western Uganda. PloS one. 2012;7(4):e35747 10.1371/journal.pone.0035747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Theuring S, Mbezi P, Luvanda H, Jordan-Harder B, Kunz A, Harms G. Male involvement in PMTCT services in Mbeya Region, Tanzania. AIDS and behavior. 2009;13 Suppl 1:92–102. 10.1007/s10461-009-9543-0 [DOI] [PubMed] [Google Scholar]
- 20.Wendy Holmes JD, Stanley Lunchers. Engaging men in reproductive, maternal and newborn health Compass; 2013. Available: http://www.who.int/pmnch/knowledge/publications/summaries/ks26/en/.
- 21. Tweheyo R, Konde-Lule J, Tumwesigye NM, Sekandi JN. Male partner attendance of skilled antenatal care in peri-urban Gulu district, Northern Uganda. BMC Pregnancy Childbirth. 2010;10:53 10.1186/1471-2393-10-53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mullany BC, Becker S, Hindin MJ. The impact of including husbands in antenatal health education services on maternal health practices in urban Nepal: results from a randomized controlled trial. Health education research. 2007;22(2):166–76. [DOI] [PubMed] [Google Scholar]
- 23. Farquhar C, Kiarie JN, Richardson BA, Kabura MN, John FN, Nduati RW, et al. Antenatal couple counseling increases uptake of interventions to prevent HIV-1 transmission. J Acquir Immune Defic Syndr. 2004;37(5):1620–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ditekemena J, Koole O, Engmann C, Matendo R, Tshefu A, Ryder R, et al. Determinants of male involvement in maternal and child health services in sub-Saharan Africa: a review. Reprod Health. 2012;9:32 10.1186/1742-4755-9-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chattopadhyay A. Men in maternal care: evidence from India. J Biosoc Sci. 2012;44(2):129–53. 10.1017/S0021932011000502 [DOI] [PubMed] [Google Scholar]
- 26. UNFPA. Maternal and Neonatal Health in East and South East Asia. Bangkok, Thailand: UNFPA Country Technical Services Team; 2006. [Google Scholar]
- 27. UNICEF, World Health Organization. Countdown to 2015: Building a future for women and children, The 2012 report Geneva, Switzerland: World Health Organization, 2012. [Google Scholar]
- 28. Acuin CS, Khor GL, Liabsuetrakul T, Achadi EL, Htay TT, Firestone R, et al. Maternal, neonatal, and child health in southeast Asia: towards greater regional collaboration. Lancet. 2011;377(9764):516–25. 10.1016/S0140-6736(10)62049-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. United Nations Country Team in Myanmar. Achieving Millennium Developments Goals in Myanmar: Thematic analysis 2011. Yangon, Myanmar: United Nations Myanmar; 2011. [Google Scholar]
- 30. Requejo J, Victora C, Bryce J. Data resource profile: countdown to 2015: maternal, newborn and child survival. Int J Epidemiol. 2014;43(2):586–96. 10.1093/ije/dyu034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ministry of Health, Myanmar. Five-year strategic plan for reproductive health in Myanmar (2009–2013) Nay Pyi Taw, Myanmar: Department of Health, Ministry of Health; 2009. [Google Scholar]
- 32. Saw YM, Win KL, Shiao LW, Thandar MM, Amiya RM, Shibanuma A, et al. Taking stock of Myanmar's progress toward the health-related Millennium Development Goals: current roadblocks, paths ahead. Int J Equity Health. 2013;12:78 10.1186/1475-9276-12-78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Shen C, Williamson JB. Maternal mortality, women's status, and economic dependency in less developed countries: a cross-national analysis. Soc Sci Med. 1999;49(2):197–214. [DOI] [PubMed] [Google Scholar]
- 34. Sein KK. Maternal health care utilization among ever married youths in Kyimyindaing Township, Myanmar. Matern Child Health J. 2012;16(5):1021–30. 10.1007/s10995-011-0815-8 [DOI] [PubMed] [Google Scholar]
- 35. Sen BK. Women and the law in Burma. Legal Issue on Burma. 2001;9:28–43. [Google Scholar]
- 36. Olayemi O, Bello FA, Aimakhu CO, Obajimi GO, Adekunle AO. Male participation in pregnancy and delivery in Nigeria: a survey of antenatal attendees. J Biosoc Sci. 2009;41(4):493–503. 10.1017/S0021932009003356 [DOI] [PubMed] [Google Scholar]
- 37. Mangeni J, Nwangi A, Mbugua S, Mukthar V. Male involvement in maternal healthcare as a determinant of utilisation of skilled birth attendants in Kenya. East Afr Med J. 2014;89(11):372–83. [PubMed] [Google Scholar]
- 38. Ampt F, Mon MM, Than KK, Khin MM, Agius PA, Morgan C, et al. Correlates of male involvement in maternal and newborn health: a cross-sectional study of men in a peri-urban region of Myanmar. BMC Pregnancy Childbirth. 2015;15:122 10.1186/s12884-015-0561-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Redshaw M, Henderson J. Fathers' engagement in pregnancy and childbirth: evidence from a national survey. BMC Pregnancy Childbirth. 2013;13:70 10.1186/1471-2393-13-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ministry of Information, Myanmar. Constitution of the Republic of the Union of Myanmar. Nay Pyi Taw, Myanmar: Ministry of Information; 2008. [Google Scholar]
- 41. Del Barco R. Monitoring birth preparedness and complication readiness Tools and indicators for maternal and newborn health. Baltimore, Maryland: JHPIEGO; 2004. [Google Scholar]
- 42. Agarwal S, Sethi V, Srivastava K, Jha PK, Baqui AH. Birth preparedness and complication readiness among slum women in Indore city, India. J Health Popul Nutr. 2010;28(4):383–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Kaso M, Addisse M. Birth preparedness and complication readiness in Robe Woreda, Arsi Zone, Oromia Region, Central Ethiopia: a cross-sectional study. Reprod Health. 2014;11:55 10.1186/1742-4755-11-55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mumtaz Z, Salway SM. Gender, pregnancy and the uptake of antenatal care services in Pakistan. Sociol Health Illn. 2007;29(1):1–26. [DOI] [PubMed] [Google Scholar]
- 45. Sein KK. Beliefs and practices surrounding postpartum period among Myanmar women. Midwifery. 2013;29(11):1257–63. 10.1016/j.midw.2012.11.012 [DOI] [PubMed] [Google Scholar]
- 46.Lawn J, Kerber K. Opportunities for Africas newborns: practical data policy and programmatic support for newborn care in Africa. Cape Town, South Africa, Partnership for Maternal, Newborn and Child Health; 2006.
- 47. Chakraborty N, Islam MA, Chowdhury RI, Bari W. Utilisation of postnatal care in Bangladesh: evidence from a longitudinal study. Health Soc Care Community. 2002;10(6):492–502. [DOI] [PubMed] [Google Scholar]
- 48. Liu N, Mao L, Sun X, Liu L, Chen B, Ding Q. Postpartum practices of puerperal women and their influencing factors in three regions of Hubei, China. BMC public health. 2006;6:274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Islam MR, Odland JO. Determinants of antenatal and postnatal care visits among Indigenous people in Bangladesh: a study of the Mru community. Rural and remote health. 2011;11(2):1672 [PubMed] [Google Scholar]
- 50. Kwambai TK, Dellicour S, Desai M, Ameh CA, Person B, Achieng F, et al. Perspectives of men on antenatal and delivery care service utilisation in rural western Kenya: a qualitative study. BMC Pregnancy Childbirth. 2013;13:134 10.1186/1471-2393-13-134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Mullany BC. Barriers to and attitudes towards promoting husbands' involvement in maternal health in Katmandu, Nepal. Soc Sci Med. 2006;62(11):2798–809. [DOI] [PubMed] [Google Scholar]
- 52. Kaye DK, Kakaire O, Nakimuli A, Osinde MO, Mbalinda SN, Kakande N. Male involvement during pregnancy and childbirth: men's perceptions, practices and experiences during the care for women who developed childbirth complications in Mulago Hospital, Uganda. BMC Pregnancy Childbirth. 2014;14:54 10.1186/1471-2393-14-54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Gyimah SO, Takyi BK, Addai I. Challenges to the reproductive-health needs of African women: on religion and maternal health utilization in Ghana. Soc Sci Med. 2006;62(12):2930–44. [DOI] [PubMed] [Google Scholar]
- 54. UNFPA. Report on situation analysis of population and development, reproductive health and gender in Myanmar Yangon, Myanmar: UNFPA; 2010. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
Data Availability Statement
Data are available upon request as a requirement of the Research Ethics Committee of the Graduate School of Medicine, the University of Tokyo, Japan. Ethical approval was also obtained from the Department of Medical Research (Lower Myanmar), Yangon, Myanmar. The authors agree to share the data set upon request considering the ethical issues from Department of Medical Research, Myanmar. Interested researchers may submit requests for data to the Corresponding Author.