Abstract
BACKGROUND
To date, most studies on deferral of blood donors have focused on men who have sex with men (MSM) and/or injecting drug users. Few have examined deferrable risk behaviors relating to transfusion-transmissible infections (TTIs) in general. This study aimed to examine the prevalence of, and factors associated with, nondisclosure of TTI-related risk behaviors in donors.
STUDY DESIGN AND METHODS
Chinese-speaking donors who had just given blood in Hong Kong were invited to self-complete an anonymous questionnaire. Practices of one or more of seven deferrable risk behaviors associated with TTI were inquired. Factors associated with noncompliance with self-disclosure were evaluated by logistic regression.
RESULTS
Over a 4-week study period in 2012, a total of 1143 donors were recruited. Overall, 0.2% gave a history of drug injection, 1.7% had had sex with sex worker(s), and 0.3% had had sex with a human immunodeficiency virus–infected partner, while none had been paid for sex. Some 1.5% of male donors reported having same-sex behaviors. Factors associated with noncompliance were male gender (odds ratio [OR] 31.1; 95% confidence interval [CI], 3.7-263.6), having multiple sex partners (OR, 89.7; 95% CI, 28.7-279.9), and previous history of temporary deferral (OR, 11.4; 95% CI, 2.5-53.3). If suspected noncompliance was included, the overall prevalence of nondisclosure of deferrable behaviors could be high at 6.5%.
CONCLUSION
Albeit uncommon, some donors fail to provide accurate answers to predonation screening questions and are not deferred appropriately. There is room for improvement to make deferral policy acceptable and understandable, so as to minimize the risk of TTI. Efforts are also needed to tackle the paucity of data on noncompliance of non-MSM donors.
Despite the small residual risk, transfusion recipients are susceptible to transfusion-transmissible infections (TTIs) from receiving contaminated blood if the donation is made within a very short period after virus entry.1,2 In the United States, for example, there were occasional reports of transfusion-transmissible human immunodeficiency virus (HIV) infections, despite the introduction of nucleic acid testing for blood donation since 1999.3 Careful selection of donors thus forms one pragmatic risk management strategy to ensure blood safety. In conjunction with universal screening for known TTI, blood donation services around the world have been deploying strict donor deferral policy to refuse certain individuals to give blood, either temporarily or permanently. For instance, men who have sex with men (MSM), injection drug users (IDUs), and sex workers are deferred permanently in China (including Hong Kong), France, Germany, and Norway,4 in view of the higher proportion of reported TTIs, notably HIV in these countries.5–8 In response to cumulating scientific evidence on blood safety and growing discussions of gay rights, permanent deferral of MSM has gradually been replaced by time-based deferral in countries such as Australia,9 United Kingdom,10 and Canada11 and in the United States in near future.12
Although the precise procedure may vary, donor selection generally involves predonation risk assessment that requires prospective donors to self-declare certain “risk” events during a specified period. In Hong Kong, for example, each potential donor is asked to self-complete a health screening questionnaire every time before donation. The questionnaire contains 30 items covering current health status, infectious diseases exposures, travel history, and risk behaviors that may sabotage blood safety because of their association with TTI.13 The questionnaire is then cross-checked by a nurse, who verifies donor eligibility against the blood bank computer database. The prospective donors’ blood pressure, pulse rate, body temperature, and hemoglobin (Hb) level are then checked. Potential donors who have not declared any deferrable risk and are physically suitable for donation are then allowed to give blood. Similar procedures are in place in most blood donation services elsewhere.
Nevertheless, the donor deferral system is highly reliant on donors’ understanding and honesty. The system would become meaningless if donors do not disclose their risk behaviors truthfully—in other words, being “noncompliant.” In Australia, a study reported an overall noncompliance rate among donors of 1.65% for any one of the eight TTI risk–related deferrable categories.9 An earlier study on 50,162 allogeneic blood donors by Williams and coworkers14 also reported a nondisclosure prevalence of 1.9% among nine deferrable categories in the United States. To date, however, most noncompliance studies have specifically focused on MSM and IDU, while few have looked into deferrable risks associated with TTI in donors in general.15–19 To fill this knowledge gap, this study was conducted to determine the prevalence of, and factors associated with, noncompliance of donors with the existing deferral policy referable to TTI in Hong Kong.
MATERIALS AND METHODS
This was a cross-sectional study on donors attending the Hong Kong Red Cross Blood Transfusion Service (BTS). BTS has been exclusively responsible for local blood supply in the city since 1952. Blood donation in Hong Kong is entirely voluntary and nonremunerated. To be eligible to donate blood, individuals have to be healthy adults between the age of 16 and 65, have to weigh at least 41 kg, and have to have not reported any deferrable risk behaviors when completing the predonation health screening questionnaire. Each potential donor is also checked for Hb level, body temperature, and blood pressure before donation. There were a total of eight BTS donation centers in Hong Kong at the time of the survey. During each recruitment session, all Chinese-speaking donors who had just donated blood at these centers were invited by four trained volunteers to participate in the study. The volunteers explained the study objectives to the donors and obtained their verbal consent. Dates of recruitment sessions were set following agreement between the research team and BTS, which included both weekdays and weekends. Donors who could not understand Chinese were excluded from this study.
All consenting respondents were invited to self-complete an anonymous questionnaire using handheld tablet computers. The study questionnaire consisted of four main parts: 1) demographics (sex, age, education level, and occupation); 2) blood donation experience (number of times and frequency of blood donation, reasons for donation, deferral experiences, and awareness of the deferral questionnaire); 3) attitudes toward blood donation (including the consideration of blood donation as a form of free health check); and 4) practice of deferrable behaviors relating to TTIs. Seven such deferrable behaviors were assessed, viz: ever having 1) male-to-male sex, 2) sex with an HIV-positive partner, 3) been paid for sex, and 4) injected illicit drugs and history of sexual contacts with any of the following in the preceding 12 months: 5) bisexual male; 6) sex worker, and 7) someone who abused or injected illicit drugs. These behaviors were identical with TTI-associated deferrable risk required to be declared in the BTS’s predonation health screening questionnaire.13
Demographic statuses, donation experiences, and deferrable risk behaviors of all respondents were described and tabulated. A self-confessed noncomplier was defined as a blood donor who answered “yes” to any one or more of the seven behavioral practices associated with TTIs, while a suspected noncomplier was one who answered “I’m not sure” against the corresponding question(s). Prevalence and respective 95% confidence intervals (CIs) for self-confessed and suspected noncompliers were determined. The worst-case scenario of noncompliance was estimated based on the total number of self-confessed and suspected noncompliers. The reasons for self-confessed noncompliers failing to declare the deferrable behaviors were evaluated. Univariate analysis was performed to compare between male and female donors and between self-confessed noncompliers and other blood donors. Chi-square tests were applied to compare categorical differences, and the t test was used to examine the differences between continuous variables (i.e., age). A logistic regression model was then constructed to examine factors associated with noncompliance. All variables were entered to the model stepwise and were removed if the p value was larger than 0.1. A p value of less than 0.05 was taken to denote significance. All analyses were conducted with computer software (SPSS 21.0, SPSS, Inc., Chicago, IL; and Microsoft Excel 2013, Microsoft Corp., Redmond, WA). The study was approved by the Survey and Behavioral Research Ethics Committee of the Chinese University of Hong Kong.
RESULTS
Over a 4-week study period in 2012, a total of 3420 donors presented at the eight blood donation centers during the recruitment timeslots, of which 1143 consented to participate in the survey (response rate, 33.4%). Approximately half of the recruited donors were less than 30 years old (53.8%) and were male (n = 591, 51.7%). Female respondents were generally younger (χ2 = 52.405, p < 0.001). Almost all respondents were permanent residents of Hong Kong (93.1%) and had attained at least secondary education (98.2%). Roughly a quarter (27.1%) were full-time students (Table1).
Table 1.
Characteristics of respondents and univariate comparison by sex
| Characteristics | All (n = 1143) | Male (n = 591) | Female (n = 552) |
|---|---|---|---|
| Demographics | |||
| Being a permanent Hong Kong resident | 1064 (93.1) | 56 (94.1) | 508 (92.0) |
| Age (years)* | |||
| 16-20 | 276 (24.1) | 101 (17.1) | 175 (31.7) |
| 21-30 | 340 (29.7) | 161 (27.2) | 179 (32.4) |
| 31-40 | 231 (20.2) | 141 (23.9) | 90 (16.3) |
| >40 | 296 (25.9) | 188 (31.8) | 109 (19.6) |
| Education level | |||
| Primary or below | 20 (1.7) | 14 (2.4) | 6 (1.1) |
| Secondary | 766 (67.0) | 383 (64.8) | 383 (69.4) |
| University or above | 357 (31.2) | 194 (32.8) | 164 (29.5) |
| Occupational status* | |||
| Student | 310 (27.1) | 111 (18.8) | 199 (56.1) |
| In full-time employment | 713 (62.4) | 429 (72.6) | 284 (51.4) |
| Retired or unemployed | 53 (5.5) | 36 (6.1) | 27 (4.9) |
| Housewives or others | 57 (5.0) | 15 (2.5) | 42 (7.6) |
| Donation history | |||
| Age at first donation (mean, SD)* | 20.7, 7.1 | 21.3, 7.5 | 20.1, 6.8 |
| First-time donors* | 171 (15.0) | 73 (12.4) | 98 (17.8) |
| Had been deferred in previous donations† | (n = 972) | (n = 518) | (n = 454) |
| Yes | 68 (7.0) | 36 (6.9) | 32 (7.0) |
| Current donation experiences | |||
| Major reasons for blood donation | |||
| To help others | 1037 (90.7) | 537 (90.9) | 500 (90.6) |
| To have health check | 404 (35.3) | 198 (33.5) | 206 (37.3) |
| The location of donation center is convenient | 513 (44.9) | 251 (42.5) | 262 (47.5) |
| My friend encouraged me | 441 (38.6) | 214 (36.2) | 227 (41.1) |
| In response to Red Cross’s advertisement | 620 (54.2) | 320 (54.1) | 300(54.3) |
| Others | 55 (4.8) | 28 (4.7) | 27 (4.9) |
| Had read the predonation questionnaire* | |||
| Read thoroughly | 563 (49.3) | 293 (49.6) | 270 (48.9) |
| Skimmed through/read selectively | 482 (42.2) | 236 (39.9) | 246 (44.6) |
| Did not read it | 98 (8.6) | 62 (10.5) | 36 (6.5) |
| Reported any of the deferrable behaviors*‡ | 32 (2.8) | 31 (5.2) | 1 (0.2) |
| Had/possibly had any of the deferrable behaviors*§ | 117 (10.2) | 84 (14.2) | 33 (6.0) |
Univariate comparisons by sex using χ2 or t test with a p value of less than 0.05.
Among repeat donors.
Deferrable behaviors included: 1) ever had male-to-male sex, 2) ever had sex with an HIV-positive partner, 3) had ever been paid for sex, 4) ever injected illicit drugs, 5) had sex with a bisexual male in past 12 months, 6) had sex with a sex worker in past 12 months, and 7) had sex with someone who abused or injected drugs in past 12 months.
Including those who answered “yes” and “I’m not sure” for the deferrable behaviors.
Most (85.1%) respondents had donated blood more than once. Female respondents were more likely to be first-time donors (χ2 = 6.546, p = 0.011). The mean (±SD) age of first donation was 20.7 (±7.1) years, with females having their first donation at a younger age (t = 2.729, p = 0.006). Among the repeat donors, 7.0% had been deferred temporarily in previous donations. The most common reason for previous deferrals was being physically unfit for immediate donation (such as having low Hb level or a fever; 80.6%). More than 90% reported that they had read the health screening questionnaire before the current donation—either thoroughly (49.3%) or skimmingly and selectively (42.2%; Table1).
As shown in Table2, this survey recruited nine (1.5% of male donors) MSM. Overall, 0.2% of all respondents reported a history of injecting drug, 1.7% reported having sex with a sex worker in the preceding year, and 0.3% reported having ever had sex with an HIV-infected partner. None reported having been paid for sex. On the other hand, some donors claimed that they were uncertain about certain behavioral risk (referred as suspected noncompliers in this study). Specifically, 5.1% reported a history of having sex with a partner who might have abused or injected drugs, and 2.9% of females reported having sex with a male who might be bisexual in the preceding year. The prevalence for self-confessed noncompliance ranged between 0.0 and 2.9% of the deferrable risk factors examined. If suspected noncompliers are included, the prevalence becomes 6.5% at the upper end of the CI (for the behavior “having had sex with someone who abused/injected drugs in the last 12 months”). Compared with female respondents, male respondents were more likely to have had sex with someone who might be HIV positive (χ2 = 33.815, p < 0.05), might be a sex worker (χ2 = 5.541, p < 0.05), or might have abused or injected drugs (χ2 = 4.667, p < 0.05; Table2).
Table 2.
Practice of deferrable risk behaviors in donors and their comparisons by sex
| Male (n = 591) | Female (n = 552) | Overall prevalence | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Deferrable risk behavior | Self-confessed | Suspected | Total | Confirmed | Suspected | Total | Self-confessed | Suspected | Worst-case scenario* | |
| History of | ||||||||||
| Male-to-male sex | 9 (1.5) | 0 (0.0) | 9 (1.5) | 1.5 (0.8-2.9) | 0.0 (0.0-0.3) | 1.5 (0.8-2.9)† | ||||
| Having sex with an HIV-positive partner‡ | 2 (0.3) | 36 (6.1) | 38 (6.4) | 1 (0.2) | 0 (0.0) | 1 (0.2) | 0.3 (0.1-0.8) | 3.1 (2.3-4.3) | 3.4 (2.5-4.6) | |
| Having been given money for sex | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0.0 (0.0-0.3) | 0.0 (0.0-0.3) | 0.0 (0.0-0.3) | |
| Injection of illicit drugs | 2 (0.3) | 0 (0.0) | 2 (0.3) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0.2 (0.1-0.6) | 0.0 (0.0-0.3) | 0.2 (0.1-0.6) | |
| In the past 12 months, had sex with | ||||||||||
| A bisexual male | 0 (0.0) | 16 (2.9) | 16 (2.9) | 0.0 (0.0-0.7) | 2.9 (1.8-4.7) | 2.9 (1.8-4.7)§ | ||||
| A sex worker‡ | 20 (3.4) | 0 (0.0) | 20 (3.4) | 0 (0.0) | 7 (1.3) | 7 (1.3) | 1.7 (1.1-2.7) | 0.6 (0.3-1.3) | 2.4 (1.6-3.4) | |
| Someone who abused or injected drugs‡ | 0 (0.0) | 38 (6.4) | 38 (6.4) | 0 (0.0) | 20 (3.6) | 20 (3.6) | 0.0 (0.0-0.3) | 5.1 (4.0-6.5) | 5.1 (4.0-6.5) | |
Worst-case scenario was estimated based on the total number of confirmed and suspected noncompliers.
Among male donors.
Univariate comparisons of total number of self-confessed and suspected noncompliers by sex using χ2 test with a p value of less than 0.05.
Among female donors.
Table3 shows the characteristics, donation experience, and sexual behaviors of four types of self-confessed noncompliers, that is, MSM, clients of sex workers, IDUs, and those having had sex with HIV-infected partners (n = 32). Most of these noncompliers were repeat donors, and some reported having a health check as a motive for blood donation (ranging from 30% of sex workers’ clients to 100% of IDUs). Approximately half of the MSM donors reported not having anal sex in the previous year, while one sex worker’s client reported bisexual exposure. One IDU reported having had sex with an HIV-infected partner. The rate of condom use in the most recent sexual contact ranged between 50% (IDUs) to 100% (MSM; Table3).
Table 3.
Characteristics of four types of confirmed noncompliant donors by deferrable behaviors (n = 32)*
| Characteristics | MSM (n = 9) | SW’s clients (n = 20) | IDUs (n = 2) | HIV partner (n = 3) |
|---|---|---|---|---|
| Demographics | ||||
| Age (years), mean, SD | 29.3, 11.1 | 36.2, 8.4 | 29.5, 6.4 | 26, 3.6 |
| University or above education | 2 (22.2) | 6 (30.0) | 2 (100.0) | 1 (33.3) |
| Donation experience | ||||
| Repeat donor | 7 (77.8) | 18 (90.0) | 2 (100.0) | 3 (100.0) |
| “Health check” as a major reason for donation | 5 (55.6) | 6 (30.0) | 2 (100.0) | 2 (66.7) |
| Sexual behaviors in the previous year | ||||
| Having male-to-male anal sex | 5 (55.6) | 1 (5.0) | 0 (0.0) | 0 (0.0) |
| Total number sex partners | ||||
| 0 | 3 (33.3) | 0 (0.0) | 1 (50.0) | 0 (0.0) |
| 1 | 1 (11.1) | 1 (5.0) | 0 (0.0) | 0 (0.0) |
| 2 or above | 5 (55.6) | 19 (95.0) | 1 (50.0) | 3 (100.0) |
| Using a condom in the most recent intercourse | 5 (100.0) | 17 (85.0) | 1 (50.0) | 2 (66.7) |
One MSM respondent was also a SW’s client, and one IDU had ever had sex with an HIV-infected partner.
SW = sex workers; HIV partner = respondents who had sex with an HIV-infected partner.
Table4 shows the results of univariate analysis and the logistic model that compared self-confessed noncompliers (n = 32) with other blood donors (n = 1111). In total nine independent variables were entered into the model, including demographics (age, sex, occupation, and education level), whether one had read the health screening questionnaire, first-time versus repeat donations, having “health check” as a reason for blood donation, donor deferral experiences, and having multiple sex partners. Only three of nine variables remained significant in the final model. Noncompliers were more likely to be male (odds ratio [OR], 31.06; 95% CI, 3.66-263.58; p = 0.002), have more than one sex partner (OR, 89.67; 95% CI, 28.72-279.94; p < 0.001), and have been deferred previously (OR, 11.42; 95% CI, 2.45-53.31; p = 0.002).
Table 4.
Univariate and logistic analysis of factors associated with noncompliance
| Variables | Noncompliers (n = 32) | Compliers (n = 1111) | Univariate χ2 or t | B | SE | Wald | p value | OR (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Male sex | 31 (96.9) | 560 (50.4) | 26.899* | 3.436 | 1.091 | 9.917 | 0.002* | 31.06 (3.66-263.58) |
| Age (years), mean, SD | 33.4, 9.4 | 31.4, 11.9 | t = −0.946 | 0.882 | ||||
| Being full-time student | 2 (6.3) | 308 (27.7) | 7.256* | 0.993 | ||||
| Having attained university education | 10 (31.3) | 347 (31.2) | 0.000 | 0.918 | ||||
| Had read the deferral questionnaire in the current donation | 28 (87.5) | 1017 (91.5) | 0.647 | 0.686 | ||||
| Being first-time donor | 4 (12.5) | 167 (15.0) | 0.156 | 0.897 | ||||
| Health check as a major reason for current donation | 13 (40.6) | 391 (35.2) | 0.402 | 0.635 | ||||
| Previous history of deferral | 3 (9.4) | 65 (5.9) | 0.691 | 2.435 | 0.786 | 9.593 | 0.002* | 11.42 (2.45-53.31) |
| Having more than one sex partner | 26 (81.3) | 67 (6.0) | 235.449* | 4.496 | 0.581 | 59.911 | <0.001* | 89.67 (28.72-279.94) |
p < 0.05.
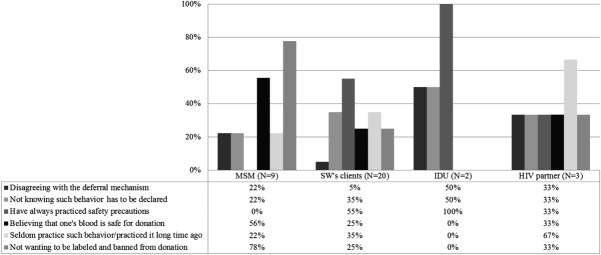
The reasons for the failure of self-confessed noncompliers to declare their risk behavior are shown in Fig. 1. For MSM donors, the most commonly reported reason was “not wanting to be labeled and banned from donation” (n = 7/9, 78%). For donors who had ever had sex with a person infected with HIV, 67% (n = 2/3) reported “seldom practicing such behavior/practiced it a long time ago.” Approximately half of the donors who had had sex with a sex worker (n = 11/20, 55%) and all IDU donors (n = 2/2, 100%) did not comply with the deferral because they had “always practiced safety precautions.”
Figure 1.
Reasons for nondisclosure of deferrable behaviors by type of noncompliance. SW = sex workers; HIV partner = respondents who had sex with an HIV-infected partner.
DISCUSSION
In this study, all respondents were donors who had just given blood at a donation center. This means that noncompliers identified in this study had not made honest disclosure about their TTI-associated behaviors when completing the predonation health screening questionnaire. The prevalence of self-confessed noncompliance ranged between 0.0 and 2.7%. In the worst-case scenario, constructed by extending the definition of noncompliance to include suspected noncompliers, up to 1/10th (117/1143) of the donors may have sidestepped the deferral mechanism and have donated blood. Noncompliers were more likely to be male, have multiple sex partners, and have been deferred in previous donations. Reasons for not complying with the deferral policy varied between the deferrable behaviors that the donors had practiced.
For MSM, the observed 1.5% (0.8%-2.9%) noncompliance prevalence is consistent with that of another study conducted in Hong Kong at around the same time (2.2%)15 and is highly comparable to figures reported in places where MSM are deferred permanently, such as the United States (2.4%) and Canada (approx. 1%).16,17 MSM donors in this study did not disclose their identity mostly because they believed that their blood was safe and did not want to be permanently barred from donating blood. In fact, all noncompliant MSM had practiced protected sex, of whom a third did not have sexual contacts for prolonged period of time. They had a lower number of sex partners compared to MSM recruited in local gay-frequent venues, as reported in another study.5 While considered as noncompliers under the current permanent deferral policy, their risk of TTI transmission should be infinitesimally small. Should a 12-month deferral period be enforced, the noncompliance rate in this study would fall to 1% (six MSM without a partner in the past 12 months divided by 591 male donors), which is closer to the 0.23% noncompliance rate in Australia, where the deferral period is 1 year.9 Given that many MSM are keen to donate blood,18,20 time-based deferral might expand the donor pool without increasing the risk of TTI, assuming that other settings remain the same. A retrospective analysis on Australian blood donors suggested that time-based deferral for MSM did not result in a significant increase in recipient risk for HIV, and compliance of MSM donors appeared to be more influential on the overall risk than the duration of deferral.21 Besides, other studies have used mathematical models to estimate the consequences of replacing the permanent deferral policy for MSM donors. In Canada, for example, it was estimated that a 5-year MSM deferral could add more than 4000 new donors to the blood service with only a negligible risk of blood contamination (one contamination in every 1072 years).22 Another study estimated that only one extra HIV infectious donation would be introduced to the blood service in England and Wales in every 455 years, under the 12-month deferral policy.23 This evidence might suggest that with time-based deferral, improved compliance of MSM could outweigh the theoretical risk of TTI. Recently, the US Food and Drug Administration issued a statement to support the change to a 12-month deferral period for MSM, after taking into account the recommendations of advisory committees such as AABB, America’s Blood Centers, and the American Red Cross.12
On the other hand, while IDU constitutes a known risk of TTI, only a small percentage of donors (0.2%) in our study had not disclosed their deferrable history of drug injection, a figure similar to that reported in Canada (0.2%),11 Australia (0.4%),9 and the United States (0.5%).14 Unlike MSM, attitudes and reasons for IDUs’ nondisclosure have received little attention in similar research. O’Brien and coworkers11 speculated that IDUs’ disclosure was affected by psychological factors such as fear of embarrassment and negative impacts on self-esteem, and some might conceal their drug injection history because of their misinterpretation of the meaning of the screening questions. Given the paucity of updated data and the high prevalence of hepatitis C infection among IDUs in Hong Kong and elsewhere,24,25 further investigations are needed before any change to the current permanent deferral policy for IDUs is considered.
Overall, this study evaluated the association between nine variables and noncompliance with deferral policy. These variables were selected because, first, donation behavior could vary across sociodemographics and donation frequency.26,27 Second, experience of deferral could also affect the likelihood of donors’ future return28 and thus compliance. Third, there have been concerns on the test-seeking behavior among donors and its effect on noncompliance,29,30 and some donors were not aware of the purpose of predonation screening.15,18 In our study, having multiple sex partners was associated with noncompliance, a phenomenon that had been reported previously.9 Consistent with previous studies, male donors15,31 and those who had multiple sex partners9 were more likely to conceal their deferrable behaviors. This could be explained by the fact that most deferrable behaviors included in this analysis were sexually related, and Chinese men generally hold more permissive sexual attitudes than women.32 Also, women in this study were more likely to have read the health screening questionnaire so they may be more aware of the deferral criteria. Separately, donors who had been temporarily deferred in previous donations were more likely to hide their deferrable behaviors. Few studies have assessed the association between previous deferral experience and noncompliance, but it has been suggested that donors are less likely to return for donation after receiving a temporary deferral.28 If donors present for donation again, they may be more concerned about being deferred again and may thus refuse to report their behaviors intentionally.
In our study, approximately one-third of all respondents reported “to have health check” as one major reason for blood donation, a figure higher than that in studies on donors’ test-seeking behaviors.29,33 In contrast to studies focusing on HIV test-seeking behaviors,29,33,34 our study has adopted a more comprehensive phrase, “health check” in the questionnaire. In practice the current predonation process in Hong Kong involves not only an HIV test, but also the “checking” of Hb level, body temperature, blood pressure, and screening for other infections like viral hepatitis and syphilis. Our analysis may have therefore included the attitudes of donors who wanted to check for health conditions other than HIV infection. Also, respondents in this study were allowed to choose as many reasons as they found appropriate. In the study by Sojka and Sojka,35 although only 2% of donors reported health check as the most important motive for donating blood, 31% rated it as one of the reasons for them to donate. In our study, approximately half of the MSM and one-third of sex workers’ clients reported “having health check” as a major reason for donating blood. While this may denote a gap for testing services provided to these vulnerable populations, further evaluations are warranted because of the small number of noncompliers recruited in this study.
One new insight that our study offers is the presentation of “the worst-case scenario” of noncompliance. Conventional noncompliance studies and deferral questionnaires have dichotomized responses into “yes” and “no” or had regarded indefinite answers as negative responses (such as in Lucky et al.9). The problem is that when respondents are under pressure to make an immediate choice, they would tend to resort to conservative responses36 or make a guess.37 In either case, the observed prevalence would be inaccurate, and true deferrable cases would be missed. The effect of this is more pronounced for questions about behaviors of donors’ sex partners. In our study, many donors answered “I’m not sure” in response to whether their partners were HIV-infected or bisexual or had abused or injected drugs. In reality, nondisclosure of HIV status and sexual risks between sex partners is very common.38 Conscientious donors would therefore answer “I’m not sure” because this was more appropriate than stating firmly that they knew definitely that their partner did not have such backgrounds. Knowingly, the major problem of including suspected noncompliers was an overestimated noncompliance rate. An alternative approach suggested in our study is to report the breakdown of both self-confessed and suspected noncompliance. In the clinical context, adding an option to indicate one’s uncertainty may also ensure a more accurate assessment of risk by facilitating these donors to discuss their risk with frontline workers. The downside is, however, the complexity of follow-up action in managing potential donors who are uncertain about their risk.
Our study carried several limitations. First, the sample size was relatively small when compared to the entire donor population. Some risk factors in this study contained around zero frequencies that impacted the CIs constructed. Moreover, the sample size was not enough to perform logistic regression for each risk factor separately. By lumping together noncompliers for one logistic regression, the model was heavily influenced by clients of sex workers (approx. two-thirds of noncompliant donors). Caution must be taken when interpreting the results because predictors for noncompliance could be different for different risk factors. Besides, adopting convenience sampling might have further lowered the generalizability of the findings. However, the patterns of noncompliance and other behaviors in this study were largely consistent with those reported in the existing literature. Second, although using touchscreen computers could increase risk reporting among donors by providing better privacy,39 it was still possible that some donors lied about their deferrable behaviors to hide their potential risk to blood safety. Also, some participants who were less computer-literate might have encountered difficulties in completing the questionnaire, although our volunteers were always around to offer help. Third, this study only examined several deferral criteria specific to TTI while other relatively indirect questions on risk behaviors such as having tattoo and piercing, and travel history, have not been included. To conclude, albeit uncommon, some donors in Hong Kong fail to provide accurate answers to predonation screening questions and appropriately self-defer. Clearly, deferral policy would never be effective without donors’ compliance, and good adherence to the policy could outweigh the negative effects of risky behaviors on blood safety. There is still plenty of room for improvement to the deferral policy to make it acceptable and understandable to the potential donors. Efforts are also needed to tackle the paucity of data on noncompliance of non-MSM donors.
Acknowledgments
The authors thank the Hong Kong Red Cross Blood Transfusion Service and the Li Ka Shing Institute of Health Science for supporting the conduction of the survey.
Glossary
- BTS
Hong Kong Red Cross Blood Transfusion Service
- IDU(s)
injection drug user(s)
- MSM
men who have sex with men
- TTI(s)
transfusion-transmissible infection(s)
CONFLICT OF INTEREST
The authors have disclosed no conflicts of interest.
REFERENCES
- Busch MP, Glynn SA, Stramer SL, et al. A new strategy for estimating risks of transfusion-transmitted viral infections based on rates of detection of recently infected donors. Transfusion. 2005;45:254–64. doi: 10.1111/j.1537-2995.2004.04215.x. [DOI] [PubMed] [Google Scholar]
- Leiss W, Tyshenko M, Krewski D. Men having sex with men donor deferral risk assessment: an analysis using risk management principles. Transfus Med Rev. 2008;22:35–57. doi: 10.1016/j.tmrv.2007.09.002. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) HIV transmission through transfusion—Missouri and Colorado, 2008. MMWR Morb Mortal Wkly Rep. 2010;59:1335–9. [PubMed] [Google Scholar]
- Benjamin RJ, Bianco C, Goldman M, et al. Deferral of males who had sex with other males. Vox Sang. 2011;;101:339–67. doi: 10.1111/j.1423-0410.2011.01489.x. [DOI] [PubMed] [Google Scholar]
- Wong HT, Wong KH, Lee SS, et al. Community-based surveys for determining the prevalence of HIV, chlamydia, and gonorrhoea in men having sex with men in Hong Kong. J Sex Transm Dis. 2013;2013:958967. doi: 10.1155/2013/958967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker JD, Henderson GE, Wang TF, et al. Surplus men, sex work, and the spread of HIV in China. AIDS. 2005;19:539–47. doi: 10.1097/01.aids.0000163929.84154.87. [DOI] [PubMed] [Google Scholar]
- Sullivan PS, Hamouda O, Delpech V, et al. Reemergence of the HIV epidemic among men who have sex with men in North America, Western Europe, and Australia, 1996-2005. Ann Epidemiol. 2009;19:423–31. doi: 10.1016/j.annepidem.2009.03.004. [DOI] [PubMed] [Google Scholar]
- Dubois-Arber F, Jeannin A, Spencer B, et al. Mapping HIV/STI behavioural surveillance in Europe. BMC Infect Dis. 2010;10:290. doi: 10.1186/1471-2334-10-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucky TT, Seed CR, Waller D, et al. Understanding noncompliance with selective donor deferral criteria for high-risk behaviours in Australian blood donors. Transfusion. 2014;54:1739–49. doi: 10.1111/trf.12554. [DOI] [PubMed] [Google Scholar]
- UK Department of Health. Donor selection criteria review. London: Department of Health; 2011. Sep [cited 2014 Nov 27]. Available from: https://www.gov.uk/government/publications/donor-selection-criteria-review. [Google Scholar]
- O’Brien SF, Ram SS, Vamvakas EC, et al. The Canadian blood donor health assessment questionnaire: lessons from history, application of cognitive science principles, and recommendations for change. Transfus Med Rev. 2007;21:205–22. doi: 10.1016/j.tmrv.2007.03.002. [DOI] [PubMed] [Google Scholar]
- US Food and Drug Administration. FDA Commissioner Margaret A. Hamburg’s statement on FDA’s blood donor deferral policy for men who have sex with men. Silver Spring (MD): US Food and Drug Administration; 2014. Dec 23 [cited 2015 Feb 26]. Available from: http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm427843.htm. [Google Scholar]
- Hong Kong Red Cross. Pre-donation information. Hong Kong: Hong Kong Red Cross; ; [cited 2014 Oct 27]. Available from: http://www5.ha.org.hk/rcbts/UPFILE/BookFile/20149415268484.pdf. [Google Scholar]
- Williams AE, Thomson RA, Schreiber GB, et al. Estimates of infectious disease risk factors in US blood donors. Retrovirus Epidemiology Donor Study. JAMA. 1997;277:967–72. [PubMed] [Google Scholar]
- Lee CK, Lee KC, Lin CK, et al. Donors’ perspectives on self-deferral of men having sex with men from blood donation. Transfusion. 2013;53:2441–8. doi: 10.1111/trf.12365. [DOI] [PubMed] [Google Scholar]
- Sanchez AM, Schreiber GB, Nass CC, et al. The impact of male-to-male sexual experience on risk profiles of blood donors. Transfusion. 2005;45:404–13. doi: 10.1111/j.1537-2995.2005.03421.x. [DOI] [PubMed] [Google Scholar]
- Goldman M, Yi QL, Ye X, et al. Donor understanding and attitudes about current and potential deferral criteria for high-risk sexual behaviour. Transfusion. 2011;51:1829–34. doi: 10.1111/j.1537-2995.2011.03078.x. [DOI] [PubMed] [Google Scholar]
- Lee SS, Lee CK, Wong NS, et al. Low compliance of men having sex with men with self-deferral from blood donation in a Chinese population. Blood Transfus. 2014;12:166–71. doi: 10.2450/2013.0103-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grenfell P, Nutland W, McManus S, et al. Views and experiences of men who have sex with men on the ban on blood donation: a cross sectional survey with qualitative interviews. BMJ. 2011;343:d5604. doi: 10.1136/bmj.d5604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belanger GA, McFarland W, Raymond HF, et al. If the permanent deferral were lifted would men who have sex with men want to donate blood, and if so, who would be eligible? Transfusion. 2013;53:2729–33. doi: 10.1111/trf.12124. [DOI] [PubMed] [Google Scholar]
- Seed CR, Kiely P, Law M, et al. No evidence of a significantly increased risk of transfusion-transmitted human immunodeficiency virus infection in Australia subsequent to implementing a 12-month deferral for men who have had sex with men. Transfusion. 2010;50:2722–30. doi: 10.1111/j.1537-2995.2010.02793.x. [DOI] [PubMed] [Google Scholar]
- Germain M, Robillard P, Delage G, et al. Allowing blood donation from men who had sex with men more than 5 years ago: a model to evaluate the impact on transfusion safety in Canada. Vox Sang. 2014;106:372–5. doi: 10.1111/vox.12109. [DOI] [PubMed] [Google Scholar]
- Davison KL, Conti S, Brailsford SR. The risk of transfusion-transmitted HIV from blood donations of men who have sex with men, 12 months after last sex with a man: 2005-2007 estimates from England and Wales. Vox Sang. 2013;105:85–8. doi: 10.1111/vox.12024. [DOI] [PubMed] [Google Scholar]
- Lee KC, Lim WW, Lee SS. High prevalence of HCV in a cohort of injectors on methadone substitution treatment. J Clin Virol. 2008;41:297–300. doi: 10.1016/j.jcv.2007.09.013. [DOI] [PubMed] [Google Scholar]
- Miller CL, Johnston C, Spittal PM, et al. Opportunities for prevention: hepatitis C prevalence and incidence in a cohort of young injection drug users. Hepatology. 2002;36:737–42. doi: 10.1053/jhep.2002.35065. [DOI] [PubMed] [Google Scholar]
- Shaz BH, James AB, Hillyer KL, et al. Demographic variations in blood donor deferrals in a major metropolitan area. Transfusion. 2010;50:881–7. doi: 10.1111/j.1537-2995.2009.02501.x. [DOI] [PubMed] [Google Scholar]
- Notari EP, IV, Zou S, Fang CT, et al. Age-related donor return patterns among first-time blood donors in the United States. Transfusion. 2009;49:2229–36. doi: 10.1111/j.1537-2995.2009.02288.x. [DOI] [PubMed] [Google Scholar]
- Custer B, Schlumpf KS, Wright D, et al. Donor return after temporary deferral. Transfusion. 2011;51:1188–96. doi: 10.1111/j.1537-2995.2010.02989.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiavetta J, Ennis M, Gula CA, et al. Test-seeking as motivation in volunteer blood donors. Transfus Med Rev. 2000;14:205–15. doi: 10.1053/tm.2000.7353. [DOI] [PubMed] [Google Scholar]
- Goncalez TT, Sabino EC, Murphy EL, et al. Human immunodeficiency virus test-seeking motivation in blood donors, São Paulo, Brazil. Vox Sang. 2006;90:170–6. doi: 10.1111/j.1423-0410.2006.00743.x. [DOI] [PubMed] [Google Scholar]
- Wang J, Liu J, Huang Y, et al. An analysis of risk factors for human immunodeficiency virus infection among Chinese blood donors. Transfusion. 2013;53(10 Pt 2):2431–40. doi: 10.1111/trf.12062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins LT, Zheng M, Liu Y, et al. Attitudes to marriage and sexual behaviours: a survey of gender and culture differences in China and United Kingdom. Sex Roles. 2002;46:75–89. [Google Scholar]
- Lau JT, Thomas J, Lin CK. HIV-related behaviours among voluntary blood donors in Hong Kong. AIDS Care. 2002;14:481–92. doi: 10.1080/09540120208629667. [DOI] [PubMed] [Google Scholar]
- Hong J, Loke AY. Hong Kong young people’s blood donation behaviour. Asian J Transfus Sci. 2011;5:49–52. doi: 10.4103/0973-6247.76000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sojka BN, Sojka P. The blood donation experience: self-reported motives and obstacles for donating blood. Vox Sang. 2008;94:56–63. doi: 10.1111/j.1423-0410.2007.00990.x. [DOI] [PubMed] [Google Scholar]
- Groothuis PA, Whitehead JC. Does don’t know mean no? Analysis of “don’t know” responses in dichotomous choice contingent valuation questions. Appl Econ. 2002;34:1935–40. [Google Scholar]
- Wang H. Treatment of “Don’t know” responses in contingent valuation surveys: a random valuation model. J Environ Econ Manag. 1997;32:219–32. [Google Scholar]
- Kalichman SC, Nachimson D. Self-efficacy and disclosure of HIV-positive serostatus to sex partners. Health Psychol. 1999;18:281–7. doi: 10.1037//0278-6133.18.3.281. [DOI] [PubMed] [Google Scholar]
- Fielding R, Lam TH, Hedley A. Risk-behavior reporting by blood donors with an automated telephone system. Transfusion. 2006;46:289–97. doi: 10.1111/j.1537-2995.2006.00714.x. [DOI] [PubMed] [Google Scholar]