Abstract
Heterozygous mutations in GATA2 underlie different syndromes, previously described as monocytopenia and mycobacterial avium complex infection (MonoMAC); dendritic cell, monocytes, B- and NK lymphocytes deficiency (DCML); lymphedema, deafness and myelodysplasia (Emberger syndrome) and familiar myelodysplastic syndrome/acute myeloid leukemia (MDS / AML). Onset and severity of clinical symptoms vary and preceding cytopenias are not always present.
We describe a case of symptomatic DCML deficiency and rather discrete bone marrow findings due to GATA2 mutation. Exome sequencing revealed a somatic ASXL1 mutation and the patient underwent allogeneic stem cell transplantation successfully.
Keywords: GATA2 mutation, Myelodysplastic syndrome, ASXL1 mutation, Allogeneic hematopoietic stem cell transplantation
Highlights
-
•
Allogeneic stem cell transplantation was performed for DCML caused by GATA2 mutation.
-
•
Genetic diagnostics were done by Sanger sequencing and whole exome sequencing.
-
•
We identified an ASXL1 mutation associated with high risk for leukemic transformation.
1. Introduction
The transcription factor GATA2 has a complex role in the development of hematopoiesis and lymphopoiesis but even in differentiation of non-hematopoietic progenitors. Haploinsufficiency of GATA2 leads to a variety of clinical and laboratory findings. It has been previously described that heterozygous mutations in GATA2 underlie different syndromes defined by monocytopenia and mycobacterial avium complex infection (MonoMAC), deficiency of dendritic cells, monocytes, B- and NK lymphocytes (DCML), lymphedema, deafness and myelodysplasia (Emberger syndrome) or familiar myelodysplastic syndrome/acute myeloid leukemia (MDS/AML) [1], [2], [3].
Different types of mutations are known to cause loss of function of the mutated allele leading to haploinsufficiency of GATA2, and a correlation with certain clinical symptoms has been described in some cases [4], [5], [6]. Germline mutations of GATA2 are transmitted with autosomal dominant inheritance. However, even among hereditary cases, there is a great variation of clinical findings, time of manifestation and even severity of disease in patients with GATA2 mutations. Clinical characteristics in most patients include immunodeficiency with susceptibility to human papillomavirus (HPV) and non-tuberculous mycobacteria (NTM), predisposition to MDS/AML, pulmonary proteinosis (PAP) and congenital lymphedema. These symptoms might occur with or without preceding cytopenias and different medical specialties are involved in the diagnosis and management of these patients. The only curative treatment so far is allogeneic hematopoietic stem cell transplantation (allo-HSCT). Therefore, it is crucial to diagnose patients with GATA2 mutations as early as possible.
We report a case of DCML deficiency and MDS in a patient with GATA2 mutation who successfully underwent allogeneic stem cell transplantation.
2. Case report
A 38-year old woman presented at the Department of Hematology, Lund University hospital in January 2011 with microcytic anemia. She was referred from the gynecology department where she has been treated for severe and recurrent condylomata. During the last 10 years, she had gone repeatedly through surgical intervention for severe condylomata, that were positive for HPV type 6. Additionally, the patient has been treated for recurrent pneumonia. Due to work related reasons, she had moved within Europe several times. Already at the age of 12, she was diagnosed with anemia in Germany, presumably caused by iron deficiency. Due to persisting anemia, a bone marrow biopsy was done in the Netherlands in 2008 and she was diagnosed with MDS refractory anemia (RA), IPSS low, normal karyotype. She has never required blood transfusions.
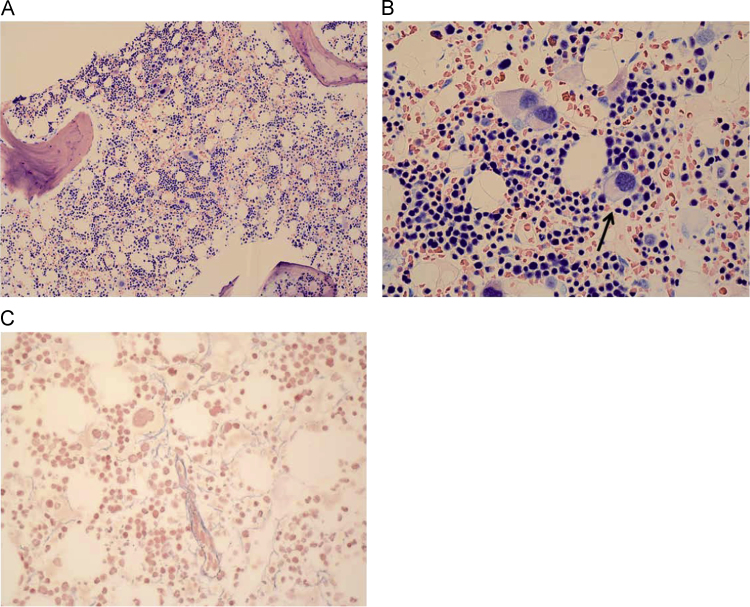
At presentation, she had adapted to a hemoglobin level of 79 g/l and had only occasional discrete symptoms of her anemia, as fatigue, other constitutional symptoms were absent. She described her menstruation as mostly normal, but sometimes heavy and prolonged due to known uterine myoma. She had no other history of bleeding. Platelets and WBC count were normal. Differential blood counts showed a discrete lymphopenia and complete absence of monocytes. A lymphocyte profile showed low levels of NK-cells (0.02×109), CD4 T-cells (0.12×109) and B-cells (0.01×109). We performed a new bone marrow biopsy in 2012 in which the previous diagnosis of MDS RA could be confirmed even if signs of dysplasia were rather discrete with mainly dysplastic megakaryocytes. No fibrosis was found (Fig. 1). The bone marrow cells still showed a normal karyotype in routine cytogenetics. She did respond to oral iron substitution to some degree with Hb around 90 g/l.
Fig. 1.
Morphology of the bone marrow biopsy before treatment. (A) May-Giemsa Grünwald (MGG), ×10: cellularity around 40%, considered to be normal for the patients age of 37, with normally distributed megakaryocytes. (B) MGG, ×40: some dysplastic megakaryocytes (arrow) with hypolobulated nuclei. (C) Gomori silver stain: normal content of reticulin fibers.
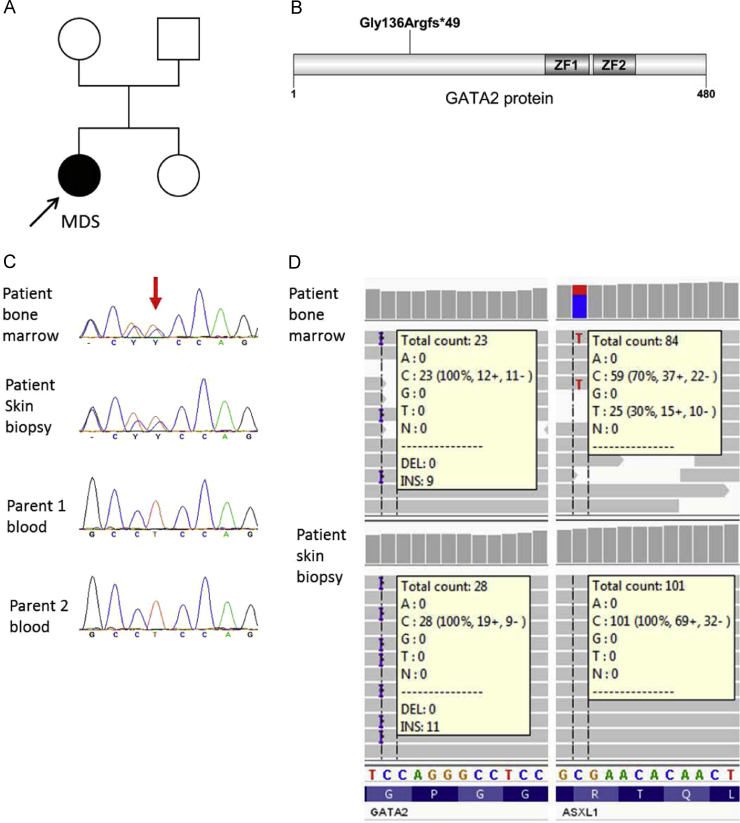
Clinical findings of symptomatic severe HPV infection, recurrent pneumonia and warts/condylomata in combination with the diagnosis of MDS RA and monocytopenia/lymphopenia, led to the suspicion of DCML syndrome. The family history revealed no individuals with similar symptoms. In particular, no other family members are known to be affected by any type of hematological malignancy or immunodeficiency (Fig. 2 A). Sequencing of material from both bone marrow and skin biopsy showed a heterozygous frameshift mutation in GATA2 (NM_001145661.1:c.404dup;Gly136Argfs*49) (Fig. 2, B–D). The patient's parents were tested but no GATA2 mutation could be detected (Fig. 2 C), suggesting that the patients disorder was caused by a de-novo mutation. To systematically screen for additional mutations, we performed exome sequencing of matched tumor (bone-marrow) and normal (skin biopsy) samples as described previously [7], [8]. Thereby, we detected a somatic ASXL1 mutation (NM_015338.4:c.2077 C>T; Arg693*) (Fig. 2 D).
Fig. 2.
Molecular diagnostic and genetic workup. (A) Pedigree of the affected family. Arrow indicates the index patient. (B) Germline mutation Gly136Argfs*49 mapped to the GATA2 protein structure using the software DOG1.0 [9]. (C) Genetic testing of the affected family by Sanger sequencing. Chromatograms of the index patient and her parents show a partial sequence of GATA2 exon 3 surrounding the cDNA position 404. (D) Exome sequence data from the index patient supporting the GATA2 germline mutation and the somatic ASXL1 mutation. Alignments of matched tumor (bone marrow) and normal (skin biopsy) samples from the index patient are shown using the Integrative Genomics Viewer (IGV) [10]. Read counts of reference and variant alleles at the altered positions are indicated for each sample.
Since no matched sibling donor was available, a search in the registry was initiated and a suitable unrelated donor with a HLA match 16/18 (difference in HLA-DPA- and HLA-DPB1-antigen), full blood group match and CMV match could be identified. After reduced conditioning with fludarabine 30 mg/m2 for 3 days and TBI 2 Gy, she underwent allo-HSCT with peripheral blood stem cells in June 2013. As GvHD prophylaxis, cyclosporin A and mycophenolate mofetil were given.
Already 4 weeks after allo-HSCT she achieved an almost normal differential WBC count with monocytes around 1×109, total lymphocytes of 0.6×109. A new lymphocyte profile showed an almost normal amount of NK-cells (0.15×109) and CD4 T-cells (0.18×109). She showed a full donor blood chimerism in October 2013.
Eight weeks after allo-HSCT, she experienced a severe menstrual bleeding accompanied by some chest discomfort and fatigue. Clinical investigation revealed a hemoglobin level of around 70g/l and discrete ECG changes. Subsequently, coronary angiography was performed showing a subtotal stenosis of the proximal left anterior descendens (LAD) coronary artery without any other signs of atherosclerosis. Percutaneous transluminal coronary angioplasty (PTCA) was done and antiplatelet therapy with clopidogrel was initiated. She underwent hystero-salpingectomy after antiplatelet therapy was terminated. The patient has neither cardiac risk factors nor a family history of heart disease.
At 4 months she developed a mild graft-versus host disease (GvHD grade 1) with skin rashes, mild eosinophilia and musculoskeletal pain, responding to an intermediate steroid dose. Around the same time, both warts and condylomata disappeared gradually.
3. Discussion
In this case report we describe a young woman that presented with a long history of condylomata and microcytic anemia due to a combination of MDS associated with the DCML syndrome and iron deficiency demonstrating that an overlap of clinical symptoms may complicate diagnosis in patients with GATA2 mutations. Genetic lesions in GATA2 that lead to Emberger syndrome seem to be affecting endothelial cells of the lymphatic system, but vascular problems have not been described in patients with GATA2 mutations, to our knowledge. Our patient suffered from a non-ST-elevation myocardial infarction (NSTEMI) caused by a stenosis in the LAD in the absence of cardiac risk factors or a family history of heart disease and is, thus, most likely triggered by anemia due to a massive menstrual bleeding aggravated by a uterine myoma. Some clinical findings may be associated with distinct type of mutation causing GATA2 haploinsufficiency. However, in two large patient cohorts published recently, diversity of phenotype in patients with GATA2 mutations was shown for the first time [4], [11]. 84% of the patients in this study met the diagnostic criteria for MDS whereas bone marrow findings in patients with GATA2 mutations seem to differ from those with typical MDS [4]. Instead, patients with GATA2 mutations present with a hypocellular bone marrow, increased reticulin fibrosis and atypical megakaryocytes in almost all cases. In addition cytogenetic abnormalities such as monosomy 7 or trisomy 8 are frequent [12], [13]. In the case presented here, repeated bone marrow biopsies showed rather discrete changes and considering the absence of cytogenetic aberrations, it was challenging to diagnose MDS. Nevertheless, exome sequencing revealed the presence of a somatic ASXL1 mutation. Myeloid transformation induced by acquired lesions of ASXL1 in patients with constitutional GATA2 mutations were previously reported [12], [13], [14]. This demonstrates that an early diagnosis and evaluation for allo-HSCT is crucial for patients with GATA2 mutations and genetic counseling should be offered to affected families.
References
- 1.Hsu A.P. Mutations in GATA2 are associated with the autosomal dominant and sporadic monocytopenia and mycobacterial infection (MonoMAC) syndrome. Blood. 2011;118(10):2653–2655. doi: 10.1182/blood-2011-05-356352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dickinson R.E. Exome sequencing identifies GATA-2 mutation as the cause of dendritic cell, monocyte, B and NK lymphoid deficiency. Blood. 2011;118(10):2656–2658. doi: 10.1182/blood-2011-06-360313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hahn C.N. Heritable GATA2 mutations associated with familial myelodysplastic syndrome and acute myeloid leukemia. Nat. Genet. 2011;43(10):1012–1017. doi: 10.1038/ng.913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spinner M.A. GATA2 deficiency: a protean disorder of hematopoiesis, lymphatics, and immunity. Blood. 2014;123(6):809–821. doi: 10.1182/blood-2013-07-515528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Holme H. Marked genetic heterogeneity in familial myelodysplasia/acute myeloid leukaemia. Br. J. Haematol. 2012;158(2):242–248. doi: 10.1111/j.1365-2141.2012.09136.x. [DOI] [PubMed] [Google Scholar]
- 6.Kazenwadel J. Loss-of-function germline GATA2 mutations in patients with MDS/AML or MonoMAC syndrome and primary lymphedema reveal a key role for GATA2 in the lymphatic vasculature. Blood. 2012;119(5):1283–1291. doi: 10.1182/blood-2011-08-374363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Opatz S. Exome sequencing identifies recurring FLT3 N676K mutations in core-binding factor leukemia. Blood. 2013;122(10):1761–1769. doi: 10.1182/blood-2013-01-476473. [DOI] [PubMed] [Google Scholar]
- 8.Greif P.A. GATA2 zinc finger 1 mutations associated with biallelic CEBPAmutations define a unique genetic entity of acute myeloid leukemia. Blood. 2012;120(2):395–403. doi: 10.1182/blood-2012-01-403220. [DOI] [PubMed] [Google Scholar]
- 9.Ren J. DOG 1.0: illustrator of protein domain structures. Cell. Res. 2009;19(2):271–273. doi: 10.1038/cr.2009.6. [DOI] [PubMed] [Google Scholar]
- 10.Thorvaldsdottir H., Robinson J.T., Mesirov J.P. Integrative Genomics Viewer (IGV): high-performance genomics data visualization and exploration. Brief Bioinform. 2013;14(2):178–192. doi: 10.1093/bib/bbs017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dickinson R.E. The evolution of cellular deficiency in GATA2 mutation. Blood. 2014;123(6):863–874. doi: 10.1182/blood-2013-07-517151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bodor C. Germ-line GATA2 p.THR354MET mutation in familial myelodysplastic syndrome with acquired monosomy 7 and ASXL1 mutation demonstrating rapid onset and poor survival. Haematologica. 2012;97(6):890–894. doi: 10.3324/haematol.2011.054361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.West R.R. Acquired ASXL1 mutations are common in patients with inherited GATA2 mutations and correlate with myeloid transformation. Haematologica. 2014;99(2):276–281. doi: 10.3324/haematol.2013.090217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Micol J.B., Abdel-Wahab O. Collaborating constitutive and somatic genetic events in myeloid malignancies: ASXL1 mutations in patients with germline GATA2 mutations. Haematologica. 2014;99(2):201–203. doi: 10.3324/haematol.2013.101303. [DOI] [PMC free article] [PubMed] [Google Scholar]