Abstract
Objective: This study aimed to examine the impact of a Stop Smoking Before Surgery (SSBS) program in a health authority where responsibility for surgical services is shared by health professionals in regional centers and outlying communities. Methods: A between-subjects, pre-post mixed method program evaluation was conducted. Elective surgery patients at 2 Northern Canadian hospitals were recruited and surveyed at 2 time points: pre-SSBS implementation (n = 150) and 1 year post-SSBS implementation (n = 90). In addition, semistructured interviews were conducted with a purposeful sample of participants (n = 18). Results: Participants who received information about stopping smoking before surgery post-SSBS implementation were more likely than expected to have reduced their smoking, χ2(1, 89) = 10.62, P = .001, and had a significantly higher Awareness of Smoking-Related Perioperative Complications score than those that were advised to quit smoking prior to SSBS implementation (U = 1288.0, P < .001). Being advised by a health care professional was the second strongest predictor of whether or not participants reduced their smoking before surgery post-SSBS implementation. However, there was no significant change in the number of participants who reported being advised to quit smoking before surgery between groups. Conclusion: Providing surgery-specific resources to increase awareness of and support for surgery-specific smoking cessation had limited success in this rural context. Additional strategies are needed to ensure that every surgical patient who smokes receives information about the benefits of quitting for surgery and is aware of available cessation resources.
Keywords: smoking, prevention, primary care, rural health, mixed methods
Introduction
Smoking cessation has been identified as an important strategy for optimizing surgical outcomes. Discussions about smoking cessation prior to surgery can be effective because of increased patient receptiveness due to heightened health concerns and because optimizing surgical outcomes can provide further incentive for stopping smoking.1,2 However, the implementation of systematic approaches for preoperative smoking cessation remain challenging, particularly in regional centers that provide services to people in rural communities. For example, one Canadian study found that few patients in a rural setting were completely abstinent prior to surgery and about half were unaware of the benefits of smoking cessation prior to surgery.3
It is well accepted that brief intervention delivered by health care professionals can increase smoking cessation.4 Furthermore, preoperative clinics have been demonstrated to be effective settings for promoting smoking cessation among surgical patients.5,6 Although, as established in clinical trials, surgical patients who smoke benefit from smoking cessation advice and support,7 there are few instances where programs have been effectively integrated into clinical practice. This becomes even more challenging when considering implementation where responsibility for surgical services is shared by health professionals in regional centers and outlying communities.3 Approaches for ensuring surgical patients receive smoking cessation advice and support need to be designed for these contexts.
The Program
The Stop Smoking Before Surgery (SSBS) program was a collaborative initiative that involved the Canadian Cancer Society, BC Cancer Agency, and Northern Health and was prompted by the collective desire to reduce smoking rates and prevent cancer. The smoking rate in northern British Columbia, Canada in 2012 was 24%,8 substantially higher than the provincial average of 11.4%.9 This region, covering the northern two-thirds of British Columbia and served by 1 health authority, includes several regional hospitals that serve many outlying communities. The SSBS initiative drew support from tobacco policy commitments in the region, and the desire for optimal surgical outcomes and reducing cancer rates. Overall, the goals of the SSBS program were to (a) increase patient awareness of the benefits of quitting for surgery, (b) increase the number of health care professionals providing brief interventions to support cessation among surgical patients, and (c) increase the number of patients who quit smoking for surgery. In particular, efforts were made to support the involvement of a variety of professionals in supporting smoking cessation and to ensure that resources were accessible to a disperse population.
To encourage and support health care providers in providing information and advice regarding stopping smoking for surgery resources (including “Butt out for surgery” rack cards and posters) were developed and distributed for use in physician and surgeon offices. All health care professionals were encouraged to provide brief intervention following the 5 As (Ask, Advise, Assess, Assist, Arrange) and online training was offered. A letter detailing the 5 As was mailed to physician offices and announcements about the SSBS program were included in a physician newsletter, professional development sessions, staff meetings, and in local media. Stress balls and a discharge brochure to encourage patients to stay smoke free for recovery were provided for distribution to surgical patients. Displays were periodically set up in the hospitals to promote smoking cessation in general and for surgery. In addition, posters and video screens in the hospital waiting areas displayed information about the benefits of stopping smoking for surgery. Finally, new surgery-specific cessation resources with photos and quotes from regional health care professionals were also developed for the online provincial smoking cessation resource (www.QuitNow.ca).
Two northern British Columbia communities were chosen for the focus of the SSBS program: Prince George and Prince Rupert. Prince George is a regional center geographically located near the center of British Columbia with a population of approximately 72 000 people.10 Prince Rupert, located in Northwest British Columbia, is a port city with a population of approximately 13 000 people. Within these 2 cities, the University Hospital of Northern British Columbia (UHNBC) and Prince Rupert Regional Hospital (PRRH) are regional hospitals that serve patients from smaller, surrounding communities. With 200 beds, UHNBC provides approximately 5700 elective surgeries annually; while PRRH is a 25-bed facility providing approximately 1600 elective surgeries per year.
The purpose of this study was to examine the impact of the SSBS program. Specific objectives were to examine (a) surgical patients’ reported exposure to the SSBS program, including being advised by a health care professional to stop smoking before surgery; (b) the program’s impact on patient smoking reduction and cessation; and (c) patients’ awareness of smoking-related perioperative complications. Patient reactions to and opinions of the program were also examined.
Methods
Study Design
A between-subjects mixed method program evaluation was conducted using cross-sectional surveys and interviews. The study protocol was approved by the University of British Columbia Behavioural Research Ethics Board and the Northern Health Research Review Committee.
Data Collection
Elective surgery patients (≥19 years) at the 2 study hospitals were recruited at 2 time points: pre-SSBS implementation and 1 year post-SSBS implementation. The SSBS program was implemented from September 2013 to Sept 2014 (and ongoing). Patients who had received surgery between December 2012 and March 2013 (pre-SSBS) were recruited from June to August 2013; and those who had surgery between May and August in 2014 (post-SSBS) were recruited from September to October 2014. A Northern Health employee contacted surgical patients (pre-SSBS n = 1767; post-SSBS n = 1349) by telephone to screen for smoking status and obtain patients permission to release their contact information to the researchers. Those who self-identified as a smoker 6 months prior to surgery (21.7% pre-SSBS and 19.6% post-SSBS) and consented to be contacted by the researchers were mailed information letters about the study and called by the researchers 1 to 2 weeks later. Telephone consent was obtained and trained research assistants using a computer-assisted telephone interviewing system subsequently conducted the survey. Of those eligible, 60% participated in the telephone survey pre-SSBS, and 51% participated in the telephone survey post-SSBS.
Semistructured interviews were also conducted with a purposeful sample of participants (n = 18) who completed the post-SSBS survey and consented to be contacted for an interview. Recruitment priority was given to patients who received general anesthetic and reported having quit or reduced smoking. In total, 36 patients were contacted and 18 returned signed consent forms and completed interviews. Interviews focused on experiences prior to surgery, advice received regarding the benefits of stopping smoking, any challenges in stopping smoking for surgery, and recommendations regarding how support for stopping smoking prior to surgery could be improved.
Measures
Advised to Quit Smoking
Participants were asked if they had been advised by a doctor or other health care professional to quit smoking at any time within 2 months prior to surgery (yes, no, I don’t know).
Quit or Reduced Smoking Prior to Surgery
Participants were asked if they were current smokers (yes/no). Those not currently smoking were asked their quit date to determine if they quit during the 2 month period prior to surgery. Current smokers were asked if they had reduced their smoking within 2 months prior to surgery (yes/no). These questions created the variable quit or reduced 2 months prior to surgery (yes/no).
Awareness of Smoking-Related Perioperative Complications
A measure adapted from Webb et al11 assessed awareness of the risks concerning smoking and surgery. Participants were asked if “smoking makes the following more likely: slower healing of wounds after surgery, increased risk of infection after surgery, increased pain after surgery, increased complications with the anaesthetic.” The response format was a 4-point Likert-type scale (“very unlikely” to “very likely,” “I do not know”). Item responses were coded 0 to 3, with “I do not know” also coded as 0, and summed to create an Awareness of Smoking-Related Perioperative Complications score ranging from 0 to 12. Cronbach’s α was .841.
Exposure to SSBS Materials
In a series of 10 questions participants were asked if they had learned about the benefits of quitting smoking before surgery from: Butt Out Before Surgery rack card; a poster in a clinic, doctor’s office or hospital; table or banner with information; stress balls; stay smoke free for recovery discharge brochure; QuitNow website; other website; media information; a friend or family member; other (yes, no). The first 6 questions were specific to the SSBS program. In contrast to all the above measures, exposure to SSBS materials was only asked of post-SSBS participants.
Demographic questions, type of elective surgery, and questions to describe smoking history (age of initiation, years of smoking, Fagerström Nicotine Dependence Scale12) were asked of all participants to describe the sample.
Data Analysis
Data were analyzed using chi-square, general linear models, and logistic regression. Interaction effects between groups and being advised to stop smoking before surgery on dependent variables were assessed. All analyses was conducted using SPSS for Windows (V.22). Interviews were transcribed and coded with QSR NVivo for descriptive content analysis.
Results
Telephone surveys were completed by 240 eligible participants; 150 pre-SSBS (2013) and 90 post-SSBS (2014). An additional 15 participants completed the survey but were not smoking at the time of survey completion and because they reported a quit date earlier than 2 months prior to surgery, these participants were removed from the data set. Participant demographics, smoking history, nicotine dependence, and smoking status 2 months prior to surgery did not differ significantly between time points (see Table 1).
Table 1.
Participant Demographics, Smoking History, and Nicotine Dependence by Pre- and Post-SSBS Implementation.
| Characteristic | Pre-SSBS (n = 150) | Post-SSBS (n = 90) |
|---|---|---|
| Age, years, mean (SD) | 51.69 (13.8) | 55.0 (14.2) |
| Female, n (%) | 89 (59.3) | 56 (62.2) |
| Ethnicity, n (%) | ||
| Caucasian | 115 (76.7) | 72 (80.0) |
| First Nation/Metis | 30 (20.0) | 15 (16.7) |
| Other | 4 (2.6) | 3 (3.3) |
| No response | 1 (0.7) | 0 (0.0) |
| Marital status, n (%) | ||
| Single/divorced/widowed | 64 (42.7) | 32 (35.6) |
| Married or common-law | 85 (56.7) | 58 (64.4) |
| No response | 1 (0.7) | 0 (0.0) |
| Education level, n (%) | ||
| High school or less | 77 (51.4) | 37 (41.1) |
| Trades/college degree/some college | 51 (34.0) | 33 (36.7) |
| Some university/ undergraduate or graduate degree | 21 (13.9) | 19 (21.1) |
| No response | 1 (0.7) | 1 (1.1) |
| Employment status, n (%) | ||
| Full-time/part-time | 85 (56.7) | 36 (40.0) |
| Not employed | 31 (20.7) | 21 (23.3) |
| Retired | 32 (21.3) | 32 (35.6) |
| No response | 2 (1.3) | 1 (1.1) |
| Annual household income, $, n (%) | ||
| ≤39 999 | 60 (40.0) | 30 (33.3) |
| 40 000-79 999 | 43 (28.7) | 27 (30.0) |
| ≥80,000+ | 40 (26.6) | 19 (21.1) |
| No response | 7 (4.7) | 14 (15.6) |
| Hospital, n (%) | ||
| UHNBC | 140 (93.3) | 81 (90.0) |
| PRRH | 10 (6.7) | 9 (10.0) |
| Surgical procedure (multiple responses allowed), n (%) | ||
| Abdominal | 43 (28.7) | 5 (5.6) |
| Orthopedic | 36 (24.0) | 21 (23.3) |
| Gynecology | 21 (14.0) | 6 (6.7) |
| Urology | 11 (7.3) | 10 (11.1) |
| Eye | 11 (7.3) | 11 (12.2) |
| Vascular | 6 (4.0) | 6 (6.7) |
| Cardiac | 3 (2.0) | 1 (1.1) |
| Cosmetic plastic surgery | 0 (0.0) | 5 (5.6) |
| Dental | 4 (2.7) | 3 (3.3) |
| Other | 17 (11.3) | 29 (32.2) |
| Smoking behavior, mean (SD) | ||
| Age started smoking daily | 18.3 (7.2) | 17.5 (5.6) |
| Years smoking | 33.4 (14.55) | 39.0 (13.5) |
| Fagerström nicotine dependence score prior to surgery (0-10) | 3.5 (2.4) | 3.4 (2.3) |
| Smoking status prior to surgery, n (%) | ||
| Quit within 2 months prior to surgery | 9 (6.0) | 7 (7.8) |
| Reduced within 2 months prior to surgery | 61 (40.7) | 40 (44.4) |
| No smoking status change prior to surgery | 80 (53.3) | 43 (47.8) |
Abbreviations: SSBS, Stop Smoking Before Surgery; UHNBC, University Hospital of Northern British Columbia; PRRH, Prince Rupert Regional Hospital.
Quantitative Findings
No significant differences were found between the 2 groups on smoking reduction before surgery, χ2(1, 239) = 0.62, P = .432, and whether or not participants were advised to stop smoking before surgery, χ2(1, 236) = 0.14, P = .705.
Prior to SSBS implementation, no significant differences in smoking reduction were found between those who were advised to stop smoking before surgery by a health care professional and those who were not, χ2(1, 146) = 0.63, P = .801). Those who were advised to quit smoking before surgery post-SSBS were more likely than expected to have reduced their smoking than those there were not advised to quit post-SSBS, χ2(1, 89) = 10.62, P = .001). Phi is .346 indicating a medium effect size. Table 2 shows frequencies and percentages of advised to quit and quit or reduced smoking by pre- and post-SSBS implementation.
Table 2.
Advised to Quit Smoking by Health Care Professional and Reduced or Quit Smoking by Pre- and Post-SSBS Implementation.
| Pre-SSBS |
Post-SSBS |
|||
|---|---|---|---|---|
| n | % | n | % | |
| Advised to quit smoking | 83 | 56.5 | 48 | 53.9 |
| Reduced or quit smoking before surgery | 70 | 47.0 | 47 | 52.2 |
| Advised to quit smoking and reduced or quit smoking | 38 | 55.1 | 33 | 70.2a |
Abbreviation: SSBS, Stop Smoking Before Surgery.
P = .001.
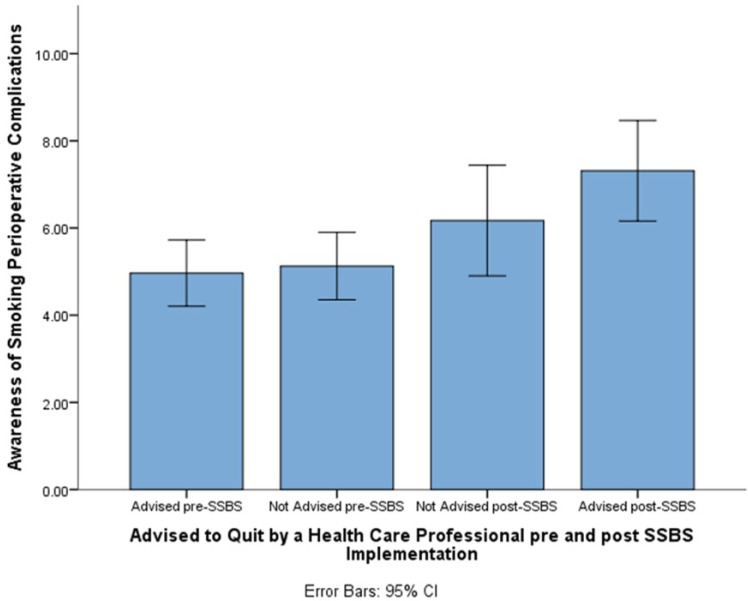
To assess whether pre- and post-SSBS implementation groups and being advised by a health care professional differed on Awareness of Smoking-Related Perioperative Complications a 2-way factorial analysis of variance was desired but violated the assumption of normal distribution. Instead, a 4-level independent variable (advised by a health care professional pre-SSBS, not advised by a health care professional pre-SSBS, advised by health care professional post-SSBS, not advised by a health care professional post-SSBS) was created and a Kruskal-Wallis analysis conducted. A statistically significant difference was found among the 4 levels of the created variable, χ2(3, 232) = 13.93, P = .003. Post hoc Mann-Whitney tests compared the 4 levels on Awareness of Smoking-Related Perioperative Complications score with a Bonferonni corrected P value of .008. The mean rank of those that were advised to quit smoking at time point two (80.67, n = 48; 67.08, n = 48) were significantly higher on Awareness of Smoking-Related Perioperative Complications than those that were advised to quit smoking at time point one ((57.52, n = 83), U = 1288.0, P =.001) and those that were not advised to quit smoking at time point one ((47.56, n = 63), U = 980.0, p =.001). Figure 1 shows means and confidence intervals for each group.
Figure 1.
Means and confidence intervals for awareness of smoking-related perioperative complications by pre- and post-SSBS implementation and being advised to quit smoking by a health care professional. Abbreviation: SSBS, Stop Smoking Before Surgery.
A majority of post-SSBS participants (57.8%) reported exposure to at least 1 SSBS resource. This increases to 73.3% if health care professionals are included as a source of information and 84.4% if all possible sources of receiving the message (ie, friends and family members) are accounted for. On average, post-SSBS participants received information about stopping smoking for surgery from 2.7 different sources.
Logistic regression assessed whether 7 sources of receiving a stop smoking before surgery message (QuitNow website, quit smoking before surgery stress balls, and other websites had insufficient cases, n < 20) could predict whether or not participants quit or reduced smoking before surgery. A significant model was found, χ2 = 29.25, df = 7, n = 82, P < .001. Table 3 shows health care professionals and information from a friend or family member as the strongest predictors.
Table 3.
Logistic Regression Predicting Smoking Reduction and Cessation Before Surgery (Post-SSBS).
| Participant’s Sources of Receiving SSBS Message (%) | Odds Ratio (Confidence Interval) | |
|---|---|---|
| Health care professional | 53.9 | 3.24 (1.09-9.63)a |
| A poster in a clinic, doctor’s office, or hospital | 47.8 | 2.74 (0.74-10.22) |
| Information from a friend or family member | 36.7 | 8.8 (2.265-34.48)a |
| Media information | 32.2 | 0.42 (0.11-1.68) |
| Butt out before surgery rack card | 22.2 | 1.00 (0.22-4.64) |
| Table or banner with information in a hospital | 24.4 | 0.93 (0.20-4.4) |
| Discharge brochure | 24.4 | 1.82 (0.45-7.4) |
| Stress balls | 8.9 | N/A |
| QuitNow website | 7.8 | N/A |
| Other website | 0.0 | N/A |
Abbreviations: SSBS, Stop Smoking Before Surgery; N/A, not applicable (insufficient cases).
P < .05.
Qualitative Findings
The majority of patients who were interviewed were unequivocal in explaining that surgery provided new or additional motivations for them to reduce or quit smoking. For some, just learning about the benefits of cessation prior to surgery prompted an immediate quit attempt. A 29-year-old patient who was provided with SSBS materials and quit prior to surgery explained,
The evidence in those pamphlets were really motivating and really compelling like to say your healing time is quicker, your risk of infection is lower, all those things are really [important]. Surgery is hard enough for people to deal with – it’s kind of like the gross out factor of you know being cut open and it kind of makes you lay low for a while. So just not adding poison to that is a pretty big motivator.
Patients’ experiences in receiving advice regarding smoking cessation for surgery varied. Although some patients specifically recalled receiving advice regarding smoking cessation from a health care professional, several were surprised that this was not discussed. These patients explained that they got their information from pamphlets in their doctor’s office, friends, and the Internet. After learning of the benefits of cessation independently or only having received advice in close proximity to their surgery date, one patient said, “Yeah, I was kind of surprised as I figured that people would be, you know, really all over the fact that I was a smoker and stuff, but no one really said anything.” In some cases, patients indicated they would not have been aware of the benefits of smoking cessation prior to surgery if not for the SSBS materials. Moreover, when asked about how the SSBS program could be improved, several patients simply suggested that physicians and surgeons should be telling patients of the benefits.
Interviews also highlighted some important factors in regards to the rural contexts, specifically the value for multiple mediums to provide cessation advice and information. Interviewees living in remote First Nations communities, for example, stressed the important role of health care professionals in supporting patients by providing one-on-one advice, and using questions to check on and reinforce their understanding of the information. Additionally the use of mail as a method to deliver SSBS materials to surgical patients was suggested as a way to ensure that all patients received this information prior to surgery.
Discussion
The evaluation of SSBS program is one of the first reports of efforts to increase surgery-related smoking cessation in a setting where responsibility for surgical services is shared by health professionals in regional centers and outlying communities. The findings of this study point to successes as well as opportunities to strengthen the program.
One year following the introduction of the SSBS program, most participants reported exposure to a stop smoking before surgery message and these came from an average of almost 3 unique sources. This is notable given the lack of population density in the region in which the program was implemented, pointing to the benefit of having multiple partners collaborating across large geographic distances. Receipt of information about the benefits of stopping smoking before surgery from combined sources contributed to a significant model predicting those patients that reduced or quit smoking. Patient interviews further highlight the impact SSBS materials had on some surgical patients.
Comparisons of data collected pre- and post-SSBS implementation indicate no significant increase in the number of patients recalling being advised by a health care professional to stop smoking for surgery, as well as no significant reduction in smoking prevalence before surgery. As being advised by a health care professional was the second strongest predictor of reducing and/or quitting smoking before surgery post-SSBS, the lack of increase in being advised to quit for surgery between pre- and post-SSBS implementation is most likely the reason that we also fail to see a significant change in smoking. More than 40% of patients reduced their smoking but did not quit before surgery showing that patients were motivated, highlighting a missed opportunity and the need for additional support from health care professionals to enable a quit. Previous studies also report that rural physicians do not consistently provide smoking cessation assistance to patients.13-16 Our qualitative interviews reinforce these findings in that patients identified times when this advice and support could have been delivered by a health care professional and that they were surprised that it was not.
Interestingly, results indicate that at post-SSBS patients who received a stop smoking before surgery message from a health care professional were more likely than expected to have reduced or quit smoking before surgery, a finding not seen prior to the implementation of SSBS. Furthermore, those individuals advised to stop smoking before surgery at post-SSBS had a significantly higher Awareness of Smoking-Related Perioperative Complications score than both those that were advised, and those that were not advised, to quit smoking pre-SSBS. The importance of health care professionals in providing smoking cessation interventions has been previously reported.17-20 The present results suggest that the stop smoking before surgery message delivered by health care professionals as a result of this program may have been more effective than the message delivered prior to the introduction of the program. Providing surgery-specific resources and training to encourage discussion of the benefits of quitting with patients may have effectively supported the inclusion of surgery-specific reasons to quit in those discussions, which may in turn may have encouraged more patients to reduce or quit their smoking.
This study provides additional support that multiple component strategies enhance the delivery of smoking cessation treatments in primary care settings.21,22 For example, a theme running throughout interviews was that surgical patients found the SSBS resources to be a motivation within themselves, and these prompted their efforts to reduce and quit smoking. In addition, given that training has been positively correlated with intervention and cessation activities,23 strengthening brief intervention training for professionals may be particularly important in contexts where access to follow-up cessation support is challenging. Although online tobacco dependence treatment training programs provide health care professionals with access to training regardless of location, the need to improve the quality of these programs has been recognized.24 For the rural context, patients frequently mentioned one of the most effective ways to increase the delivery of this message beyond interactions with health care professionals was through mailing the SSBS materials to patients prior to surgery. Print materials mailed to patients on surgical waiting lists has been reported to effectively encourage patients to be abstinent for longer durations prior to their surgeries.25 Interestingly, patients’ reports of messages relayed by friends and family were the strongest contributor in a model predicting which patients quit/reduced smoking prior to surgery. As evaluating advice from friends/family was not a goal of the study, rates were not captured pre-SSBS for comparison; however, Webb et al25 found that more patients reported receiving advice from friends/family after an intervention involving mailing print materials to patients was initiated. It seems likely that friends and family who inadvertently see the messages to stop smoking before surgery become advocates and encourage patients to quit. The present finding also suggests that friends/family could be directly targeted in future as another avenue to better support patients in quitting smoking.
More work needs to be done to integrate smoking cessation resources and support as a standard of care for surgical patients at all stages of the surgical trajectory. The present SSBS program could have been enhanced if the assessment of smoking status and support for cessation were integrated into hospital protocols (eg, surgical booking procedures); however, at the time of this study our team lacked an avenue to make such changes within the two regional hospitals. Electronic health systems hold the potential to allow facilities to improve coordinated efforts by ensuring that that all patients are screened for tobacco use, all smokers are counselled to quit, and outcomes are documented. Other systematic approaches to providing information and resources to patients who smoke who are on waiting lists for elective surgery (eg, mailing print materials to all patients) should also be considered.
The study findings need to be considered in light of several limitations. The data were collected retrospectively and varying time frames between presurgery experiences and survey completion may have influenced recall. In addition, smoking patterns were based on self-report. The SSBS program was oriented to encouraging patients to stop smoking 6 to 8 weeks before surgery; as such we did not capture advice patients may have received prior to this time frame (eg, while on waitlists for surgery), nor whether patients were able to maintain their reduction or quit. In this study, we focused on patient outcomes and perspectives related to the SSBS program. Experiences of health care professionals may also be helpful in strengthening surgery-specific smoking cessation.
Conclusion
The SSBS program and the results of this evaluation provide a valuable information about the realities of promoting surgery-specific smoking cessation in regional centers serving dispersed populations. Despite the value of supporting a range of health care professionals in providing advice and support for cessation prior to surgery with training and appropriate resources, other strategies are needed to ensure that every surgical patient who smokes receives information about the benefits of quitting for surgery and is aware of available resources to assist with smoking cessation.
Acknowledgments
The authors would also like to recognize other members of the Stop Smoking Before Surgery team for their collective contributions to this project: Lucy Beck, Sherri Tillotson and Kelsey Yarmish from Northern Health; Sonia Lamont and El Taylor from the BC Cancer Agency, and Kerensa Medhurst and Cathy Adair from the Canadian Cancer Society.
Author Biographies
Joan L. Bottorff, PhD, FCAHS, FAAN, is a professor in the School of Nursing and director of the Institute for Healthy Living and Chronic Disease Prevention at the University of British Columbia. She is also a professorial fellow with the Faculty of Health Sciences, Australian Catholic University.
Cherisse L. Seaton, PhD, is a research coordinator for the Institute for Healthy Living and Chronic Disease Prevention at the University of British Columbia.
Nancy Viney is a registered nurse and Tobacco Reduction lead with Northern Health’s Population Health Team.
Sean Stolp, MA, is a data analyst for the Institute for Healthy Living and Chronic Disease Prevention at the University of British Columbia.
Sandra Krueckl, PhD, is the vice president of Cancer Control with the Canadian Cancer Society, BC and Yukon.
Nikolai Holm, Mphil, is a research assitant for the Institute for Healthy Living and Chronic Disease Prevention at the University of British Columbia.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was funded through Canadian Cancer Society (Grant No. 701259-01).
References
- 1. Oyston J. The role of anesthesiologists in promoting smoking cessation. Can J Anesth. 2011;58:897-901. [DOI] [PubMed] [Google Scholar]
- 2. Shi Y, Warner DO. Surgery as a teachable moment for smoking cessation. Anesthesiology. 2010;112:102-107. [DOI] [PubMed] [Google Scholar]
- 3. Bottorff JL, Seaton CL, Lamont S. Patients’ awareness of the surgical risks of smoking: implications for supporting smoking cessation. Can Fam Physician. In press. [PMC free article] [PubMed] [Google Scholar]
- 4. Stead LF, Buitrago D, Preciado N, Sanchez G, Hartmann-Boyce J, Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2013;5:CD000165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zaki A, Abrishami A, Wong J, Chung FF. Interventions in the preoperative clinic for long term smoking cessation: a quantitative systematic review. Can J Anesth. 2008;55:11-21. [DOI] [PubMed] [Google Scholar]
- 6. Sachs R, Wild TC, Thomas L, Hammal F, Finegan BA. Smoking cessation interventions in the pre-admission clinic: assessing two approaches. Can J Anesth. 2012;59:662-669. [DOI] [PubMed] [Google Scholar]
- 7. Thomsen T, Villebro N, Møller AM. Interventions for preoperative smoking cessation. Cochrane Database of Systematic Reviews. 2014;3:CD002294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Northern Health Authority. Position on tobacco reduction: an integrated population health approach. 2012. https://northernhealth.ca/Portals/0/About/PositionPapers/documents/TobaccoReductionPosition_V1_2012_01_31WEB.pdf. Accessed July 8, 2015.
- 9. Government of Canada. Canadian tobacco, alcohol and drugs survey. http://healthycanadians.gc.ca/science-research-sciences-recherches/data-donnees/ctads-ectad/index-eng.php. Updated February 3, 2015. Accessed July 8, 2015.
- 10. Coen SE, Oliffe JL, Johnson JL, Kelly MT. Looking for Mr. PG: Masculinities and men’s depression in a northern resource-based Canadian community. Health Place. 2013;21:94-101. [DOI] [PubMed] [Google Scholar]
- 11. Webb AR, Robertson N, Sparrow M. Smokers know little of their increased surgical risks and may quit on surgical advice. ANZ J Surg. 2013;83:753-757. [DOI] [PubMed] [Google Scholar]
- 12. Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerström Test for nicotine dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86:1119-1127. [DOI] [PubMed] [Google Scholar]
- 13. Ellerbeck EF, Choi WS, McCarter K, Jolicoeur DG, Greiner A, Ahluwalia JS. Impact of patient characteristics on physician’s smoking cessation strategies. Prev Med. 2003;36:464-470. [DOI] [PubMed] [Google Scholar]
- 14. Lum EY, Sharpe HM, Nilsson C, et al. Urban and rural differences in the management of asthma amongst primary care physicians in Alberta. Can J Clin Pharmacol. 2007;14:e275-e282. [PubMed] [Google Scholar]
- 15. Scott LD, LaSala KB, Lyndaker CZ, Neil-Urban S. Smoking cessation practices of rural and urban health care providers. Online J Rural Nurs Health Care. 2012;3:29-43. [Google Scholar]
- 16. Kruger J, Shaw L, Kahende J, Frank E. Health care providers’ advice to quit smoking, national health interview survey, 2000, 2005, and 2010. Prev Chronic Dis. 2012;9:E130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Aveyard P, Begh R, Parsons A, West R. Brief opportunistic smoking cessation interventions: a systematic review and meta-analysis to compare advice to quit and offer of assistance. Addiction. 2012;107:1066-1073. [DOI] [PubMed] [Google Scholar]
- 18. Hutcheson TD, Greiner KA, Ellerbeck EF, Jeffries SK, Mussulman LM, Casey GN. Understanding smoking cessation in rural communities. J Rural Health. 2008;24:116-124. [DOI] [PubMed] [Google Scholar]
- 19. Stead LF, Hartmann-Boyce J, Perera R, Lancaster T. Telephone counselling for smoking cessation. Cochrane Database Syst Rev. 2013;(8):CD002850. [DOI] [PubMed] [Google Scholar]
- 20. Nelms E, Wang L, Pennell M, et al. Trust in physicians among rural Medicaid-enrolled smokers. J Rural Health. 2014;30:214-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Papadakis S, McDonald P, Mullen K, Reid R, Skulsky K, Pipe A. Strategies to increase the delivery of smoking cessation treatments in primary care settings: a systematic review and meta-analysis. Prev Med. 2010;51:199-213. [DOI] [PubMed] [Google Scholar]
- 22. Papadakis S, McDonald PW, Pipe AL, Letherdale ST, Reid RD, Brown KS. Effectiveness of telephone-based follow-up support delivered in combination with a multi-component smoking cessation intervention in family practice: a cluster-randomized trial. Prev Med. 2013;56:390-397. [DOI] [PubMed] [Google Scholar]
- 23. Carson KV, Verbiest ME, Crone MR, et al. Training health professionals in smoking cessation. Cochrane Database Syst Rev. 2012;(5):CD000214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Selby P, Goncharenko K, Barker M, et al. Review and evaluation of online tobacco dependence treatment training programs for health care practitioners. J Med Internet Res. 2015;17:e97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Webb AR, Robertson N, Sparrow M, Borland R, Leong S. Printed quit-pack sent to surgical patients at time of waiting list placement improved perioperative quitting. ANZ J Surg. 2014;84:660-664. [DOI] [PubMed] [Google Scholar]