Abstract
The treatment of brain abscesses in newborn infants is controversial. We report on a 6-week-old infant with multiple brain abscesses caused by Citrobacter koseri that resolved after treatment with combined surgical drainage and intravenous therapy with meropenem and fosfomycin.
Keywords: Newborn infant, Citrobacter koseri, Brain abscess, Fosfmycin, Meropenem
Introduction
Citrobacter koseri is a particular cause of meningitis and abscess especially during the neonatal period associated with high mortality and morbidity. Neonatal Citrobacter disease is mostly considered sporadic, however vertical transmission during delivery and other healthcare linked spread may occur. Since abscesses may grow very large in neonates before manifesting clinical signs, neuroimaging studies are pivotal for diagnosis and prediction of adverse complication as early as possible [1].
Case report
Our patient was a male baby born after 37 weeks gestation with a birth weight of 2140 g. Delivery was by Cesarean section because of preeclampsia, Apgar score was 9 and 10 at 1 and 5 min. The infant was admitted to the neonatal unit because of hypoglycemia. Initial blood workup showed elevated interleukin-6 of 425 ng/l (normal value: <50 ng/l) and empiric antimicrobial therapy with ampicillin and gentamicin was started. Upon the negative result of blood culture, the antimicrobial therapy was discounted after 5 days. Because of a good response to treatment, there was no lumbar puncture performed. The slow oral intake und hypoglycemia was accepted for low birth weight and he was discharged at 11 days of age.
At 4 weeks of age, the infant presented to our emergency room with irritability and fever (38.5 °C). He had leukocytosis (20.54/nl) and elevated C-reactive protein (CRP) of 17.8 mg/l (normal value: <5 mg/l). A urinalysis was negative and blood culture was negative. Lumbar puncture was not considered at that time. No antimicrobials were started and he was discharged well after 2 days.
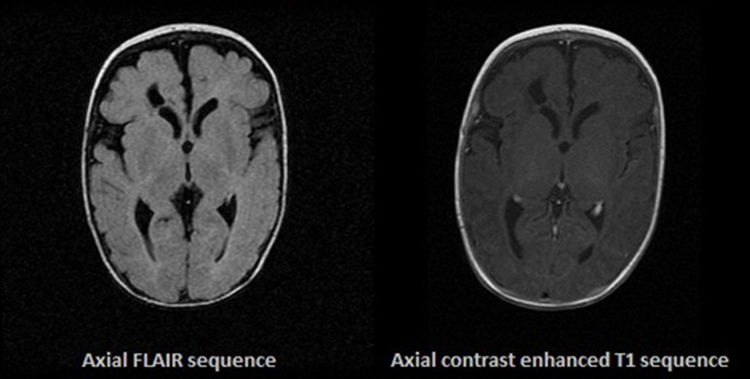
Two weeks later, the infant presented with irritability, sub-febrile a temperature of 38.0 °C and poor oral intake for 1 day. Initial physical examination was normal and there was no focal neurological deficit. No antimicrobials had been given prior to admission. Because of the child's presentation, a full sepsis workup was done. The infant had a C-reactive protein of 13.20 mg/l. The blood and cerebrospinal fluid (CSF) cultures were negative for bacterial growth, and there was no pleocytosis. A head ultrasound examination revealed 2 fluid filled cavities in the frontal region (Fig. 1). Magnetic resonance imaging (MRI) of the head was suggestive of brain abscesses (Fig. 2).
Fig. 1.

Cranial ultrasound imaging showing 2 fluid filled cavities in the frontal region.
Fig. 2.
Cranial MRI showing 2 cerebral abscesses.
Empiric therapy was initiated with ampicillin, gentamicin and cefotaxime. The infant underwent burr-hole drainage of the right frontal abscess cavity at day 3 of admission and approximately 6 ml of yellow-colored sero-sanguineous fluid was drained. The culture of the abscess fluid grew C. koseri. After review of literature addressing C. koseri infections, ampicillin, gentamicin and cefotaxime were discontinued and intravenous meropenem (120 mg/kg/d) at day 12 of admission was started. After the bacteria isolated were found to be sensitive to this drug, intravenous fosfomycin was added at a dose of 120 mg/kg/d at day 18 of admission.
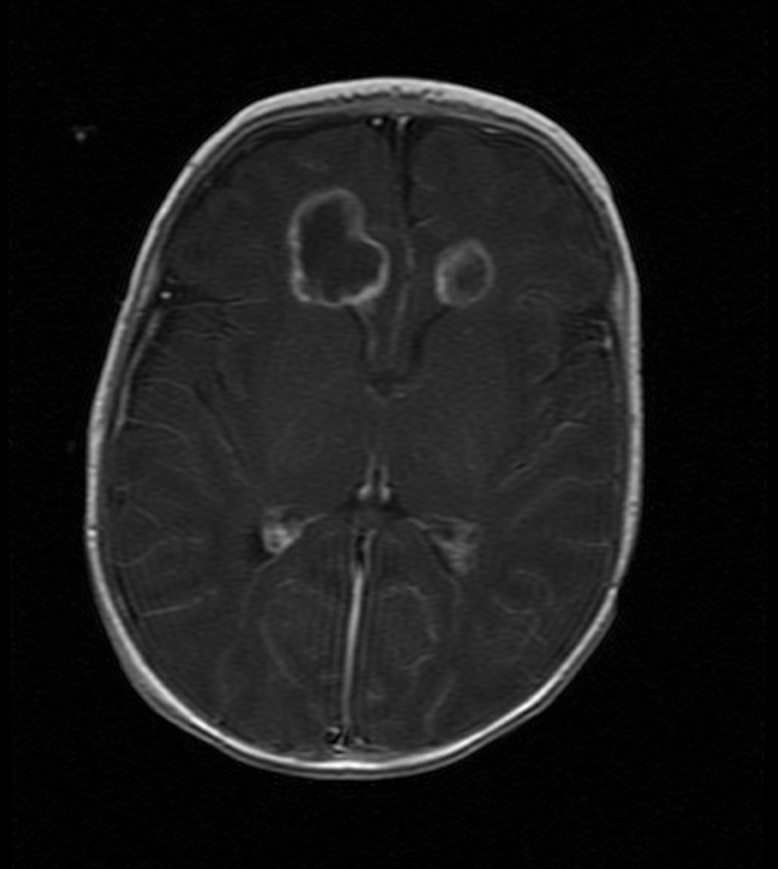
Repeated ultrasound of the head revealed resolution of the abscesses at day 24 of admission. After a total of 6 weeks antimicrobial therapy was discontinued and the infant was discharged. MRI at the time of discharge showed a cystic defect in the right frontal lobe and a complete resolution of the abscess in the left frontal lobe (Fig. 3).
Fig. 3.
Cranial MRI showing no residuals from the cerebral abscesses.
At 9-month follow up, the patient was found in a good clinical condition, with only mild delay in gross motor skills, but with normal vision and hearing. By elective orchidopexy at age of 2 years, the patient was seen with a mild speech delay, but other aspects of development were appropriate for age.
Discussion
A bacterial brain abscess is usually a well-circumscribed collection of purulent fluid within the brain parenchyma. Certain gram-negative bacteria have a predilection for causing brain abscess, including Acinetobacter, C. Enterobacter, Salmonalle, Serratia, Proteus and Pseudomonas [2].
During the first 2 months of life, C. koseri shows a strong predilection for meningitis and brain abscesses. The mortality rate for meningitis due to Citrobacter is around 30%, and of infants who survive, more than 80% have some degree of neurological deficit [1].
Organisms of the genus Citrobacter are gram-negative bacilli of the family Enterobacteriaceae, tribe Citrobactereae [1]. The pathogenesis of Citrobacter meningitis and brain abscess in humans is still not clear. During experimental central nervous system (CNS) infection in neonatal rats, C. koseri resides primarily intracellularly within macrophages and neutrophils. Accumulation of necrotic tissue and infiltrating phagocytes results in expansion of the brain abscess [3]. Some instances of intraparenchymal abscesses do not follow the classic pattern of common cerebral abscesses and lack a fibrous capsule [4].
In our case, the source of infection could not be determined as the infant became symptomatic at age of 4 weeks, so vertical transmission from the mother during delivery is unlikely. She was asymptomatic throughout her pregnancy and there was no sign of vaginal or intestinal infection or chorioamnionitis. In general, Citrobacter infections occur in a sporadic fashion [1]. Almost one-third of the sporadic cases are of late onset, typically occurring around 4–5 weeks, compared with early onset cases, which tend to occur between 5 and 12 days of age. No cases of brain abscess have been reported in vertically transmitted Citrobacter meningitis [5]. Approximately one-third of the affected patients are less than 36 weeks gestational age at birth, suggesting that preterm infants have an increased risk of acquiring Citrobacter infection [1].
The clinical manifestations of C. koseri meningitis include poor feeding, vomiting, lethargy, apneic spells, seizures, irritability and bulging fontanelle. Some infants who have brain abscess initially may exhibit no apparent neurologic symptoms other than increased irritability as has been described in our case. Neurologic deficits are less obvious in extremely preterm infants [2]. Infants with such signs and symptoms should have a complete evaluation, including blood culture, urine culture, and lumbar puncture for CSF chemistries, cytology, gram staining and culture. Once the diagnosis of C. koseri meningitis is established, all infants should undergo serial neuroimaging evaluation. Ultrasonography can be used for initial screening [4] but MRI is the diagnostic method of choice.
Repeat imaging examination may be helpful at the conclusion of therapy [1]. It is not clear whether serial neuroimaging at first admission at the age of 4 weeks in our case could have been beneficial to pick up brain abscesses earlier.
The optimal management of Citrobacter CNS abscesses is antimicrobial therapy alone or a combination of antimicrobial therapy and surgical aspiration/drainage [4], [6]. The unique characteristics of C. koseri, including localization in neutrophils and rapid CSF penetration, allow bacterial survival and replication despite treatment with commonly used antimicrobial agents for meningitis. According to in vitro antimicrobial sensitivity aminoglycosides, ciprofloxacin, meropenem, and imipenem/cilastatin are active against more than 90% of Citrobacter isolates [7]. Aminoglycosides, however, do not achieve adequate concentrations in the brain and C. koseri is usually ampicillin-resistant [1]. In our case, initially we started with the third-generation cephalosporin cefotaxime, but after reviewing the literature we switched the therapy to meropenem. However, the evidence to date seems rather sparse to recommend carbapenems in favor of third-generation cephalosporins without evaluation or proof of real antimicrobial resistance in individual cases [6].
The ability of carbapenems to penetrate CSF and macrophages makes those drug a logical option to treat Citrobacter infection. Meropenem appears to have a better safety profile and thus would be the preferred choice in neonates [7]. Lee et al. had reported a case of Lemierre syndrome complication multiple brain abscesses caused by extended-spectrum beta-lactamase-producing Klebsiella pneumonia which responded very well to fosfomycin and meropenem [8]. In the presented case, we added fosfomycin because its well-known bactericidal activity against gram negative pathogens including C. koseri and especially multidrug-resistant organisms [8], [9].
Surgical drainage is probably desirable but is not mandatory in every case. Abscesses are often multiple or inaccessible, making a surgical approach impractical. The neurosurgical approach may be associated with a better prognosis [4]. In our patient, a complete regression of cerebral abscesses was reached after the aspiration of abscess and the introduction of meropenem and fosfomycin antimicrobial scheme.
Duration of seizures for more than 72 h, presence of coma, use of inotropes, and leukopenia have been reported to be the most important predictors of adverse outcome [10]. Gram negative ancillary meningitis was associated with worse prognosis comparing with those caused by gram-positive organisms [11]. Favorable outcomes have been reported [6] as also seen in our case. We suggest that meropenem in combination with fosfomycin as well as surgical drainage have probably attributed to a good outcome of our patient. Long-term neurodevelopment follow up and neuroimaging studies are indicated.
References
- 1.Doran T.I. The role of Citrobacter in clinical disease of children: review. Clin Infect Dis. 1999;28:384–394. doi: 10.1086/515106. [DOI] [PubMed] [Google Scholar]
- 2.Stallworth L., Mani C., Murry D. Index of suspicion in the nursery. Neoreviews. 2005;6:e436–e438. [Google Scholar]
- 3.Townsend S.M., Pollak H.A., Gonzalez-Gomez I., Shimada H., Badger J.L. Citrobacter koseri brain abscess in the neonatal rat: survival and replication within human and rat macrophages. Infect Immun. 2003;71:5871–5880. doi: 10.1128/IAI.71.10.5871-5880.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martínez-Lage J.F., Martínez-Lage Azorín L., Almagro M.J., Bastida M.E., Reyes S., Tellez C. Citrobacter koseri meningitis: a neurosurgical condition? Eur J Paediatr Neurol. 2010;14:360–363. doi: 10.1016/j.ejpn.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 5.Papasian C.J., Kinney J., Coffman S., Hollis R.J., Pfaller M.A. Transmission of Citrobacter koseri from mother to infant documented by ribotyping and pulsed-field gel electrophoresis. Diagn Microbiol Infect Dis. 1996;26:63–67. doi: 10.1016/s0732-8893(96)00177-0. [DOI] [PubMed] [Google Scholar]
- 6.Straussberg R., Harel L., Amir J. Long term outcome of Citrobacter koseri meningitis treated with imipenem/meropenem and surgical drainage. Infection. 2001;9:280–282. doi: 10.1007/s15010-001-1136-4. [DOI] [PubMed] [Google Scholar]
- 7.McPherson C., Gal P., Ransom J.L. Treatment of Citrobacter koseri infection with ciprofloxacin and cefotaxime in a preterm infant. Ann Pharmacother. 2008;42:1134–1138. doi: 10.1345/aph.1L008. [DOI] [PubMed] [Google Scholar]
- 8.Lee W.S., Wang F.D., Shieh Y.H., Teng S.O., Ou T.Y. Lemierre syndrome complicating multiple brain abscesses caused by extended-spectrum β-lactamase-producing Klebsiella pneumoniae cured by fosfomycin and meropenem combination therapy. J Microbiol Immunol Infect. 2012;45:72–74. doi: 10.1016/j.jmii.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 9.Falagas M.E., Kastoris A.C., Kapaskelis A.M., Karageorgopoulos D.E. Fosfomycin for the treatment of multidrug-resistant, including extended-spectrum beta-lactamase producing Enterobacteriaceae infections: a systemic review. Lancet Infect Dis. 2010;10:43–50. doi: 10.1016/S1473-3099(09)70325-1. [DOI] [PubMed] [Google Scholar]
- 10.Klinger G., Chin C.N., Beyene J., Perlman M. Predicting the outcome of neonatal bacterial meningitis. Pediatrics. 2000;106:477–482. doi: 10.1542/peds.106.3.477. [DOI] [PubMed] [Google Scholar]
- 11.May M., Daley A.J., Donath S., Isaacs D., Australasian Study Group for Neonatal Infections Early onset neonatal meningitis in Australia and New Zealand, 1992–2002. Arch Dis Child Fetal Neonatal Ed. 2005;90:F324–F327. doi: 10.1136/adc.2004.066134. [DOI] [PMC free article] [PubMed] [Google Scholar]