Abstract
Study Design Systematic review.
Objective Determine whether closed suction wound drains decrease the incidence of postoperative complications compared with no drain use in patients undergoing spine surgery for lumbar degenerative conditions.
Methods Electronic databases and reference lists of key articles were searched up through January 22, 2015, to identify studies comparing the use of closed suction wound drains with no drains in spine surgery for lumbar degenerative conditions. Outcomes assessed included the cumulative incidence of epidural hematoma, superficial and deep wound infection, and postoperative blood transfusion. The overall strength of evidence across studies was based on precepts outlined by the Grades of Recommendation Assessment, Development and Evaluation Working Group.
Results Five heterogeneous studies, three randomized controlled trials, and two cohort studies form the evidence basis for this report. There was no difference in the incidence of hematoma, superficial wound infection, or deep infection in patients with compared with patients without closed suction wound drains after lumbar surgery. The upper bounds of the 95% confidence interval for hematoma ranged from 1.1 to 16.7%; for superficial infection, 1.0 to 7.3%; and for deep infection, 1.0 to 7.1%. One observational study reported a 3.5-fold increase in the risk of blood transfusion in patients with a drain. The overall strength of evidence for these findings is considered low or insufficient.
Conclusions Conclusions from this systematic review are limited by the quality of included studies that assessed the use of closed suction wound drains in lumbar spine surgeries for degenerative conditions. We believe that spine surgeons should not routinely rely on closed suction wound drains in lumbar spine surgery until a higher level of evidence becomes available to support its use.
Keywords: lumbar spine surgery, spinal drains, closed suction drains, wound drain, infection, hematoma, postoperative complications
Study Rationale and Context
Wound suction drains have been used to decrease the rate of postoperative hematoma formation and thus wound infections for many years throughout all surgical subspecialties. Although the use of surgical drains dates back to the years of Hippocrates,1 in the orthopedic literature these drains have not been shown to be beneficial in decreasing the rates of these complications, especially in orthopedic procedures including fracture fixation or arthroplasty surgeries.2 3 4 5 However, these drains are still commonly used throughout the orthopedic community, including spine surgery.
Debate in this area remains, as proponents of its use in the immediate postoperative period believe that it will prevent fluid collection in the surgical dead space and thus eliminate the media for bacterial growth. On the other hand, opponents believe that they are considered a foreign body that promotes inflammation and even sometimes provokes an infectious response.
In spine surgery, the controversy is even more profound because it decreases the rare but devastating complication of postoperative epidural hematoma, but it may have a hypothetical increase in the risk of infection.6 7 In the spine literature, the incidence of epidural hematoma in the postprocedural period ranges from 0.2 to 2.9%,8 9 10 and the incidence of postoperative wound infection is 0.7 to 16%,11 12 thus identifying a method that can decrease the incidence of these complications would be of great benefit.
To help address this debate, we conducted a systematic review of the use of these drains and extensively explored the efficacy and safety of closed suction wound drainage in spine surgery in the postoperative period.
Clinical Question
In patients undergoing spine surgery for lumbar degenerative conditions, does the use of closed suction wound drains decrease the incidence of postoperative complications compared with no drain use?
Materials and Methods
Study design: Systematic review.
Search: PubMed, Embase, the Cochrane Library, Web of Science, Scopus, and bibliographies of key articles
Dates searched: through January 22, 2015.
Inclusion criteria: (1) comparative studies in peer-reviewed journals; (2) adult patients undergoing spinal surgery for degenerative conditions in the lumbar spine receiving postoperative closed suction drains or no drains; (3) outcomes included at least one of the following: epidural hematoma, superficial wound infection, deep wound infection, or postoperative blood transfusion.
Exclusion criteria: (1) skeletally immature patients (<18 years of age); (2) surgery for intradural pathology, dural tears, tumor, trauma, fracture, or infection; (3) cervical or thoracic spine surgery; (4) nonclinical studies, case reports, and case series.
Outcomes: (1) epidural hematoma; (2) superficial wound infection; (3) deep wound infection; and (4) postoperative blood transfusion.
Analysis: Due to heterogeneity in patient populations (including differences in patient demographics, diagnoses, and surgical procedures) and differences in study design, a meta-analysis was not performed. We calculated the cumulative incidence by dividing the number of patients with an event by the number at risk for the event and the associated 95% confidence interval. When zero events were reported for an outcome, the confidence interval was found using the “rule of three” estimation.13
Details about the methods can be found in the online supplementary material.
Overall strength of evidence: The overall strength of evidence across studies was based on precepts outlined by the Grades of Recommendation Assessment, Development and Evaluation Working Group. Study critical appraisals and reasons for upgrading and downgrading for each outcome can be found in the online supplementary material.
Results
Three randomized controlled trials (RCTs) and two cohort studies met the inclusion criteria and form the basis for this report (Fig. 1). Their characteristics are described in Table 1. A list of studies excluded and the reason for exclusion can be found in the online supplementary material.
One RCT included patients undergoing multilevel decompression or fusion as a primary or reoperation procedure for herniated nucleus pulposus, spinal stenosis, degenerative spondylolisthesis, or postlaminectomy syndrome in an older population (mean age 67.4 years; Table 1).14 Two RCTs included patients undergoing single-level laminectomy for herniated disk or degenerative stenosis, though one study placed the drains in the epidural space (mean age 46.7 years),15 and the second placed the drain in the lumbodorsal fascia (mean age not reported).7
Two retrospective cohorts included patients undergoing single or multilevel laminoplasty, diskectomy, or fusion for varying diagnoses (mean age 46 to 57.3 years).16 17
Fig. 1.
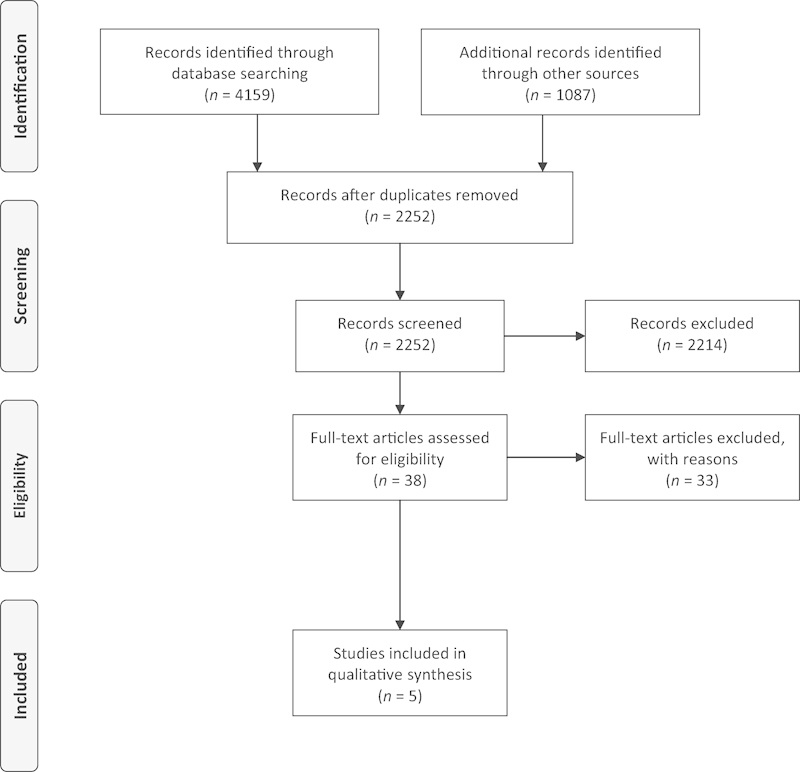
Flowchart showing results of literature search.
Table 1. Characteristics of included studies.
| First author (year) | Study type | Population | Treatment | Diagnosis | Surgery type |
|---|---|---|---|---|---|
| Payne (1996)7 | RCT |
n = 200 Age: NR % male: NR |
Drain (n = 103) No drain (n = 97) |
• Herniated disk (% NR) • Degenerative stenosis (% NR) |
• Singe-level hemilaminectomy (% NR) • Decompressive laminectomy (% NR) |
| Brown (2004)14 | RCT |
n = 83 Age: 67.4 y % male: NR |
Drain (n = 42) No drain (n = 41) |
• Herniated nucleus pulposus: n = 13 (16%) • Spinal stenosis: n = 73 (88%) • Degenerative spondylolisthesis: n = 40 (48%) • Postlaminectomy syndrome: n = 15 (18%) |
• Decompression (2–4 levels) Primary: n = 15 (35%) Reoperation: n = 12 (15%) • Fusion with instrumentation: n = 16 (19%) • Fusion without instrumentation: n = 30 (36%) |
| Mirzai (2006)15 | RCT |
n = 50 Age: 46.7 ± 7.6 y 58% male |
Drain (n = 22) No drain (n = 28) |
• Herniated disk: n = 50 (100%) | • Virgin single-level microdiskectomy with hemipartial laminectomy and flavectomy |
| Kanayama (2010)16 | Retro cohort |
n = 560 Age: 46 y 64.3% male |
Drain (n = 298) No drain (n = 262) |
NR | • Single-level laminoplasty (medial facetectomy) (% NR) • Diskectomy (% NR) |
| Walid (2012)17 | Retro cohort |
n = 402 Age: 57.3 ± 11.5 y 43% male |
Drain (n = 285) No drain (n = 117) |
• Spondylosis: n = 31 (8%) • Disk displacement: n = 145 (36%) • Disk degeneration: n = 84 (21%) • Disk disease with myelopathy: n = 23 (6%) • Lumbar spinal stenosis: n = 79 (20%) • Acquired spondylolisthesis: n = 29 (7%) • Spondylolisthesis: n = 11 (3%) |
• Lateral fusion: n = 301 (75%) • Posterior fusion: n = 101 (25%) |
Abbreviations: NR, not reported; RCT, randomized controlled trial.
Hematoma
The evidence base included three RCTs and two retrospective cohorts.
The method of identification of hematoma varied among studies. One small RCT reported 89% of the patients with drains and 36% of the patients without drains had epidural hematomas as detected by magnetic resonance imaging. Most were minimal in size with only 7% prominent in the no-drain group compared with 0% prominent in the drain group.15 All other studies assessed hematomas that required drainage or reoperation. The risk in these studies ranged from 0.0 to 0.7%.7 14 16 17
There was no difference in risk for hematoma comparing drains with no drains across studies of different design, surgeries of varying complexity, patients of different ages, or complexity of diagnosis.7 14 15 16 17 The upper 95% confident limit of risk for hematoma in the patients with drains was 13.6% compared with 16.7% for the patients without drains (Table 2).
Table 2. Hematoma, superficial wound infection, deep infection, and postoperative blood transfusion among patients receiving closed wound drains compared with those who do not receive closed wound drains following lumbar surgery.
| First author (year) | Treatment | Hematoma | Superficial wound infection | Deep infection | Postoperative blood transfusion | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | n | % (95% CI) | ||
| Payne (1996)7 | Drain (n = 103) No drain (n = 97) |
0a
0a |
0.0 (0.0–2.9) 0.0 (0.0–3.1) |
2 1 |
1.9 (0.0–4.6) 1.0 (0.0–3.0) |
NR | NR | NR | NR |
| Brown (2004)14 | Drain (n = 42) No drain (n = 41) |
0 0 |
0.0 (0.0–7.1) 0.0 (0.0–7.3) |
0 0 |
0.0 (0.0–7.1) 0.0 (0.0–7.3) |
0/42 0/41 |
0.0 (0.0–7.1) 0.0 (0.0–7.3) |
NR | NR |
| Mirzai (2006)15 | Drain (n = 22) No drain (n = 28) |
0b
2b |
0.0 (0.0–13.6) 7.1 (0.0–16.7) |
NR | NR | NR | NR | NR | NR |
| Kanayama (2010)16 | Drain (n = 298) No drain (n = 262) |
2c
0c |
0.7 (0.0–1.6) 0.0 (0.0–1.1) |
0 0 |
0.0 (0.0–1.0) 0.0 (0.0–1.1) |
0 0 |
0.0 (0.0–1.0) 0.0 (0.0–1.1) |
NR | NR |
| Walid (2012)17 | Drain (n = 285) No drain (n = 117) |
0d
0d |
0.0 (0.0–1.1) 0.0 (0.0–2.6) |
10 3 |
3.5 (1.4–5.7) 2.6 (0.0–5.4) |
NR | NR | 68 8 |
23.9 (18.9–28.8) 6.8 (2.3–11.4) |
Abbreviations: CI, confidence interval; FU, follow-up; NR, not reported.
Reported as hematoma requiring drainage.
“Prominent” hematoma detected with magnetic resonance imaging. Minimal hematoma was found in 31.8% of patients with drains versus 60.7% without drains, and moderate in 4.5% patients with drains versus 21.4% without drains.
Reported as epidural hematoma causing neurologic compromise requiring surgical evacuation.
Reported as hematoma requiring reoperation.
Superficial Wound Infection
The evidence base included two RCTs and two retrospective cohorts.
There was no difference in risk between the patients receiving closed suction wound drains (range of risks, 0.0 to 3.5%) compared with the patients with no drains (range of risks, 0.0 to 2.6%; Table 2).7 14 16 17 The upper 95% confident limit of risk for superficial wound infection in the patients with drains was 7.1% and for the patients without drains was 7.3%.
Deep Infection
The evidence base included one RCT and one retrospective cohort.
There are no events recorded in the two studies that report risk for deep infection in the patients treated with versus patients treated without closed suction wound drains after lumbar surgery (Table 2).14 16 The upper limit of risk for deep infection in the patients with drains was 7.1% and in the patients without drains was 7.3%.
Postoperative Blood Transfusion
The evidence base included one retrospective cohort.
One observation study reported a greater risk of blood transfusion after lumbar surgery in the patients with drains (24%) versus patients without drains (7%; risk ratio 3.5; 95% confidence interval 1.7 to 7.0).17
Evidence Summary
There was no difference in the incidence of hematoma, superficial wound infection, or deep infection in the patients with versus patients without closed suction wound drains after lumbar surgery. The overall strength of evidence for these findings is considered low or insufficient (Table 3). There is insufficient evidence to draw conclusions on the effect of closed suction wound drains on the risk for postoperative blood transfusion.
Table 3. Evidence summary: Do closed suction wound drains decrease the incidence of postoperative complications?
| Outcome | Overall quality of evidence | Studies | Effect size |
|---|---|---|---|
| Range of upper bound of 95% confidence intervala | |||
| Hematoma | Low due to risk of bias and imprecision | 3 RCTs (n = 333) | Drain: 2.9–13.6% No drain: 3.1–16.7% |
| 2 retro cohorts (n = 962) | Drain: 1.1–1.6% No drain: 1.1–2.6% |
||
| Superficial wound infection | Insufficient due to risk of bias and imprecision | 2 RCTs (n = 283) | Drain: 4.6–7.1% No drain: 3.0–7.3% |
| 2 retro cohorts (n = 962) | Drain: 1.0–5.7% No drain: 1.1–5.4% |
||
| Deep infection | Insufficient due to risk of bias and imprecision | 1 RCT (n = 83) | Drain: 7.1% No drain: 7.3% |
| 1 retro cohort (n = 560) | Drain: 1.0% No drain: 1.1% |
||
| Postoperative blood transfusion | Insufficient due to risk of bias | 1 retro cohort (n = 402) | Drain: 28.8% No drain: 11.4% RR: 3.5 (1.7, 7.0) |
Abbreviations: RCT, randomized controlled trial; retro, retrospective cohort; RR, risk ratio.
Calculated using Hanley's rule of three when zero events are reported for a given outcome.
Clinical Guidelines
No clinical guidelines were found.
Discussion
In the setting of spinal surgery, one of the biggest concerns is an epidural hematoma; some spine surgeons use drains to decrease the incidence of postoperative hematomas and subsequently neurologic complications. However, there is no clear consensus whether is it beneficial by decreasing hematomas or harmful by increasing the risk of infection and the rate of blood transfusion.
Five studies assessing the use of closed suction wound drains in spine surgeries for lumbar degenerative conditions were identified and included in this systematic review.
One strength of our study was the thorough and systematic search of the evidence performed. The limitations included the following: the methodologies of studies included in this review were heterogeneous, and all studies had small sample sizes. There was a lack of random sequence generation or allocation concealment in the RCTs. In addition, there was a lack of observer blinding and lack of controlling for confounding factors. (See Table 3 in the online supplementary material.)
Contrary to previous beliefs, there is no difference in the incidence of hematoma, superficial wound infection, or deep infection in the patients with versus patients without closed suction wound drains after lumbar surgery.
As this systematic review was of low or insufficient evidence, more randomized trials of the use of closed suction wound drains in lumbar spine surgery are needed with sufficient sample sizes and appropriate methodology protocols to adequately assess the effect of drain use on these rare outcomes.
Conclusions
Conclusions from this systematic review are limited by the quality of included studies that assessed the use of closed suction wound drains in lumbar spine surgeries for degenerative conditions. The small sample sizes, lack of random sequence generation, or allocation concealment in RCTs and lack of controlling for confounding factors may not have allowed us to detect differences between treatment groups, particularly for rare outcomes. We believe that spine surgeons should not routinely rely on the use of closed suction wound drains in lumbar spine surgery until a higher level of evidence becomes available to support its use.
Acknowledgments
Analytic support for this work was provided by Spectrum Research, Inc. with funding from AOSpine.
Footnotes
Disclosures Feras Waly, none Mohammad Alzahrani, none Fahad H. Abduljabbar, none Tara Landry, none Jean Ouellet, none Kathryn Moran, none Joseph R. Dettori, none
Editorial Perspective
Surgical practice is the invasive treatment of human ailments through the application of skill and technology drawn from a combination of experiential and of learned behaviors. The placement of drains in elective posterior spine surgery is one of these time-honored learned behaviors. Use of postoperative drains is a big deal from the medical and business side of medicine as their use may influence the occurrence of certain complications and may also be a factor on length of stay and other direct expenses such as material costs and use of antibiotics as well as personnel costs. In this era of questioning everything, the use of drains should not be considered as a given but should be subjected to a rigorous review of the evidence base. Waly and coauthors received universal praise from the reviewers for their choice of the subject of the evidence-based foundation of the use of drains by performing a formal systematic review.
The purported benefits of postoperative drainage are clear: a hopefully decreased infection rate and wound-healing disruption through the removal of postoperative fluid accumulation from the wound cavity and a decreased rate of epidural hematoma formation with the added risk of potential secondary neurologic deterioration. Using an extensive search strategy going all the way back to antiquity for this meritorious topic, the authors came up with two surprising results: (1) there is no evidence whatsoever to use posterior wound drains in the spine for either infection or hematoma; (2) there are remarkably few studies of higher quality that have actually examined the merits of postoperative wound drainage in spine surgery. Certainly, the evidence base for postoperative wound drainage is inverse to the commonality with which wound drainage is performed.
In reviewing these studies, the fact that there were no greater differences identified is not entirely surprising. The overall number of patients in the three prospective RCTs was 333. The two retrospective cohort studies combined for 962 patients, which leaves us with a patient cohort of ∼1,300 patients as a basis for the investigation of the merits of postoperative drain use in spine surgery. For sporadic occurrences like symptomatic epidural hematomas and their reported incidence of less than 1%, this number of subjects is simply too small to be able to hope to detect any differences. Especially when “simple surgeries” such as primary microdiskectomies in low-risk patients are part of the patient cohort, the expected rate of symptomatic postoperative complications could be expected to be sporadic at best. The cohort size is insufficient even for the far more common postoperative complication of wound infections, with a reported incidence of up to 7.1%. The pool of patients includes a mixture with instrumentation and no hardware used with variable degrees of invasiveness and unclear handling of important comorbidities such as diabetes, body habitus, immune or nutritional compromise, blood thinners, and cerebrospinal fluid leak, which simply does not allow for a meaningful assessment of the influence of drains on the desired outcome of reducing infections. Other important variables, such as duration of drain placement and use of perioperative antibiotics as well as type of wound closure and incision management, are also not factored into this evaluation.
In conclusion, the best we can say for now is that the use of drains does not seem to prevent an increase of postoperative wound infections. On the contrary, the claim that postoperative wound drainage would actually reduce this dreaded complication can certainly not be maintained. Given the number of variables at hand and the differences in practices and patient comorbidities, the question arises if a prospective RCT or a retrospective study format can actually ever be sufficient to actually pick up important differences in complication rates such as symptomatic epidural hematoma or wound infections. A much larger patient base, such as found in a registry, may turn out to be a preferred study format to try to better investigate this topic. Until then, the editors of the Evidence-Based Spine-Care Journal edition of the Global Spine Journal invite the commentaries of its readers around the world on their recommendations on postoperative drain use and also what pathway to use to arrive at a best practices consensus.
Supplementary Material
References
- 1. Hippocrates The Genuine Works of Hippocrates Baltimore, MD: Williams & Wilkins; 1939 [Google Scholar]
- 2.Joshy S, Tharian B. Wound drainage versus non-drainage for proximal femoral fractures. A prospective randomised study. Injury. 2006;37(1):85. doi: 10.1016/j.injury.2005.06.058. [DOI] [PubMed] [Google Scholar]
- 3.Lang G J, Richardson M, Bosse M J. et al. Efficacy of surgical wound drainage in orthopaedic trauma patients: a randomized prospective trial. J Orthop Trauma. 1998;12(5):348–350. doi: 10.1097/00005131-199806000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Parker M J, Roberts C P, Hay D. Closed suction drainage for hip and knee arthroplasty. A meta-analysis. J Bone Joint Surg Am. 2004;86-A(6):1146–1152. doi: 10.2106/00004623-200406000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Ritter M A, Keating E M, Faris P M. Closed wound drainage in total hip or total knee replacement. A prospective, randomized study. J Bone Joint Surg Am. 1994;76(1):35–38. doi: 10.2106/00004623-199401000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Parker M J, Livingstone V, Clifton R, McKee A. Closed suction surgical wound drainage after orthopaedic surgery. Cochrane Database Syst Rev. 2007;(3):CD001825. doi: 10.1002/14651858.CD001825.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Payne D H, Fischgrund J S, Herkowitz H N, Barry R L, Kurz L T, Montgomery D M. Efficacy of closed wound suction drainage after single-level lumbar laminectomy. J Spinal Disord. 1996;9(5):401–403. [PubMed] [Google Scholar]
- 8.Awad J N, Kebaish K M, Donigan J, Cohen D B, Kostuik J P. Analysis of the risk factors for the development of post-operative spinal epidural haematoma. J Bone Joint Surg Br. 2005;87(9):1248–1252. doi: 10.1302/0301-620X.87B9.16518. [DOI] [PubMed] [Google Scholar]
- 9.Kou J, Fischgrund J, Biddinger A, Herkowitz H. Risk factors for spinal epidural hematoma after spinal surgery. Spine (Phila Pa 1976) 2002;27(15):1670–1673. doi: 10.1097/00007632-200208010-00016. [DOI] [PubMed] [Google Scholar]
- 10.Scuderi G J, Brusovanik G V, Fitzhenry L N, Vaccaro A R. Is wound drainage necessary after lumbar spinal fusion surgery? Med Sci Monit. 2005;11(2):CR64–CR66. [PubMed] [Google Scholar]
- 11.O'Toole J E, Eichholz K M, Fessler R G. Surgical site infection rates after minimally invasive spinal surgery. J Neurosurg Spine. 2009;11(4):471–476. doi: 10.3171/2009.5.SPINE08633. [DOI] [PubMed] [Google Scholar]
- 12.Schimmel J J, Horsting P P, de Kleuver M, Wonders G, van Limbeek J. Risk factors for deep surgical site infections after spinal fusion. Eur Spine J. 2010;19(10):1711–1719. doi: 10.1007/s00586-010-1421-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eypasch E, Lefering R, Kum C K, Troidl H. Probability of adverse events that have not yet occurred: a statistical reminder. BMJ. 1995;311(7005):619–620. doi: 10.1136/bmj.311.7005.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brown M D, Brookfield K F. A randomized study of closed wound suction drainage for extensive lumbar spine surgery. Spine (Phila Pa 1976) 2004;29(10):1066–1068. doi: 10.1097/00007632-200405150-00003. [DOI] [PubMed] [Google Scholar]
- 15.Mirzai H, Eminoglu M, Orguc S. Are drains useful for lumbar disc surgery? A prospective, randomized clinical study. J Spinal Disord Tech. 2006;19(3):171–177. doi: 10.1097/01.bsd.0000190560.20872.a7. [DOI] [PubMed] [Google Scholar]
- 16.Kanayama M, Oha F, Togawa D, Shigenobu K, Hashimoto T. Is closed-suction drainage necessary for single-level lumbar decompression? Review of 560 cases. Clin Orthop Relat Res. 2010;468(10):2690–2694. doi: 10.1007/s11999-010-1235-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walid M S, Abbara M, Tolaymat A. et al. The role of drains in lumbar spine fusion. World Neurosurg. 2012;77(3–4):564–568. doi: 10.1016/j.wneu.2011.05.058. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


