Abstract
Study Design Case report.
Objective Treatment of gunshot wounds to the spine is a topic of continued discussion and controversy. The following case study provides a description of a patient with a gunshot wound to the lumbar spine with a retained bullet in the intrathecal space.
Methods Immediately after gunshot injury, a patient developed lumbar and radicular pain, as well as neurologic deficits. He was taken for surgery to remove the retained bullet.
Results Following surgery, pain and neurologic function improved. The operative techniques and the postoperative clinical management are discussed in this report.
Conclusion In our opinion, it was necessary to remove the bullet to avoid migration and possible worsening of neurologic function. However, surgical intervention is not appropriate in every case, and ultimately decisions should be based on patient presentation, symptomology, and imaging.
Keywords: intrathecal foreign object, bullet, gunshot wound
Introduction
Despite an increased incidence of studies analyzing bullet fragments lodged in the spinal canal, there is no clear consensus regarding the treatment of such injuries. In cases of spinal fracture secondary to a gunshot wound, the evidence suggests the fractures tend to be stable and not necessitate surgical intervention.1 However, some researchers advocate that surgery is indicated due to the possibility of migration of the intrathecal fragment, particularly when in close proximity to the conus.2 When surgery is elected, careful attention to the surrounding structures with regards to the location of the fragment is required, as well as a thorough analysis of the preexisting neurologic compromise and duration from the time of injury. In this report, we discuss a patient with a 4-week-old gunshot wound and retained bullet in the lumbar spine, including the technical nuances to consider for the procedure and subsequent care.
Case Report
A 30-year-old man presented to an outside emergency department with a penetrating gunshot wound to the abdomen. Upon examination, the patient had one gunshot wound to the left upper quadrant. A computed tomography (CT) scan of the abdomen verified the bullet had fractured the left L2 pedicle before becoming lodged in the spinal canal between L2 and L3. Neurologically, his only deficit was left lower extremity quadriceps weakness, 4/5 strength. He was taken for an urgent laparotomy for exploration of the peritoneum, with findings of a hemoperitoneum, six small bowel enterotomies, a left perinephric hematoma, a grade 2 renal laceration, as well as a laceration of the left psoas muscle. Postoperatively, the patient had urinary retention, which resolved within 2 days.
The patient was directed to our institution 4 weeks after the injury for specialized neurosurgical care. The left quadriceps weakness was unchanged from the time of injury, but the patient had developed subsequent paresthesia in the left foot, as well as bilateral lower extremity radiculopathy radiating down the lateral thighs and posterior calves (pain score of 8 to 9 on a scale of 0 to 10). A CT myelogram of the lumbar spine confirmed the unchanged location of the bullet in the spinal canal with high-grade blockage of the cerebrospinal fluid (CSF) above the level of the bullet (Fig. 1).
Fig. 1.

Computed tomography myelogram of the lumbar spine. (A) Sagittal view showing the unchanged location of the bullet in the spinal canal with high-grade blockage of the cerebrospinal fluid above the level of the bullet. (B) Axial view showing a fracture of the left L2 pedicle.
Operative Procedure
The patient was taken to the operative theater for a lumbar laminectomy of L2–L3 and removal of the bullet. Although a fusion was not expected to be necessary, the required instrumentation was available if instability was noted intraoperatively. After induction of general anesthesia, the patient was placed in a prone position on a Jackson table. A standard L2–L3 laminectomy was performed, and a palpable, hard mass was discerned in the dural sac. Prior to opening the dura, a thorough inspection of the thecal sac was completed to evaluate the exact location of the bullet (i.e., intradural, extradural) and to assess if there was a sealed durotomy from the injury or whether a remaining open, leaking portion of the sac required further intervention and repair.
Once concluded that the bullet was intrathecal, an 11-blade knife was used to open the dura at the midline. There was no release of CSF with the incision. A 9-mm bullet was found with its head facing the incision, completely encased in scar tissue, blocking the flow of CSF (Fig. 2). It was deduced that the high amount of heat produced by the bullet entering the dural sac split the nerve roots and encased the bullet. A slow dissection was performed with caution to avoid any damage to the nerve roots. Microscopic magnification with extraction of 1 to 2 mm of dissection at a time was utilized for the release of the bullet from the scar tissue and dura. Excessive retraction was avoided to reduce risk of undue stress on the nerve roots. Ultimately, the bullet was successfully released from the surrounding tissue (Fig. 3).
Fig. 2.
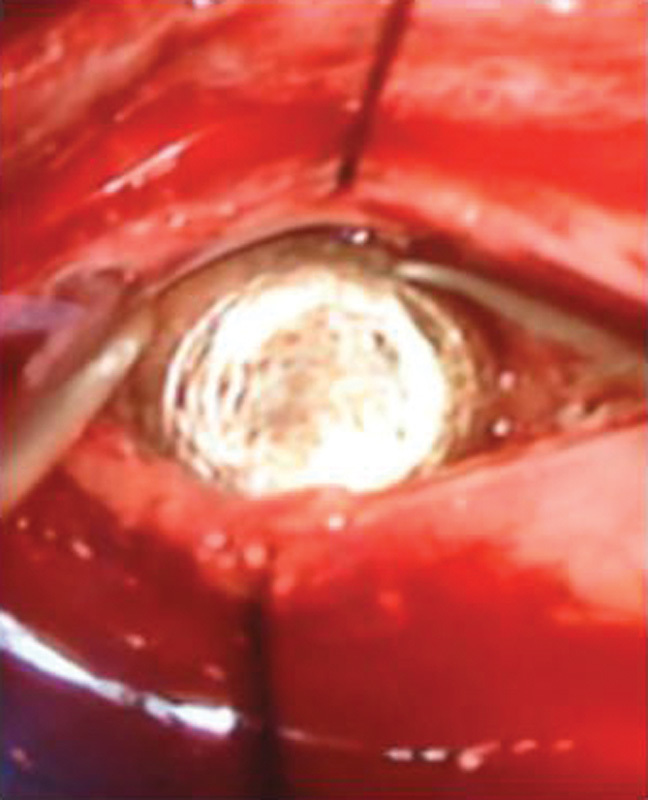
Intraoperative view of the 9-mm bullet with its head facing the incision, completely encased in scar tissue, blocking the flow of cerebrospinal fluid.
Fig. 3.
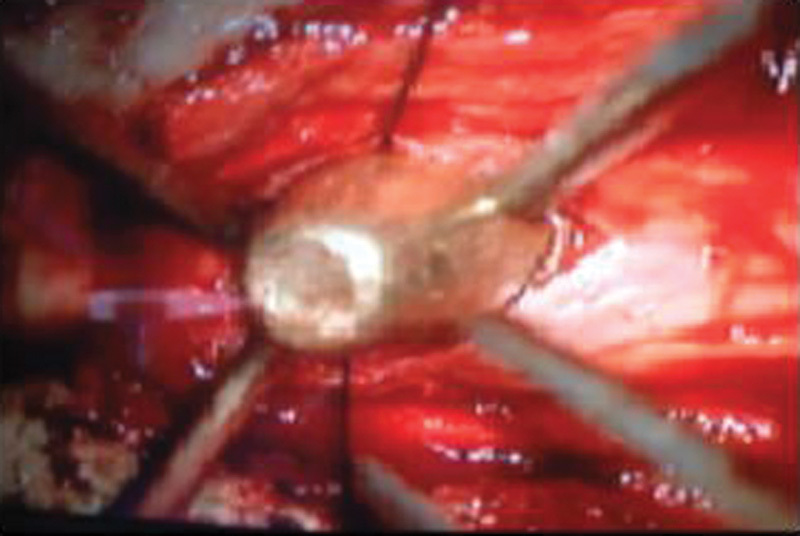
Intraoperative view demonstrating the bullet successfully released from the surrounding tissue.
Throughout the dissection and with wound closure, no CSF was appreciated. Multiple Valsalva maneuvers were administered to a pressure of 40 cmH2O with still no noticeable leak. The dura was closed in a watertight fashion with a 6–0 Prolene (Ethicon, Somerville, New Jersey, United States). A lumbar drain was inserted above the level of the laminectomy as a precaution to avoid an unrecognized fistula leaking at a later time.
Postoperative Course
Upon awaking from anesthesia, the patient had worsening of his left lower extremity weakness (3+/5), but notable improvement in his lumbar and radicular symptoms (pain score of 4 on a scale of 0 to 10). The lumbar drain was kept in place for 72 hours with intermittent drainage of 10 to 15 mL of CSF hourly. It was clamped on the evening of postoperative day 3, and the patient was ambulated multiple times without evidence of a CSF leak (i.e., drainage from the wound, nausea/vomiting, or headache). The drain was discontinued without complication on postoperative day 4. At discharge, his left lower extremity weakness was improved from his baseline at admission (5−/5).
Discussion
The management of an intradural bullet continues to remain controversial.3 4 5 Proponents of the conservative theory support a nonsurgical approach with cautious measures involving pain management and rehabilitation,6 although others recommend surgical intervention with the anticipation of a more rapid improvement in neurologic symptoms.7 At the root level of the spine, it is our opinion that in several case instances, the removal of the foreign object will lead to better outcomes and carries a higher potential for regeneration of the axons of the injured nerve roots.4 5 A thorough understanding of the regional anatomy is crucial when determining the appropriateness of surgery versus conservative measures; decisions should be made on a case-by-case basis.
For the case presented, we felt the removal of the bullet from the canal was necessary to improve this patient's quality of life, as evidenced by decreased pain, as well as to avoid future complications related to the possible migration of the bullet. Although continued back pain secondary to arachnoiditis is possible, given the patient's young age, it was our opinion that preserving his neurologic function was of utmost importance. Ultimately, a careful dissection technique and detailed postoperative care are imperative to success with each case.
Conclusion
In our opinion, it is necessary to remove an intradural bullet or larger fragments to avoid migration and possible worsening of neurologic function. However, surgical intervention is not appropriate in every case, and ultimately decisions should be based on patient presentation, symptomology, and imaging.
Footnotes
Disclosures Marc D. Moisi, none Jeni Page, none Seymour Gahramanov, none Rod J. Oskouian, none
Editorial Perspective
Sadly, the subject of gunshot wounds to the spine and the preferred form of management remain a relevant but commonly overlooked topic, in large part due to the variability of injury mechanisms (high versus low velocity; hollow tip versus penetrating missiles or shrapnel; metal composition and presence of wadding; concurrent concussive trauma or cavitation) and patient factors (region of spine hit; type of neural structures encountered; bacterial wound contamination; concurrent vascular/abdominal trauma, overall injury load, health of patient, among others), which make any attempt at generalization or formal protocol-driven study difficult. As a review of the references in the article by Moisi et al and the commentary by Schroeder show, many of the key articles date back to the1980s and 1990s. The question of surgical removal of bullets and other projectiles from the spinal column and decompression of neural elements as well as the question of when to perform a surgical reconstruction with an instrumented fusion remain a prime example of anecdotal medicine.
As confirmed by Schroeder in his commentary, a few agreements have emerged over time:
Apply Advanced Trauma Life Support principles when approaching penetrating spine trauma.
Penetrating injuries to the cervical spine are probably best approached with a multispecialty concept under inclusion of interventional angiography.1
Penetrating spinal column trauma with concurrent viscous or esophageal contamination does not require surgical debridement of the spine to prevent infection; a course of appropriately selected intravenous antibiotics over a period of up to 2 weeks can suffice.2
Structural instability of the spinal column as a result of civilian-type low-velocity injures is rare in the thoracolumbar spine.
Patients with complete thoracic-level spinal cord injury have a nearly absent rate of recovery.3
Routine decompression of the spinal canal to clear it from smaller bony and metal fragments is not necessary.
Steroid use for spinal cord injury has not been shown to be beneficial.4
Long-term toxic effect of lead, copper, and other materials may emanate from bullet casings that are exposed to cerebrospinal fluid, disks, or joints (“plumbism”).5
Magnetic resonance imaging of a patient with retained bullet fragments requires clarification of the metal composition—alloy and copper is deemed safe, steel is not.6
Beyond these agreements, many issues remain unresolved; the exact indications for surgical decompression and the role of reconstructive surgery in ballistic and penetrating trauma are prime examples of this lack of clarity. Based on empirical insights, one of the leading concerns in earlier publications about decompressing a spinal canal with penetrating trauma is not a real issue anymore; cerebrospinal fluid leaks are not major concerns in the more recent literature. Advances in dural reconstruction techniques may be one cause, but the exact reason has not been studied yet.
Perhaps the evolving importance of databases and registries will help provide better insights toward guiding our specialty toward a more concise treatment algorithm.7 The large numbers of armed conflicts and violent crime around the world necessitate our increased attention to this acutely relevant topic.8
References
- 1.Bono C M, Heary R F. Gunshot wounds to the spine. Spine J. 2004;4(2):230–240. doi: 10.1016/S1529-9430(03)00178-5. [DOI] [PubMed] [Google Scholar]
- 2.Ben-Galim P, Reitman C A. Intrathecal migratory foreign body without neurological deficit after a gunshot wound. Spine J. 2008;8(2):404–407. doi: 10.1016/j.spinee.2006.10.025. [DOI] [PubMed] [Google Scholar]
- 3.Benzel E C, Hadden T A, Coleman J E. Civilian gunshot wounds to the spinal cord and cauda equina. Neurosurgery. 1987;20(2):281–285. doi: 10.1227/00006123-198702000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Waters R L, Adkins R H. The effects of removal of bullet fragments retained in the spinal canal. A collaborative study by the National Spinal Cord Injury Model Systems. Spine (Phila Pa 1976) 1991;16(8):934–939. doi: 10.1097/00007632-199108000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Waters R L, Sie I H. Spinal cord injuries from gunshot wounds to the spine. Clin Orthop Relat Res. 2003;(408):120–125. doi: 10.1097/00003086-200303000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Tanguy A, Chabannes J, Deubelle A, Vanneuville G, Dalens B. Intraspinal migration of a bullet with subsequent meningitis. A case report. J Bone Joint Surg Am. 1982;64(8):1244–1245. [PubMed] [Google Scholar]
- 7.Soges L J, Kinnebrew G H, Limcaco O G. Mobile intrathecal bullet causing delayed radicular symptoms. AJNR Am J Neuroradiol. 1988;9(3):610. [PMC free article] [PubMed] [Google Scholar]
References
- 1.Syre P III, Rodriguez-Cruz L, Desai R. et al. Civilian gunshot wounds to the atlantoaxial spine: a report of 10 cases treated using a multidisciplinary approach. J Neurosurg Spine. 2013;19(6):759–766. doi: 10.3171/2013.8.SPINE12907. [DOI] [PubMed] [Google Scholar]
- 2.Rabinowitz R P, Tabatabai A, Stein D M, Scalea T M. Infectious complications in GSW's through the gastrointestinal tract into the spine. Injury. 2012;43(7):1058–1060. doi: 10.1016/j.injury.2012.01.014. [DOI] [PubMed] [Google Scholar]
- 3.Mirovsky Y, Shalmon E, Blankstein A, Halperin N. Complete paraplegia following gunshot injury without direct trauma to the cord. Spine (Phila Pa 1976) 2005;30(21):2436–2438. doi: 10.1097/01.brs.0000184588.54710.61. [DOI] [PubMed] [Google Scholar]
- 4.Levy M L Gans W Wijesinghe H S SooHoo W E Adkins R H Stillerman C B Use of methylprednisolone as an adjunct in the management of patients with penetrating spinal cord injury: outcome analysis Neurosurgery 19963961141–1148., discussion 1148–1149 [DOI] [PubMed] [Google Scholar]
- 5.Rentfrow B, Vaidya R, Elia C, Sethi A. Lead toxicity and management of gunshot wounds in the lumbar spine. Eur Spine J. 2013;22(11):2353–2357. doi: 10.1007/s00586-013-2805-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dedini R D, Karacozoff A M, Shellock F G, Xu D, McClellan R T, Pekmezci M. MRI issues for ballistic objects: information obtained at 1.5-, 3- and 7-Tesla. Spine J. 2013;13(7):815–822. doi: 10.1016/j.spinee.2013.02.068. [DOI] [PubMed] [Google Scholar]
- 7.National Spinal Cord Injury Statistical Center Spinal Cord Injury (SCI) Facts and Figures at a Glance; August 2014 Available at: https://www.nscisc.uab.edu/PublicDocuments/fact_figures_docs/Facts%202014.pdf. Accessed July 15, 2015
- 8.Blair J A, Possley D R, Petfield J L, Schoenfeld A J, Lehman R A, Hsu J R. et al. Military penetrating spine injuries compared with blunt. Spine J. 2012;12(9):762–768. doi: 10.1016/j.spinee.2011.10.009. [DOI] [PubMed] [Google Scholar]


