Abstract
Background
Clinician-administered measures to assess severity of illness anxiety and response to treatment are few. The authors evaluated a modified version of the hypochondriasis-Y-BOCS (H-YBOCS-M), a 19-item, semistructured, clinician-administered instrument designed to rate severity of illness-related thoughts, behaviors, and avoidance.
Methods
The scale was administered to 195 treatment-seeking adults with DSM-IV hypochondriasis. Test–retest reliability was assessed in a subsample of 20 patients. Interrater reliability was assessed by 27 interviews independently rated by four raters. Sensitivity to change was evaluated in a subsample of 149 patients. Convergent and discriminant validity was examined by comparing H-YBOCS-M scores to other measures administered. Item clustering was examined with confirmatory and exploratory factor analyses.
Results
The H-YBOCS-M demonstrated good internal consistency, interrater and test–retest reliability, and sensitivity to symptom change with treatment. Construct validity was supported by significant higher correlations with scores on other measures of hypochondriasis than with nonhypochondriacal measures. Improvement over time in response to treatment correlated with improvement both on measures of hypochondriasis and on measures of somatization, depression, anxiety, and functional status. Confirmatory factor analysis did not show adequate fit for a three-factor model. Exploratory factor analysis revealed a five-factor solution with the first two factors consistent with the separation of the H-YBOCS-M items into the subscales of illness-related avoidance and compulsions.
Conclusions
H-YBOCS-M appears to be valid, reliable, and appropriate as an outcome measure for treatment studies of illness anxiety. Study results highlight “avoidance” as a key feature of illness anxiety—with potentially important nosologic and treatment implications.
Keywords: assessment, diagnosis, measurement, psychometrics, illness anxiety, hypochondriasis, anxiety, anxiety disorders, obsessive-compulsive disorder (OCD), health services
Hypochondriasis is characterized by preoccupation with the fear or belief of having a serious disease, based on a misinterpretation of normal bodily symptoms that persists despite medical reassurance.[1] It exerts a heavy toll on the afflicted individuals and on national health-care resources.[2, 3] It is also a common disorder in the primary care population in the United States, with an estimated prevalence of 4%.[4] In the last decade, hypochondriasis (also referred to as health anxiety or illness anxiety) has received increased research attention, both phenomenologically and therapeutically.[5–7] However, the lack of consistently used and validated clinician-administered measures limits researchers’ ability to adequately assess severity and treatment effectiveness.[8]
Currently, there are two widely used well-validated, self-report measures of hypochondriasis severity: the Whiteley Index[9] and the Illness Attitude Scale.[10] These measures, although excellent for assessing illness-related cognitions and fears, do not adequately assess other important features of hypochondriasis—such as illness-related behaviors (e.g., reassurance seeking) and illness-related avoidance. In the assessment of the severity of other disorders characterized by obsessional thoughts, clinician-administered measures have been developed that examine not only repetitive thoughts but also the behaviors conducted in response to these thoughts. These sensitive and reliable instruments—such as the Yale-Brown Obsessive Compulsive Scale (Y-BOCS)[11, 12] to assess obsessive-compulsive disorder (OCD) and the BDD-YBOCS[13] to assess body dysmorphic disorder—quantify the impact of obsessive thoughts and behaviors not by evaluating the symptom’s idiosyncratic content but by assessing thoughts and behaviors along the dimensions of duration, functional interference, distress, and the degree to which the patient can resist or control the symptoms. Neither the Whiteley Index nor the Illness Attitudes Scale assesses all of these dimensions.
More recently, the psychometric properties of a clinician-administered instrument for assessing hypochondriasis (the H-YBOCS) were published.[14] As the first validated, clinician-administered instrument to assess illness anxiety, this scale represents a significant advance in the field. The H-YBOCS was modeled after the Y-BOCS and therefore assesses symptoms by examining time, distress, resistance, control, and functional interference. Because both OCD and hypochondriasis share similar phenomenology (obsessive thoughts and compulsive behaviors), the use of the Y-BOCS as a model for the development of a measure of illness anxiety was a logical step.[15, 16] Although the H-YBOCS retains the dimensional format of the original Y-BOCS, it also expands upon the Y-BOCS by including item clusters that measure not only obsessive thinking and compulsive behavior, but also avoidance.
This article reports on the psychometric validation of a modified version of the H-YBOCS, termed as the H-YBOCS-M. Because of the close similarity between the two instruments, this report should be considered both a replication and extension of the initial psychometric article on the H-YBOCS.[14] The extension in this reports refers to: (a) a comparison of the sensitivity to change for the H-YBOCS-M with measures of change on other dimensions of psychopathology; (b) the determination of whether a measure of quality of life relates to either baseline or change scores on the H-YBOCS-M; and (c) a psychometric assessment of this revised version that includes new items and a new self-report component (a Symptom Checklist). Both the Checklist and the Questionnaire are included in the Appendix.
Our prior research[7] used an unpublished hypochondriasis-modified version of the Y-BOCS (labeled CHIC-OCS—“Columbia Heightened Illness Concern-Obsessive Compulsive Scale”). The H-YBOCS and H-YBOCS-M represent an improvement on the CHIC-OCS by including a major section on avoidance behaviors. One feature of hypochondriasis that neither the original H-YBOCS nor the CHIC-OCS was designed to measure however was the waxing and waning quality of illness-related anxiety. Unlike the intrusions and compulsions in OCD that are typically a daily experience, the illness worries and behaviors of the hypochondriacal patient can have a wider range of frequency—from daily to less than once a week. Therefore, to enhance the measurement of illness anxiety severity, our revised instrument (i.e., H-YBOCS-M) has added items that specifically assess frequency (number of days per week in which there are illness-related worries, behaviors, or avoidance).
Five additional modifications distinguish the H-YBOCS-M from the H-YBOCS. First, retaining the convention in the original Y-BOCS, the insight item of the H-YBOCS-M is considered an independent item and is not included in the calculation of the total severity score. Second, to help the interviewer identify the most prominent manifestations of illness anxiety, a self-report Checklist has been added to the H-BOCS-M that itemizes many common illness-related obsessions, compulsions, and avoidance behaviors; a similar checklist approach guides the interviewer in the use of the Y-BOCS for OCD and was used in the CHIC-OCS. Third, because patients with health anxiety view the term “hypochondriac” as pejorative, the H-YBOCS-M has replaced the term “hypochondriacal” with phrases that ask about fears of “illness” or “a serious disease.” This terminology is also consistent with the changes proposed for the Somatic Symptom Disorder section of DSM-5 in which the term hypochondriasis is replaced by such terms as “illness anxiety” and “health anxiety.”[17] Fourth, in the assessment of distress associated with illness-related behaviors, the H-YBOCS-M phrases the question quite differently from the H-YBOCS. Because reassurance seeking in hypochondriasis is often ego-syntonic and experienced at least temporarily as a source of relief, this item in the H-YBOCS-M is phrased to assess the degree of distress that would arise if checking and reassurance-seeking behaviors were prevented, whereas in the H-YBOCS, the corollary question asks about distress associated with seeking of reassurance itself. Finally, the H-YBOCS-M adds an instructional section to assist in the assessment of avoidance and an item asking about the number of situations that the patient currently avoids.
MATERIALS AND METHODS
SAMPLE
The data for this psychometric study, collected 2006–2011, came from a dual-site, randomized, controlled treatment study of hypochondriasis comparing pharmacological, cognitive-behavioral, and combined treatments. The study protocol was approved by the institutional review boards of the New York State Psychiatric Institute and the Brigham Women’s Hospital and all patients provided signed informed consent.
All patients met DSM-IV criteria for hypochondriasis, established with the Structured Diagnostic Interview for Hypochondriasis (SDIH).[18] Comorbid diagnoses were assessed with the Mini-International Neuropsychiatric Interview (M.I.N.I.).[19] Patients were recruited through print and Internet ads and doctor referrals. Evaluations before the start of the treatment conducted with 195 consecutively enrolled participants are included in this report. The subsample for sensitivity to change includes all 149 patients for whom ratings at baseline and week 12 were obtained.
STUDY INSTRUMENT
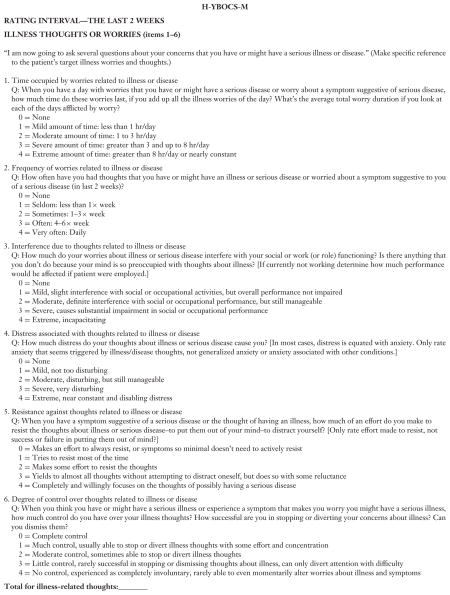
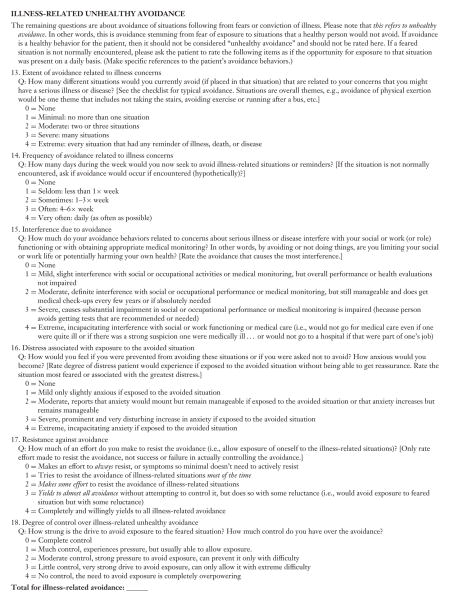
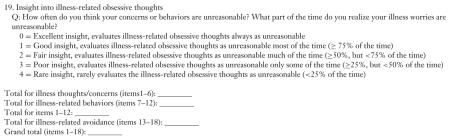
First, the patient completes the Illness Concern Checklist, which lists a variety of illness-related worries, behaviors, and avoidance. Next, the interviewer reviews with the patient which disease-related symptoms should serve as the primary targets for questions during the H-YBOCS-M interview. The H-YBOCS-M is a 19-item semistructured, clinician-administered instrument designed to assess the severity of illness worries, behaviors, and avoidance during the previous 2 weeks. Similar to the Y-BOCS, the H-YBOCS-M has specific probes for each item and the individual item scores range from 0 to 4 with the larger score indicating higher symptom severity. The H-YBOCS-M total severity score is the sum of items 1 through 18.
The instrument contains three clinically derived subscales: illness worries, illness-related behaviors and unhealthy avoidance. Each of the subscales consists of six items with the sum of the six items producing a composite subscale severity score. Within each subscale, the items examine frequency, time spent, interference, distress, resistance, and degree of control. Item 19 indicates degree of insight and is not included in the composite severity score calculations.
PROCEDURES
Interrater reliability was assessed by blind audit of a random selection of 27 audiotaped interviews with 25 participants conducted by independent evaluators. Each of these interviews was rated independently by three other raters. For two of the audiotaped interviews, the same participant was used twice, but ratings were conducted on assessments collected at two different phases of treatment. Test–retest reliability was assessed in 20 participants by the same rater with an interval of 1 week either before the start or after completion of the treatment phase of the study.
To assess convergent validity, baseline H-YBOCS-M scores for the 195 participants were compared to other measures of hypochondriasis and/or somatization administered at the same visit—the Whiteley Index,[9] Heightened Illness Concern-Severity Scale (HIC-Severity),[20] Patient Health Questionnaire-15 (PHQ-15),[21] and Somatosensory Amplification Scale (SSAS).[22] The Whiteley Index is a well-validated self-report measure of hypochondriasis severity that is the most widely used measure of hypochondriasis in the published literature. The HIC Severity is a clinician-administered instrument focusing on the patient’s most intense episode of hypochondriasis in the prior 2 weeks. The PHQ-15 is a brief self-administered screening measure of somatization that has been shown to have good psychometric properties,[23] whereas the SSAS is a 10-item self-report that assesses sensitivity to ambiguous, distressing bodily discomfort.
To assess discriminant validity, baseline H-YBOCS-M scores for the 195 participants were compared to scores on the Beck Depression Inventory-II (BDI-II),[24] State-Trait Anxiety Inventory, Form Y, State subscale (STAI),[25] Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q Short Form [SF]),[26] the Sickness Impact Profile (SIP),[27] as well as age and race of the participants. BDI-II is a validated self-report measure of depression severity. STAI is a validated measure of anxiety in adults. Q-LES-Q SF is a validated measure of perceived quality of life and satisfaction. The SIP is a validated behaviorally based self-report measure of functional impairment whose total score covers 12 areas, encompassing physical, psychosocial, vocational, and recreational activities.
Sensitivity of the H-YBOCS-M to change with treatment was evaluated using the full sample of 149 patients who completed the first 12 weeks of treatment in the study. Percentage change was calculated as follows: [(baseline score − week 12 score)/baseline score] × 100. To further test the ability of the H-YBOCS-M to detect changes in hypochondriacal symptoms, point biserial correlations for the percentage change in scores were calculated between the H-YBOCS-M and the Whiteley Index, HIC Severity Scale, SSAS, PHQ-15, BDI-II, STAI, Q-LES-Q SF, and SIP.
STATISTICAL ANALYSIS
To evaluate interrater and test–retest reliability, intraclass correlation coefficients (ICCs) were used; Cronbach’s alpha coefficient was used to evaluate internal consistency. Pearson’s correlation coefficients were used to evaluate convergent and discriminant validity. Sensitivity to change was evaluated with t-tests, percentage change and Cohen’s d effect sizes comparing baseline and week 12 scores. Significance required an α-level <.05.
To assess the construct validity of the three subscales, we employed confirmatory factor analysis (CFA; PROC CALIS procedure in SAS). It was applied to the raw score of the 18-item H-YBOCS-M of the whole sample of 195 participants to verify the hypothesized three-factor structure. To determine the adequacy of model fit to the data, several fit statistics were estimated: the Chi-square (χ2) goodness-of-fit (GFI) statistics, the absolute fit indices (the GFI, root mean square error of approximate [RMSEA]), and the incremental fit indices (the Bentler’s comparative fit index [CFI], normed fit index [NFI], Bentler and Bonett’s nonnormed fit index [NNFI]). Acceptable model fit is indicated by a χ2 value close to zero and a χ2 probability ≥ 0.05, GFI, CFI, NFI, and NNFI values ≥ 0.90 and an RMSEA value ≤ 0.06.[28] Subsequent exploratory factor analysis (EFA; PROC FACTOR procedure in SAS) with promax rotation was performed to identify the number of latent constructs and determine the factor structure. The number of factors was determined by examining the eigenvalues, scree plot, and significant factor loadings.
RESULTS
PATIENT SAMPLE
The mean age of the 195 participants was 39.7 ± 14.3 years and 56.4% were females, 64.1% self-identified as White, 16.4% Black, 5.1% Asian, and 14.3% were of other racial background. Current Axis I comorbidity was common: major depression (33.3%), generalized anxiety disorder (28.1%), panic disorder (14.6%), OCD (13%), and somatization disorder (11%).
The subsample of 149 patients who completed 12 weeks of treatment had a mean age of 41.0 ± 14.6 years and 59.1% were females; the ethnicity was 64.4% White, 16.8% Black, 5.4% Asian, and 13.4% other.
The subsample of 25 participants for interrater reliability had a mean age of 43.4 ± 15.4 years and 48.0% were females; the ethnicity was 60.0% White, 28.0% Black, and 12.0% other. The subsample of 20 participants for test–retest reliability had a mean age of 36.6 ± 13.2 years and 60.0% were females; the ethnicity was 55.0% White, 15.0% Black, 5.0% Asian, and 25.0% other.
ANALYSIS OF INDIVIDUAL ITEMS
Each item was frequently endorsed with scores covering the range of symptom severity (Table 1). No one was free from illness worries or distress from them (items 1, 2, and 4). Means and standard deviations are presented in Table 1.
TABLE 1.
H-YBOCS-M mean scores and observed range, interrater reliability intraclass correlation coefficients and correlations of individual items with the total score (N = 195)
| Item | M | SD | Range of scores | ICCs | r |
|---|---|---|---|---|---|
| Worries | |||||
| 1. Time | 2.35 | 0.96 | 1–4 | .96b | .44b |
| 2. Frequency | 3.26 | 0.87 | 1–4 | .92b | .21a |
| 3. Interference | 1.61 | 0.88 | 0–4 | .93b | .58b |
| 4. Distress | 2.19 | 0.65 | 1–4 | .99b | .36b |
| 5. Resistance | 1.83 | 1.10 | 0–4 | .96b | .14 |
| 6. Degree of control | 2.33 | 0.89 | 0–4 | .96b | .42b |
| Behaviors | |||||
| 7. Time | 1.68 | 0.92 | 0–4 | .91b | .61b |
| 8. Frequency | 2.67 | 1.19 | 0–4 | .86b | .41b |
| 9. Interference | 1.25 | 0.97 | 0–4 | .87b | .58b |
| 10. Distress | 2.05 | 1.11 | 0–4 | .91b | .44b |
| 11. Resistance | 2.34 | 1.36 | 0–4 | .89b | .17a |
| 12. Degree of control | 2.16 | 1.19 | 0–4 | .83b | .57b |
| Avoidance | |||||
| 13. Extent of avoidance | 1.49 | 1.03 | 0–4 | .77b | .63b |
| 14. Frequency | 2.19 | 1.52 | 0–4 | .81b | .61b |
| 15. Interference | 1.40 | 1.14 | 0–4 | .87b | .70b |
| 16. Distress | 1.81 | 1.26 | 0–4 | .88b | .66b |
| 17. Resistance | 1.76 | 1.41 | 0–4 | .86b | .57b |
| 18. Degree of control | 1.50 | 1.21 | 0–4 | .87b | .63b |
| Total score | 35.91 | 11.11 | .96b | ||
| 19. Insight (n = 180) | 2.27 | 1.12 | 0–4 | .82b | −.10 |
Correlation significant at α < .05.
Correlation significant at α ≤ .001.
RELIABILITY
Interrater (Table 1) and test–retest reliability were excellent. ICCs for test–retest reliability and interrater agreement were .99 for total H-YBOCS-M scores. For item 19 (insight), ICCs were .87 for test–retest and .82 for interrater reliability (data were available only on 19 interviews). Cronbach’s alpha coefficient for the 18-item version was α = .87, and for the 19-item version α = .85. For the subscales, Cronbach’s alpha coefficients were .67 for illness worries, .82 for illness-related behaviors, and .92 for avoidance.
Table 1 also shows Pearson’s product–moment correlations between each individual item and the 18-item total score minus that item. All except two items (5—resistance against illness worries, and 19–insight) had significant correlations with the 18-item total score, ranging from .17 to .70.
CONVERGENT AND DISCRIMINANT VALIDITY
The H-YBOCS-M total scores were significantly positively correlated with other measures of hypochondriasis severity, including the Whiteley Index (r = .45) and HIC Severity (r = .51; Table 2), supporting the convergent validity. Correlations with measures of somatic amplification (SSAS) and distress from somatic symptoms (PHQ-15) were lower but significant for the total severity score (r = .28 and .17, respectively). The BDI-II and STAI were selected to assess discriminant validity. The H-YBOCS-M total score correlations with the BDI-II (r = .19) and the STAI (r = .35) were significant, but low to moderate in size (Table 2). Partial correlation (r = .049, P = .50) between the H-YBOCS-M and the BDI-II after removing the contribution of the Whiteley Index was not significant. The BDI-II did not add significant information beyond the common shared variance with the H-YBOCS-M and the Whiteley Index. Partial correlation (r = .17, P = .015) between the H-YBOCS-M and STAI after removing the contribution of the Whiteley Index was significant, although small. H-YBOCS-M total scores were significantly negatively correlated with perceived quality of life (Q-LES-Q SF) scores (r = −.35) and positively correlated with functional status (SIP) scores (r = .28), but not with participant’s age or race.
TABLE 2.
Pearson’s correlation coefficients of the H-YBOCS-M 18-item total score at baseline and percent change score at week 12 with other measures
| Scale | H-YBOCS-M total score at baseline (n = 195) | H-YBOCS-M percent change score (n = 149) |
|---|---|---|
| Whiteley Index | .448b | .561b |
| HIC Severity | .505b | .719b |
| SSAS | .278b | .378b |
| PHQ-15 | .167a | .358b |
| BDI-II | .194b | .318b |
| STAI | .352b | .274b |
| Q-LES-Q SF | −.348b | −.168a |
| SIP total | .281b | .495b |
| Age | .012 | n/a |
| Race | −.029 | n/a |
Correlation significant at α < .05.
Correlations are significant at α ≤ .01.
SENSITIVITY TO CHANGE
After 12 weeks of treatment, the mean percent change in the H-YBOCS-M total score was 37.4 percent (SD = 42.3). Changes in the total and subscale scores were significant at α < .001 with medium to large effect sizes (Table 3). Percent change scores on the H-YBOCS-M also correlated moderately or higher with percent change scores on other measures of hypochondriasis, somatic amplification, physical symptoms, depression, anxiety, and functional status (Table 2). At week 12, the H-YBOCS-M total score significantly negatively correlated with Q-LES-Q SF score (r = −.46, P < .001), connecting lower hypochondriasis scores with higher perceived quality of life.
TABLE 3.
Sensitivity to change (N = 149)
| Scales | Baseline
|
Week 12
|
t-valuea | Cohen’s d | ||
|---|---|---|---|---|---|---|
| M | SD | M | SD | |||
| Illness worries | 13.46 | 3.32 | 8.57 | 4.83 | 12.57 | 1.18 |
| Behaviors | 12.03 | 5.03 | 7.10 | 5.59 | 8.96 | 0.93 |
| Avoidance | 10.09 | 6.67 | 5.85 | 6.40 | 7.61 | 0.65 |
| Total score | 35.57 | 11.23 | 21.50 | 14.30 | 11.63 | 1.10 |
Significant at α < .001.
FACTOR STRUCTURE
Confirmatory factor analysis
First, the three-factor model comprised illness worries, illness-related behaviors, and avoidance was tested. Items 1–6 were hypothesized to load on the illness worries factor, items 7–12 to load on the illness behaviors factor, and items 13–18 on the avoidance factor. Results indicated that this model was not an optimal fit; all goodness-of-fit statistics failed to meet established guidelines (Table 4). Factor loadings presented in Table 5 indicate the strongest loadings were for avoidance items.
TABLE 4.
Relative fit of confirmatory factor analysis model (N = 195).
| Fit statistics | Value |
|---|---|
| χ2 | 395.43 |
| df | 132 |
| P-value | <.0001 |
| GFI | 0.81 |
| RMSEA | 0.1014 |
| CFI | 0.8483 |
| NNFI | 0.82 |
| NFI | 0.79 |
Note: The fit indices above include the goodness-of-fit index (GFI), root mean square error of approximate (RMSEA), Bentler’s comparative fit index (CFI), Bentler and Bonett’s nonnormed fit index (NNFI), and normed fit index (NFI).
TABLE 5.
Confirmatory factor analysis loadings (N = 195)
| Items | Factor 1 | Factor 2 | Factor 3 |
|---|---|---|---|
| 1. Worry time | 0.69 | ||
| 2. Frequency | 0.29 | ||
| 3. Interference | 0.70 | ||
| 4. Distress | 0.65 | ||
| 5. Resistance | 0.26 | ||
| 6. Degree of control | 0.55 | ||
| 7. Behavior time | 0.77 | ||
| 8. Frequency | 0.63 | ||
| 9. Interference | 0.72 | ||
| 10. Distress | 0.44 | ||
| 11. Resistance | 0.79 | ||
| 12. Degree of control | 0.79 | ||
| 13. Extent of avoidance | 0.84 | ||
| 14. Frequency | 0.83 | ||
| 15. Interference | 0.84 | ||
| 16. Distress | 0.88 | ||
| 17. Resistance | 0.76 | ||
| 18. Degree of control | 0.81 |
Note: All loadings significant at α < .05.
Exploratory factor analysis
Given the absence of a good fit for these data using CFA, an EFA was conducted. The principal axis factoring with a promax rotation identified five factors based on eigenvalues greater than 1, the scree plot and loadings of at least .50 (Table 6). The total variance explained by the five factors was 71.7%. Factor 1 included all six of the avoidance items, with strong loadings ranging between .82 and .89. This factor was labeled “Avoidance” and explained 34.0% of the variance. All six of the illness-related compulsive behavior items loaded on Factor 2 (loadings from .69 to .83; cross-loading of .55 for item 9). This factor was labeled “Compulsive Behaviors” and accounted for 15.2% of the variance. Factors 3, 4, and 5 primarily concerned the illness worry subscale items. Factor 3 (Interference) explained 9.7% of the variance and consisted of loadings of items 1, 3, 4, and 9 and cross-loading on item 7. Factor 4 (Worry Control) explained 7.1% of the variance and consisted of .86 and .74 loadings of items 5 and 6. Factor 5 (Worry Frequency) explained 5.6% of the variance and consisted of the loading of item 2 and cross-loading of item 1. Overall, this EFA confirmed the item groupings for avoidance and for compulsive behaviors, but split the obsessional items into three additional factors with some cross-loading.
TABLE 6.
Exploratory factor analysis loadings (N = 195)
| Items | Factor 1 | Factor 2 | Factor 3 | Factor 4 | Factor 5 |
|---|---|---|---|---|---|
| 1. Worry time | 0.32 | 0.11 | 0.65 | 0.31 | 0.50 |
| 2. Frequency | 0.11 | 0.13 | 0.20 | 0.01 | 0.91 |
| 3. Interference | 0.45 | 0.35 | 0.81 | −0.02 | 0.13 |
| 4. Distress | 0.14 | 0.15 | 0.71 | 0.37 | 0.18 |
| 5. Resistance | 0.04 | 0.05 | 0.09 | 0.86 | 0.00 |
| 6. Degree of control | 0.19 | 0.32 | 0.45 | 0.74 | 0.12 |
| 7. Behavior time | 0.31 | 0.70 | 0.58 | 0.11 | 0.19 |
| 8. Frequency | 0.12 | 0.73 | 0.30 | −0.01 | 0.37 |
| 9. Interference | 0.41 | 0.55 | 0.68 | 0.03 | −0.05 |
| 10. Distress | 0.20 | 0.81 | 0.31 | −0.03 | −0.15 |
| 11. Resistance | −0.03 | 0.69 | −0.20 | 0.23 | 0.07 |
| 12. Degree of control | 0.30 | 0.83 | 0.35 | 0.19 | 0.08 |
| 13. Extent of avoidance | 0.87 | 0.18 | 0.38 | −0.03 | 0.05 |
| 14. Frequency | 0.87 | 0.18 | 0.31 | −0.09 | 0.22 |
| 15. Interference | 0.85 | 0.24 | 0.54 | −0.04 | 0.13 |
| 16. Distress | 0.89 | 0.21 | 0.40 | 0.02 | 0.03 |
| 17. Resistance | 0.82 | 0.16 | 0.25 | 0.13 | 0.01 |
| 18. Degree of control | 0.85 | 0.21 | 0.34 | 0.12 | 0.02 |
| Variance explained (%) | 34.1 | 15.2 | 9.7 | 7.1 | 5.6 |
Note: Loadings of 0.50 and larger are bolded to illustrate which factor an item loaded on.
DISCUSSION
The H-YBOCS-M is a psychometrically sound and valid measure for assessing the severity of illness anxiety in adults with hypochondriasis. The instrument covers the key features of illness thoughts, behaviors, and avoidance by examining each along multiple dimensions. The instrument is relatively brief and easy to administer. Similar to the Y-BOCS, the H-YBOCS-M is specifically designed to measure symptom severity and does not depend on the idiosyncratic content of worries or behaviors.
The H-YBOCS-M items were endorsed across the range of severity and correlated significantly with the total scores. The 1-week test–retest reliability and interrater reliability were high. Construct validity was supported by much stronger correlations with other measures of hypochondriasis than with measures of somatic symptoms, depression, anxiety, or perceived quality of life. Sensitivity to change in response to treatment was demonstrated by correlations with improvement on measures of hypochondriasis, somatization, depression, anxiety, and functional status.
As had been reported for the Y-BOCS[11] and the BDD-YBOCS,[13] the item that measures resistance to obsessive worries had the lowest correlation with the total 18-item score. Our finding that the insight item was not related to the total H-BOCS-M score was similarly reported for the BDD-YBOCS.[13]
Although the hypothesis-driven CFA did not support the clinically derived segregation of the 18 items into three subscales, the exploratory analysis did provide partial support for the factor structure. The EFA segregated out the six avoidance items as one factor and the six compulsive behavior items as a second factor. In parallel, initial models for the Y-BOCS II were not supported by the CFA, but the EFA generally supported separation between obsessions and compulsions.[29] In that analysis, the interference from obsessions item did not conform to the theoretical model and loaded on both the obsessions and compulsions factors. Similarly, in the current study, the interference items for obsessions, compulsions, and avoidance loaded together into a separate factor on the EFA.
Perhaps the most valuable contribution of Greeven et al.[14] in their adaptation of the Y-BOCS for hypochondriasis was to expand beyond obsessions and compulsions by including avoidance. Their validation study supported the segregation of items into these three clusters by use of factor analysis. Although reassurance seeking behaviors and illness-related unhealthy avoidance are not among the DSM-IV-TR criteria of hypochondriasis, they have been cited as important characteristics of the disorder.[14, 30] Indeed, in the proposed revision of DSM-5, the new diagnostic category of “Illness Anxiety Disorder” specifically includes criteria encompassing illness-related behaviors and avoidance.[17] Both illness-related behaviors and avoidance subscales of the H-YBOCS-M performed well psychometrically in this study.
Given that recent research suggests that hypochondriasis may be better understood as a severe manifestation of an illness anxiety disorder,[31,32] the assessment of avoidance is essential. For example, patients with illness anxiety may avoid situations that provoke symptoms or potentially exacerbate the feared illness,[33] such as physical exertion that triggers palpitations or shortness of breath. Paradoxically, patients with illness anxiety may also avoid doctors to the point of neglecting health[34] because they fear that the medical evaluation will confirm their worst suspicions. To assist clinicians and researchers, the H-BOCS-M Checklist includes many examples of avoidance, thus facilitating a more complete assessment of the patient with illness anxiety. Assessment of illness-related worries, behaviors, and avoidance will contribute to a better understanding of the phenomenology and morbidity of hypochondriasis and enable the identification of more effective strategies to treat the different dimensions. It is noteworthy that increased attention has been given to avoidance in the newly published second edition of the Y-BOCS[29] and, as noted above, avoidance is now included as a criterion in the DSM-5 draft of Illness Anxiety Disorder.[17]
From a psychometrics perspective, the H-YBOCS-M performed comparably to the H-YBOCS. Cronbach’s alpha, interrater ICCs and convergent and discriminant validity for the H-YBOCS[14] and H-YBOCS-M were very similar. Both measures had significant correlations with the Whiteley Index and with depression and anxiety scales. Both measures appear sensitive to change with comparable effect sizes. This report extends the prior psychometric study of the H-YBOCS by demonstrating that the change on the H-YBOCS-M scores between baseline and week 12 correlated significantly with improvement not only in hypochondriacal concerns, but also in somatization, anxiety, depression, and functional status. The correlation between improvement in illness anxiety and behavioral functioning was moderately strong (r = .495), whereas the correlation with perceived quality of life was weak (r = −.168); the discrepancy between these two measures may suggest that concrete behavioral change is a more sensitive or an earlier marker of improvement than the individual’s self-assessment of satisfaction with his/her life. These findings suggest that the H-YBOCS-M is an excellent measure to document improvement over time. This psychometric study also confirms that the H-BOCS-M has excellent interrater reliability. Although the inter-rater reliability of the original H-YBOCS was established using two experts in the area of hypochondriasis, our study demonstrated high reliability among four raters from different locations and with different levels of experience. Finally, the H-YBOCS-M was validated on an English-speaking sample of the Northeastern United States, whereas the H-YBOCS used a Dutch sample.
Limitations of this study include the method by which interrater reliability was evaluated as audiotaped interviews likely provide an upper bound estimate;[13] a more stringent test would be for each rater to conduct his or her own interview with each patient. A second limitation deals with discriminant validity; although the correlation with the total H-BOCS-M score was higher with the hypochondriacal measures (Whiteley Index), both the BDI-II and STAI also correlated significantly. The correlation with the BDI-II was low and disappeared when the partial correlation was examined after the contribution of the Whiteley Index was removed. The correlation with the STAI was moderate in size, but the partial correlation was small after removing the Whiteley Index’s contribution. These analyses suggest that the H-YBOCS-M has good discriminant validity. Third, because we did not compare the H-YBOCS and the H-YBOCS-M directly, we cannot determine whether the modifications introduced into the H-YBOCS-M represent an improvement upon the H-YBOCS or are simply an alternative version. Finally, generalizability of the study results might be limited to patients who are willing to receive treatment for hypochondriasis.
CONCLUSIONS
The H-YBOCS-M appears to be a valid and reliable measure of the severity of illness-related thoughts, behaviors, and avoidance. It shows sensitivity to change and is likely to be a suitable outcome measure for illness anxiety in clinical and research settings.
Further research might investigate whether H-YBOCS-M and its subscales are helpful in identifying clinically meaningful patient subgroups. Although H-YBOCS-M is a clinical scale and is not intended for use with nonclinical populations, it would be informative to administer this scale to a nonclinical sample to develop reference for future comparisons.
Acknowledgments
This work was supported by National Institute of Mental Health research grants (5R01MH071688 and 5R01MH071456) awarded to AJB and BAF.
APPENDIX: ILLNESS-RELATED CHECKLIST


References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 2000. text revision. [Google Scholar]
- 2.Barsky AJ, Ettner SL, Horsky J, Bates DW. Resource utilization of patients with hypochondriacal health anxiety and somatization. Med Care. 2001;39:705–715. doi: 10.1097/00005650-200107000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Hansen MS, Fink P, Sondergaard L, Frydenberg M. Mental illness and health care use: a study among new neurological patients. Gen Hosp Psychiatry. 2005;27:119–124. doi: 10.1016/j.genhosppsych.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Barsky AJ, Wyshak G, Klerman GL, Latham KS. The prevalence of hypochondriasis in medical outpatients. Soc Psychiatry Psychiatr Epidemiol. 1990;25:89–94. doi: 10.1007/BF00794988. [DOI] [PubMed] [Google Scholar]
- 5.Barsky AJ, Ahern DK. Cognitive behavior therapy for hypochondriasis. JAMA. 2004;291:1464–1470. doi: 10.1001/jama.291.12.1464. [DOI] [PubMed] [Google Scholar]
- 6.Greeven A, van Balkom AJLM, Visser S, et al. Cognitive behavior therapy and paroxetine in the treatment of hypochondriasis: a randomized controlled trial. Am J Psychiatry. 2007;164:91–99. doi: 10.1176/ajp.2007.164.1.91. [DOI] [PubMed] [Google Scholar]
- 7.Fallon BA, Petkova E, Skritskaya N, et al. A double-masked, placebo-controlled study of fluoxetine for hypochondriasis. J Clin Psychopharmacol. 2008;28:638–645. doi: 10.1097/JCP.0b013e31818d21cf. [DOI] [PubMed] [Google Scholar]
- 8.Thomson AB, Page LA. Psychotherapies for hypochondriasis. Cochrane Database Syst Rev. 2007;4:1–35. doi: 10.1002/14651858.CD006520.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pilowsky I. Dimensions of hypochondriasis. Br J Psychiatry. 1967;113:89–93. doi: 10.1192/bjp.113.494.89. [DOI] [PubMed] [Google Scholar]
- 10.Kellner R. Abridged Manual of the Illness Attitude Scales (Mimeographed) Albuquerque, NM: University of New Mexico Press; 1987. [Google Scholar]
- 11.Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale: I. Development, use and reliability. Arch Gen Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 12.Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale: II. Validity Arch Gen Psychiatry. 1989;46:1012–1016. doi: 10.1001/archpsyc.1989.01810110054008. [DOI] [PubMed] [Google Scholar]
- 13.Phillips KA, Hollander E, Rasmussen SA, et al. A severity rating scale for body dysmorphic disorder: development, reliability, and validity of a modified version of the Yale-Brown Obsessive-Compulsive Scale. Psychopharmacol Bull. 1997;33:17–22. [PubMed] [Google Scholar]
- 14.Greeven A, Spinhoven P, van Balkom AJLM. Hypochondriasis Y-BOCS: a study of the psychometric properties of a clinician-administered semi-structured interview to assess hypochondriacal thoughts and behaviors. Clin Psychol Psychotherapy. 2009;16(5):431–443. doi: 10.1002/cpp.634. [DOI] [PubMed] [Google Scholar]
- 15.Fallon BA, Javitch JA, Hollander E, Liebowitz MR. Hypochondriasis and obsessive compulsive disorder: overlaps in diagnosis and treatment. J Clin Psychiatry. 1991;52:457–460. [PubMed] [Google Scholar]
- 16.Greeven A, van Balkom AJ, van Rood YR, et al. The boundary between hypochondriasis and obsessive-compulsive disorder: a cross-sectional study from the Netherlands. J Clin Psychiatry. 2006;67(11):1682–1689. doi: 10.4088/jcp.v67n1103. [DOI] [PubMed] [Google Scholar]
- 17.American Psychiatric Association. [Accessed November 19, 2011.];DSM-V Development. J 02 Illness Anxiety Disorder. Available at: http://www.dsm5.org/ProposedRevision/Pages/proposedrevision.aspx?rid=10.
- 18.Barsky AJ, Cleary PD, Wyshak G, et al. A Structured Diagnostic Interview for Hypochondriasis: a proposed criterion standard. J NervMent Dis. 1992;180:20–27. doi: 10.1097/00005053-199201000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. quiz 34–57. [PubMed] [Google Scholar]
- 20.Fallon BA. Pharmacologic strategies for hypochondriasis. In: Starcevic V, Lipsett DR, editors. Hypochondriasis: Modern Perspectives on an Ancient Malady. Oxford University Press; New York: 2001. pp. 329–368. [Google Scholar]
- 21.Kroenke K, Spitzer RL, Williams JBW. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;648:258–266. doi: 10.1097/00006842-200203000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Barsky AJ, Wyshak G, Klerman GL. The Somatosensory Amplification Scale and its relationship to hypochondriasis. J Psychiatr Res. 1990;24(4):323–334. doi: 10.1016/0022-3956(90)90004-a. [DOI] [PubMed] [Google Scholar]
- 23.Interian A, Allen LA, Gara MA, et al. Somatic complaints in primary care: further examining the validity of the Patient Health Questionnaire (PHQ-15) Psychosomatics. 2006;47:392–398. doi: 10.1176/appi.psy.47.5.392. [DOI] [PubMed] [Google Scholar]
- 24.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 25.Spielberger CD. Manual for the State-Trait Anxiety Inventory (Form Y) Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 26.Endicott J, Nee J, Harrison W, Blumenthal R. Quality of Life Enjoyment and Satisfaction Questionnaire: a new measure. Psychopharmacol Bull. 1993;29:321–326. [PubMed] [Google Scholar]
- 27.Bergner M, Bobbit RA, Carter WB, Gilson BS. The Sickness Impact Profile: development and final revision of a health status measure. Med Care. 1981;19(8):787–805. doi: 10.1097/00005650-198108000-00001. [DOI] [PubMed] [Google Scholar]
- 28.Hu L, Bentler PM. Cut-score criteria for fit indices in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- 29.Storch EA, Rasmussen SA, Price LH, et al. Development and psychometric evaluation of the Yale-Brown Obsessive-Compulsive Scale—second edition. Psychol Assessment. 2010;22:223–232. doi: 10.1037/a0018492. [DOI] [PubMed] [Google Scholar]
- 30.Warwick HMC, Salkovskis PM. Hypochondriasis. Behav Res Ther. 1990;28:105–117. doi: 10.1016/0005-7967(90)90023-c. [DOI] [PubMed] [Google Scholar]
- 31.Fink P, Ornbol E, Toft T, et al. A new, empirically established hypochondriasis diagnosis. Am J Psychiatry. 2004;161:1680–1691. doi: 10.1176/appi.ajp.161.9.1680. [DOI] [PubMed] [Google Scholar]
- 32.Kroenke K, Sharpe M, Sykes R. Revising the classification of somatoform disorders: key questions and preliminary recommendations. Psychosomatics. 2007;48:277–285. doi: 10.1176/appi.psy.48.4.277. [DOI] [PubMed] [Google Scholar]
- 33.Neziroglu F, McKay D, Yaryura-Tobias J. Overlapping and distinctive features of hypochondriasis and obsessive-compulsive disorder. J Anxiety Disord. 2000;14:603–614. doi: 10.1016/s0887-6185(00)00053-0. [DOI] [PubMed] [Google Scholar]
- 34.Fallon BA, Qureshi AI, Laje G, Klein B. Hypochondriasis and its relationship to obsessive-compulsive disorder. Psychiatr Clin North Am. 2000;23:605–616. doi: 10.1016/s0193-953x(05)70183-0. [DOI] [PubMed] [Google Scholar]


