Abstract
Dirofilaria repens, a filarial nematode of dogs and other carnivores, can accidentally infect humans. The infection occurs widely throughout Europe. We report a case of D. repens in a Danish woman who had been traveling to Crete. A nematode was visualized on examination and ELISA was positive for antibodies against D. repens.
Keywords: Dirofilaria repens, Travel, Denmark, Europe, Human
Introduction
Dirofilaria repens is a filarial nematode transmitted by mosquitoes that primarily affects dogs and other carnivores. The adult worms are found in the subcutaneous tissues of dogs and other animals and the adult filariae deposit microfilariae in the blood of the host. Mosquitoes ingest the first-stage larve with a blood meal from the infected host, which develop into the infective third-stage filariform larvae. When the third stage larva have matured and are found in the salivary glands of the mosquito, the infection can be transmitted to the next animal including humans from which the mosquito take the next blood meal. The incubation period in the vertebrate host is 6–8 months [1] (Fig. 1).
Fig. 1.
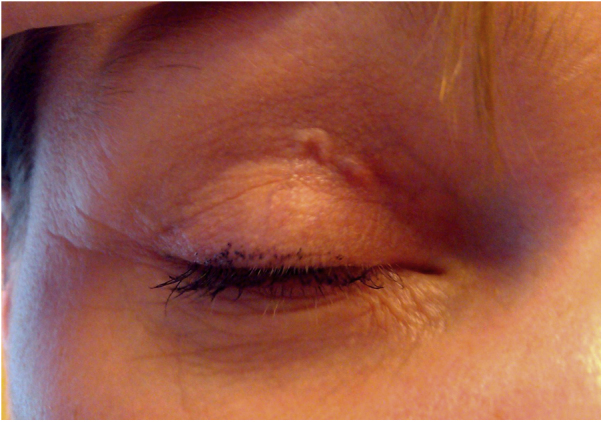
The worm was seen at the upper eyelid on the day of admission.
Incidental human infection can manifest as a single subcutaneous nodule. Migration of the worm may result in local swellings with changing localization. The majority of cases are found on the upper half of the body, mainly around the eyes [1]. Severe clinical manifestations have also been reported and may affect organs including the brain and lungs [2].
Infections have been reported from various regions of the world, mainly Europe, Africa, Middle East and Asia. Areas in Europe where D. repens has been solidly established include countries of the Mediterranean region where the warmer climate facilitates the development of infectious larvae in mosquitoes [3]. Studies from Russia and northern Germany found that the geographical distribution is expanding [1], [4]. So far there are no data from Denmark.
Case report
A 39-year-old Danish woman was seen in January 2014 referred by an ophthalmologist on suspicion of a larval infestation around the right eye.
Symptoms began suddenly one week before referral. The patient had noticed a larvae moving under the skin around the right eye with redness and swelling of the skin. Periodically, the structure disappeared. Severe headache in the right temporal area occurred when the structure disappeared.
The patient had visited Crete in August 2013 and had never traveled outside Europe. In September 2013 the patient had noticed a subcutaneous nodule on her left leg. The patient lives on a farm and has a dog.
On examination a larva was seen moving across the right upper eyelid. MRI of the right orbit did not demonstrate any abnormalities. The MRI was performed four days after the patient were first seen and after start of albendazole treatment. There was no eosinophilia and IgE was normal. Toxocara antibody titer was negative, but there was a positive filarial antibody titer, using Dirofilaria immitis as antigen.
Serum was sent to the Rostov Scientific Research Institute of Microbiology and Parasitology, Rostov-on-Don, Russia, for determination of specific antibodies against D. repens, which has developed an ELISA for the detection of Dirofilaria-specific antibodies based on purified somatic antigen of immature female D. repens removed from human cases [1]. The test was found positive for D. repens-specific antibodies. ELISA tests with echinococcus, toxocarosis and trichinellosis antigens were performed, and they were all negative. The patient's dog was tested negative for microfilariae in the blood.
Antihelminthic treatment with albendazole 400 mg twice daily orally for 5 days was initiated and the patient recovered rapidly.
On the day of admission we send the patient to an ophthalmologist for surgical removal of the worm. The diagnosis may be achieved parasitological when a living and intact worm can be extracted. Unfortunately it could not be removed.
Discussion
This is the first reported case of human infection with D. repens in Denmark, probably imported from Crete.
In Greece the prevalence of dirofilariasis in dogs caused by D. repens infection has been estimated to range between 6.7% and 22% [5]. During the last years cases of human dirofilariasis have also been reported from countries farther north, including Austria, Poland and Germany [6], [7], [8]. However, with the increasing prevalence of D. repens in northern Germany infection in Denmark is another possibility as D. repens may be present in Danish canines. In February 2014 dogs and mosquitoes have been found positive with D. repens in northern Germany and a case of human D. repens was reported [3], [6]. The climate change and increased translocation of dogs might be responsible for the spread to the north [9].
It is surprising that both the eosinophil count and IgE were normal, as these parameters are usually elevated in invasive nematode infections. However, we believe that it reflects that the patient only had a single nematode and that it caused modest local inflammation and thus failed to elicit eosinophilia and an increase IgE. Indeed in a large case series from Russia eosinophilia was found in only 38% of cases (IgE were not measured) [1].
Although this is the only case reported from Denmark, infection with D. repens probably occurs more frequently and is either unrecognized or misdiagnosed. In 2013 67.4% of the Danish population traveled by air outside Denmark [11], [12]. Patients who traveling in Europe should consider limit their exposure to mosquitoes and protect themselves from bites.
In conclusion a subcutaneous dirofilariasis should be considered as a differential diagnosis in patients who presents with a subcutaneous nodules or a migrating larva.
Conflicts of interest
None of the authors have any conflicts of interest to declare.
Acknowledgments
The authors wish to thanks Rostov Scientific Research Institute of Microbiology and Parasitology in Russia for providing results of ELISA testing. The authors are grateful to the patient for letting us sharing her picture.
References
- 1.Ermakova L.A., Nagorny S.A., Krivorotova E.Y., Pshenichnaya N.Y., Matina O.N. Dirofilaria repens in the Russian Federation: current epidemiology, diagnosis, and treatment from a federal reference center perspective. Int J Infect Dis. 2014;23:47–52. doi: 10.1016/j.ijid.2014.02.008. [DOI] [PubMed] [Google Scholar]
- 2.Poppert S., Hodapp M., Krueger A., Hefasy G., Niesen W., Kern W.V. Dirofilaria repens infection and concomitant meningoencephalitis. Emerg Infect Dis. 2009;15:1844–1845. doi: 10.3201/eid1511.090936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Genchi C., Kramer L.H., Rivasi F. Dirofilarial infections in Europe. Vector Borne Zoonotic Dis. 2011;11:1307–1317. doi: 10.1089/vbz.2010.0247. [DOI] [PubMed] [Google Scholar]
- 4.Czajka C., Becker N., Jöst H., Poppert S., Schmidt-Chanasit J., Krüger A. Stable transmission of Dirofilaria repens nematodes Northern Germany. Emerg Infect Dis. 2014;20:329–331. doi: 10.3201/eid2002.131003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tzanetou K., Gasteratos S., Pantazopoulou A., Gogou C., Konidaris D., Fragia K. Subcutaneous dirofilatiasis caused by Dirofilaria repens in Greece: a case report. J Cutan Pathol. 2009;36:892–895. doi: 10.1111/j.1600-0560.2008.01144.x. [DOI] [PubMed] [Google Scholar]
- 6.Tappe D., Plauth T., Muntau B., Diessel L., Tannich E., Herrmann-Trist P. A case of autochthonous human Dirofilaria infection, Germany March 2014. Euro Surveill. 2014;19(17) pii=20790. [PubMed] [Google Scholar]
- 7.Cielecka D., Zarnowska-Prymek H., Masny A., Saalamatin R., Wesolowska M., Golab E. Human dirofilariosis in Poland: the first cases of autochthonous infections with Dirofilaria repens. Ann Agric Environ Med. 2012;19:445–450. [PubMed] [Google Scholar]
- 8.Salamatin R.V., Pavlikovska T.M., Sagach O.S., Nikolayenko S.M., Kornyushin V.V., Kharchenko V.O. Human dirofilariasis due to Dirofilaria repens in Ukraine, an emergent zoonosis epidemiological report of 1465 cases. Acta Parasitol. 2013;58:592–598. doi: 10.2478/s11686-013-0187-x. [DOI] [PubMed] [Google Scholar]
- 9.Genchi C., Mortarino M., Rinaldi L., Cringoli G., Traldi G., Genchi M. Changing climate and changing vector-borne disease distribution: the example of Dirofilaria in Europe. Vet Parasitol. 2011;176:295–299. doi: 10.1016/j.vetpar.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 11.Statistics Denmark-statbank.dk . 2014. Population statistics. Available at: http://www.dst.dk/pukora/epub/Nyt/2014/NR427.pdf [accessed August 2014] [Google Scholar]
- 12.Nielsen U.S., Larsen C.S., Howitz M., Petersen E. Hepatitis A among Danish travellers 1980–2007. J Infect. 2009;58:47–52. doi: 10.1016/j.jinf.2008.10.010. [DOI] [PubMed] [Google Scholar]


