Abstract
Study Design Case report.
Objectives Symptomatic triple-region spinal stenosis (TRSS), defined as spinal stenosis in three different regions of the spine, is extremely rare. To our knowledge, treatment with simultaneous decompressive surgery is not described in the literature. We report a case of a patient with TRSS who was treated successfully with simultaneous decompressive surgery in three separate regions of the spine.
Methods A 50-year-old man presented with combined progressive cervical and thoracic myelopathy along with severe lumbar spinal claudication and radiculopathy. He underwent simultaneous decompressive surgery in all three regions of his spine and concomitant instrumented fusion in the cervical and thoracic regions.
Results Estimated blood loss for the procedure was 600 mL total (250 mL cervical, 250 mL thoracic, 100 mL lumbar) and operative time was ∼3.5 hours. No changes were noted on intraoperative monitoring. The postoperative course was uncomplicated. The patient was discharged to inpatient rehabilitation on postoperative day (POD) 7 and discharged home on POD 11. At 6-month follow-up, his gait and motor function was improved and returned to normal in all extremities. He remains partially disabled due to chronic back pain.
Conclusions This report is the first of symptomatic TRSS treated with simultaneous surgery in three different regions of the spine. Simultaneous triple region stenosis surgery appears to be an effective treatment option for this rare condition, but may be associated with prolonged hospital stay after surgery.
Keywords: tandem stenosis, tandem spine, decompression surgery, triple region, cervical, thoracic, lumbar, simultaneous, single-stage
Introduction
Spinal stenosis is a narrowing of the neural canal and foramina, resulting in the compression of the neurologic structures with resultant symptoms. The first description may have very well been by Portal of France in 1803, and details have been popularized by Verbiest and classified by Arnoldi et al based on the pathology of the stenosis.1 2 3 4 In 1957, Brain and Wilkinson described stenosis in both the cervical and lumbar regions, a condition that would later be termed tandem spinal stenosis (TSS) by Dagi et al.5 6 Teng and Papatheodorou in 1964 further expanded on the topic, observing significant spinal stenosis occurring in both the cervical and lumbar regions of the spine.7 Patients typically present with both upper and lower motor neuron dysfunction, including progressive gait disturbance and neurologic claudication. Spinal decompression procedures for isolated spinal stenosis are common in the adult population with relatively good outcomes noted in the literature.8 9 However, there is limited literature addressing the surgical management of symptomatic spinal stenosis in multiple regions of the spine. In particular, triple-region spinal stenosis (TRSS), or stenosis in the cervical, thoracic, and lumbar spine, is not well described.
To date, 15 articles were identified on the topic of TSS. The prevalence of this condition as well as the optimal surgical management are not clear. The available literature demonstrates a wide variation in the prevalence, ranging from 0.9% to 25%.10 11 12 13 14 15 16 Due to the potential risk and morbidity of simultaneous surgery, four available publications recommended a staged decompression approach for TSS.6 10 11 16 The purpose of this study is to review the available literature and to present a unique case of TRSS treated with simultaneous tandem decompression surgery.
Case Report
Clinical Presentation
A 50-year-old male commercial truck and bus driver had a history of a work-related ground-level fall 10 years prior to presentation complicated by chronic back pain. Upon clinic presentation, he reported a 2-month history of progressive gait instability, worsening leg weakness, difficulty walking, numbness in both of his forearms, numbness in his left C7 dermatome, difficulty picking up objects, and pain in his lumbar, thoracic, and lower cervical spine. He denied any specific inciting event related to his recent worsening gait instability. His examination was remarkable for unsteady gait, inability to stand on a single leg, limited lumbar flexion and extension, global weakness in multiple upper and lower extremity muscle groups, numbness in the upper and lower extremity regions, and a positive Hoffman sign in the left hand.
Neuroradiology
Magnetic resonance imaging of the cervical, thoracic, and lumbar spine revealed severe C5–T1 stenosis, severe T9–T11 stenosis, and severe L4–L5 stenosis (Figs. 1, 2, and 3). Computed tomography was obtained for preoperative planning.
Fig. 1.
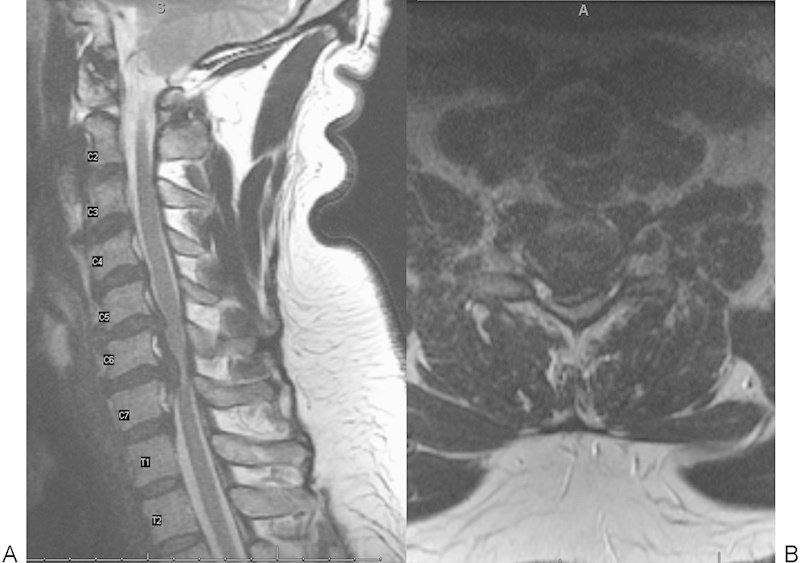
(A) Sagittal and (B) axial magnetic resonance imaging showing severe cervical stenosis.
Fig. 2.
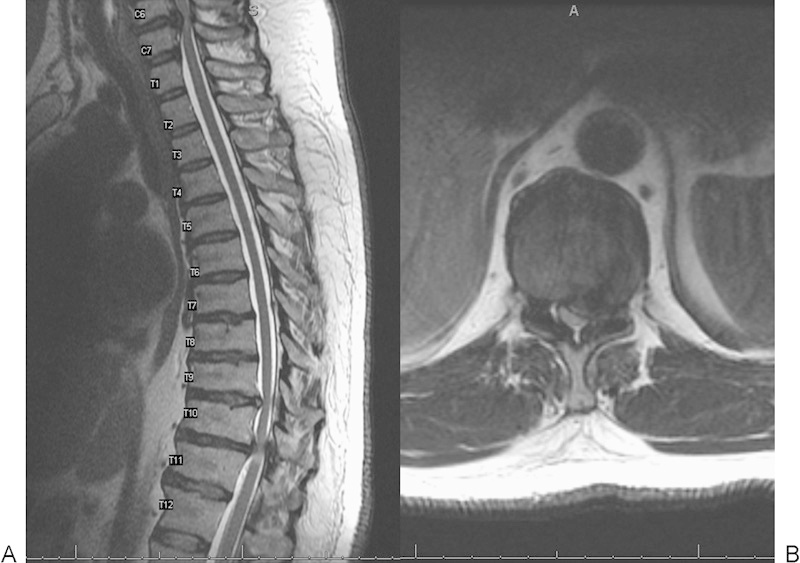
(A) Sagittal and (B) axial magnetic resonance imaging showing severe thoracic stenosis.
Fig. 3.
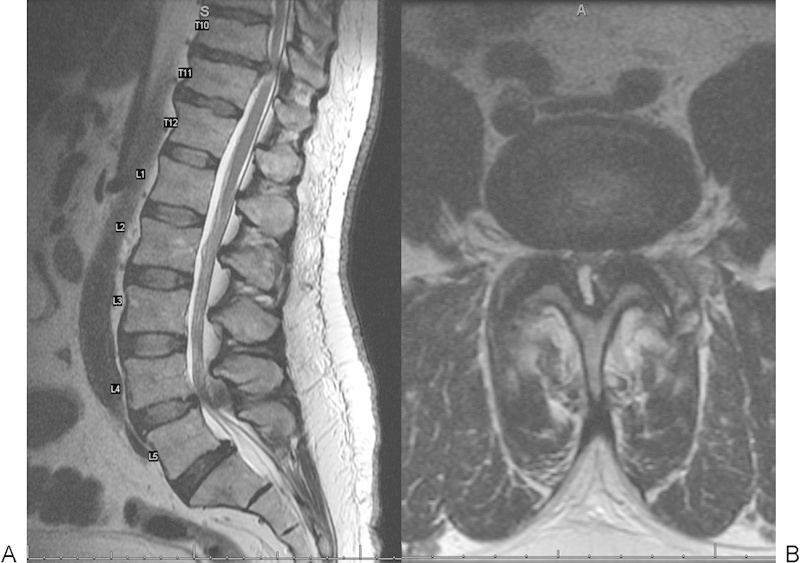
(A) Sagittal and (B) axial magnetic resonance imaging showing severe lumbar stenosis.
Surgical Management and Postoperative Course
The patient was diagnosed with progressive myelopathy and severe lumbar spinal stenosis with evidence of symptomatology from all three spinal regions. Due to his history of progressive and worsening symptoms, he was found to be an appropriate surgical candidate, and surgical intervention was offered. Prior to the surgery, the patient underwent presurgical cardiac risk stratification by the cardiology team for left heart strain found on electrocardiogram. The patient had a history of long-standing hypertension and severe left ventricular hypertrophy and was found to be low risk for any cardiac event in the perioperative period.
He was taken to the operating room for triple-level tandem surgery. Somatosensory evoked potential and motor evoked potential monitoring was used throughout the entire operation. A Mayfield tong head-holding device was applied, and the spine was prepped and draped from the occiput to the sacrum. Via three separate incisions, the following procedures were performed:
Posterior cervical C5–C7 laminectomy and C4–T1 instrumented posterolateral fusion using local autogenous bone graft and multilevel cervical polyaxial lateral mass screws, T1 pedicle screws, 3.5-mm rods, and one crosslink
T9–T11 laminectomy and decompression of the spinal cord and T8–T12 posterior instrumented fusion using local autogenous bone graft and left-sided T8–T12 unilateral instrumentation consisting of titanium pedicle screws and a unilateral rod
L4–L5 bilateral lumbar decompression (partial laminectomy, partial facetectomy, and bilateral foraminotomy)
The surgery was performed in succession by a single attending surgeon and surgical assistant with closure then performed simultaneously (Figs. 4 and 5). At each level, a fenestrated active drain device was placed prophylactically and sewn into the skin. Closure was achieved with absorbable polyglactin sutures for the fascia and subcutaneous tissues and staples for the skin. The patient tolerated the procedure well with no changes noted on somatosensory evoked potentials or motor evoked potential monitoring. The estimated blood loss (EBL) for the procedure was 600 mL total (250 mL cervical, 250 mL thoracic, 100 mL lumbar). The total operative time was ∼3.5 hours.
Fig. 4.

Intraoperative photograph demonstrating simultaneous operative procedure.
Fig. 5.
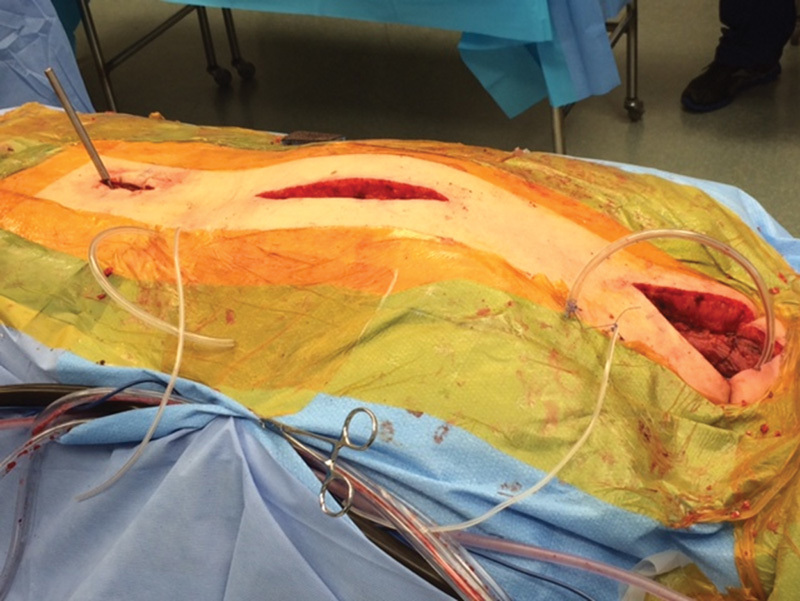
Intraoperative photograph demonstrating simultaneous limited surgical wounds in three separate regions of the spine.
The patient's postoperative course was without complication. He was discharged to inpatient rehabilitation on postoperative day 7 and discharged home on postoperative day 11. At 6-month follow-up, radiographs revealed that the alignment was maintained (Figs. 6, 7, and 8), gait was markedly improved, and motor function returned to normal in both upper and lower extremities. He remains partially disabled due to his chronic back pain.
Fig. 6.
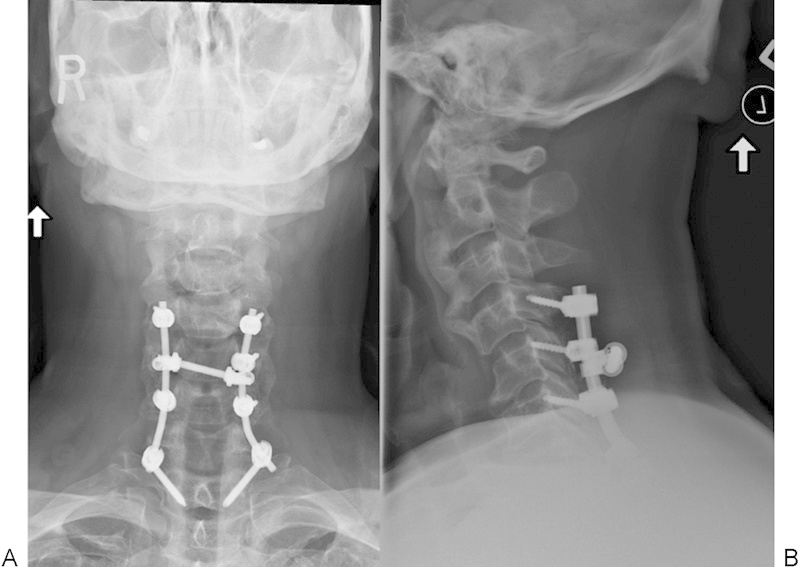
(A) Anteroposterior and (B) lateral cervical spine radiographs at postoperative 6 months.
Fig. 7.
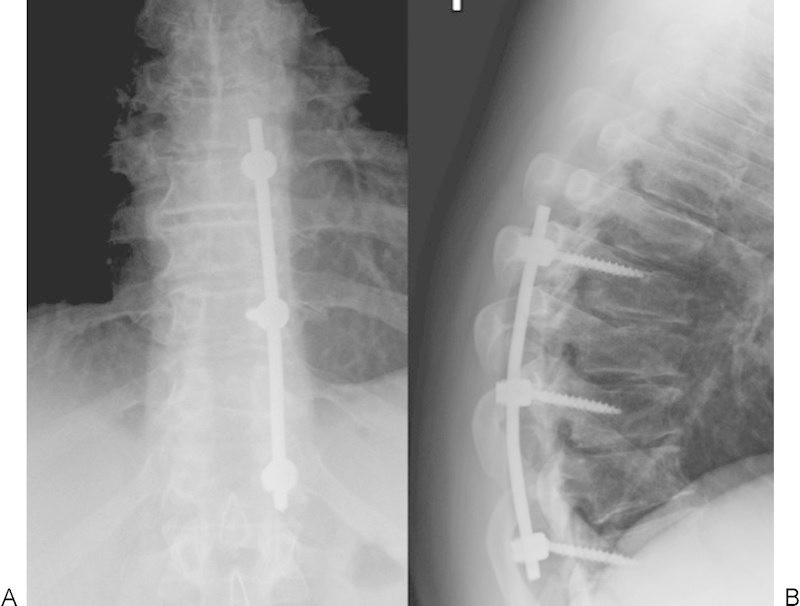
(A) Anteroposterior and (B) lateral thoracic spine radiographs at postoperative 6 months.
Fig. 8.
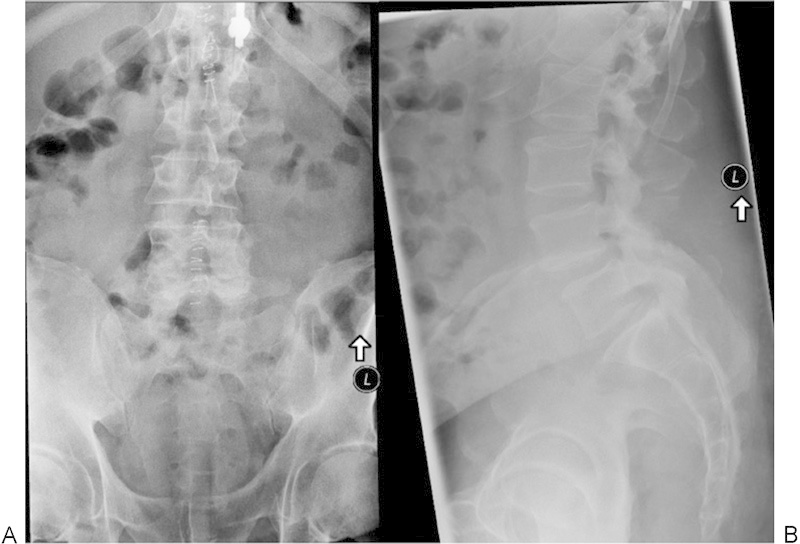
(A) Anteroposterior and (B) lateral lumbar spine radiographs at postoperative 2 weeks.
Discussion
The Medline database was searched using the key words “tandem stenosis,” “tandem spine,” “triple region,” and “cervical, thoracic, and lumbar stenosis.” No publications involving TRSS were identified. A total of 15 articles were identified as having been published on the topic of treatment of tandem stenosis. Several of the articles did not include patients who were treated surgically; only 10 of the 15 published articles included patients who underwent surgical management for TSS. Five publications included patients who were treated with a staged surgical approach, and six publications included small numbers of patients who had a one-staged or simultaneous surgical approach. All of the published studies were either commentaries or retrospective reviews containing small numbers of patients with multiple surgeons.
Authors have previously described degenerative spine conditions that may confuse clinical presentations by having symptoms from two different spine regions. LaBan and Green suggested that when there is a combination of symptomatic spinal stenosis from different regions, the surgical decision-making process can be confusing.12 The authors suggested that symptoms of one region usually predominate, and only after one is treated does the second become more evident.
Since TSS was first described, estimates of its frequency have varied widely, ranging from as low as 0.9% to as high as 28%.10 11 12 13 Several studies have attempted to accurately define the incidence of TSS.12 14 15 17 Lee et al examined cervical and lumbar cadaveric specimens of 440 skeletally mature spines and found the prevalence of tandem stenosis between 0.9% and 5.4%. The authors defined spinal stenosis as an absolute midsagittal canal diameter less than 12 mm present in at least one spinal level.17 LaBan and Green performed a 10-year retrospective review of 460,964 hospital admissions at a large community teaching hospital to identify the frequency of TSS.12 The authors identified a base population of only 54 patients with TSS, with a frequency rate for all ages of 12 per 100,000 admissions. Ninety-four percent of the patients identified were over the age of 51. More recently, in a cadaveric study of 1,072 adult skeletons, Bajwa et al attempted to determine whether tandem stenosis is related to congenital narrowing in specific regions of the spine.14 15 The authors reported the incidence of tandem cervical and lumbar stenosis to be 2%, with tandem cervical and thoracic stenosis at only 1%. In general, the best estimates of the incidence of tandem stenosis in the general population appear to be ∼1 to 2%, and symptomatic tandem stenosis is much less. Within certain patient populations, however, specifically patients with symptomatic stenosis in one region, the prevalence of tandem stenosis can be higher.10 11 12 16
Few studies in the literature address the surgical management of TSS, with only 10 being identified at the time of this manuscript writing.6 10 11 16 18 19 20 21 22 23 Each of these studies consists of small numbers of patients and are of a retrospective nature. Our report is unique as it describes a safe and simultaneous surgery for all three regions of the stenosis.
With regards to these studies, most authors recommend a staged approach for patients with TSS requiring surgery. Dagi et al performed a retrospective review of 19 patients with TSS with a mean follow-up of 22 months. The authors recommended decompression of both the cervical and lumbar regions, but suggested the more symptomatic level be performed first.6 An excellent outcome was seen in 5 patients (26%), 4 improved (21%), 5 deteriorated despite initial improvement (26%), and 1 was unchanged. There was 1 postoperative death and 3 patients could not be found for follow-up. The postoperative improvement correlated inversely with symptom duration, and the authors stressed the importance of an early diagnosis and timely surgical intervention.
Hsieh et al reported an overall incidence of 7.6% of TSS in a series of 158 patients who had surgery for degenerative spinal stenosis.16 The authors' surgical preference in the treatment of these 12 patients diagnosed with TSS required that cervical surgery be addressed first if signs of upper motor neuron or upper extremity symptoms were predominant. For patients with predominant lower extremity symptoms but no upper motor neuron exam findings, lumbar surgery was performed first. In this series, the majority (67%) of the patients received cervical surgery first. The average follow-up was 32 months, and good or excellent clinical outcomes were demonstrated in 67% of patients. In 7 of the 12 patients with TSS, ossification of the posterior longitudinal ligament (OPLL) was noted (58%), which the authors felt might be a predominant factor found in TSS.
Epstein et al felt that the correct order for operative treatment in TSS depended on the severity of myelopathy and radiculopathy.11 Patients requiring cervical surgery first had stenosis with a cervical spinal canal of 10 mm or less in anteroposterior diameter. Patients requiring lumbar surgery first had a lumbar spinal canal between 11 and 13 mm in diameter and first presented with symptomatic lumbar radiculopathy, with a significant portion (50%) having intermittent neurogenic claudication. In this series, cervical decompression often improved lumbar symptoms with the resolution of pain, spasticity, and sensory deficits of myelopathic origin. Latent findings of severe claudication due to lumbar spinal stenosis were not relieved by cervical decompression and increased in severity. Significant improvement was shown in 90% of the patients in this series, with latent severe lumbar symptoms treated with staged multilevel lumbar decompressive surgery.
Aydogan et al also performed a retrospective study on TSS between 1998 and 2004.10 Eight adult patients were diagnosed with TSS in a series of 230 patients who underwent surgery for spinal stenosis for an overall incidence of 3.4%. Three patients first received cervical surgery and five patients first received lumbar surgery based on main symptomatology and physical exam findings. The Japanese Orthopaedic Association (JOA) scores of all patients improved from an average of 8.1 preoperatively to an average of 12.7 points at final follow-up with a mean follow-up of 35 months. The Oswestry Disability Index (ODI) scores improved from a mean of 58.1 to 19.3, and all patients had good or excellent results without neurologic deterioration. Similar to other authors, the researchers felt that the order of decompression surgery should be based on the clinical symptoms and exam findings. All surgeries were staged, with the second surgery performed between 2 weeks to 2 months after the first surgery in an attempt to avoid higher complication rates.
Simultaneous surgery for TSS has not been addressed extensively in the literature, with only six published studies identified.18 19 20 21 22 23 Limits of these studies include the small numbers of patients and the retrospective nature of a relatively uncommon condition.
In their case report, Naderi and Mertol described two patients with symptomatic TSS in which simultaneous decompressive surgery was performed.22 The total surgical time for these patients was 130 and 150 minutes, and the authors reported neurologic and gait improvement postoperatively. No outcome measures were utilized in this case report, but the authors recommended simultaneous surgery as an alternative approach for patients with symptomatic TSS.
Kikuike et al performed a retrospective review of elderly patients (average age 71 years) with TSS who received single-stage combined cervical and lumbar decompression with average follow-up of 5 years.20 The authors utilized clinical outcomes with JOA-B and JOA-C scores and activities of daily life prior to surgery, 6 months postoperatively, and at final follow-up. The JOA-B and JOA-C scores and activities of daily life improved significantly 6 months after surgery, but ultimately deteriorated with additional follow-up in 7 patients (41%). Complications involving other parts of the body significantly influenced clinical deterioration at final follow-up, including lower extremity fractures, knee osteoarthritis, malignant tumor diagnosis, and cerebral infarction. Twelve patients (70%) were satisfied with their surgical outcome at the final follow-up. The authors felt that reasons other than the spinal pathology affected symptom deterioration at final follow-up, and that single-stage combined cervical and lumbar decompression surgery was safe for elderly patients.
In 2011, Eskander et al published a retrospective study on the outcomes after simultaneous decompression of the cervical and lumbar spine versus staged operations in 43 patients.19 Twenty-one patients, or nearly half (49%), underwent simultaneous decompression of both the cervical and lumbar spine, and 22 patients (51%) underwent staged decompression of the cervical spine followed by decompression of the lumbar spine at a later date. Both groups improved in JOA and ODI scores. There was no significant difference between the groups in regards to major or minor complications and JOA and ODI scores at 7-year follow-up. Several factors increased the risk of minor complications, including age above 68 years, EBL 400 mL or more, and operative time 150 minutes or more. The authors concluded that TSS can be managed by either surgical intervention or simultaneous or staged decompression, but that patient age, blood loss, and operative time should be considered when planning surgical strategies to help minimize postoperative complications.
Chen et al reported a retrospective series of 15 patients found to have combined cervical and thoracic OPLL or ossification of the ligament flavum, in which the authors termed “tandem ossification.” The patients were treated with a single-stage combined decompression of the cervical and thoracic spine.18 The authors reported significant overall improvements in JOA score and Nurick classification at minimum follow-up of 2 years, but noted that satisfaction was tied to perioperative complications and disease progression. The authors stressed preoperative communication with patients and realistic postoperative goals.
Krishnan et al reported a retrospective series of 53 patients undergoing single-stage decompression for TSS, the largest series yet reported.21 The authors noted improvement in modified JOA and ODI scores. They found that operating room time of <150 minutes and EBL <400 mL lessened complications and improved scores. They stressed patient selection, noting significant improvement in ODI and Nurick grade in the group younger than 60 years. The authors recommended single-stage surgery in this younger group, but staged surgery in patients over 60 years of age.
Hong and Liu described a case of multiregional spinal stenosis involving OPLL in a 36-year-old man in which one-stage cervical and thoracic decompression and fusion surgery was performed.23 The patient did well initially with upper cervical laminectomy and instrumented fusion, lower cervical laminoplasty, and upper thoracic laminectomy and instrumented fusion. However, 10 months postoperatively, severe tandem mid- and lower thoracic stenosis due to OPLL required further surgical intervention. The postoperative course was complicated by epidural hematoma and paraplegia that required additional surgery with some eventual return of neurologic function at 3.5-year follow-up. The authors stressed the importance of reducing kyphosis, performing an adequate decompression, and using increased implant density to prevent kyphosis and further spinal cord injury.
Conclusions
We have reported a patient with symptomatic stenosis in three separate regions of the spine. Only the cervical region had radiographic evidence of OPLL. The thoracic and lumbar regions demonstrated stenosis due to the typical degenerative cascade involving disk degeneration with bulging and facet and ligamentum flavum hypertrophy. We demonstrate that simultaneous surgery for TRSS appears to be an effective treatment option but may be associated with prolonged hospital stay after the surgery.
There is a paucity of literature describing TSS and successful management. To our knowledge, this report is the first of symptomatic TRSS treated with simultaneous surgery in three different regions of the spine.
Footnotes
Disclosures Joseph C. Schaffer, none Brandon L. Raudenbush, none Christine Molinari, none Robert W. Molinari, none
Editorial Perspective
This case report was selected by Evidence-Based Spine-Care Journal (EBSJ)–Global Spine Journal (GSJ) due to the clinical concerns raised in Dr. Cheung's discussion: the difficulty in making a clinical diagnosis of symptomatic spinal stenosis in the setting of concurrent upper and lower motor neuron compression. Most surgeons would agree that most patients who have complaints of diffuse back pain probably suffer from a somatization disorder. Similarly, nonfocal upper and lower extremity complaints as presented in this case report may lead to a deferral of neuroimaging investigation and be managed by prolonged rehabilitative care and even exploration of psychological confounders. In our era of increasing use of algorithm-driven medicine, simple findings—such as back pain with clear radicular symptoms—will be managed with a carefully choreographed sequence of diagnostic and management steps. Patients with complex multifocal spine disease like the case presented by Dr. Schaffer and colleagues clearly challenge such scripted cookbook approaches to spine care. How should we as spine professionals in charge of offering our patients best possible responsible care respond to such a conundrum? Should we perhaps lower our threshold for ordering neuroimaging studies in patients with certain stigmata for multifocal stenosis or disk disease? Can we come up with better questions or physical tests to screen our patients better? Clearly patients with conditions such as severe congenital stenosis in one region of the spine are probably reasonable candidates for consideration for coordinated neuroimaging of the remainder of their spinal columns. Similarly, patients with OPLL or pervasive advanced disk degeneration or hypertrophic osteoarthropathy would likely benefit from neural axis imaging prior to making a detailed surgical plan. At present, our diagnostic algorithm lacks such clarity and routinely leads to contentious approval procedures for more expanded neuroimaging requests.
As we are still trying to sort out the threshold for imaging screening for patients with possible multiregional spine disease, the other question of management—either contemporaneously, as done by Schaffer et al, or staged in separate surgeries—remains completely unanswered at the present time. The magnitude of performing three spine surgeries at the same setting in three different parts of the body of one patient is a major logistics and physiologic undertaking in all regards and likely requires considerably greater investments in postoperative rehabilitation. Any complication in one area would probably have undesirable consequences in the other surgical sites. This question is similar to the option of performing bilateral hip or knee replacement surgeries—a surgical option that has yet to be resolved well over a decade after its introduction. EBSJ-GSJ hopes that its readership will find the discussions of diagnostic and treatment challenges for patients with multiregional symptomatic spinal stenosis to be interesting and worthy of further discussion.
References
- 1.An H S, Glover J M. Lumbar spinal stenosis: historical perspectives, classification, and pathoanatomy. Semin Spine Surg. 1994;6(2):69–77. [Google Scholar]
- 2.Verbiest H. Pathomorphologic aspects of developmental lumbar stenosis. Orthop Clin North Am. 1975;6(1):177–196. [PubMed] [Google Scholar]
- 3.Verbiest H. Results of surgical treatment of idiopathic developmental stenosis of the lumbar vertebral canal. A review of twenty-seven years' experience. J Bone Joint Surg Br. 1977;59(2):181–188. doi: 10.1302/0301-620X.59B2.141452. [DOI] [PubMed] [Google Scholar]
- 4.Arnoldi C C, Brodsky A E, Cauchoix J. et al. Lumbar spinal stenosis and nerve root entrapment syndromes. Definition and classification. Clin Orthop Relat Res. 1976;(115):4–5. [PubMed] [Google Scholar]
- 5.Brain R, Wilkinson M. The association of cervical spondylosis and disseminated sclerosis. Brain. 1957;80(4):456–478. doi: 10.1093/brain/80.4.456. [DOI] [PubMed] [Google Scholar]
- 6.Dagi T F, Tarkington M A, Leech J J. Tandem lumbar and cervical spinal stenosis. Natural history, prognostic indices, and results after surgical decompression. J Neurosurg. 1987;66(6):842–849. doi: 10.3171/jns.1987.66.6.0842. [DOI] [PubMed] [Google Scholar]
- 7.Teng P, Papatheodorou C. Combined cervical and lumbar spondylosis. Arch Neurol. 1964;10:298–307. doi: 10.1001/archneur.1964.00460150068007. [DOI] [PubMed] [Google Scholar]
- 8.Arinzon Z, Adunsky A, Fidelman Z, Gepstein R. Outcomes of decompression surgery for lumbar spinal stenosis in elderly diabetic patients. Eur Spine J. 2004;13(1):32–37. doi: 10.1007/s00586-003-0643-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yamashita K, Ohzono K, Hiroshima K. Five-year outcomes of surgical treatment for degenerative lumbar spinal stenosis: a prospective observational study of symptom severity at standard intervals after surgery. Spine (Phila Pa 1976) 2006;31(13):1484–1490. doi: 10.1097/01.brs.0000219940.26390.26. [DOI] [PubMed] [Google Scholar]
- 10.Aydogan M, Ozturk C, Mirzanli C, Karatoprak O, Tezer M, Hamzaoglu A. Treatment approach in tandem (concurrent) cervical and lumbar spinal stenosis. Acta Orthop Belg. 2007;73(2):234–237. [PubMed] [Google Scholar]
- 11.Epstein N E, Epstein J A, Carras R, Murthy V S, Hyman R A. Coexisting cervical and lumbar spinal stenosis: diagnosis and management. Neurosurgery. 1984;15(4):489–496. doi: 10.1227/00006123-198410000-00003. [DOI] [PubMed] [Google Scholar]
- 12.LaBan M M, Green M L. Concurrent (tandem) cervical and lumbar spinal stenosis: a 10-yr review of 54 hospitalized patients. Am J Phys Med Rehabil. 2004;83(3):187–190. doi: 10.1097/01.phm.0000113405.48879.45. [DOI] [PubMed] [Google Scholar]
- 13.Long D M. Lumbar and cervical spondylosis and spondylotic myelopathy. Curr Opin Neurol Neurosurg. 1993;6(4):576–580. [PubMed] [Google Scholar]
- 14.Bajwa N S, Toy J O, Ahn N U. Is congenital bony stenosis of the cervical spine associated with congenital bony stenosis of the thoracic spine? An anatomic study of 1072 human cadaveric specimens. J Spinal Disord Tech. 2013;26(1):E1–E5. doi: 10.1097/BSD.0b013e3182694320. [DOI] [PubMed] [Google Scholar]
- 15.Bajwa N S, Toy J O, Ahn N U. Is lumbar stenosis associated with thoracic stenosis? A study of 1,072 human cadaveric specimens. Spine J. 2012;12(12):1142–1146. doi: 10.1016/j.spinee.2012.10.029. [DOI] [PubMed] [Google Scholar]
- 16.Hsieh C H, Huang T J, Hsu R W. Tandem spinal stenosis: clinical diagnosis and surgical treatment. Changge-ng Yi-xue Zazhi. 1998;21(4):429–435. [PubMed] [Google Scholar]
- 17.Lee M J, Garcia R, Cassinelli E H, Furey C, Riew K D. Tandem stenosis: a cadaveric study in osseous morphology. Spine J. 2008;8(6):1003–1006. doi: 10.1016/j.spinee.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 18.Chen Y, Chen D Y, Wang X W, Lu X H, Yang H S, Miao J H. Single-stage combined decompression for patients with tandem ossification in the cervical and thoracic spine. Arch Orthop Trauma Surg. 2012;132(9):1219–1226. doi: 10.1007/s00402-012-1540-5. [DOI] [PubMed] [Google Scholar]
- 19.Eskander M S, Aubin M E, Drew J M. et al. Is there a difference between simultaneous or staged decompressions for combined cervical and lumbar stenosis? J Spinal Disord Tech. 2011;24(6):409–413. doi: 10.1097/BSD.0b013e318201bf94. [DOI] [PubMed] [Google Scholar]
- 20.Kikuike K, Miyamoto K, Hosoe H, Shimizu K. One-staged combined cervical and lumbar decompression for patients with tandem spinal stenosis on cervical and lumbar spine: analyses of clinical outcomes with minimum 3 years follow-up. J Spinal Disord Tech. 2009;22(8):593–601. doi: 10.1097/BSD.0b013e3181929cbd. [DOI] [PubMed] [Google Scholar]
- 21.Krishnan A, Dave B R, Kambar A K, Ram H. Coexisting lumbar and cervical stenosis (tandem spinal stenosis): an infrequent presentation. Retrospective analysis of single-stage surgery (53 cases) Eur Spine J. 2014;23(1):64–73. doi: 10.1007/s00586-013-2868-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Naderi S Mertol T Simultaneous cervical and lumbar surgery for combined symptomatic cervical and lumbar spinal stenoses J Spinal Disord Tech 2002153229–231., discussion 231–232 [DOI] [PubMed] [Google Scholar]
- 23.Hong C C, Liu K P. A rare case of multiregional spinal stenosis: clinical description, surgical complication, and management concept review. Global Spine J. 2015;5(1):49–54. doi: 10.1055/s-0034-1378139. [DOI] [PMC free article] [PubMed] [Google Scholar]


