Abstract
Purpose. To present a novel protocol for alveolar bone regeneration in parallel to early implant placement. Methods. 497 patients in need of extraction and early implant placement with simultaneous bone augmentation were treated in a period of 10 years. In all patients the same specific method was followed and grafting was performed utilizing in situ hardening fully resorbable alloplastic grafting materials consisting of β-tricalcium phosphate and calcium sulfate. The protocol involved atraumatic extraction, implant placement after 4 weeks with simultaneous bone augmentation, and loading of the implant 12 weeks after placement and grafting. Follow-up periods ranged from 6 months to 10 years (mean of 4 years). Results. A total of 601 postextraction sites were rehabilitated in 497 patients utilizing the novel protocol. Three implants failed before loading and three implants failed one year after loading, leaving an overall survival rate of 99.0%. Conclusions. This standardized protocol allows successful long-term functional results regarding alveolar bone regeneration and implant rehabilitation. The concept of placing the implant 4 weeks after extraction, augmenting the bone around the implant utilizing fully resorbable, biomechanically stable, alloplastic materials, and loading the implant at 12 weeks seems to offer advantages when compared with traditional treatment modalities.
1. Introduction
According to the Branemark original protocol, implant placement was carried out 6 to 8 months after tooth extraction followed by a 3- to 6-month stress-free osseointegration period resulting in a long overall treatment time [1]. In an attempt to shorten the time frame between extraction and prosthetic delivery and to reduce cost, patient discomfort, and the number of surgical interventions, the immediate placement of implants at the time of tooth extraction has been proposed [2]. Other potential advantages with immediate implants are that the amount of bone loss at the extraction site might be reduced and optimal soft tissue aesthetics may be achieved [3]. On the other hand, there are some disadvantages with immediate implants such as the enhanced risk of infection and the lack of soft tissue closure [4, 5]. In order to overcome these potential problems early placement of implants has been proposed [2]. In this technique the clinicians wait 2 to 8 weeks before placing the implant to achieve some soft tissue healing and decrease the risk of infections [5].
The short-term survival rate of implant placement appears similar between immediate, early, and late approaches. However, at present there is little data on the success of immediate and early placement compared to late placement [2, 3, 5]. A few reviews evaluating the efficacy of immediate or early implants have been published over the years, but so far evidence is inconclusive [4–11].
With immediate or early implants it is possible that one or more bony walls of the postextraction socket are either partly or completely missing due to the preexisting inflammatory processes or damaged as a complication of the tooth extraction procedure. As a result, a portion of the implants could remain exposed due to hard tissue defect. Sockets with dehiscence defects may lack the potential for complete bone regeneration, and the risk of long-term complications may be increased with immediate or early implants placed at these sites [5]. However, several reports have shown that bone regeneration may be achieved in defective sites adjacent to immediate or early implants using a variety of bone augmentation techniques, such as autogenous bone grafts, bone substitutes, and guided bone regeneration with resorbable or nonresorbable barriers [4]. However, there is no enough reliable evidence supporting or refuting the need for augmentation procedures in parallel to immediate or early implant placement or whether any of the augmentation techniques is superior to the others [4, 5, 12].
When regenerating lost alveolar bone with the use of grafting materials, an important concern is the presence of residual particles, which might interfere with normal healing and bone-to-implant contact. The quality of the regenerated bone around immediate or early implants might be critical in determining the long-term function and stability of dental implants and the peri-implant tissues [13]. Beta-tricalcium phosphate (β-TCP) has a compressive strength similar to that of cancellous bone and undergoes resorption over a 6–18-month period being completely replaced by newly formed vital bone [14–18]. However, few studies to date have evaluated the long-term outcome of using β-TCP as grafting material simultaneously with implant placement into extraction sites [14, 19].
It would be of great benefit to investigate if completely resorbable in situ hardening alloplastic grafting materials could be used, without the need of membrane coverage, during early implant placement in a successful and predictable way. The purpose of the present study was therefore to assess the long-term survival rate of implants early placed into defective sockets with simultaneous bone grafting with in situ hardening β-TCP, following a standardized protocol.
2. Patients and Methods
This study reports a series of 497 patients treated according to the novel protocol, from August 2004 to July 2014. Patients were referred for consultation and treatment of nonsalvageable teeth due to root fractures, advanced caries, trauma, periodontitis, or failed endodontic treatment. All patients were treated in 2 private implantology clinics by 2 different clinicians. In the present study, only cases with defective buccal bone wall and need for bone augmentation in parallel to early implant placement were included. Patients with intact 4-wall postextraction sockets, with uncontrolled diabetes, alcoholics, and drug abusers were excluded, but smokers were included. All patients signed a letter of consent for the use of the alloplastic bone graft substitutes and implant placement.
After thorough clinical examination, periapical radiographs were taken. In 48% of the cases where additional information was required, a CBCT was prescribed.
In all cases the same standardized methodology was followed: Firstly, after local anaesthesia, teeth were “atraumatically” extracted without raising a flap. Extractions were facilitated by the use of periotomes and gentle elevation. Attention was given not to damage the surrounding soft and hard tissues. In cases of multirooted teeth, teeth were sectioned and removed in pieces. After extraction, the sockets were thoroughly curetted and debrided of inflammatory tissue, followed by rinsing with sterile saline. Postextraction sockets were allowed to heal by secondary intention.
After 4 weeks a site-specific full thickness flap was raised buccally using vertical releasing incisions, without including the papillae of the adjacent teeth. After flap elevation all granulation tissue was removed from the site and a tapered implant (Dio, Dio Co., Busan, Korea) was placed in the optimal position. After placing the cover screw, the site was augmented utilizing an in situ hardening resorbable alloplastic bone grafting material.
Fortoss Vital (Biocomposites, Staffordshire, UK) is a biphasic alloplastic bone graft consisting of β-TCP in a calcium sulfate (CS) matrix. This graft material has an increased negative isoelectric charge (Zeta Potential Charge [ZPC]) in an aqueous solution, which has been shown to upregulate the host response by attracting positively charged host bone morphogenetic proteins to the site. These in turn result in the increased presence of osteoblasts to the site for improved early bone regeneration. Fortoss Vital acts as a scaffold for bony proliferation as it is slowly resorbed by osteoclastic activity and substituted by living bone cells that grow directly in contact with the mineral. The product forms a simple to use, moldable cohesive paste that sets to form a hard, but resorbable, osteoconductive bone graft material.
Ethoss (Regenamed Ltd., London, UK) is a biphasic alloplastic grafting material consisting of β-TCP (65%) and CS (35%). When mixed with sterile saline, the material forms an easily handling moldable mass that hardens in situ.
No barrier membranes were used. The mucoperiosteal flap was repositioned and sutured without tension with resorbable 4-0 sutures (Vicryl, Ethicon, Johnson & Johnson, Somerville, NJ, USA). The sutures were removed after a 7-day healing period.
After 10 weeks a similar site-specific full-thickness flap was raised to access the cover screw. In 60% of the cases the stability of the implants was evaluated by resonance frequency analysis (Osstell ISQ, Gothenburg, Sweden). A healing abutment was placed and the flap was then sutured using 4-0 sutures (Vicryl Rapide, Ethicon, Johnson & Johnson, Somerville, NJ, USA). Lastly after allowing the soft tissue to mature for 2 weeks the final titanium abutment was placed and a cemented metal-ceramic restoration was fabricated.
3. Results
This retrospective study of 497 patients included 243 females (48.9%) and 254 males (51.1%) with mean age of 54.24 years (range 23 to 91). In total 601 implants were early placed in different locations according to the novel protocol, and, of the 601 sites, 471 (78.4%) were grafted with Fortoss Vital, and 130 (21.6%) were grafted with Ethoss. The implant distribution, in accordance with the grafting material used, is shown in Figures 1 and 2.
Figure 1.
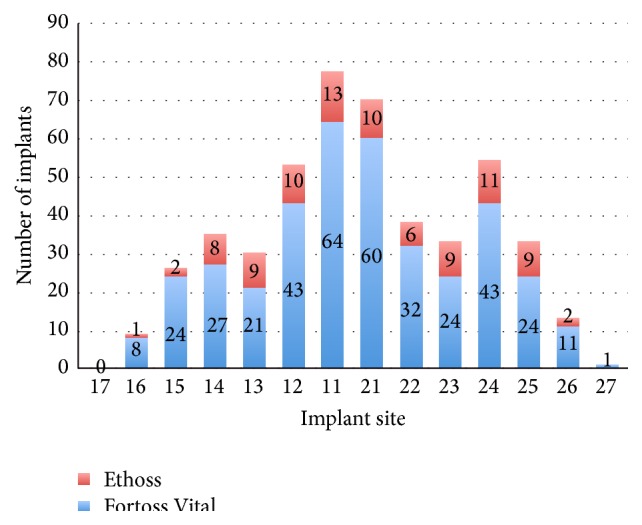
Implant distribution and grafting material used in maxilla.
Figure 2.
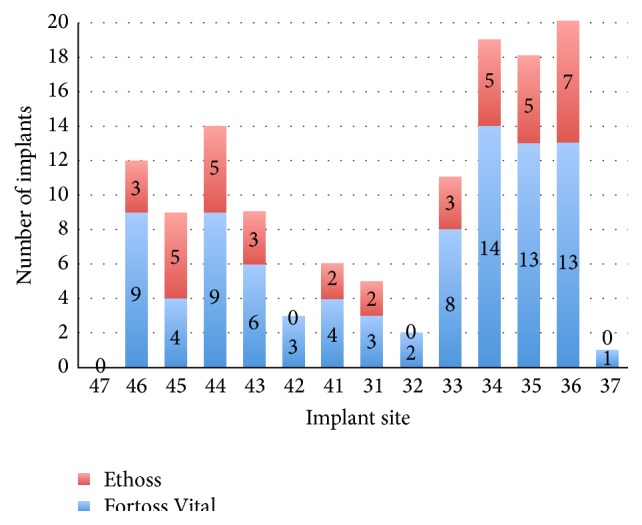
Implant distribution and grafting material used in mandible.
Of the 601 implants placed, 3 were lost before loading (2 grafted with Fortoss Vital and 1 with Ethoss) due to infection and granulation tissue development; and 3 implants (2 grafted with Fortoss Vital and 1 with Ethoss) were lost 1 year after loading, corresponding to an overall success rate of 99.0%.
Apart from the 6 lost implants, none of the patients experienced postoperative complications.
At reentry, 10 weeks after implant placement and grafting, the sites were filled with newly formed bone. Remnants of the grafting materials could be identified, be embedded, and be in continuity with the newly formed bone. In many cases, the regenerated bone was completely or partially covering the implant cover screw. Out of the 595 successful cases only 5 (3 grafted with Fortoss Vital and 2 grafted with Ethoss) needed minor additional grafting buccally with the same material in order to cover still exposed cervical implant threads, without compromising the final result. At this time point all implants were firmly integrated and ISQ measurements, when available, showed high (70–84) values.
All successful cases were loaded with cemented crowns and the pleasing esthetic outcomes were noted.
Follow-up radiological examinations with periapical X-rays (follow-up periods ranged from 6 months to 10 years, mean of 4 years) demonstrated stable peri-implant hard tissues.
Figures 3 –6 show 4 cases treated according to the proposed protocol.
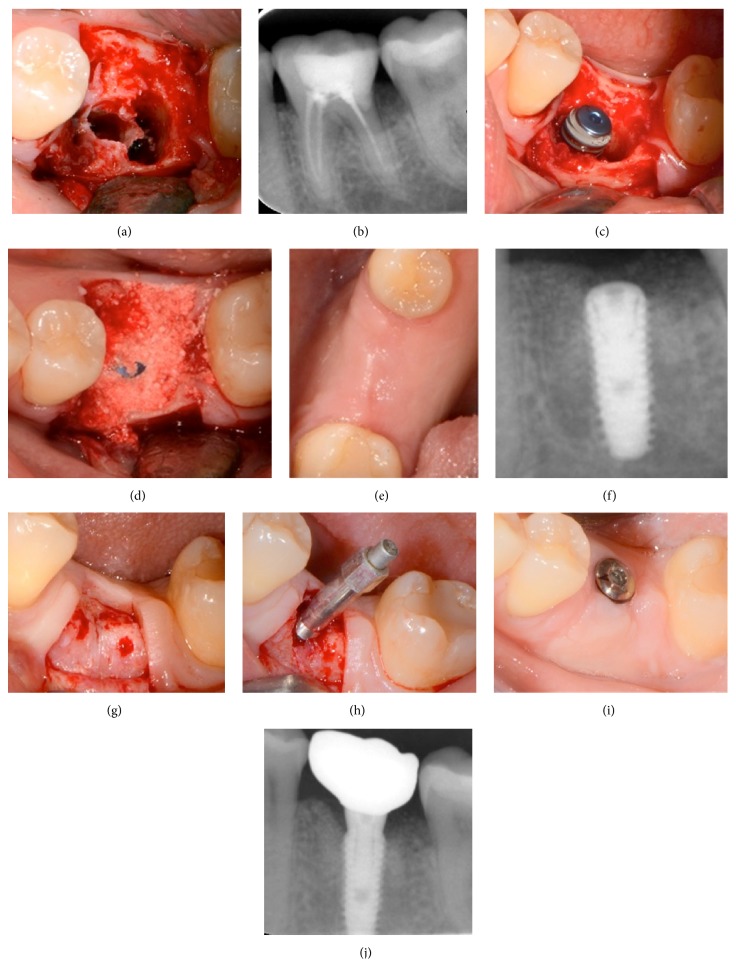
Figure 3.
Case 1: a 47-year-old woman with crown and root fracture in the left mandibular first molar. (a) Clinical view of the site after thorough debridement of the socket. (b) Periapical X-ray of the nonrestorable tooth. (c) Implant placement at the correct 3D positioning. ISQ reading was 48. (d) Grafting with β-TCP/CS (Ethoss). (e) Clinical view after 10 weeks. (f) X-ray 10 weeks after implant placement and grafting showing the consolidation of the grafting material around the implant and new bone formation over the implant head and towards the adjacent interproximal heights of bone. (g) At reentry the site is filled with regenerated bone. Note the head of the implant covered by newly formed bone. (h) After removing the supernatant newly formed bone with a round burr implant stability is assessed (ISQ measurement: 78) revealing a significant increase through the 10-week healing period. (i) Maturation of the soft tissues 2 weeks after placement of the healing abutment. (j) X-ray 9 months after loading.
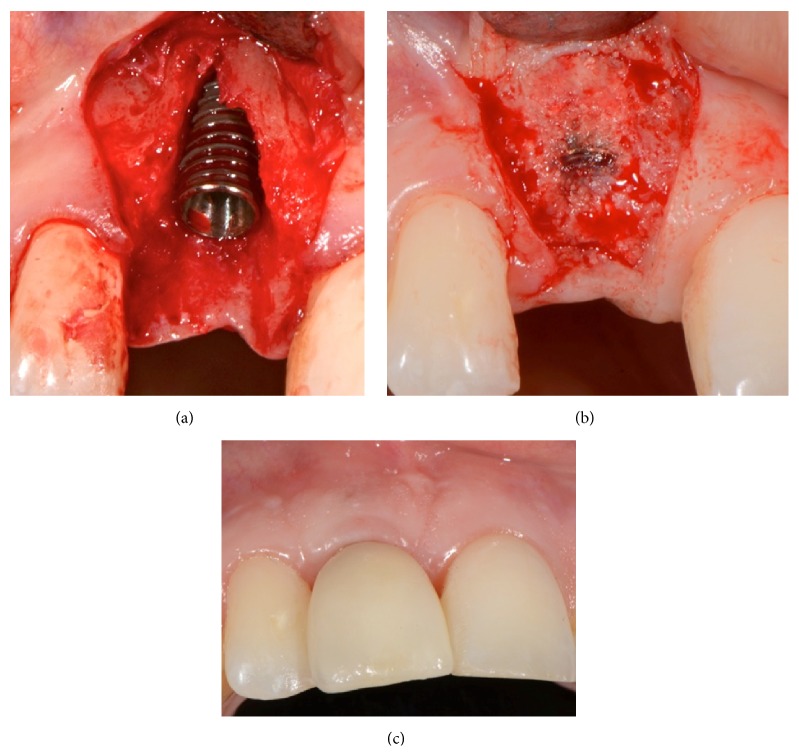
Figure 4.
Case 2: a 28-year-old woman with root fracture in the maxillary right central incisor. (a) Implant placed at the optimum 3D positioning leaving a buccal dehiscence. (b) Reentry after 10 weeks revealing complete bone regeneration of the site. The head of the implant is partially covered by newly formed bone and the ridge is also significantly augmented laterally. ISQ reading was 75. (c) Six months after loading, excellent preservation of the buccal profile.
Figure 5.
Case 3: a 62-year-old male with root fracture in the maxillary left second premolar. (a) Implant placed at the optimum 3D positioning with low initial stability, leaving a buccal dehiscence. (b) Reentry after 10 weeks showing excellent bone regeneration of the site. ISQ reading was 76.
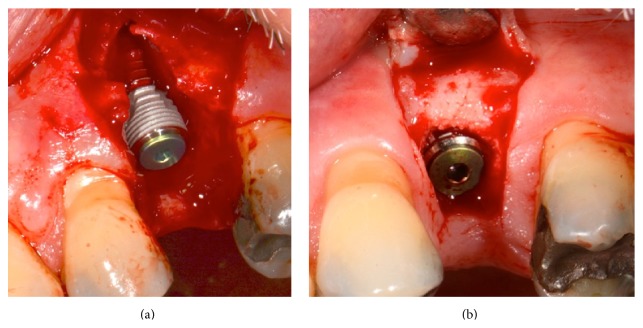
Figure 6.

Seven-year follow-up clinical picture of a maxillary left canine case treated according to the protocol and grafted with Fortoss Vital.
4. Discussion
This report proposes a protocol for early implant placement and simultaneous bone augmentation in sites with dehiscence-type bone defects.
A potential advantage with early implantation compared to immediate placement seems to be the decreased risk of infections and associated implant failures. The findings of the present study support this hypothesis as from the 601 placed implants 4 weeks after extraction only 3 (0.5%) were lost due to infection during the healing period. The overall success rate in this study was 99.0%, higher than the success rate reported in the literature with regard to survival percentages ranging from 95% to 97.5% [7, 8, 20–24].
Although there is currently too little evidence to draw definitive conclusions [5], the literature suggests that the placement of dental implants at an early timing after tooth extraction may also offer advantages in terms of soft and hard tissue preservation, when compared with immediate or delayed protocols [7, 12, 20–26]. The survival rates presented in this case series study show stable functional outcomes in a follow-up period up to 10 years (mean of 4 years). In 595 cases the contour augmentation technique described in this protocol was able to regenerate the hard tissues around the implants, as observed at the 10-week postop reentry, and allow for long-term function and clinical survival of the implants.
The concept of bone augmentation with the use of xenogeneic bone graft and a resorbable barrier membrane in conjunction with early implant placement was carried out in several clinical studies with successful results [23, 24, 26, 27].
In contrast to the above augmentation protocols, in the present study a different rationale for bone augmentation in parallel with early implant placement was followed. In all cases the dehiscence-type bone defects were treated with resorbable biphasic alloplastic bone grafting materials composed of β-TCP and CS and no barrier membranes were used. Significant bone formation at the buccal aspect of the implants was demonstrated at reentry after 10 weeks and only in 0.8% of the cases additional grafting was needed in order to cover still exposed cervical implant threads. It seems that the biomechanical properties of the grafting materials used in this study fulfilled the main principles of successful bone regeneration of the alveolar bone, that is, exclusion of gingival tissue from the regenerating site and maintenance of a stable bacterial-free closed compartment [28]. The CS component of the grafting materials used is pyrogen-free and bacteriostatic, creating a nanoporous cell-occlusive membrane that prevents the early stage invasion of unwanted soft tissue cells and when mixed with other grafting materials enhances graft containment, making the mixture more stable and pressure resistant [29–31]. Adding CS to β-TCP produces an in situ hardening grafting material that binds directly to the host bone, maintains the space and shape of the grafted site, and acts as a stable osteoconductive scaffold [32, 33]. The improved stability throughout the graft material seems to further improve the quality of the bone to be regenerated due to reduced micromotion of the material, which may lead to mesenchymal differentiation to fibroblasts instead of osteoblasts [34]. It is known that micromovements between bone and any implanted grafted material prevent bone formation, resulting in the development of fibrous tissue [35]. A possible problem with particulate grafts like deproteinized bovine bone mineral might be the lack of stability of the grafting material at the recipient site. In such cases a resorbable membrane is needed to cover and stabilize the particulate grafting material [36].
In the present study the β-TCP/CS bone grafts were covered only with the mucoperiosteal flap. The 4-week healing period after the extraction enabled the production of adequate newly formed keratinized tissue, achieving tension-free primary closure and maintenance throughout the healing and regeneration phases. The no need for a barrier membrane in the proposed protocol significantly reduced the surgical time and cost and may be attributed to enhanced bone regeneration as the periosteum was not isolated from the grafted site. Periosteum has been shown to play a pivotal role in bone graft incorporation, healing, and remodeling, as it contains multipotent mesenchymal stem cells that are capable of differentiating into bone and cartilage and provides a source of blood vessels and growth factors [37, 38].
The profound bone regeneration shown after 10 weeks in the present study may also be explained by the biological properties that characterize alloplastic materials used. It has been found that β-TCP when covered with vascularized periosteum enhances osteoconduction and osteoblastic activity while resorbing simultaneously with the formation of new bone. There is also ongoing important evidence that TCP possesses high osteoinductive potential [14, 39–42]. Moreover, experimental research has shown that the addition of the resorbable CS to the graft significantly accelerates osteogenesis and increases calcification and the quantity of new bone in a shorter period of time [33, 43]. It is also important that the most intensive osteogenic activity during healing of extraction sites takes place between 4 and 8 weeks after extraction. Placement of the implant and the grafting material at 4 weeks after atraumatic extraction takes advantage of this enhanced host bone-healing environment [14, 44]. Also, it has been found that implant insertion increases bone metabolic activity at the site [45], further contributing to enhanced bone regeneration. Although a histological evaluation of the regenerated hard tissue was not performed in this study, it can be assumed that the bone defects around the implants have been repaired and finally filled with high quality vital bone free of residual graft particles.
There are concerns that bone grafting materials like β-TCP and CS that are fully resorbed in a short timeframe may contribute to site collapse [15, 16, 33, 42, 46]. Early loading of the implants after 12 weeks, as proposed in the present protocol, may further enhance the metabolic activity and trigger the remodelling of the regenerated labial bone [44]. Assuming that the newly formed hard tissue at the facial aspect of the implant is vital bone with no residual graft particles, it can be concluded that it adapted successfully to the transmitted occlusal forces according to Wolff's law, became stronger to resist to the type of loading, and thus maintained long-term the bone function [47, 48].
5. Conclusions
The results of this study suggest that this novel standardized protocol allows successful and predictable long-term successful functional outcomes regarding alveolar bone regeneration and implant rehabilitation. The concept of placing the implant 4 weeks after extraction, augmenting the bone around the implant utilizing only fully resorbable, biomechanical stable, alloplastic β-TCP/CS materials, and loading the implant at 12 weeks seems to offer advantages when compared with traditional treatment modalities. Additional studies are needed in order to confirm the present findings.
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- 1.Branemark P.-I. Osseointegration and its experimental background. The Journal of Prosthetic Dentistry. 1983;50(3):399–410. doi: 10.1016/s0022-3913(83)80101-2. [DOI] [PubMed] [Google Scholar]
- 2.Koh R. U., Rudek I., Wang H.-L. Immediate implant placement: positives and negatives. Implant Dentistry. 2010;19(2):98–108. doi: 10.1097/id.0b013e3181d47eaf. [DOI] [PubMed] [Google Scholar]
- 3.Jofre J., Valenzuela D., Quintana P., Asenjo-Lobos C. Protocol for immediate implant replacement of infected teeth. Implant Dentistry. 2012;21(4):287–294. doi: 10.1097/id.0b013e31825cbcf8. [DOI] [PubMed] [Google Scholar]
- 4.Chen S. T., Wilson T. G., Jr., Hämmerle C. H. F. Immediate or early placement of implants following tooth extraction: review of biologic basis, clinical procedures, and outcomes. The International Journal of Oral & Maxillofacial Implants. 2004;19(19):12–25. [PubMed] [Google Scholar]
- 5.Esposito M., Grusovin M. G., Polyzos I. P., Felice P., Worthington H. V. Timing of implant placement after tooth extraction: immediate, immediate-delayed or delayed implants? A Cochrane systematic review. European Journal of Oral Implantology. 2010;3(3):189–205. [PubMed] [Google Scholar]
- 6.Fugazzotto P. A. Treatment options following single-rooted tooth removal: a literature review and proposed hierarchy of treatment selection. Journal of Periodontology. 2005;76(5):821–831. doi: 10.1902/jop.2005.76.5.821. [DOI] [PubMed] [Google Scholar]
- 7.Schropp L., Isidor F. Timing of implant placement relative to tooth extraction. Journal of Oral Rehabilitation. 2008;35(supplement 1):33–43. doi: 10.1111/j.1365-2842.2007.01827.x. [DOI] [PubMed] [Google Scholar]
- 8.Rieder D., Eggert J., Krafft T., Weber H.-P., Wichmann M. G., Heckmann S. M. Impact of placement and restoration timing on single-implant esthetic outcome—a randomized clinical trial. Clinical Oral Implants Research. 2014 doi: 10.1111/clr.12539. [DOI] [PubMed] [Google Scholar]
- 9.Chen S. T., Buser D. Esthetic outcomes following immediate and early implant placement in the anterior maxilla—a systematic review. The International Journal of Oral & Maxillofacial Implants. 2014;29, supplement:186–215. doi: 10.11607/jomi.2014suppl.g3.3. [DOI] [PubMed] [Google Scholar]
- 10.Knoernschild K. L. Early survival of single-tooth implants in the esthetic zone may be predictable despite timing of implant placement or loading. Journal of Evidence-Based Dental Practice. 2010;10(1):52–55. doi: 10.1016/j.jebdp.2009.11.027. [DOI] [PubMed] [Google Scholar]
- 11.Hof M., Pommer B., Ambros H., Jesch P., Vogl S., Zechner W. Does timing of implant placement affect implant therapy outcome in the aesthetic zone? A clinical, radiological, aesthetic, and patient-based evaluation. Clinical Implant Dentistry and Related Research. 2014 doi: 10.1111/cid.12212. [DOI] [PubMed] [Google Scholar]
- 12.Schropp L., Kostopoulos L., Wenzel A. Bone healing following immediate versus delayed placement of titanium implants into extraction sockets: a prospective clinical study. The International Journal of Oral & Maxillofacial Implants. 2003;18(2):189–199. [PubMed] [Google Scholar]
- 13.Chan H.-L., Lin G.-H., Fu J.-H., Wang H.-L. Alterations in bone quality after socket preservation with grafting materials: a systematic review. The International Journal of Oral & Maxillofacial Implants. 2013;28(3):710–720. doi: 10.11607/jomi.2913. [DOI] [PubMed] [Google Scholar]
- 14.Harel N., Moses O., Palti A., Ormianer Z. Long-term results of implants immediately placed into extraction sockets grafted with β-tricalcium phosphate: a retrospective study. Journal of Oral and Maxillofacial Surgery. 2013;71(2):e63–e68. doi: 10.1016/j.joms.2012.09.022. [DOI] [PubMed] [Google Scholar]
- 15.Palti A., Hoch T. A concept for the treatment of various dental bone defects. Implant Dentistry. 2002;11(1):73–78. doi: 10.1097/00008505-200201000-00017. [DOI] [PubMed] [Google Scholar]
- 16.Artzi Z., Weinreb M., Givol N., et al. Biomaterial resorption rate and healing site morphology of inorganic bovine bone and beta-tricalcium phosphate in the canine: a 24-month longitudinal histologic study and morphometric analysis. The International Journal of Oral & Maxillofacial Implants. 2004;19(3):357–368. [PubMed] [Google Scholar]
- 17.Trisi P., Rao W., Rebaudi A., Fiore P. Histologic effect of pure-phase beta-tricalcium phosphate on bone regeneration in human artificial jawbone defects. International Journal of Periodontics and Restorative Dentistry. 2003;23(1):69–78. [PubMed] [Google Scholar]
- 18.Nair P. N., Luder H.-U., Maspero F. A., Fischer J. H., Schug J. Biocompatibility of b-tricalcium phosphate root replicas in porcine tooth extraction sockets—a correlative histological, ultrastructural, and X-ray microanalytical pilot study. Journal of Biomaterials Applications. 2006;20(4):307–324. doi: 10.1177/0885328206054167. [DOI] [PubMed] [Google Scholar]
- 19.Ormianer Z., Palti A., Shifman A. Survival of immediately loaded dental implants in deficient alveolar bone sites augmented with β-tricalcium phosphate. Implant Dentistry. 2006;15(4):395–403. doi: 10.1097/01.id.0000239316.82325.8c. [DOI] [PubMed] [Google Scholar]
- 20.Schropp L., Isidor F., Kostopoulos L., Wenzel A. Interproximal papilla levels following early versus delayed placement of single-tooth implants: a controlled clinical trial. The International Journal of Oral & Maxillofacial Implants. 2005;20(5):753–761. [PubMed] [Google Scholar]
- 21.Schropp L., Wenzel A., Kostopoulos L., Karring T. Bone healing and soft tissue contour changes following single-tooth extraction: a clinical and radiographic 12-month prospective study. International Journal of Periodontics and Restorative Dentistry. 2003;23(4):313–323. [PubMed] [Google Scholar]
- 22.Schropp L., Kostopoulos L., Wenzel A., Isidor F. Clinical and radiographic performance of delayed-immediate single-tooth implant placement associated with peri-implant bone defects. A 2-year prospective, controlled, randomized follow-up report. Journal of Clinical Periodontology. 2005;32(5):480–487. doi: 10.1111/j.1600-051x.2005.00699.x. [DOI] [PubMed] [Google Scholar]
- 23.Nemcovsky C. E., Artzi Z., Moses O., Geernter I. Healing of dehiscence defects at delayed-immediate implant sites primarily closed by a rotated palatal flap following extraction. The International Journal of Oral & Maxillofacial Implants. 2000;15(4):550–558. [PubMed] [Google Scholar]
- 24.Nemcovsky C. E., Artzi Z. Comparative study of buccal dehiscence defects in immediate, delayed, and late maxillary implant placement with collagen membranes: clinical healing between placement and second-stage surgery. Journal of Periodontology. 2002;73(7):754–761. doi: 10.1902/jop.2002.73.7.754. [DOI] [PubMed] [Google Scholar]
- 25.Sanz I., Garcia-Gargallo M., Herrera D., Martin C., Figuero E., Sanz M. Surgical protocols for early implant placement in post-extraction sockets: a systematic review. Clinical Oral Implants Research. 2012;23(5):67–79. doi: 10.1111/j.1600-0501.2011.02339.x. [DOI] [PubMed] [Google Scholar]
- 26.Buser D., Chappuis V., Kuchler U., et al. Long-term stability of early implant placement with contour augmentation. Journal of Dental Research. 2013;92(12, supplement):176S–182S. doi: 10.1177/0022034513504949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buser D., Chappuis V., Bornstein M. M., Wittneben J.-G., Frei M., Belser U. C. Long-term stability of contour augmentation with early implant placement following single tooth extraction in the esthetic zone: a prospective, cross-sectional study in 41 patients with a 5-to 9-year follow-up. Journal of Periodontology. 2013;84(11):1517–1527. doi: 10.1902/jop.2013.120635. [DOI] [PubMed] [Google Scholar]
- 28.Moses O., Pitaru S., Artzi Z., Nemcovsky C. E. Healing of dehiscence-type defects in implants placed together with different barrier membranes: a comparative clinical study. Clinical Oral Implants Research. 2005;16(2):210–219. doi: 10.1111/j.1600-0501.2004.01100.x. [DOI] [PubMed] [Google Scholar]
- 29.Eleftheriadis E., Leventis M. D., Tosios K. I., et al. Osteogenic activity of β-tricalcium phosphate in a hydroxyl sulphate matrix and demineralized bone matrix: a histological study in rabbit mandible. Journal of Oral Science. 2010;52(3):377–384. doi: 10.2334/josnusd.52.377. [DOI] [PubMed] [Google Scholar]
- 30.Horowitz R. A., Rohrer M. D., Prasad H. S., Tovar N., Mazor Z. Enhancing extraction socket therapy with a biphasic calcium sulfate. Compendium of Continuing Education in Dentistry. 2012;33(6):420–428. [PubMed] [Google Scholar]
- 31.Smeets R., Kolk A., Gerressen M., et al. A new biphasic osteoinductive calcium composite material with a negative Zeta potential for bone augmentation. Head & Face Medicine. 2009;5(1, article 13) doi: 10.1186/1746-160x-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Podaropoulos L., Veis A. A., Papadimitriou S., Alexandridis C., Kalyvas D. Bone regeneration using β-tricalcium phosphate in a calcium sulfate matrix. The Journal of Oral Implantology. 2009;35(1):28–36. doi: 10.1563/1548-1336-35.1.28. [DOI] [PubMed] [Google Scholar]
- 33.Al Ruhaimi K. A. Effect of adding resorbable calcium sulfate to grafting materials on early bone regeneration in osseous defects in rabbits. International Journal of Oral and Maxillofacial Implants. 2000;15(6):859–864. [PubMed] [Google Scholar]
- 34.Dimitriou R., Mataliotakis G. I., Calori G. M., Giannoudis P. V. The role of barrier membranes for guided bone regeneration and restoration of large bone defects: current experimental and clinical evidence. BMC Medicine. 2012;10(1, article 81) doi: 10.1186/1741-7015-10-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Buser D., Dahlin C., Schenk R. K. Guided Bone Regeneration in Implant Dentistry. London, UK: Quintessence Publishing; 1995. [Google Scholar]
- 36.Amano Y., Ota M., Sekiguchi K., Shibukawa Y., Yamada S. Evaluation of a poly-l-lactic acid membrane and membrane fixing pin for guided tissue regeneration on bone defects in dogs. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 2004;97(2):155–163. doi: 10.1016/j.tripleo.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 37.Elshahat A., Inoue N., Marti G., Safe I., Manson P., Vanderkolk C. Guided bone regeneration at the donor site of iliac bone grafts for future use as autogenous grafts. Plastic and Reconstructive Surgery. 2005;116(4):1068–1075. doi: 10.1097/01.prs.0000178783.44190.ec. [DOI] [PubMed] [Google Scholar]
- 38.Zhang X., Awad H. A., O'Keefe R. J., Guldberg R. E., Schwarz E. M. A perspective: engineering periosteum for structural bone graft healing. Clinical Orthopaedics and Related Research. 2008;466(8):1777–1787. doi: 10.1007/s11999-008-0312-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saito M., Shimizu H., Beppu M., Takagi M. The role of β-tricalcium phosphate in vascularized periosteum. Journal of Orthopaedic Science. 2000;5(3):275–282. doi: 10.1007/s007760050163. [DOI] [PubMed] [Google Scholar]
- 40.Yuan H., Fernandes H., Habibovic P., et al. Osteoinductive ceramics as a synthetic alternative to autologous bone grafting. Proceedings of the National Academy of Sciences of the United States of America. 2010;107(31):13614–13619. doi: 10.1073/pnas.1003600107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barradas A. M. C., Yuan H., van Blitterswijk C. A., Habibovic P. Osteoinductive biomaterials: current knowledge of properties, experimental models and biological mechanisms. European Cells & Materials. 2011;21:407–429. doi: 10.22203/ecm.v021a31. [DOI] [PubMed] [Google Scholar]
- 42.Miron R. J., Sculean A., Shuang Y., et al. Osteoinductive potential of a novel biphasic calcium phosphate bone graft in comparison with autographs, xenografts, and DFDBA. Clinical Oral Implants Research. 2015 doi: 10.1111/clr.12647. [DOI] [PubMed] [Google Scholar]
- 43.Horowitz R. A., Leventis M. D., Rohrer M. D., Prasad H. S. Bone grafting: history, rationale, and selection of materials and techniques. Compendium of Continuing Education in Dentistry. 2014;35(4, supplement):1–6. [PubMed] [Google Scholar]
- 44.Evian C. I., Rosenberg E. S., Coslet J. G., Corn H. The osteogenic activity of bone removed from healing extraction sockets in humans. Journal of Periodontology. 1982;53(2):81–85. doi: 10.1902/jop.1982.53.2.81. [DOI] [PubMed] [Google Scholar]
- 45.Sasaki H., Koyama S., Yokoyama M., Yamaguchi K., Itoh M., Sasaki K. Bone metabolic activity around dental implants under loading observed using bone scintigraphy. The International Journal of Oral & Maxillofacial Implants. 2008;23(5):827–834. [PubMed] [Google Scholar]
- 46.Leventis M. D., Fairbairn P., Dontas I., et al. Biological response to β-tricalcium phosphate/calcium sulfate synthetic graft material: an experimental study. Implant Dentistry. 2014;23(1):37–43. doi: 10.1097/id.0000000000000030. [DOI] [PubMed] [Google Scholar]
- 47.Brunski J. B., Puleo D. A., Nanci A. Biomaterials and biomechanics of oral and maxillofacial implants: current status and future developments. The International Journal of Oral & Maxillofacial Implants. 2000;15(1):15–46. [PubMed] [Google Scholar]
- 48.Duyck J., Vandamme K. The effect of loading on peri-implant bone: a critical review of the literature. Journal of Oral Rehabilitation. 2014;41(10):783–794. doi: 10.1111/joor.12195. [DOI] [PubMed] [Google Scholar]