Abstract
Objectives
Female genital fistula remains a public health concern in developing countries. From January 2007 to September 2013, the Fistula Care project, managed by EngenderHealth in partnership with the Ministry of Health and supported by USAID, integrated fistula repair services in the maternity wards of general hospitals in Guinea. The objective of this article was to present and discuss the clinical outcomes of 7 years of work involving 2116 women repaired in three hospitals across the country.
Methods
This was a retrospective cohort study using data abstracted from medical records for fistula repairs conducted from 2007 to 2013. The study data were reviewed during the period April to August 2014.
Results
The majority of the 2116 women who underwent surgical repair had vesicovaginal fistula (n = 2045, 97%) and 3% had rectovaginal fistula or a combination of both. Overall 1748 (83%) had a closed fistula and were continent of urine immediately after surgery. At discharge, 1795 women (85%) had a closed fistula and 1680 (79%) were dry, meaning they no longer leaked urine and/or faeces. One hundred and fifteen (5%) remained with residual incontinence despite fistula closure. Follow-up at 3 months was completed by 1663 (79%) women of whom 1405 (84.5%) had their fistula closed and 80% were continent. Twenty-one per cent were lost to follow-up.
Conclusion
Routine programmatic repair for obstetric fistula in low resources settings can yield good outcomes. However, more efforts are needed to address loss to follow-up, sustain the results and prevent the occurrence and/or recurrence of fistula.
Objectifs
La fistule génitale féminine reste un problème de santé publique dans les pays en développement. De janvier 2007 à septembre 2013, le projet Fistula Care, géré par Engender Health en partenariat avec le Ministère de la Santé et soutenu par l’USAID, a intégré les services de réparation de fistules dans les maternités des hôpitaux généraux en Guinée. L'objectif de cet article est de présenter et de discuter les résultats cliniques de sept années de travail impliquant 2116 femmes traitées dans trois hôpitaux à travers le pays.
Méthodes
Il s'agit d'une étude de cohorte rétrospective utilisant des données extraites des dossiers médicaux de réparations de fistules menées de 2007 à 2013. Les données de l’étude ont été analysées au cours de la période allant d'avril à août 2014.
Résultats
La majorité des 2116 femmes qui ont subi une réparation chirurgicale avaient une fistule vésico vaginale (n = 2 045, 97%) et 3% avaient une fistule recto vaginale ou une combinaison des deux. Au total, 1748 (83%) femmes ont eu leur fistule refermée et sont devenues continentes d'urine immédiatement après la chirurgie. À la sortie, 1795 femmes (85%) avaient une fistule fermée et 1680 (79%) étaient sèches, c'est à dire qu'elles n'avaient plus de fuite d'urine et/ou de matières fécales. 115 (5%) femmes avaient toujours une incontinence résiduelle malgré la fermeture de la fistule. Le suivi à trois mois a été complété par 1663 (79%) femmes dont 1405 (84,5%) ont eu leur fistule fermée et 80% étaient continentes. 21% ont été perdues au suivi.
Conclusion
La réparation programmatique de routine de la fistule obstétricale dans les régions à faibles ressources peut donner de bons résultats. Toutefois, davantage d'efforts sont nécessaires pour remédier à la perte au suivi, maintenir les résultats et prévenir l'apparition et/ou la réapparition de fistules.
Objetivos
La fístula genital femenina continúa siendo una preocupación de salud pública en países en vías de desarrollo. Entre Enero 2007 y Septiembre 2013, el proyecto Fistula Care, manejado por EngenderHealth junto con el Ministerio de Salud de Guinea, y financiado por USAID, integró los servicios de reparación de fistula en las maternidades de hospitales generales en Guinea. El objetivo de este artículo es presentar y discutir los resultados clínicos de 7 años de trabajo con 2116 mujeres intervenidas en tres hospitales del país.
Métodos
Estudio retrospectivo de cohortes utilizando datos tomados de historias clínicas de reparaciones de fístula realizadas entre el 2007 y el 2013. Los datos del estudio se revisaron durante el periodo entre Abril y Agosto 2014.
Resultados
La mayoría de las 2116 mujeres que se sometieron a la reparación quirúrgica tenían una fistula vesico-vaginal (n = 2045, 97%) y 3% tenían una fístula recto-vaginal o una combinación de ambas. En general, 1748 (83%) tenían la fístula cerrada y eran continentes inmediatamente después de la cirugía. En el momento del alta, 1795 mujeres (85%) tenían la fistula cerrada y 1680 (79%) estaban secas, es decir que ya no perdían orina y/o heces. 115 (5%) continuaron teniendo incontinencia residual a pesar de que la fistula estaba cerrada. El seguimiento a los tres meses se completó para 1663 (79%) mujeres, de las cuales 1405 (84.5%) tenían la fistula cerrada y 80% eran continentes. Un 21% fueron perdidas durante el seguimiento.
Conclusión
La reparación rutinaria programada de la fístula obstétrica en lugares con pocos recursos puede dar buenos resultados. Sin embargo, se requieren más esfuerzos para resolver la pérdida durante el seguimiento, mantener los resultados y prevenir la aparición y/o reaparición de la fístula.
Keywords: obstetric fistula, Guinea, fistula care, operational research, SORT-IT
Introduction
Female genital fistula is a serious medical condition in which a perforation develops either between most commonly bladder and vagina [vesicovaginal fistula (VVF)], between rectum and vagina [rectovaginal fistula (RVF)] or a combination of both. It occurs most commonly after prolonged labour when the head of the unborn child compresses the birth canal and leads to tissue necrosis 1,2. More rarely, fistula may be caused by genital cutting such as yankan gishiri, sexual violence, iatrogenic reasons (from c-section, hysterectomy or poorly performed abortions), pelvic fractures, and malignancy or radiation 3–5. Female genital fistula is no longer prevalent in the developed world, but remains a common public health concern in developing countries 6,7. There are no good estimates of the burden of fistula, but the most recent estimates of its prevalence range from one to two million worldwide, based on reviews by Stanton et al. and Adler et al. 8,9.
In Guinea, 0.6% of women experienced obstetric fistula in their lifetime 10. As in many other resource-limited settings, the local capacity to diagnose and to perform surgical repair is very limited. Up to 2006, only the Department of Urology of the Ignace Deen Hospital was recognised and was performing quality surgical repair for female genital fistula in Guinea. In 2007, EngenderHealth (an international reproductive health non-governmental organisation) helped to establish and strengthen three additional centres for fistula management in Guinea, of which three continued to perform surgical repair up to the end of this project in 2013.
While immediate post-operative closure rates for obstetric fistula can be as high as 90% 11,12, this rate varies by repair centre and other factors such as the size of fistula, surgeon's experience, pre-operative bladder size, degree of vaginal scarring, degree of urethral involvement and number of previous repairs 13,14. Although urinary continence is not always achieved immediately after surgical repair even with closure of the fistula, residual incontinence can improve or be resolved with time 15. Repair breakdown can happen as a consequence of inadequate post-operative care or poor catheter management and has been reported following hospital discharge, for reasons including heavy work, sexual intercourse, wound infections and at the subsequent pregnancy in case of prolonged labour or poor management of vaginal delivery 16.
Many published studies have reported on fistula characteristics, risk factors and outcomes of repair from different settings 11,12,17–20. However, all previous studies in West Africa either focused on outcomes at discharge or most used a relatively small sample size from one repair centre 21,22. This study assesses the characteristics of more than 2000 women and their clinical outcomes after fistula repair from three local repair hospitals across Guinea. Routine programme data could yield useful and reliable information to guide future fistula programmes in Guinea.
Using data on women who underwent surgical repair of female genital fistula at three hospitals in Guinea with repair services supported by Fistula Care, we report on (i) the demographic and clinical characteristics of patients; (ii) the number and proportion of fistula types; and (iii) the outcomes of the treatment up to 3-month follow-up (fistula closed and dry, fistula closed with residual incontinence and fistula not closed) stratified by fistula type, number of previous repairs, duration of fistula and year of repair at the time of hospital discharge.
Methods
Study design
This was a retrospective cohort study using data abstracted from medical records for fistula repairs conducted from 2007 to 2013.
Setting
Guinea is a West African country with a population of about 12 million 6. It is among the poorest countries in the world with the majority (65%) of the population living in rural areas. Health indicators are poor including a maternal mortality ratio of 724 per 100 000 live births 10.
Fistula Care supported both prevention and treatment, with a focus on treatment at three geographically dispersed centres, as well as reintegration of fistula patients into the community. The three centres that continued with repairs during the Fistula Care project are integrated within the maternity unit of hospitals in geographically dispersed regions of Guinea (Jean Paul II Hospital in Conakry, the Regional Hospital of Labé and the Prefectoral Hospital of Kissidougou).
Building capacity included ongoing training of surgeons, training of nursing staff, counselling training, quality improvement, medical monitoring, equipment provision and mentorship for continuous skills building 23. Surgeons from the Geneva Foundation for Medical Education and Research (GFMER) travelled to Guinea on a quarterly basis to lead training sessions and monitor progress of trainees. Sixteen Guinean local surgeons received training with support from Fistula Care. They attended an average of 22 training sessions, with 12 continuing to provide surgery after the Fistula Care ended. Each centre was staffed by two or three surgeons, an anaesthetist, a counsellor and two to four nurses all trained in fistula prevention and management. Community awareness campaigns on fistula and the availability of fistula management services were conducted regularly through collaboration with rural radio, community leaders and community volunteers (village safe motherhood committees).
The three centres collectively performed on average 300–400 surgical repair operations per year. Treatment in the centres was free and included assessment and surgical repair by a surgeon, and counselling about exercises, family planning methods and restrictions on sexual intercourse and heavy labour during the healing period.
For each woman, surgical outcomes (fistula closed and dry, fistula closed with residual incontinence and fistula not closed) were assessed immediately after surgery, at hospital discharge and 3 months later. Women with a fistula that was not closed at the time of the follow-up visit were usually scheduled for another repair surgery. Patients were considered lost to follow-up if they failed to attend the follow-up appointment within 6 months of their discharge for reasons that could include residence out of the country, death and farming.
The fistula was considered not closed (immediately after surgery or in the case of initial closure breakdown within 3 months of surgery) if the woman reported an uncontrolled and continuous leakage of urine. Residual incontinence, some incontinence remaining despite fistula closure, could be urge, stress or overflow incontinence. The woman was considered dry if the fistula was closed and there was no leakage of urine or faeces.
Study population and participants
We included all women who underwent fistula repair surgery in each of the three sites between 1 January 2007 and 30 September 2013.
Data variables, source of data and data collection
The sociodemographic and clinical characteristics of fistula patients were extracted from patient files and included age at admission in the repair site, marital status, age at marriage, occupation, level of education, residence (rural/urban), parity, number of previous repairs, duration of fistula, mode of delivery causing fistula, neonatal outcome at causal delivery and type of fistula (VVF, RVF or both). Treatment outcomes (fistula closed and dry, fistula closed with residual incontinence and fistula not closed) were assessed by a dye test immediately after surgery, at the time of hospital discharge and at 3-month follow-up visit in most, but not all cases. Data were sourced from patients' files, kept at each fistula care repair hospital, using structured forms. Patient files were reviewed between April and August 2014.
Data analysis
Collected data were double-entered by two independent encoders into EpiData Entry software (version 3.1; EpiData Association, Odense, Denmark). The two data files were compared and discordances resolved by cross-checking with the data collection forms. Data were analysed using STATA 13 software (STATA Corporation, College Station, TX, USA). Frequencies (%) were calculated to describe patients' characteristics and treatment outcomes. Pearson's chi-square (χ2) was used to compare proportions of treatment outcomes for selected variables with a level of significance set at P = 0.05 and a 95% confidence intervals.
Ethics
Ethics approval was obtained from the Guinean National Ethics Committee for Health Research, the MSF Ethics Review Board (Geneva, Switzerland) and the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease, Paris, France.
Results
Sociodemographic and clinical characteristics
Overall 2116 women underwent surgical repair for female genital fistula at the three repair hospitals. The demographic and clinical characteristics of these women are presented in Table1. The median age at presentation was 32 years (interquartile range (IQR) 25–40). The majority of women (n = 2045, 97%) had vesicovaginal fistula and 3% had rectovaginal fistula or a combination of both. Half of the women were married before the age of 17 years and 29% developed the fistula at their first pregnancy and 1978 women (93%) had stillbirths for the referent pregnancy. Almost one of five women had the fistula for 5 years or more at the time they came to the hospital for repair.
Table 1.
Demographic and clinical characteristics of women who underwent fistula repair in hospitals supported by Fistula Care in Guinea, 2007 to 2013
| Variables | Number (%) |
|---|---|
| Total | 2116 |
| Age at presentation to repair centre (in years) | |
| <17 | 63 (3.0) |
| 17–24 | 402 (19.0) |
| 25–49 | 1293 (61.1) |
| ≥50 | 326 (15.4) |
| Unknown | 32 (1.5) |
| Marital status | |
| Single | 82 (3.9) |
| Married/Union | 1442 (68.1) |
| Separated | 378 (17.9) |
| Widow | 189 (8.9) |
| Unknown | 25 (1.2) |
| Age at marriage (in years) | |
| <17† | 1212 (57.3) |
| ≥17 | 279 (13.2) |
| Unknown | 625 (29.5) |
| Occupation | |
| Housewife | 2026 (95.7) |
| Worker | 65 (03.1) |
| Unknown | 25 (1.2) |
| Education | |
| None | 1896 (89.6) |
| Primary | 99 (4.7) |
| Secondary and higher | 22 (1.0) |
| Unknown | 99 (4.7) |
| Residence | |
| Rural | 1912 (90.4) |
| Urban | 195 (09.2) |
| Unknown | 9 (0.4) |
| Parity | |
| 1 birth | 625 (29.5) |
| 2–5 births | 950 (44.9) |
| ≥6 birth | 510 (24.1) |
| Unknown | 31 (1.5) |
| Previous repairs attempts | |
| 0 | 1219 (57.6) |
| 1 | 514 (24.3) |
| 2 | 236 (11.1) |
| ≥3 | 107 (5.1) |
| Unknown | 40 (1.9) |
| Duration of fistula (in years) | |
| ≤1 | 405 (19.1) |
| 2 to 4 | 448 (21.2) |
| ≥5 | 1017 (48.1) |
| Unknown | 246 (11.6) |
| Mode of causal delivery | |
| Vaginal | 1377 (65.1) |
| Caesarean section | 698 (33.0) |
| Unknown | 41 (1.9) |
| Neonatal outcome | |
| Alive | 102 (4.8) |
| Stillborn | 1978 (93.5) |
| Unknown | 36 (1.7) |
| Type of fistula | |
| Vesicovaginal fistula (VVF) | 2045 (96.6) |
| Rectovaginal fistula (RVF) | 23 (1.1) |
| VVF + RVF | 48 (2.3) |
In Guinea, the legal age of marriage for women is 17 years.
Treatment outcomes
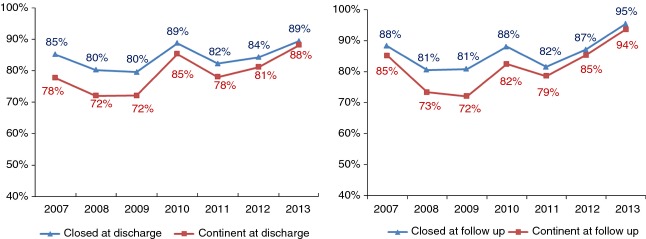
Figure1 shows patient flow and treatment outcomes after surgery, at discharge and 3 months after follow-up. Of the 2116 women who underwent surgical repair, 1748 (83%) had a closed fistula and were dry immediately after surgery. At discharge, 1795 (85%) of all the repaired women had a closed fistula. A total of 1680 of these (79%) were closed and dry of urine and/or faeces, while 115 (5%) had residual incontinence despite fistula closure. Of the 1663 (79%) who completed 3 months of follow-up, 1405 (84.5%) had a closed fistula and 80% were continent (dry). Overall 453 women (21%) were lost to follow-up.
Figure 1.
Patient flow and follow-up at three fistula repair hospitals supported by the Fistula Care Project in Guinea, 2007 to 2013.
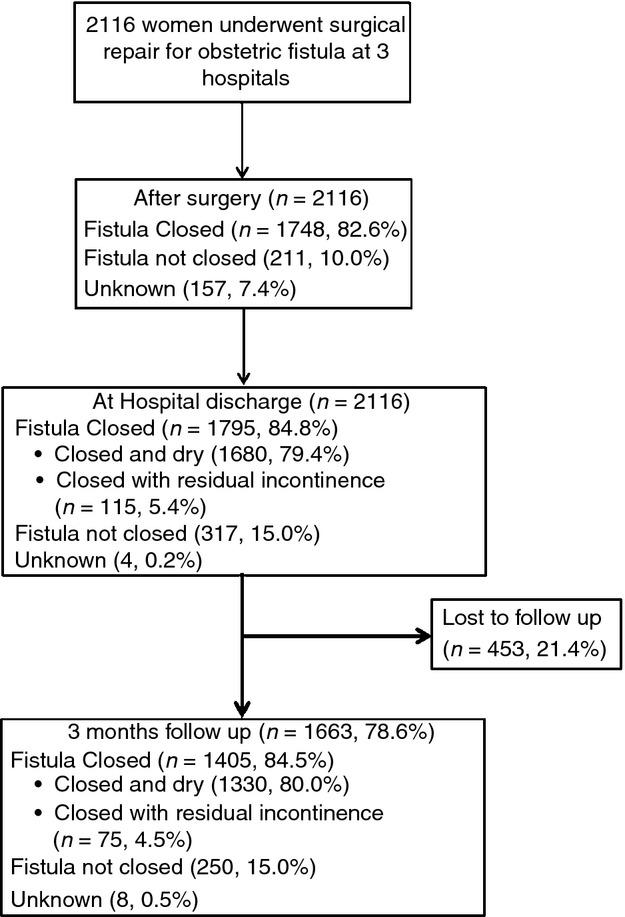
Over the 7-year duration of the project, fistula closure rate at discharge increased from 85% in 2007 to 89% in 2013, and the continence rate rose from 78% in 2007 to 88% in 2013 (Figure2). At 3 months of follow-up, fistula closure rate increased from 88% in 2007 to 95% in 2013, and the continence rate from 85% in 2007 to 94% in 2013 (Figure2).
Figure 2.
Annual trend in treatment outcomes at hospital discharge and at 3 months of follow-up for women undergoing surgical repair for fistula in Guinea, 2007 to 2013.
At hospital discharge, all women with a rectovaginal fistula (RVF) had a closed fistula and remained dry (Table2). Of those with vesicovaginal fistula, 80% had a closed fistula and were dry, while 5% had a closed fistula with residual incontinence. Of those with both a VVF and an RVF, 56% were closed and dry and 2% were closed but had residual incontinence. Compared to women with a previous history of repair attempts, women with no previous history of repair attempts had statistically significantly better surgical outcomes (P = 0.001). Women who had their fistula fewer than 5 years had a better outcome than women with 5 years or more duration (P = 0.003). Also surgical outcomes were better in women with rectovaginal fistula than those with vesicovaginal fistula or both types (P < 0.001).
Table 2.
Fistula closure and continence status by type, number of previous repair attempts and duration of fistula for women undergoing surgical repair for obstetric fistula at hospital discharge in Guinea, 2007 to 2013
| Surgical outcome | |||||
|---|---|---|---|---|---|
| Fistula closed | |||||
| Selected variables | Dry | Residual incontinence | Fistula not closed | Fistula status unknown | P* |
| Type of fistula (n = 2116) | |||||
| VVF | 1630 (79.7) | 114 (5.6) | 297 (14.5) | 4 (0.2) | <0.001 |
| RVF | 23 (100.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| VVF and RVF | 27 (56.3) | 1 (2.0) | 20 (41.7) | 0 (0.0) | |
| Previous repair attempts (n = 2076) | |||||
| No previous repair attempt | 1019 (83.6) | 48 (3.8) | 153 (12.5) | 1 (0.1) | 0.001 |
| ≥1 previous repair attempt | 634 (74.0) | 67 (7.8) | 153 (17.9) | 3 (0.3) | |
| Duration of fistula (1870) | |||||
| ≤1 year | 350 (86.4) | 13 (3.2) | 41 (10.1) | 1 (0.2) | 0.003 |
| 2 to 4 years | 371 (82.8) | 23 (5.1) | 54 (12.1) | 0 (0.0) | |
| ≥5 years | 777 (76.4) | 72 (7.1) | 167 (16.4) | 1 (0.1) | |
Comparing proportions of closed fistula.
Discussion
This is the first retrospective study of data from Guinea reporting on cumulative outcomes at 3-month follow-up among women who underwent surgical repair for female genital fistula over a period of 7 years. Overall, the study showed high rates of fistula closure and continence at discharge and at 3-month follow-up. The rate of loss to follow-up at 3 months in this setting is low compared to 40% reported by Bishinga et al. 15 from Burundi.
We observed a high closure rate at discharge (85%) and at 3 months of follow-up (84.5%), similar to what was reported in other studies in African settings [11,24–27]. The continence rate was 79% at discharge and 80% at 3 months of follow-up, which falls within the range reported by Arrowsmith et al. 13 and higher than what was reported by Bishinga et al. (67%) 15 in Burundi. Even though rates of closure and continence depend on the severity of the fistula, making comparison of different settings difficult, one explanation could be the fact that our programme built on experience in surgical repair of fistula over time, with closure and continence rates increasing over time, while the one in Burundi was in its first year of implementation. In addition, fistula management requires specialised training for not only surgeons but also medical staff involved in the hospital management of patients to ensure good and sustainable results. Our results showed an improvement in the continence rate over time suggesting an improvement in the quality of care due to continuous training and supervision throughout the project life cycle. It has been reported that fistula that is repaired sooner after occurrence, as well as simple fistula provides better results 12,20, and our results could suggest the unusual situation of an established programme seeing progressively ‘earlier’ and ‘simpler’ cases. Introducing physiotherapy in the package of fistula care at the repair hospitals could also contribute in improving outcomes and reducing residual incontinence 28.
Our loss to follow-up rate at 3 months (21%) was lower than that reported from a routine programme setting (41%) in Burundi by Bishinga et al. 15 and by Browning et al. 16 at 6 months (39.5%). However, some of the women in our study (17%) were part of either a prospective cohort study or a randomised controlled trial conducted at one of the sites, which used specific proactive strategies to reduce loss to follow-up 14,24, thus potentially causing an artificial inflation of our follow-up rate.
Our loss to follow-up rate was, however, higher than the 8% reported by Maulet et al. 25 from a 18-month prospective follow-up of a 120 fistula patients' cohort conducted in Mali and Niger, and the 14% reported by Nielsen et al. 26 in Western Ethiopia after a 14- to 28-month community-based follow-up. In both studies, active search of women was conducted and could explain the low rate of loss to follow-up observed.
We observed a high rate of stillbirths with the referent delivery, better repair outcomes in women with no history of previous repair attempt, women with shorter duration of fistula and women having rectovaginal fistula, consistent with the findings reported by other studies from Africa 12,20.
Finally, prevention of fistula occurrence is the definite answer towards a fistula-free generation. This must include education about community awareness to reduce sociocultural factors that increase risk of obstetric fistula, promotion of deliveries in health facilities, improvement of contraceptive methods use 27 and advocacy for compliance with country laws aimed to reduce pregnancies in teenagers.
As the government in Guinea is planning to launch a new fistula project, we concur with Bishinga et al. 15 that fistula programmes might benefit from a model of cohort monitoring such as that used routinely with chronic diseases such as tuberculosis, where patients are closely followed up for longer periods with various strategies (phones, home visits, community health workers, etc.) to evaluate programmes success.
For instance, a study in Ethiopia 16 reported 22 women who came back leaking at 6 months of follow-up among 141 women initially cured at discharge. This confirms the risk of late breakdown after successful repair and warrants more research into the causes and associations of late fistula.
The main limitation of this study was that the reasons for loss to follow-up could not be determined, as patients lost to follow-up were not routinely followed up using home visits or phone calls. A strength of our study is the large number of patients with different types of fistula, making this the largest reported national cohort of fistula patients. Because some data were routinely collected during the course of the Fistula Care project at the three repair hospitals, capacity building in the area of data recording and review, with regular monitoring and supervision, was routinely carried out; thus, the data are likely to be accurate and representative of what was actually going on at the sites. Finally, we report our results using the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines 29.
Conclusion
In conclusion, routine repair services for female genital fistula in low resources settings are feasible and can yield good outcomes. However, for clinical services to be successful, they must be couched in a ‘holistic programme’ that encompasses supportive policies, active community engagement and partnership, and psychosocial support in addition to an effective and functioning supply of services. Further work is needed to trace women who are lost to follow-up and to maintain excellent repair services throughout Guinea and other countries where obstetric fistulas are common.
Acknowledgments
This research was conducted through the Structured Operational Research and Training Initiative (SORT-IT), a global partnership led by the Special Programme for Research and Training in Tropical Diseases at WHO/TDR. The model is based on a course developed jointly by the International Union Against Tuberculosis and Lung Disease and Medécins sans Frontières. The specific SORT-IT programme which resulted in this publication was jointly developed and implemented by Médecins Sans Frontières, Luxembourg; the Centre for Operational Research, The Union, Paris, France; the Centre for International Health, University of Bergen, Norway; the Institute of Tropical Medicine, Antwerp, Belgium; The University of Nairobi, Kenya; and the University of Chester, United Kingdom. The programme was funded by The Union, MSF, the Department for International Development (DFID) and WHO. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. Fistula Care was managed by EngenderHealth and funded by the U.S. Agency for International Development. Views expressed here do not necessarily reflect those of USAID, EngenderHealth or the Institute of Tropical Medicine of Antwerp.
References
- Wall LL. A framework for analyzing the determinants of obstetric fistula formation. Stud Fam Plann. 2012;43:255–272. doi: 10.1111/j.1728-4465.2012.00325.x. [DOI] [PubMed] [Google Scholar]
- Zheng AX, Anderson FW. Obstetric fistula in low-income countries. Int J Gynaecol Obstet. 2009;104:85–89. doi: 10.1016/j.ijgo.2008.09.011. [DOI] [PubMed] [Google Scholar]
- Capes T, Ascher-Walsh C, Abdoulaye I, Brodman M. Obstetric fistula in low and middle income countries. Mt Sinai J Med. 2011;78:352–361. doi: 10.1002/msj.20265. [DOI] [PubMed] [Google Scholar]
- Longombe A, Claude K, Ruminjo J. Fistula and traumatic genital injury from sexual violence in a conflict setting in Eastern Congo: case studies. Reprod Health Matters. 2008;16:132–141. doi: 10.1016/S0968-8080(08)31350-0. [DOI] [PubMed] [Google Scholar]
- Raassen T, Ngongo C, Mahendeka M. Iatrogenic genitourinary fistula: an 18-year retrospective review of 805 injuries. Int Urogynecol J. 2014;25:1699–1706. doi: 10.1007/s00192-014-2445-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall LL. Obstetric fistula is a “neglected tropical disease”. PLoS Negl Trop Dis. 2012;6:e1769. doi: 10.1371/journal.pntd.0001769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osotimehin B. Obstetric fistula: ending the health and human rights tragedy. Lancet. 2013;381:1702–1703. doi: 10.1016/S0140-6736(13)61001-6. [DOI] [PubMed] [Google Scholar]
- Stanton C, Holtz SA, Ahmed S. Challenges in measuring obstetric fistula. Int J Gynaecol Obstet. 2007;99(Suppl 1):S4–S9. doi: 10.1016/j.ijgo.2007.06.010. [DOI] [PubMed] [Google Scholar]
- Adler AJ, Ronsmans C, Calvert C, Filippi V. Estimating the prevalence of obstetric fistula: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2013;13:246. doi: 10.1186/1471-2393-13-246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institut National des Statistiques G. Enquête Démographique et de Santé et a Indicateurs Multiples, Guinée 2012. Claverton, MD, USA: INS & Macro; 2014. [Google Scholar]
- Tayler-Smith K, Zachariah R, Manzi M, et al. Obstetric Fistula in Burundi: a comprehensive approach to managing women with this neglected disease. BMC Pregnancy Childbirth. 2013;14:164. doi: 10.1186/1471-2393-13-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins L, Spitzer RF, Christoffersen-Deb A, Leah J, Mabeya H. Characteristics and surgical success of patients presenting for repair of obstetric fistula in western Kenya. Int J Gynaecol Obstet. 2013;120:178–182. doi: 10.1016/j.ijgo.2012.08.014. [DOI] [PubMed] [Google Scholar]
- Arrowsmith SD, Barone MA, Ruminjo J. Outcomes in obstetric fistula care: a literature review. Curr Opin Obstet Gynecol. 2013;25:399–403. doi: 10.1097/GCO.0b013e3283648d60. [DOI] [PubMed] [Google Scholar]
- Barone MA, Frajzyngier V, Ruminjo J, et al. Determinants of postoperative outcomes of female genital fistula repair surgery. Obstet Gynecol. 2012;120:524–531. doi: 10.1097/AOG.0b013e31826579e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishinga A, Zachariah R, Hinderaker S, Tayler-Smith K, van den Boogaard W, Taryor R. High loss to follow-up following obstetric fistula repair surgery in rural Burundi: is there a way forward? Public Health Action. 2013;3:113–117. doi: 10.5588/pha.13.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browning A, Menber B. Women with obstetric fistula in Ethiopia: a 6-month follow-up after surgical treatment. BJOG. 2008;115:1564–1569. doi: 10.1111/j.1471-0528.2008.01900.x. [DOI] [PubMed] [Google Scholar]
- Frajzyngier V, Ruminjo J, Barone MA. Factors influencing urinary fistula repair outcomes in developing countries: a systematic review. Am J Obstet Gynecol. 2012;207:248–258. doi: 10.1016/j.ajog.2012.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landry E, Frajzyngier V, Ruminjo J, et al. Profiles and experiences of women undergoing genital fistula repair: Findings from five countries. Glob Public Health. 2013;8:926–942. doi: 10.1080/17441692.2013.824018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muleta M, Rasmussen S, Kiserud T. Obstetric fistula in 14,928 Ethiopian women. Acta Obstet Gynecol Scand. 2010;89:945–951. doi: 10.3109/00016341003801698. [DOI] [PubMed] [Google Scholar]
- Kayondo M, Wasswa S, Kabakyenga J, et al. Predictors and outcome of surgical repair of obstetric fistula at a regional referral hospital, Mbarara, western Uganda. BMC Urol. 2011;11:23. doi: 10.1186/1471-2490-11-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umoiyoho AJ, Inyang-Etoh EC, Etukumana EA. Obstetric fistula repair: experience with hospital-based outreach approach in Nigeria. Glob J Health Sci. 2012;4:40–45. doi: 10.5539/gjhs.v4n5p40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leye MM, Ndiaye P, Diongue M, et al. Socio-demographic factors and the treatment of obstetric fistula in southeastern Senegal. Sante Publique. 2012;24:47–54. . [ ]. [PubMed] [Google Scholar]
- Fistula C. Project Report: October 2007 to December 2013, Part 1I: Country Accomplishments. New York: Fistula Care/EngenderHealth; 2013. [Google Scholar]
- Barone M, Frajzyngier V, Arrowsmith SD, et al. Non-inferiority of short-term urethral catheterization following fistula repair surgery: study protocol for a randomized controlled trial. BMC Pregnancy Childbirth. 2012;12:5. doi: 10.1186/1472-6874-12-5. . doi: 10.1186/1472-6874-12-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maulet N, Keita M, Macq J. Medico-social pathways of obstetric fistula patients in Mali and Niger: an 18-month cohort follow-up. Trop Med Int Health. 2013;18:524–533. doi: 10.1111/tmi.12086. [DOI] [PubMed] [Google Scholar]
- Nielsen HS, Lindberg L, Nygaard U, et al. A community-based long-term follow-up of women undergoing obstetric fistula repair in rural Ethiopia. BJOG. 2009;116:1258–1264. doi: 10.1111/j.1471-0528.2009.02200.x. [DOI] [PubMed] [Google Scholar]
- Delamou A, Koivogui A, Dubourg D, Delvaux T. Family planning in Guinea: a need for better public commitment. Trop Med Int Health. 2014;19:65–73. doi: 10.1111/tmi.12219. [DOI] [PubMed] [Google Scholar]
- Castille YJ, Avocetien C, Zaongo D, Colas JM, Peabody JO, Rochat CH. Impact of a program of physiotherapy and health education on the outcome of obstetric fistula surgery. Int J Gynaecol Obstet. 2014;124:77–80. doi: 10.1016/j.ijgo.2013.06.032. [DOI] [PubMed] [Google Scholar]
- von Elm E, Altman D, Egger M, Gøtzsche P, Vandenbroucke J. STROBE Initiative: The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]