Abstract
Mesenteric lymphangiomas, which involve near total mesentery, are extremely rare. A mesenteric lymphangioma should be treated through excision because they can cause invasion of vital structures, bleeding, or infection. After excision of a huge mesenteric lymphangioma, internal herniation may occur through a large mesenteric defect leading to intestinal volvulus, obstruction, and other life-threatening circumstances. We report a case in which a biologic collagen implant (Permacol) was used for mesenteric defect repair after excision of a huge mesenteric lymphangioma. The implant did not cause any symptoms or complications during follow-up for 4 years. When encountering large defects of mesentery, closure with implant can be a feasible choice, and Permacol could be a possible implant for closing the defect.
Keywords: Mesenteric lymphangioma, Mesenteric defect, Repair material, Prostheses and implant, Permacol
INTRODUCTION
Lymphangiomas are usually located in the head and neck area as well as the abdominal wall, but rarely in the mesentery [1]. Although mesenteric lymphangiomas can occur at any age, they are present at birth in 65% of all patients and nearly 60% of all patients are diagnosed before the age of 5 years [2,3]. The incidence of mesenteric lymphangioma is about 1 in 20,000 pediatric hospital admissions in the United States [4]. Most mesenteric lymphangiomas are initially asymptomatic, but some patients complain of vague subjective symptoms, such as pain, nausea, vomiting, or alterations in bowel habits depending on the size and location of the lymphangiomas [3,4]. Lymphangiomas should be treated through complete resection because they can cause bleeding or infection as well as invasion of vital structures [3]. After excision of a mass that involves the whole mesentery, internal herniation is likely to occur through the skeletonized vessels. We used a biologic collagen implant (Permacol, Covidien, Norwak, USA) to repair the mesenteric defect after excision of a huge mesenteric lymphangioma and followed up for 4 years.
CASE REPORT
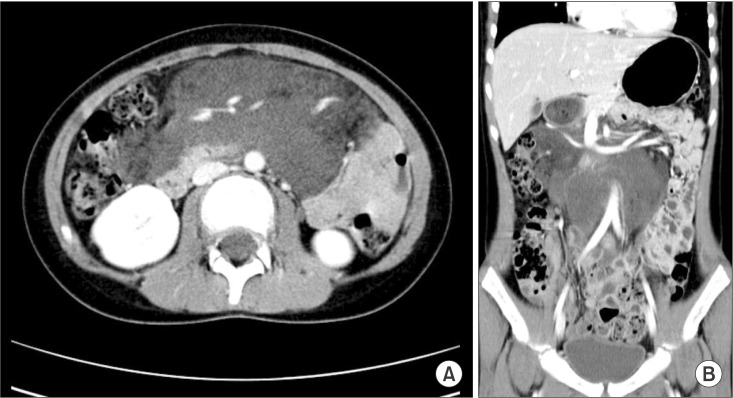
An 11-year-old girl was referred to Seoul National University Children's Hospital with pain in the right lower quadrant of the abdomen that began 2 months prior to admission. She did not have a specific past medical history, and did not report either fever or any other relevant gastrointestinal symptoms, such as anorexia or vomiting. On physical examination, the patient had mild tenderness in the right lower quadrant of the abdomen. A fixed mass was palpable around the periumbilical region. No other specific findings were noted in the laboratory tests, including complete blood counts, and C-reactive protein. CT revealed an infiltrative cystic mass in the mesentery measuring 10.5 cm × 8.7 cm × 7.5 cm, and that the small bowel was displaced laterally and inferiorly due to the mass (Fig. 1).
Fig. 1. Preoperative abdominal CT. (A) Axial view shows low attenuated mass measuring 10.5 cm × 8.7 cm × 7.5 cm in size without enhancement by contrast medium, which is displacing the small bowel. (B) Coronal view shows huge low-attenuated mass occupying the anterior abdominal cavity, traversing abdominal aorta and other mesenteric vessels.
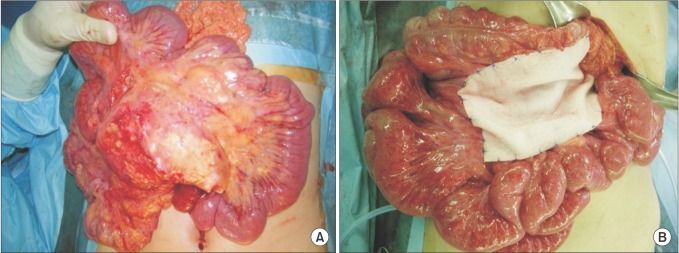
The radiological diagnoses included mesenteric lymphangioma, lipoblastoma, and neurogenic tumor. Exploratory laparotomy demonstrated a broad-based multiple cystic lymphangioma within the mesentery ranging from the Treitz ligament to the transverse colon (Fig. 2A). However, it did not involve the surrounding viscera. The lymphangioma was excised nearly completely saving mesenteric vessels by skeletonization. As a result, a very large-sized mesenteric defect from that of the jejunum to the transverse colon with centrally skeletonized vessels developed. Initially, we tried to close the defect without implant, but failed, because the intestine and vessels came to be angulated and lead to obstruction. The mesenteric defect was repaired with a Permacol (Fig. 2B). Histopathologic findings were consistent with mesenteric lymphangioma. On postoperative day 7, the chyle leak was developed through the drainage tube and was resolved by conservative management. The patient was discharged from the hospital on postoperative day 17 without other problems from the biomaterial implant.
Fig. 2. Intraoperative findings. (A) There are multiple cystic lymphangiomas within the small bowel mesentery. (B) Mesenteric defect was repaired with biologic implant.
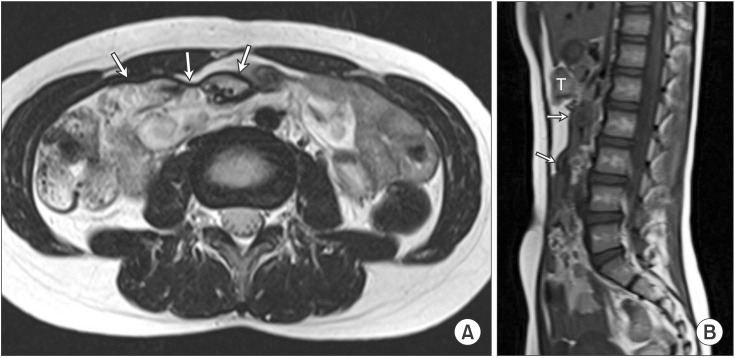
She was regularly checked with ultrasonography, CT, and MRI at our outpatient clinics. After 3 months, abdominal CT revealed a residual lymphangioma around the head of the pancreas and the portal vein. The implant did not cause any problems. At a recent follow-up, 4 years after operation, abdominal MRI did not showed any changes from 3 months postoperative status (Fig. 3). During the follow-up period, she has been doing well without complaint of any symptoms.
Fig. 3. Magnetic resonance findings after 4 years of follow-up revealed implant, line of low intensity at mesentery in both T1 sagittal (A), T2 axial (B) image. Arrows, implant; T, transverese colon.
DISCUSSION
A standard treatment of huge mesenteric lymphangioma has not yet been established due to its very low incidence. However, surgical excision is necessary because it invades adjacent organs and can cause infection or bleeding [3]. In this case, we performed surgical resection of the huge mesenteric lymphangioma because of abdominal pain and invasion to the adjacent organs.
As in our case, excision of a huge lymphangioma may create mesenteric defects of various sizes, which can cause internal herniations that result in intestinal volvulus and obstruction. Some authors suggested that patients with segmental mesenteric defects require intestinal fixation and resection of the affected intestine [5]. De la Cruz-Munoz et al. [6] reported that the incidence of internal hernia decrease through the closure of mesenteric defects. However, controversy exists regarding closure of the mesenteric defect in specific circumstances. Cabot et al. [7] reported that mesenteric defects are not associated with significant rates of relevant internal hernia in specific operations, such as laparoscopic right hemicolectotomy and laparoscopic Roux-en-Y gastric bypass.
The use of an implant for the empty space is another solution. There are two available materials for mesenteric repair including synthetic meshes and biologic collagen implants. Synthetic meshes, such as polyprophylene implants, are commonly used, but they have limited tissue-incorporation abilities as well as an increased risk of complications, such as adhesion, erosion, or fistula formation [8,9]. To overcome the shortcomings, attention has recently been focused on biological implants derived from allogenic or xenogenic sources [10]. Permacol is a sheet of porcine dermal collagen. Cross-links between collagen fibers give it its durability by preventing collagenase destruction. It gradually remodels human tissue while preserving its structural integrity. Moreover, porcine dermal implants induce minimal inflammation and adhesion even when they come into direct contact with viscera [8,9]. Although porcine dermal implants have a disadvantage of forming intra-abdominal abscess or sepsis in contaminated circumstances, they have widely been used for abdominal wall repair, chest wall repair, and reconstruction surgery and have proved to be stable [10]. In this case, Permacol also did not showed any complications for 4 years.
In summary, to avoid internal herniation through a large mesenteric defect, after excision of huge mesenteric lymphangiomas, closure with implant would be a good choice, and Permacol would be a possible implant for closing the defect. To the best of our knowledge, this is the first case on the use of Permacol for a huge mesenteric defect in children.
Footnotes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Okazaki T, Iwatani S, Yanai T, Kobayashi H, Kato Y, Marusasa T, et al. Treatment of lymphangioma in children: our experience of 128 cases. J Pediatr Surg. 2007;42:386–389. doi: 10.1016/j.jpedsurg.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 2.Caro PA, Mahboubi S, Faerber EN. Computed tomography in the diagnosis of lymphangiomas in infants and children. Clin Imaging. 1991;15:41–46. doi: 10.1016/0899-7071(91)90047-y. [DOI] [PubMed] [Google Scholar]
- 3.Losanoff JE, Richman BW, El-Sherif A, Rider KD, Jones JW. Mesenteric cystic lymphangioma. J Am Coll Surg. 2003;196:598–603. doi: 10.1016/S1072-7515(02)01755-6. [DOI] [PubMed] [Google Scholar]
- 4.Takiff H, Calabria R, Yin L, Stabile BE. Mesenteric cysts and intra-abdominal cystic lymphangiomas. Arch Surg. 1985;120:1266–1269. doi: 10.1001/archsurg.1985.01390350048010. [DOI] [PubMed] [Google Scholar]
- 5.Black PR, Mueller D, Crow J, Morris RC, Husain AN. Mesenteric defects as a cause of intestinal volvulus without malrotation and as the possible primary etiology of intestinal atresia. J Pediatr Surg. 1994;29:1339–1343. doi: 10.1016/0022-3468(94)90111-2. [DOI] [PubMed] [Google Scholar]
- 6.de la Cruz-Munoz N, Cabrera JC, Cuesta M, Hartnett S, Rojas R. Closure of mesenteric defect can lead to decrease in internal hernias after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2011;7:176–180. doi: 10.1016/j.soard.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 7.Cabot JC, Lee SA, Yoo J, Nasar A, Whelan RL, Feingold DL. Long-term consequences of not closing the mesenteric defect after laparoscopic right colectomy. Dis Colon Rectum. 2010;53:289–292. doi: 10.1007/DCR.0b013e3181c75f48. [DOI] [PubMed] [Google Scholar]
- 8.Zheng F, Lin Y, Verbeken E, Claerhout F, Fastrez M, De Ridder D, et al. Host response after reconstruction of abdominal wall defects with porcine dermal collagen in a rat model. Am J Obstet Gynecol. 2004;191:1961–1970. doi: 10.1016/j.ajog.2004.01.091. [DOI] [PubMed] [Google Scholar]
- 9.Kaleya RN. Evaluation of implant/host tissue interactions following intraperitoneal implantation of porcine dermal collagen prosthesis in the rat. Hernia. 2005;9:269–276. doi: 10.1007/s10029-005-0003-0. [DOI] [PubMed] [Google Scholar]
- 10.Pomahac B, Aflaki P. Use of a non-crosslinked porcine dermal scaffold in abdominal wall reconstruction. Am J Surg. 2010;199:22–27. doi: 10.1016/j.amjsurg.2008.12.033. [DOI] [PubMed] [Google Scholar]