Abstract
Measurement of blood pressure (BP) by a doctor in the clinic has limitations that may result in an unrepresentative measure of underlying BP which can impact on the appropriate assessment and management of high BP. Home BP monitoring is the self-measurement of BP in the home setting (usually in the morning and evening) over a defined period (e.g. 7 days) under the direction of a healthcare provider. When it may not be feasible to measure 24-h ambulatory BP, home BP may be offered as a method to diagnose and manage patients with high BP. Home BP has good reproducibility, is well tolerated, is relatively inexpensive and is superior to clinic BP for prognosis of cardiovascular morbidity and mortality. Home BP can be used in combination with clinic BP to identify ‘white coat’ and ‘masked’ hypertension. An average home BP of at least 135/85 mmHg is an appropriate threshold for the diagnosis of hypertension. Home BP may also offer the advantage of empowering patients with their BP management, with benefits including increased adherence to therapy and lower achieved BP levels. It is recommended that, when feasible, home BP should be considered for routine use in the clinical management of hypertension.
Keywords: blood pressure, blood pressure measurement, guidelines, home blood pressure, hypertension, management, treatment
INTRODUCTION
There is a strong association between high blood pressure (BP) and cardiovascular mortality [1]. About 30% of the Australian adult population have hypertension, although the prevalence is very high (e.g. >80%) in those aged at least 65 years [2,3]. High BP is the most important modifiable population factor contributing to absolute cardiovascular disease (CVD) risk [4]. There is good evidence that BP reduction with antihypertensive therapy reduces cardiovascular events, particularly in those with moderate to severe hypertension [5,6]. More than half of the Australians with elevated BP are not taking antihypertensive medication, but have a high absolute risk of CVD and would benefit from treatment [2].
Uncertainty with respect to the ‘true underlying BP’ is a recognized barrier to correctly diagnose and treat high BP in Australian general practice [7]. Problems with accuracy of clinic BP as a diagnostic tool arise due to the high prevalence of readings that are discordant with out-of-clinic BP. The major advantage of out-of-clinic BP monitoring is that it provides a relatively large number of BP measurements away from the medical environment where the BP relates more closely to risk than does clinic BP. Although home BP monitoring is already in widespread use in Australia and other countries, there is a wide variation in the protocol used and the interpretation of home BP values, indicating a need for guidance [7–11].
The purpose of this document is to provide information on the utility of home BP in the assessment and management of high BP. The review process involved compilation of a draft document by the writing committee, with the intention of updating previous international consensus statements and contextualizing with Australian practice taking into account the overall cardiovascular risk. The manuscript was re-drafted on open discussion among the writing committee during several teleconferences, and then posted to the website of the High Blood Pressure Research Council of Australia with an open call for members to comment. Additional review by a secondary reference panel of Australian professors with expertise in BP was undertaken to produce this final document.
The content of this paper has been endorsed by the High Blood Pressure Research Council of Australia as well as a secondary reference panel comprising: Professors Lawrie Beilin (University of Western Australia, Perth, WA), Mark Brown (University of New South Wales, Sydney, NSW), John Chalmers (The George Institute for Global Health, Sydney, NSW), Garry Jennings (Baker IDI Heart and Diabetes Institute, Melbourne, VIC). Arduino Mangoni (Flinders University, Adelaide, SA), Chris Reid (Monash University, Melbourne, VIC), Lindon Wing (Flinders University, Adelaide, SA).
WHAT IS HOME BLOOD PRESSURE AND HOW DOES IT RELATE TO TWENTY-FOUR-HOUR AMBULATORY BLOOD PRESSURE MONITORING?
Home BP refers to the self-measurement of BP at home and is optimal when readings are taken seated at rest at around the same time in the morning and evening, usually over a period of 1 week. The BP values are recorded by the patient using a validated, automatic BP device, and then conveyed to their doctor for interpretation. The average BP over the monitoring period (discarding the first day of recordings) is used to gauge the risk related to BP. The method is reasonably convenient for patients, is well tolerated [12] and relatively inexpensive. Home BP has reasonable precision, and when approached in a standardized fashion, appears to have better reproducibility than clinic BP and 24-h ambulatory BP monitoring (24-ABPM) [13–15]. Compared with 24-ABPM, home BP is more widely available and provides values of longer-term (day-to-day) BP variability.
The 24-ABPM offers some advantages beyond home BP, such as more detailed identification of morning BP surge, short-term BP variability and nocturnal hypertension or ‘non-dipping’ BP patterns in which prognosis is worse [16,17]. It is possible to also measure night-time BP using some home BP devices, which provide night-time BP values comparable to 24-ABPM [18–21]. BP measured with home BP has also been shown to have good correlation with daytime 24-ABPM [22]. Table 1 provides a summary comparison of the two methods, as well as clinic BP.
TABLE 1.
Comparison of considerations when measuring clinic blood pressure, home blood pressure and 24-h ambulatory blood pressure monitoring
| Considerations | Clinic BP | Home BP | 24-ABPM |
| Doctor-related | |||
| Confidence in assessment | No | Yes | Yes |
| Ability to monitor the effect of therapies | Yes | Yes | Yes |
| Medicare rebate | Yes | No | No |
| Ability to identify ‘white-coat’ and ‘masked’ hypertension | No | Yes | Yes |
| Ability to identify nocturnal BP | No | Yes | Yes |
| Availability for repeat measures | High | High | Low |
| Reproducibility | Low | High | Moderate |
| ’Hypertension’ threshold determined | Yes | Yes | Yes |
| Reference thresholds determined | Yes | Limited | Limited |
| Prognostic value | Low | High | High |
| Patient-related | |||
| Cost of device | Relatively cheap | Relatively cheap | Relatively expensive |
| Health insurance rebate | Not applicable | Yes | No |
| Tolerability | Yes | Yes | Generally ok |
| Encourages engagement and empowerment with medical management | Moderate | High | Moderate |
| Encourages adherence to prescribed medication | Moderate | High | Moderate |
| Healthcare system-related | |||
| Health economic benefit | Moderate | High | High |
| Availability of devices | Yes | Yes | May be limited |
Adapted from [83,119]. 24-ABPM, 24-h ambulatory blood pressure monitoring; BP, blood pressure.
Several international guidelines recommend using home BP as an alternative to 24-ABPM for high BP assessment and management [23–25]. Japanese researchers [26] are the strongest advocates for preferential use of home BP on the basis of a significant body of literature generated in that population. There are many potential scenarios in which complementary use of the methods could aid patient management. For example, among patients with evidence of target organ disease, but normal home BP, night-time BP from 24-ABPM may help explain the clinical findings and thus, therapy may be tailored towards controlling night-time BP [27] (Table 2).
TABLE 2.
Summary points
| High BP is the most important modifiable population factor contributing to cardiovascular disease risk. |
| Uncertainty with respect to ‘true underlying BP’ is a barrier to correctly diagnose and treat high BP in general practice. |
| Home BP provides a more reliable estimate of BP predicting risk than clinic BP. |
BP, blood pressure.
HOME BLOOD PRESSURE AND PROGNOSIS
Multiple BP measures away from the clinic have a better predictive value than clinic readings regarding BP-related clinical outcomes, and studies with 24-ABPM have shown prognostic superiority beyond clinic and home BP for predicting cardiovascular events [28,29]. Compared with clinic BP, home BP has stronger associations with hypertensive target organ disease [30–34], as well as being a better predictor of cardiovascular events and mortality [35–41]. Despite this, there is a lack of randomized, controlled data showing that antihypertensive intervention based on home BP improves prognosis [42] or is superior to clinic BP [43]. It should also be noted that clinic BP still has an important role in general practice for screening BP as part of the usual physical examination for CVD risk and also for monitoring BP in those people where there is little (or no) discrepancy between clinic and out-of-clinic BP.
HOME BLOOD PRESSURE FOR DETECTION OF WHITE-COAT AND MASKED HYPERTENSION
While the gold standard for determining white-coat or masked hypertension is 24-ABPM [44], home BP can also be used to detect these phenomena among treated or untreated patients [45–50]. White-coat hypertension is relatively common, with a prevalence of approximately 13% in the general population and approximately 32% among adults with hypertension based on clinic readings [51; all remaining references, 51–119, are contained in the supplementary material]. It is yet to be fully confirmed if white coat hypertension confers increased cardiovascular risk, however, the condition is associated with increased probability for developing sustained hypertension and type 2 diabetes [53,54], but does not appear to increase mortality risk [55,56]. Interpretation of mortality risk data can be problematic due to differing definitions of white-coat hypertension, and the possibility that patients with white-coat hypertension were commenced on antihypertensive treatment based on repeated high BP readings in the doctor's clinic [57].
Home BP measurement can be used to detect masked hypertension [48–50], which carries a similar risk for incident cardiovascular events to that of sustained high BP [55,56,58]. Prevalence rates range from 10 to 17% [24] and may be up to 29% in untreated patients with diabetes [59] or even as high as 50% in some studies of patients with treated hypertension [58] or exercise hypertension [60]. It remains unclear whether treatment of masked hypertension or white-coat hypertension is beneficial, but since each condition is associated with increased cardiovascular risk due to developing sustained hypertension, appropriate ongoing monitoring of these patients is advised. Masked hypertension should be suspected in general practice when the clinic BP appears normal, but there is target organ damage consistent with having hypertension (Table 3).
TABLE 3.
Summary points
| Home BP is optimal when readings are taken around the same time in the morning and evening (usually over 7 days). |
| Home BP is superior to clinic BP in terms of associations with end-organ disease, cardiovascular events and mortality. |
| Home BP can be used to detect ‘white-coat’ and ‘masked hypertension’. |
BP, blood pressure.
HOME BLOOD PRESSURE FOR ASSESSMENT OF ANTIHYPERTENSIVE TREATMENT
Home BP provides a reliable estimate of the effectiveness of antihypertensive treatment [61–65]. A pharmacist-led randomized controlled study found that therapy guided by home BP compared with usual care based on clinic BP led to significantly more patients achieving BP control, larger BP reductions, more medication intensification and higher patient satisfaction [62]. The addition of home BP telemonitoring managed by pharmacists produces similar improvements in BP control [66]. Home BP can also be used to identify true drug resistance [61,64]. A meta-analysis on the effectiveness of home BP measured with additional patient support showed a significant reduction in BP over 12 months of intervention [67].
COST-EFFECTIVENESS OF HOME BLOOD PRESSURE
Health economic assessment using home BP compared with usual care based on clinic BP or in combination with 24-ABPM is complex and varies between countries, as well as study designs. There has been a strong call to action to use and reimburse the costs of home BP measurement in the United States [68], but little movement in Australia. Most home BP devices are relatively cheap (∼AUD 100), and may be reimbursable through Australian private health insurance. Lending schemes (hire or borrow) through healthcare providers can also be used to improve access to home BP devices.
Home BP has been shown to be cost neutral after taking into account the number of consultations, drugs, referrals, equipment and training expenses [69], and cost-effective in terms of reduced medication [70] and potential health insurance savings [71]. Health system savings may also accrue by avoiding treating white-coat hypertension [72]. In keeping with these data [69–72], a meta-analysis of randomized controlled studies found that home BP monitoring was associated with lower medical costs, but these savings were offset by equipment and technology costs relating to telemonitoring, such that overall home BP was more costly than usual care [73]. Telemonitoring is distinct from routine home BP, and despite being an effective means to reduce BP [74], cheaper home BP telemonitoring methods need to be developed to improve cost-effectiveness of this approach [73]. At present, telemonitoring is not common in Australia.
OTHER ADVANTAGES OF HOME BLOOD PRESSURE MEASUREMENT
Home BP has advantages of engaging and empowering the patient in their own BP management, strengthening the doctor–patient relationship and increasing adherence to therapy [66,75–77]. Additionally, regular home BP monitoring can lead to lower BP than standard care [78–80] and more active treatment by doctors [79]. On the basis of limited evidence, a systematic review [81] concluded that improved medication adherence by using home BP was not as successful in the primary care setting compared with hospital-based or non-clinical (community centre/work place) settings, suggesting that patient adherence-enhancing strategies may need to be considered for optimizing care in general practice (e.g. patient education and follow-up contact with health professionals leading to clinical action/change) [82] (Table 4).
TABLE 4.
Summary points
| Home BP can be used to estimate the effectiveness of antihypertensive treatment. |
| Health system savings are possible using home BP. |
| Home BP may help engage and empower the patient in their hypertension management and increases adherence to therapy, thus improving hypertension control. |
BP, blood pressure.
STANDARDIZED MEASUREMENT OF HOME BLOOD PRESSURE
It is well known that a multitude of intrinsic (e.g. level of relaxation) and extrinsic (e.g. BP device validation) factors can affect the reliability of BP readings in all settings, and care should be taken to minimize these potential sources of error by adopting a standardized approach. The recommendations in Table 5 are based on international guidelines [23,83], and review articles [84], with Australian context built in.
TABLE 5.
Recommendations for patients on how to measure home blood pressure
| What BP device to use? |
| Use a validated automated machine, preferably with storage memory (a list of validated BP devices can be found at http://www.bhsoc.org/bp-monitors/bp-monitors/) |
| Buya, hire or borrow a machine |
| Use an appropriate-sized cuff (fits the arm within the accepted range indicated on the cuff) |
| Use an upper arm cuff (not a wrist or finger cuff) |
| When to take home BP? |
| Take measures at around the same time in the morning and evening |
| Take before medication, food or vigorous exercise |
| Take for 7 days (5 day minimum) |
| Take as advised by your doctor, for example, before visiting the doctor or after medication change |
| How to take home BP? |
| Sit quietly for 5 min (no talking/distractions such as TV/extreme temperatures) |
| Sit with feet flat on floor, legs uncrossed, upper arm bare, back and arm supported (relaxed position with the cuff at heart level) |
| Take two BP readings 1 min apart |
| Record each BP reading in a paper diary or an electronic spreadsheet |
| Take a copy of the BP readings to the doctor appointmentb |
| Do not smoke or drink caffeine 30 min before measuring BP |
| Do not measure your BP if uncomfortable, stressed or in pain |
BP, blood pressure.
aAutomated BP machines can be purchased from a chemist, online or from a medical equipment supplier. Rebates (up to 100% depending on individual policy) are available from most Australian private health insurance providers.
bAverage the BP values over all the days, but discard the readings on the first day of monitoring.
What blood pressure device to use?
A validated, automated BP monitor (preferably with storage memory) using a correct-sized upper arm cuff should be used.
The device should be tested for validity in the specific patient population intended for use (e.g. pregnant, arrhythmia) [23]. A list of validated devices can be found at the British Hypertension Society website (http://www.bhsoc.org/bp-monitors/bp-monitors/). Validation is judged according to British Hypertension Society standards [85] or the International Protocol [86,87] based on comparison with mercury sphygmomanometry. Devices with storage memory (or unbiased methods such as that achieved with telemonitoring) are preferred because patient diaries may lack reliability due to selective reporting [88–91].
An appropriate-sized cuff must be used (i.e. fits the arm within the accepted range indicated on the cuff). A cuff that is too small will overestimate BP (‘under-cuffing’), and a cuff that is too large will underestimate BP (‘over-cuffing’) [92]; thus, inappropriate cuff size (‘mis-cuffing’) can lead to incorrect home BP values [93]. Wrist and finger cuff monitors should be avoided as these are less likely to have passed validation testing and have greater propensity for inaccuracy due to arm positioning [23]. However, in patients with a very large arm circumference that is beyond the cuff range, it may be a reasonable option to use a validated wrist device.
When to take home blood pressure?
As advised by a healthcare provider, home BP should be measured at around the same time in the morning and the evening over a 7-day period.
Monitoring should only be performed over periods as directed by a healthcare provider. This may include initial assessment of BP, but also to assess the effects of treatment. Typically, this would be the 7-day period before a clinic visit; approximately 4 weeks after initiating a change in medication regimen [94] or at regular long-term intervals (e.g. 6 months) in keeping with appropriate clinical follow-up according to baseline cardiovascular risk [84,95], as per the treatment algorithm (Fig. 1). A period of 7 days appears to be the measurement period with the best prognostic and diagnostic value [96,97], and is the accepted standard [23,25,26,83,98], although a minimum of 5 days has been shown to provide a reliable estimate of BP control [99,100].
FIGURE 1.
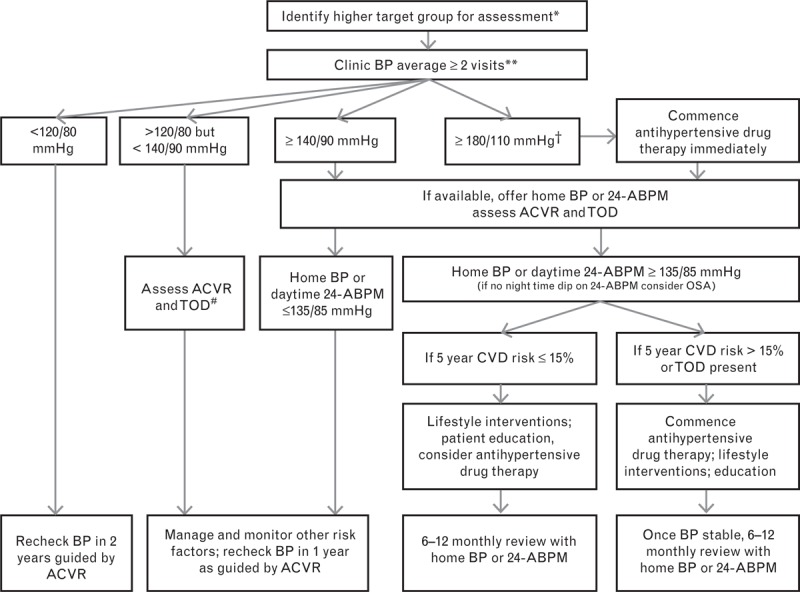
Proposed algorithm for blood pressure (BP) assessment in general practice. Home BP values determined from the average of two morning and two evening readings (taken over 7 days), but discarding the first day of monitoring. This algorithm is derived from: the Australian Heart Foundation Guidelines to Management of Hypertension (2010); the Australian National Vascular Disease Prevention Alliance, Guidelines for the assessment of absolute cardiovascular disease risk; the Australian Ambulatory Blood Pressure Monitoring Consensus Position Statement (2012); The United Kingdom National Institute of Clinical Excellence Clinical Management of Primary Hypertension in Adults Guidelines (2011); the Canadian Hypertension Education Program Recommendations for the Management of Hypertension (2012); the European Society of Hypertension and of the European Society of Cardiology Guidelines for the management of arterial hypertension (2013) and Palatini Ambulatory and home blood pressure measurement (2012). ∗Higher-risk individuals include all adults aged 45–74 years without known history of CVD, Aboriginal and Torres Strait Islander adults aged 35 years or older, adults with diabetes aged 45–60 years, adults who are overweight or obese, adults with atrial fibrillation. ∗∗Australian Heart Foundation Guidelines suggest ‘multiple measurements taken on several separate occasions, for example, at least twice, one or more weeks apart unless severe.’ †If hypertensive emergency/accelerated hypertension refer same day for specialist care. #If raised ACVR or evidence of TOD, consider home BP or 24-ABPM. 24-ABPM, 24-h ambulatory BP monitoring; ACVR, absolute cardiovascular risk; CVD, cardiovascular disease; OSA, obstructive sleep apnoea; TOD, target organ disease.
The circadian pattern of BP changes from the morning to evening, with evidence linking morning and evening high BP to increased cardiovascular risk [101–104]. Home BP should be recorded in the morning (before medication if treated) and in the evening. Measures should be taken after voiding and before food or vigorous exercise. Caffeine and cigarettes each have an acute pressor effect, and when combined, are additive [105]. Home BP, therefore, should preferably be measured before, or at least 30 min after, these stimulants. It may be useful to ask patients to record home BP at other times in addition to the morning and evening (or in positions other than sitting as described in the next section).
How to take home blood pressure?
At home, BP should be measured in a quiet room after 5 min seated rest; two readings should be taken, 1 min apart, with the BP recorded immediately in a diary (if device has no memory function).
The seated position should be feet flat on floor, legs uncrossed, upper arm bare, back supported and arm supported in a relaxed position, with the cuff at heart level. If the cuff is above or below the level of the heart, BPs may be decreased or increased, respectively (approximately 0.7 mmHg/cm) due to the contribution of hydrostatic pressure changes and local vasoactive responses [106]. If the cuff is applied so that its midpoint is at about the midpoint of the upper arm, this will approximate the level of the heart. Patients should not be distracted (e.g. talking, television). Similarly, BP should not be taken if the patient is affected by extremes of temperature, or is uncomfortable, stressed or in pain.
After 5 min rest, the patient should take two consecutive measures 1 min apart, and after each measure record the SBP and DBP. Patients may not be compliant with a rest period before recording BP and this could lead to higher home BP values [107]. They should be asked to note any unusual things that may affect readings. Standing BP may be requested when orthostatic hypotension is suspected. BP measures at 1 and 3 min after standing are recommended in these circumstances. The home BP measure is derived by averaging of the BP values after discarding the first day of readings (Table 6).
TABLE 6.
Summary points
| Many factors can affect the reliability of home BP readings and care should be taken to minimize this possibility by using a standardized approach to measurement. |
| Home BP devices should be validated. |
| Standing BP measures may be taken when orthostatic hypotension is suspected. |
BP, blood pressure.
USE OF HOME BLOOD PRESSURE FOR HIGH BLOOD PRESSURE ASSESSMENT/BLOOD PRESSURE THRESHOLDS
Whilst 24-ABPM is recommended in Australia for diagnosis and provision of optimal care related to BP management, concerns remain about availability, the logistics of training and cost. Assessment of high BP has lower cut points for BP measured away from the clinic due to reduction in white-coat effects. Definitions of BP categories based on clinic, home and 24-ABPM are denoted in Table 7. The recommended home BP hypertension threshold of at least 135/85 mmHg is based on a systematic review of evidence by a writing committee of the European Society of Hypertension [83]. Gaps in evidence exist with respect to home BP thresholds across BP categories.
TABLE 7.
Definition of blood pressure categories in Australia based on average SBP and DBP measured in the clinic, home or with 24-h ambulatory blood pressure monitoring
| BP category | Clinic BP (mmHg) | Home BP (mmHg) | 24-ABPM (mmHg) | ||
| 24-h | Day | Night | |||
| ‘Normal’ | <120/80 | Not yet determined | <115/75a | <120/80a | >105/65a |
| High-normal threshold | ≥120/80 | Not yet determined | ≥115/75a | ≥120/80a | ≥105/65a |
| Stage 1 (mild) hypertension threshold | ≥140/90 | ≥135/85b | ≥130/80 | ≥135/85 | ≥120/70 |
| Stage 2 (moderate) hypertension threshold | ≥160/100 | ≥145/90c | ≥148/93a | ≥152/96a | ≥139/84a |
| Stage 3 (severe) hypertension threshold | ≥180/110 | Not yet determined | ≥163/101a | ≥168/105a | ≥157/93a |
Home BP values determined from the average of two morning and two evening readings (taken over 7 days), but discarding the first day of monitoring. 24-ABPM, 24-h ambulatory blood pressure monitoring; BP, blood pressure. As per usual recommendations, if the patient's SBP or DBP falls into different categories, the higher diagnostic category is applied.
aThresholds based on systematic review and consensus by a writing committee of the Australian Consensus Statement [44].
bThresholds based on systematic review and consensus by a writing committee of the European Society of Hypertension [83].
cThresholds based on systematic review and consensus by a writing committee of the International Database of Home Blood Pressure in Relation to Cardiovascular Outcome Investigators [108,109].
Analyses from the International Database of Home Blood Pressure in Relation to Cardiovascular Outcome (IDHOCO) Investigators [108–110] provide rounded home BP thresholds across clinic BP categories according to European hypertension management guidelines [24]. These home BP thresholds were derived from 10-year cardiovascular risk estimates and tended to be slightly lower than previous recommendations [83]. However, there was evidence that home BP thresholds may be slightly higher among people aged at least 60 years [109], which could have clinical relevance, but further investigation will be needed to confirm this.
Guidelines produced by the National Vascular Diseases Prevention Alliance [for adults without known history of CVD aged 45 years and over (35 years and over for Aboriginal Australians and Torres Strait Islanders)] recommend that the decision to medicate previously untreated patients should be based on an absolute CVD risk assessment [111]. Algorithms used in the Australian cardiovascular risk calculator are based on clinic BP measures. Whilst there is little evidence to guide this, we suggest correcting the home BP measure before entry into the risk calculator (i.e. add 5 mmHg to the SBP and DBPs) [112].
SCREENING FOR HYPERTENSION
Clinic BP remains the most practical way to screen for high BP [28]. However, clinic BP readings by a doctor will overestimate cardiovascular risk in white-coat hypertension and underestimate risk in masked hypertension. A potentially important advance in screening has been the use of unobserved automated BP recording [113]. This gives an approximation of average daytime ABPM and minimizes the white-coat effect. While there are sound reasons to promote the widespread use of unobserved automated BP measurement in the clinic, in pharmacies and at other sites where BP screening is undertaken, more data are needed to confirm the value of this method.
The algorithm for BP assessment in general practice (Fig. 1) takes into consideration current national and international BP and absolute CVD risk management guidelines [24,25,28,44,111,114,115]. As stated above, at present, cardiovascular risk calculations are based on clinic BP readings. When relevant, individual disease management guidelines can be referred to [111,116–118] (Table 8).
TABLE 8.
Summary points
| Home BP hypertension threshold is at least 135/85 mmHg. |
| The decision to medicate should be based on absolute risk estimation. |
BP, blood pressure.
In conclusion, home BP offers several advantages beyond clinic BP: detection of white-coat and masked hypertension, better prognostic indication, better evaluation of BP control, improved long-term compliance with drug treatment (and, thereby, hypertension control) and greater engagement with and empowerment of patients. It is cost-effective and may also be used as a complementary tool to 24-ABPM. Home BP should be recorded using validated devices in a systematic and standardized fashion at the direction of health practitioners. It is optimal for decisions regarding BP therapy to be made with consideration of absolute cardiovascular risk and, when feasible, home BP should be considered for routine use in clinical practice.
ACKNOWLEDGEMENTS
The writing group is very grateful to Alison Wilson from the National Heart Foundation of Australia for the significant input she had to the content of this paper. Open access to this article was made possible with funding from the High Blood Pressure Research Council of Australia.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Abbreviations: 24-ABPM, 24-h ambulatory BP monitoring; BP, blood pressure; CVD, cardiovascular disease
The content of this paper has been endorsed by the High Blood Pressure Research Council of Australia as well as a secondary reference panel comprising: Professors Lawrie Beilin (University of Western Australia, Perth, WA), Mark Brown (University of New South Wales, Sydney, NSW), John Chalmers (The George Institute for Global Health, Sydney, NSW), Garry Jennings (Baker IDI Heart and Diabetes Institute, Melbourne, VIC). Arduino Mangoni (Flinders University, Adelaide, SA), Chris Reid (Monash University, Melbourne, VIC), Lindon Wing (Flinders University, Adelaide, SA).
REFERENCES
- 1.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002; 360:1903–1913. [DOI] [PubMed] [Google Scholar]
- 2.Briganti EM, Shaw JE, Chadban SJ, Zimmet PZ, Welborn TA, McNeil JJ, Atkins RC. Untreated hypertension among Australian adults: the 1999–2000 Australian Diabetes, Obesity and Lifestyle Study (AusDiab). Med J Aust 2003; 179:135–139. [DOI] [PubMed] [Google Scholar]
- 3.Australian Health Survey. Health service usage and health related actions, 2011–12 (cat. no. 4364.0.55.002). [Google Scholar]
- 4.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380:2224–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Musini VM, Tejani AM, Bassett K, Wright JM. Pharmacotherapy for hypertension in the elderly. Cochrane Database Syst Rev 2009; CD000028. [DOI] [PubMed] [Google Scholar]
- 6.Wright JM, Musini VM. First-line drugs for hypertension. Cochrane Database Syst Rev 2009; CD001841. [DOI] [PubMed] [Google Scholar]
- 7.Howes F, Hansen E, Williams D, Nelson M. Barriers to diagnosing and managing hypertension: a qualitative study in Australian general practice. Aust Fam Physician 2010; 39:511–516. [PubMed] [Google Scholar]
- 8.Howes F, Hansen E, Nelson M. Management of hypertension in general practice: a qualitative needs assessment of Australian GPs. Aust Fam Physician 2012; 41:317–323. [PubMed] [Google Scholar]
- 9.McManus RJ, Wood S, Bray EP, Glasziou P, Hayen A, Heneghan C, et al. Self-monitoring in hypertension: a web-based survey of primary care physicians. J Hum Hypertens 2014; 28:123–127. [DOI] [PubMed] [Google Scholar]
- 10.Ostchega Y, Berman L, Hughes JP, Chen TC, Chiappa MM. Home blood pressure monitoring and hypertension status among US adults: the National Health and Nutrition Examination Survey (NHANES), 2009–2010. Am J Hypertens 2013; 26:1086–1092. [DOI] [PubMed] [Google Scholar]
- 11.Wang Y, Wang Y, Gu H, Qain Y, Zhang J, Tang X, et al. Use of home blood pressure monitoring among hypertensive adults in primary care: Minhang community survey. Blood Press Monit 2014; 19:140–144. [DOI] [PubMed] [Google Scholar]
- 12.Nasothimiou EG, Karpettas N, Dafni MG, Stergiou GS. Patients’ preference for ambulatory versus home blood pressure monitoring. J Hum Hypertens 2014; 28:224–229. [DOI] [PubMed] [Google Scholar]
- 13.Stergiou GS, Baibas NM, Gantzarou AP, Skeva II, Kalkana CB, Roussias LG, Mountokalakis TD. Reproducibility of home, ambulatory, and clinic blood pressure: implications for the design of trials for the assessment of antihypertensive drug efficacy. Am J Hypertens 2002; 15:101–104. [DOI] [PubMed] [Google Scholar]
- 14.Warren RE, Marshall T, Padfield PL, Chrubasik S. Variability of office, 24-h ambulatory, and self-monitored blood pressure measurements. Br J Gen Pract 2010; 60:675–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ragot S, Genes N, Vaur L, Herpin D. Comparison of three blood pressure measurement methods for the evaluation of two antihypertensive drugs: feasibility, agreement, and reproducibility of blood pressure response. Am J Hypertens 2000; 13:632–639. [DOI] [PubMed] [Google Scholar]
- 16.Hansen TW, Li Y, Boggia J, Thijs L, Richart T, Staessen JA. Predictive role of the nighttime blood pressure. Hypertension 2011; 57:3–10. [DOI] [PubMed] [Google Scholar]
- 17.Roush GC, Fagard RH, Salles GF, Pierdomenico SD, Reboldi G, Verdecchia P, et al. Prognostic impact from clinic, daytime, and night-time systolic blood pressure in nine cohorts of 13 844 patients with hypertension. J Hypertens 2014; 32:2332–2340. [DOI] [PubMed] [Google Scholar]
- 18.Ishikawa J, Shimizu M, Sugiyama Edison E, Yano Y, Hoshide S, Eguchi K, Kario K. Assessment of the reductions in night-time blood pressure and dipping induced by antihypertensive medication using a home blood pressure monitor. J Hypertens 2014; 32:82–89. [DOI] [PubMed] [Google Scholar]
- 19.Ishikawa J, Hoshide S, Eguchi K, Ishikawa S, Shimada K, Kario K. Nighttime home blood pressure and the risk of hypertensive target organ damage. Hypertension 2012; 60:921–928. [DOI] [PubMed] [Google Scholar]
- 20.Ushio H, Ishigami T, Araki N, Minegishi S, Tamura K, Okano Y, et al. Utility and feasibility of a new programmable home blood pressure monitoring device for the assessment of nighttime blood pressure. Clin Exp Nephrol 2009; 13:480–485. [DOI] [PubMed] [Google Scholar]
- 21.Stergiou GS, Triantafyllidou E, Cholidou K, Kollias A, Destounis A, Nasothimiou EG, et al. Asleep home blood pressure monitoring in obstructive sleep apnea: a pilot study. Blood Press Monit 2013; 18:21–26. [DOI] [PubMed] [Google Scholar]
- 22.Little P, Barnett J, Barnsley L, Marjoram J, Fitzgerald-Barron A, Mant D. Comparison of agreement between different measures of blood pressure in primary care and daytime ambulatory blood pressure. BMJ 2002; 325:254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parati G, Stergiou GS, Asmar R, Bilo G, de Leeuw P, Imai Y, et al. European Society of Hypertension Practice Guidelines for home blood pressure monitoring. J Hum Hypertens 2010; 24:779–785. [DOI] [PubMed] [Google Scholar]
- 24.Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013; 31:1281–1357. [DOI] [PubMed] [Google Scholar]
- 25.Daskalopoulou SS, Khan NA, Quinn RR, Ruzicka M, McKay DW, Hackam DG, et al. The 2012 Canadian Hypertension Education Program recommendations for the management of hypertension: blood pressure measurement, diagnosis, assessment of risk, and therapy. Can J Cardiol 2012; 28:270–287. [DOI] [PubMed] [Google Scholar]
- 26.Imai Y, Kario K, Shimada K, Kawano Y, Hasebe N, Matsuura H, et al. The Japanese Society of Hypertension guidelines for self-monitoring of blood pressure at home (second edition). Hypertens Res 2012; 35:777–795. [DOI] [PubMed] [Google Scholar]
- 27.Hermida RC, Ayala DE, Mojon A, Smolensky MH, Portaluppi F, Fernandez JR. Sleep-time ambulatory blood pressure as a novel therapeutic target for cardiovascular risk reduction. J Hum Hypertens 2014; 28:567–574. [DOI] [PubMed] [Google Scholar]
- 28.Hypertension. The clinical management of primary hypertension in adults: update of clinical guidelines 18 and 34 [Internet]. 2011; 2013. [PubMed] [Google Scholar]
- 29.Niiranen TJ, Maki J, Puukka P, Karanko H, Jula AM. Office, home, and ambulatory blood pressures as predictors of cardiovascular risk. Hypertension 2014; 19:03292. [DOI] [PubMed] [Google Scholar]
- 30.Tsunoda S, Kawano Y, Horio T, Okuda N, Takishita S. Relationship between home blood pressure and longitudinal changes in target organ damage in treated hypertensive patients. Hypertens Res 2002; 25:167–173. [DOI] [PubMed] [Google Scholar]
- 31.Mule G, Caimi G, Cottone S, Nardi E, Andronico G, Piazza G, et al. Value of home blood pressures as predictor of target organ damage in mild arterial hypertension. J Cardiovasc Risk 2002; 9:123–129. [DOI] [PubMed] [Google Scholar]
- 32.Gaborieau V, Delarche N, Gosse P. Ambulatory blood pressure monitoring versus self-measurement of blood pressure at home: correlation with target organ damage. J Hypertens 2008; 26:1919–1927. [DOI] [PubMed] [Google Scholar]
- 33.Tachibana R, Tabara Y, Kondo I, Miki T, Kohara K. Home blood pressure is a better predictor of carotid atherosclerosis than office blood pressure in community-dwelling subjects. Hypertens Res 2004; 27:633–639. [DOI] [PubMed] [Google Scholar]
- 34.Matsumoto A, Satoh M, Kikuya M, Ohkubo T, Hirano M, Inoue R, et al. Day-to-day variability in home blood pressure is associated with cognitive decline: the Ohasama study. Hypertension 2014; 63:1333–1338. [DOI] [PubMed] [Google Scholar]
- 35.Imai Y, Ohkubo T, Sakuma M, Tsuji II, Satoh H, Nagai K, et al. Predictive power of screening blood pressure, ambulatory blood pressure and blood pressure measured at home for overall and cardiovascular mortality: a prospective observation in a cohort from Ohasama, northern Japan. Blood Press Monit 1996; 1:251–254. [PubMed] [Google Scholar]
- 36.Ohkubo T, Imai Y, Tsuji I, Nagai K, Kato J, Kikuchi N, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens 1998; 16:971–975. [DOI] [PubMed] [Google Scholar]
- 37.Sega R, Facchetti R, Bombelli M, Cesana G, Corrao G, Grassi G, Mancia G. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) study. Circulation 2005; 111:1777–1783. [DOI] [PubMed] [Google Scholar]
- 38.Ward AM, Takahashi O, Stevens R, Heneghan C. Home measurement of blood pressure and cardiovascular disease: systematic review and meta-analysis of prospective studies. J Hypertens 2012; 30:449–456. [DOI] [PubMed] [Google Scholar]
- 39.Fuchs SC, Mello RG, Fuchs FC. Home blood pressure monitoring is better predictor of cardiovascular disease and target organ damage than office blood pressure: a systematic review and meta-analysis. Curr Cardiol Rep 2013; 15:013–0413. [DOI] [PubMed] [Google Scholar]
- 40.Noguchi Y, Asayama K, Staessen JA, Inaba M, Ohkubo T, Hosaka M, et al. Predictive power of home blood pressure and clinic blood pressure in hypertensive patients with impaired glucose metabolism and diabetes. J Hypertens 2013; 31:1593–1602. [DOI] [PubMed] [Google Scholar]
- 41.Niiranen TJ, Hänninen M-R, Johansson J, Reunanen A, Jula AM. Home-measured blood pressure is a stronger predictor of cardiovascular risk than office blood pressure. Hypertension 2010; 55:1346–1351. [DOI] [PubMed] [Google Scholar]
- 42.Asayama K, Ohkubo T, Metoki H, Obara T, Inoue R, Kikuya M, et al. Cardiovascular outcomes in the first trial of antihypertensive therapy guided by self-measured home blood pressure. Hypertens Res 2012; 35:1102–1110. [DOI] [PubMed] [Google Scholar]
- 43.Staessen JA, Den Hond E, Celis H, Fagard R, Keary L, Vandenhoven G, O’Brien ET. Antihypertensive treatment based on blood pressure measurement at home or in the physician's office: a randomized controlled trial. JAMA 2004; 291:955–964. [DOI] [PubMed] [Google Scholar]
- 44.Head GA, McGrath BP, Mihailidou AS, Nelson MR, Schlaich MP, Stowasser M, et al. Ambulatory blood pressure monitoring in Australia: 2011 consensus position statement. J Hypertens 2012; 30:253–266. [DOI] [PubMed] [Google Scholar]
- 45.Shimizu M, Shibasaki S, Kario K. The value of home blood pressure monitoring. Curr Hypertens Rep 2006; 8:363–367. [DOI] [PubMed] [Google Scholar]
- 46.Saladini F, Benetti E, Malipiero G, Casiglia E, Palatini P. Does home blood pressure allow for a better assessment of the white-coat effect than ambulatory blood pressure? J Hypertens 2012; 30:2118–2124. [DOI] [PubMed] [Google Scholar]
- 47.Mancia G, Facchetti R, Bombelli M, Grassi G, Sega R. Long-term risk of mortality associated with selective and combined elevation in office, home, and ambulatory blood pressure. Hypertension 2006; 47:846–853. [DOI] [PubMed] [Google Scholar]
- 48.Asayama K, Thijs L, Brguljan-Hitij J, Niiranen TJ, Hozawa A, Boggia J, et al. Risk stratification by self-measured home blood pressure across categories of conventional blood pressure: a participant-level meta-analysis. PLoS Med 2014; 11:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nagai K, Imai Y, Tsuji I, Ohkubo T, Sakuma M, Watanabe N, et al. Prevalence of hypertension and rate of blood pressure control as assessed by home blood pressure measurements in a rural Japanese community, Ohasama. Clin Exp Hypertens 1996; 18:713–728. [DOI] [PubMed] [Google Scholar]
- 50.Terawaki H, Metoki H, Nakayama M, Ohkubo T, Kikuya M, Asayama K, et al. Masked hypertension determined by self-measured blood pressure at home and chronic kidney disease in the Japanese general population: the Ohasama study. Hypertens Res 2008; 31:2129–2135. [DOI] [PubMed] [Google Scholar]


