Abstract
Methods
A matched case–control study was conducted among 591 consecutive patients with diabetes attending a tertiary hospital in Dhaka and 591 controls matched for age, sex and area of residence without diabetes not related with the index–case. Depression was measured using the Patient Health Questionnaire–9. Multivariate logistic regression was performed to examine the association between depression and diabetes.
Results
The mean age (±standard deviation) of the participants was 50.4 ± 11.4 years, with a male to female ratio of 43:57. The prevalence of depression was 45.2% and 19.8% among cases and controls, respectively. In the multivariate analysis, mild as well as moderate to severe depression were significantly associated with diabetes and independent of sociodemographic factors and co–morbidity (adjusted odds ratio (OR) = 2.0, 95% confidence interval (CI) = 1.4–2.9 and adjusted OR = 6.4, 95% CI = 3.4–12.3; P < 0.001 for both).
Conclusion
The high prevalence and strong association of depression in individuals with diabetes in Bangladesh suggests that depression should be routinely screened for patients with diabetes at the clinics and that management strategies adequate for resource–poor settings need to be developed. Further research to determine the pathophysiological role of depression in the development of diabetes is merited.
Diabetes and depression are two major non–communicable diseases which have become global epidemics and cause significant mortality and morbidity [1–3]. Worldwide, there are 382 million people with diabetes and within next two decades this number is projected to increase to 592 million with an increasing trend in the younger population [1]. The International Diabetes Federation (IDF) estimated that in 2013, diabetes caused 5.1 million deaths and cost US$ 548 billion in health care spending [1]. Diabetes is a major global cause of premature mortality, reduced quality of life, and imposes huge social and economic impact on health care systems, households and nations as a whole [1]. The global burden of disease study predicted that by 2030, depression is set to become the leading disease with 6.3% of the overall disease burden, and diabetes will be in 10th place with 2.3% of the overall disease burden as a percentage of the overall disability adjusted life years [4].
Diabetes and depression often present together and represent a major clinical challenge as the outcome of each condition can be worsened by the other [5]. Several studies have reported that comorbid diabetes and depression produced the greatest level of disability compared to other conditions, predicted sub–optimum outcomes, and incurred higher health care costs that increased with depression severity [6–9]. Despite high rates of comorbid depression in patients with diabetes, depression is often unrecognized and untreated in approximately two–thirds of patients in primary care settings [10].
The prevalence of both diabetes and depression are increasing in Southeast Asia [11]. Previous studies in Bangladesh have reported that the prevalence of depression among patients with diabetes was between 15.3–36% [12–15]. However, two of these studies had no control group [13–15] whereas the other two were population–based studies with relatively small numbers of incident cases of diabetes and insufficient data to examine sociodemographic and other factors potentially influencing the association of depression and diabetes [12,14]. Based on the data available, it is difficult to appreciate the true magnitude of the problem of depression among individuals with diabetes in Bangladesh as well as exclude important confounding factors. To close these knowledge gaps, we conducted a matched case–control study of individuals with and without diabetes at a large outpatient treatment facility in the Bangladeshi capital city, Dhaka. We hypothesized that persons with diabetes would have higher prevalence of depression than persons without diabetes.
METHODS
Study design, population and place
We conducted a matched case–control study among 1182 participants from January to July 2014 in the outpatient department (OPD) of the Bangladesh Institute of Health Sciences (BIHS) hospital. Detailed methods have been published elsewhere [16]. In brief, 591 consecutive patients with diabetes diagnosed by the BIHS attending physicians were recruited as cases. For each index–case, we recruited one control matched for age (±5 years), sex and area of residence from the persons accompanying other patients in the OPD waiting room. All individuals aged between 20–60 years were eligible for the study. Inclusion criteria for cases were: diagnosis of diabetes according to WHO criteria by attending BIHS physician. We excluded participants who were pregnant, had a terminal illness such as cancer or required urgent medical attention.
The BIHS is a 500–bed national–level tertiary health care covers all disciplines of medicine under a single roof having modern biomedical laboratory and research institute for diabetes affiliated with the Diabetes Association of Bangladesh and World Diabetic Federation. The OPD of BIHS hospital has one of the largest diabetes patient’s turnover in Bangladesh and serves a diverse population of about 2.2 million in Dhaka city and nearby districts.
Data collection process
Data were collected by a team consisting of one project research physician, one research officer and three research assistants experienced in hospital data collection. The team was trained for 4 weeks on diabetes epidemiology, study design, study aims and objective, interview skills, research ethics, anthropometric and blood pressure measurements. The research tools and instruments were developed by the Health Economic Group of the International Diabetes Federation (IDF) and translated into Bengali as per WHO standards of translating and back–translating. The questionnaires were pre–tested in a similar setting in BIRDEM hospital OPD for 25 cases and 25 control subjects. Feedback from the field testing was used to improve the language and contents of the questionnaire and tools.
The questionnaire contained information about socio–demographic factors such as age, sex, marital status, education, occupation, income, history of depression, diabetes, family history of diabetes, smoking history, and self–reported complications (eye, hypertension, cardiovascular diseases, kidney diseases, etc). Weight, height, and hip and waist circumference were measured using standard protocol. Blood pressure was measured using digital blood pressure monitor (Omron, SEM–1, Omron Corporation, Japan). Two repeated measurements were recorded after an interval of 5 minutes, alternating right and left hands and the average of two readings was considered. Hypertension was defined as systolic blood pressure (SBP)≥140 mm Hg and/or diastolic blood pressure (DBP)≥90 mm Hg as per JNC 7 guideline. Blood tests on HbA1c were measured at the BIHS Research Laboratory.
Level of depression was measured using the Patient Health Questionnaire (PHQ–9) which consists of nine items on a 4–point Likert–type scale with scores ranging from 0–27 corresponding to the Diagnostic and Statistical Manual of Mental Disorder (DSM–IV) diagnostic criteria for major depressive disorder [17]. Depression scores of 0–4, 5–9, and ≥10 was used to classify minimal, mild and moderate to severe depression, respectively [18]. The PHQ–9 is one of the most widely used depression screening tools in primary health care and a cut–off score of ≥10 has shown to have 88% sensitivity and 88% specificity to diagnose major depression [19]. In this study we used a previously developed and evaluated Bengali version of PHQ–9. The PHQ–9 and its cut–off points have been validated in Bangladeshi population and considered to be reliable tool for diagnosis of depression [13].
Data analysis
Data were entered into a Microsoft Access database with built–in range and consistency checks and analyzed using SPSS version 20 (IBM Corporation, NY, USA). Frequencies and percentages were calculated for categorical variables and mean±SD and median (Q1–Q3) were calculated for normality distributed and non–normally distributed continuous variable. T–test, χ2 and Mann-Whitney U tests were performed for differences between cases and controls. Univariate analysis was performed with diabetes as the dichotomous outcome variable. The category of the independent variable with the minimum level of association with diabetes was taken as reference value. Conditional logistic regression was performed to evaluate the association of depression and other independent variables with diabetes. Odds ratios (OR) are reported with their respective 95% confidence intervals (CI) and P–value. A P–value of less than 0.05 was considered significant.
RESULTS
A total of 1265 participants were approached for this study and 1240 (98%) agreed to participate. Of those, 40 individuals were not included in the study (15 controls who had a history of diabetes, 8 cases who were pregnant, 17 cases who had no medical records available at the time of data collection). Another 18 participants were excluded before data analysis due to matching problems and incomplete information. The final sample therefore consisted of 1182 participants.
Characteristics of the study participants
The study included 1182 participants with a male to female ratio of 43:57 and mean age (±standard deviation) of 50.4 ± 11.4 years. The majority of the participants were married and Muslims. About two–thirds of the participants completed secondary education or higher. About half of the participants were housewives, and one–third were service holders or businessmen. The overall median (Q1–Q3) household income was BDT 25 000 (15 000–60 000) or US$ 323.42 (194.05–776.20) and about two–thirds earned BDT 30 000 (US$ 388.10) or less per month (US$ 1 = BDT 77.3, 2014). Self–reported complications generally associated with diabetes (hypertension, cardiovascular diseases (CVD) and eye problems) were significantly higher among persons with diabetes than persons without diabetes (52.8% vs 19.3%, 10% vs 3.4% and 60.1% vs 38.1% respectively). Current tobacco use was higher among persons without diabetes than persons with diabetes (P = 0.04). The prevalence of hypertension measured by systolic blood pressure (SBP) and diastolic blood pressure (DBP) was higher for persons with diabetes than persons without diabetes (35.2% vs 28.1%, P = 0.009). Waist circumference and waist–hip ratio was significantly higher for persons with diabetes than persons without diabetes. Persons with diabetes also had a higher number of complications than persons without diabetes (1.76 ± 1.2 vs 2.05 ± 1.34). Persons with diabetes reported taking higher number of medication than persons without diabetes (3.67 ± 1.76 vs 1.79 ± 1.07) (Table 1).
Table 1.
Characteristics of study participants
| Variables | Case n = 591 | Control n = 591 | Total n = 1182 | P–value | |||
|---|---|---|---|---|---|---|---|
| n |
% |
n |
% |
n |
% |
||
|
Age (years): | |||||||
| Mean±SD |
51.4 ± 11.6 |
49.5 ± 11.1 |
50.4 ± 11.4 |
0.004 |
|||
| <40 |
96 |
16.2 |
115 |
19.5 |
211 |
17.9 |
0.027 |
| 40–49 |
142 |
24.0 |
144 |
24.4 |
286 |
24.2 |
0.027 |
| 50–59 |
194 |
32.8 |
215 |
36.4 |
409 |
34.6 |
0.027 |
| ≥ 60 |
159 |
26.9 |
117 |
19.8 |
276 |
23.4 |
0.027 |
|
Sex | |||||||
| Male |
255 |
43.1 |
255 |
43.1 |
510 |
43.1 |
1.0 |
| Female |
336 |
56.9 |
336 |
56.9 |
672 |
56.9 |
1.0 |
|
Marital status: | |||||||
| Married |
476 |
80.5 |
517 |
87.5 |
993 |
84.0 |
0.001 |
| Single |
115 |
19.5 |
74 |
12.5 |
189 |
16.0 |
0.001 |
|
Education: | |||||||
| No education |
116 |
19.6 |
76 |
12.9 |
192 |
16.2 |
0.001 |
| Primary |
103 |
17.4 |
96 |
16.2 |
199 |
16.8 |
0.001 |
| Secondary |
190 |
32.1 |
178 |
30.1 |
368 |
31.1 |
0.001 |
| Higher secondary and above |
182 |
30.8 |
241 |
40.8 |
423 |
35.8 |
0.001 |
|
Household monthly income (BDT): | |||||||
| Median (in thousands) (Q 1–3) |
25 (15–42) |
25 (16–40) |
25 (15–60) |
0.714 |
|||
| ≤BDT 30 000 |
338 |
63.7 |
353 |
63.8 |
691 |
63.7 |
0.951 |
| >BDT 30 000 |
193 |
36.3 |
200 |
36.2 |
393 |
36.3 |
0.951 |
|
Occupation: | |||||||
| Unemployed |
6 |
1.0 |
9 |
1.5 |
15 |
1.3 |
<0.001 |
| Service |
170 |
28.8 |
248 |
42.0 |
418 |
35.4 |
<0.001 |
| Housewife |
309 |
52.3 |
271 |
45.9 |
580 |
49.1 |
<0.001 |
| Others (retired, labors, etc) |
106 |
17.9 |
63 |
10.7 |
196 |
14.3 |
<0.001 |
|
Self–reported complications: | |||||||
| Hypertension |
312 |
52.8 |
114 |
19.3 |
426 |
36.0 |
<0.001 |
| Cardiovascular diseases (CVD) |
59 |
10 |
20 |
3.4 |
79 |
6.7 |
<0.001 |
| Eye problems |
355 |
60.1 |
225 |
38.1 |
580 |
49.1 |
<0.001 |
|
Tobacco use: | |||||||
| Never |
471 |
79.7 |
445 |
75.3 |
916 |
77.5 |
0.040 |
| Former (stopped 6 months) |
6 |
1.0 |
2 |
0.3 |
8 |
0.7 |
0.040 |
| Current (in last 6 months) |
114 |
19.3 |
144 |
24.4 |
258 |
21.8 |
0.040 |
|
Depression (PHQ–9): | |||||||
| No or minimal depression (0–4) |
324 |
54.8 |
474 |
80.2 |
798 |
67.5 |
<0.001 |
| Mild depression (5–9) |
167 |
28.3 |
100 |
16.9 |
267 |
22.6 |
<0.001 |
| Moderate to severe depression (≥10) |
100 |
16.9 |
17 |
2.9 |
117 |
9.9 |
<0.001 |
|
Hypertension (SBP>140 /or DBP>90): |
208 |
35.2 |
166 |
28.1 |
374 |
31.6 |
0.009 |
|
Body Mass Index (BMI): | |||||||
| Underweight (<18.5 kg/m2) |
9 |
1.5 |
18 |
3.1 |
27 |
2.3 |
0.071 |
| Normal (18.5 –24.9 kg/m2) |
219 |
37.1 |
235 |
39.9 |
454 |
38.5 |
0.071 |
| Overweight (25–29 kg/m2) |
274 |
46.4 |
271 |
46.0 |
545 |
46.2 |
0.071 |
| Obese (≥30 kg/m2) |
88 |
14.9 |
65 |
11 |
153 |
13.0 |
0.071 |
|
Waist circumference (WC): | |||||||
| Normal (≤90 cm M; ≤80 cm F) |
154 |
26.1 |
215 |
36.4 |
369 |
31.2 |
<0.001 |
| High (>90 cm M, >80 cm F) |
437 |
73.9 |
376 |
63.6 |
813 |
68.8 |
<0.001 |
|
Waist–to–hip ratio (WHR): | |||||||
| Normal (<0.90 M, <0.80 F) |
29 |
4.9 |
55 |
9.3 |
84 |
7.1 |
0.003 |
| High (≥0.90 M, ≥0.80 F) |
562 |
95.1 |
536 |
90.7 |
1098 |
92.9 |
0.003 |
|
Number of complications: | |||||||
| No complication |
91 |
15.4 |
240 |
40.6 |
331 |
28.0 |
<0.001 |
| 1–3 |
451 |
76.3 |
328 |
55.5 |
779 |
65.9 |
<0.001 |
| >3 |
49 |
8.3 |
23 |
3.9 |
72 |
6.1 |
<0.001 |
| Median (IQR) |
2 (2) |
2 (2) |
2 (2) |
<0.001 |
|||
|
Number of medications: | |||||||
| 1–2 |
157 |
27.2 |
98 |
80.3 |
255 |
36.4 |
<0.001 |
| 3–4 |
259 |
44.8 |
21 |
17.2 |
280 |
40.0 |
<0.001 |
| >4 |
162 |
28.0 |
3 |
2.5 |
165 |
23.6 |
<0.001 |
| Median (IQR) | 3(3) | 1(1) | 3(2) | <0.001 | |||
SD – standard deviation, IQR – interquartile range, Q – quartile, BDT – Bangladeshi Taka, PHQ – Patient Health Questionnaire, SBP – systolic blood pressure, DBP – diastolic blood pressure, M – male, F – female, BMI – body mass index (kg/m2)
Prevalence of depression
The prevalence of depressive illness was found higher among persons with diabetes (28.3%) than persons without diabetes (16.9%; P < 0.001). The prevalence of moderate to severe depression was 16.9% in persons with diabetes vs 2.9% in persons without diabetes (P < 0.001) (Table 1 and Figure 1).
Figure 1.
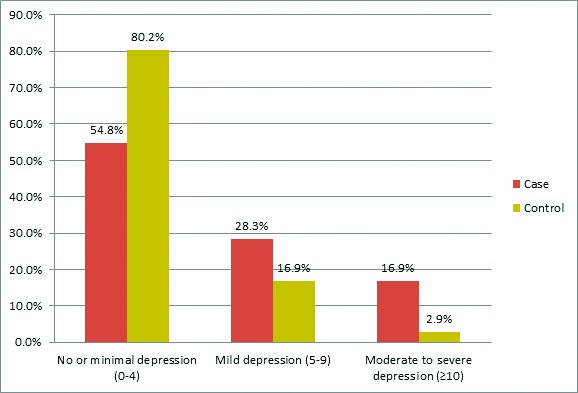
Prevalence of depression among study participants using PHQ–9.
Association between diabetes and depression
Table 2 shows the univariate analysis of factors associated with diabetes with unadjusted OR and 95% CI. No depression or minimal and moderate to severe depression were significantly associated with diabetes (OR = 2.7, 95% CI = 2.0–3.8) and (OR = 9.9, 95% CI = 5.4–18.0), respectively. Other factors found to be significantly associated with diabetes were age ≥40 years, secondary and higher education (inverse association), housewife or other occupation (such as retirees, day laborers), marital status single, obesity, hypertension and having higher number of complications (Table 2).
Table 2.
Univariate analysis of factors associated with diabetes
| Variables | Odds ratio (OR) | Confidence interval | P–value |
|---|---|---|---|
|
Depression: | |||
| Minimal depression (0–4) |
Ref |
||
| Mild depression (5–9) |
2.7 |
2.0–3.8 |
<0.001 |
| Moderate to severe depression (≥10) |
9.9 |
5.4–18.0 |
<0.001 |
|
Education: | |||
| No education |
Ref |
||
| Primary |
0.7 |
0.5–1.1 |
0.093 |
| Secondary |
0.7 |
0.5–1.0 |
0.034 |
| Higher secondary and above |
0.5 |
0.3–0.7 |
<0.001 |
|
Age: | |||
| <40 |
Ref |
||
| ≥40 |
4.2 |
1.7–10.2 |
0.002 |
|
Household monthly income (BDT): | |||
| ≤BDT 30 000 |
Ref |
||
| >BDT 30 000 |
1.0 |
0.8–1.3 |
0.842 |
|
Occupation: | |||
| Unemployed |
Ref |
||
| Service |
1.1 |
0.4–3.2 |
0.876 |
| Housewife |
3.1 |
1.0–9.6 |
0.048 |
| Others (retired, labors, etc) |
3.2 |
1.0–9.7 |
0.046 |
|
Marital status: | |||
| Married |
Ref |
||
| Single |
1.7 |
1.2–2.4 |
0.001 |
|
BMI: | |||
| Underweight (<18.5 kg/m2) |
0.5 |
0.2–1.2 |
0.098 |
| Normal (18.5–24.9 kg/m2) |
Ref |
||
| Overweight (25–29.9 kg/m2) |
1.1 |
0.9–1.4 |
0.435 |
| Obese (≥30 kg/m2) |
1.5 |
1.0–2.1 |
0.044 |
|
Hypertension: | |||
| Absent |
Ref |
||
| Present |
1.4 |
1.1–1.8 |
0.009 |
|
Number of complications: | |||
| No complication |
Ref |
||
| 1–3 |
4.0 |
2.9–5.6 |
<0.001 |
| >3 | 6.7 | 3.7–12.0 | <0.001 |
BMI – body mass index (kg/m2)
Table 3 presents the results of conditional logistic regression analyses for factors associated with diabetes after adjusting for confounders. No depression or minimal and moderate to severe depression were significantly associated with diabetes (OR = 2.0, 95% CI = 1.4–2.9) and (OR = 6.4, 95% CI = 3.4–12.3) respectively. Having 1–3 complications (OR = 3.1, 95% CI = 2.2–4.4), ≥3 complications (OR = 3.1, 95% CI = 1.5–6.2), other occupations (OR = 4.9, 95% CI = 1.3–18.0) and completing higher secondary education and above (OR = 0.52, 95% CI = 0.3–0.8) were also significantly associated with diabetes, controlling for other confounding variables.
Table 3.
Conditional logistic regression analyses for factors associated with diabetes
| Variables | Odds ratio (OR) | Confidence interval | P-value |
|---|---|---|---|
|
Depression: | |||
| No or minimal depression (0–4) |
Ref |
||
| Mild depression (5–9) |
2.0 |
1.4–2.90 |
<0.001 |
| Moderate to severe depression (≥10) |
6.4 |
3.4–12.3 |
<0.001 |
|
Age (years): | |||
| <40 |
Ref |
||
| ≥40 |
1.71 |
0.65–4.47 |
0.278 |
|
Education: | |||
| No education |
Ref |
||
| Primary |
0.76 |
0.46–1.24 |
0.269 |
| Secondary |
0.76 |
0.48–1.19 |
0.224 |
| Higher secondary and above |
0.52 |
0.33–0.83 |
0.006 |
|
Occupation: | |||
| Unemployed |
Ref |
||
| Service or business |
1.70 |
0.49–5.83 |
0.400 |
| Housewife |
3.67 |
0.98–13.75 |
0.054 |
| Others |
4.92 |
1.34–18.00 |
0.016 |
|
Marital status: | |||
| Married |
Ref |
||
| Single |
1.50 |
1.00–2.26 |
0.051 |
|
BMI: | |||
| Underweight (<18.5 kg/m2) |
0.32 |
0.11–0.96 |
0.042 |
| Normal (18.5–24.9 kg/m2) |
Ref |
||
| Overweight (25 –29.9 kg/m2) |
1.14 |
0.83–1.55 |
0.420 |
| Obese (≥30 kg/m2) |
1.36 |
0.85–2.17 |
0.194 |
|
Hypertension: | |||
| Absent |
Ref |
||
| Present |
1.24 |
0.91–1.68 |
0.171 |
|
Number of complications: | |||
| No complication |
Ref |
||
| 1–3 |
3.07 |
2.15–4.38 |
<0.001 |
| >3 | 3.06 | 1.52–6.17 | 0.002 |
BMI – body mass index (kg/m2)
DISCUSSION
This study, to the best of our knowledge, is the first matched case–control study determining the prevalence of depression among people with and without diabetes in Bangladesh that also measures the association between depression and diabetes. Our study showed that depression, particularly in a moderate to severe form, is much more common among those with diabetes than those without the disease. In addition, we found that the association of depression and diabetes is independent of socio–demographic factors and diabetes–associated complications.
Several longitudinal studies have reported that increased depressive symptoms at baseline are associated with incident type 2 diabetes [7,20,21]. Several factors associated with depression, such as physical inactivity, hypercaloric diet, neuroendocrine and inflammatory responses resulting in increased cortisol, catecholamines, and cytokines can induce insulin resistance leading to the development of diabetes [7]. A meta–analysis showed that the risk of developing type 2 diabetes was 37% higher in depressed adults than in non–depressed adults [22].
Conversely, the psychosocial demands of diabetes management, lifestyle change, incidence of complications and resulting functional impairment may influence depression severity, decrease quality of life, and contribute to prolonged or recurrent episodes of depression [23]. Depression in patients with chronic illness might cause nonspecific amplification of physical symptoms associated with the medical condition [24]. Compared to non–depressed patients, patients with major depressive disorders were 2 to 5 times more likely to report the presence of 10 diabetic symptoms after controlling for a number of diabetes complications [25]. These results are in line with our findings of an increased number of complications associated with diabetes which might lead to or aggravate depression.
Depressive symptoms are associated with decreased glycemic control and increased diabetic complications, which worsen depression and lessen response to antidepressant treatment [26]. Previous studies have shown that the correlation between depression and poor diabetic self–care is consistent across diverse socioeconomic and cultural groups [27,28]. Comorbid depression in patients with diabetes is also associated with increased numbers and severity of diabetic symptoms and complications [29,30]. A meta–analysis demonstrated a clinically significant relation between depression and several diabetic complications [31]. Our results show that patients with more complications had 3 times the odds to be significantly associated with diabetes.
Previous studies have shown that type 2 diabetes is associated with an increased risk of depressive symptoms [32,33]. A Bangladeshi study reported 31.6% of comorbid depression among patients with type 2 diabetes while the prevalence of depression in persons without diabetes was 12.6%, which is similar to our findings [14]. Another study in Bangladesh reported 36.2% of participants with moderate to severe depression, which was significantly higher among females [34]. A worldwide survey by WHO reported that 9.3% of patients with diabetes also had depression [6]. A meta–analysis reported that people with type 2 diabetes have a 24% increased risk of incident depression compared with people without diabetes [35]. A study in China reported that depression was three times higher among persons with diabetes compared to those without diabetes [36]. Our results show a much higher prevalence of depressive symptoms among patients with diabetes compared to previous studies in Bangladesh, which might be due to selection of samples from a specialized hospital as well as the use of different scale and cut–off values to measure depression. Also, participants with moderate to severe depression in our study had 6.4 times higher odds of having diabetes, which is almost double what is reported by a study from China [36].
A recent systematic review reported that the prevalence of depression among individuals with diabetes is higher in population with low socioeconomic status in low–and–middle–income countries. However, the available evidence base was small [10]. We found that the association of diabetes and depression was independent of an individual’s education and household income in our sample. Additionally, it was not affected by other socio–demographic factors, BMI, hypertension, or the number of diabetes–associated complications.
Even in well–funded health care systems, depression is under diagnosed and undertreated in individuals with diabetes [5]. In Bangladesh, where there is a shortage of trained workforce in mental health and diabetes, patients with comorbid diabetes and depression are even less likely to receive adequate management for both conditions [37]. This may contribute to the fact that diabetes management in Bangladesh is suboptimal even in the best clinical settings, and the majority of the patients present with high rates of complications [38].
Strengths and limitations
The strength of this study is the matched case–control design which controlled for the age, sex and area of residence of the study participants during the recruitment stage. Both case and controls were recruited at the same time, under similar conditions, by the same research assistants and from the same source population reducing confounding bias. The limitations of this study include that controls were selected on the basis of self–reported absence of diabetes, which could not be verified by laboratory investigations. However, our study physician ensured that the controls were not on any anti–diabetic medications. We used PHQ–9 which was not designed to measure clinical depression. However, PHQ–9 is an efficient and valid tool and has been commonly used to identify depression in primary health care in previous studies [13,39]. Furthermore, we measured depression at a single–time point and did not consider the use of antidepressants, which might have misclassified our participants. Finally, our data on complications are self–reported by participants for cardiovascular diseases, eye problems and kidney diseases which could not be verified by clinical or laboratory investigations. They were however verified to the extent possible by a review of the participants’ medical records. Well–designed longitudinal studies with objective measurements of clinical complications and measures of neuroendocrine markers will help to establish the direction of association and pathophysiology of both depression and diabetes among the Bangladeshi population.
CONCLUSION
The prevalence of depression, particularly moderate to severe, is very high among adult Bangladeshis with diabetes. Therefore, patients with diabetes should be routinely screened for depression in Bangladesh and probably similar other developing countries. Management strategies and guidelines adequate for the country level need to be developed and further research to determine the pathophysiological role of depression in the development of diabetes in Southeast Asians is merited.
Acknowledgments
ICDDR,B gratefully acknowledges the following donors which provide unrestricted support: Australian Agency for International Development (AusAID), Government of the People’s Republic of Bangladesh, Canadian International Development Agency (CIDA), Swedish International Development Cooperation Agency (SIDA), and the Department for International Development, UK (DFID). We thank the study team and participants for their contribution to the study. We express our deep thanks and gratitude to Prof. MHA Rouf, Director, BIHS Hospital and colleagues at CIH, LMU for support in different stages of the study. We also thank Mr. Pear Hossain, Statistical Officer, CCCD, ICDDR,B for assisting in data analysis and Ms. Natalie Linton, Oregon State University, USA for editorial assistance.
Ethics approval: The objectives and importance of the research were explained to all participants prior to recruitment. Participation in the study was voluntary. The confidentiality of the participants was maintained, and written informed consent was obtained from all participants. The study was approved by the Research Review Committee and Ethical Review Committee of the International Center for Diarrhoeal Diseases Research, Bangladesh (PR–13062) and obtained an ethical clearance waiver from Ludwig–Maximilians Universität (LMU) and BIHS.
Funding: This research protocol was funded by ICDDR,B’s core Sida Grant Number GR–01014. Shariful Islam also received support from Center for International Health (CIH), Ludwig–Maximilians–Universität (LMU), Munich, Germany, DAAD, BMZ and Exceed as PhD scholar for this study. The funding organizations had no role in the design and conduct of the study; collection, management, analysis and interpretation of data; or preparation, review or approval of the manuscript, or decisions to submit for publication.
Authorship declaration: SI, the principal investigator, is involved in concept, design, developing the intervention and the instruments, as well as in the implementation, analysis and reporting aspects of the study. LN and AL were involved in all aspects of the study and provided expert advice for the study design and writing of manuscript. UF and JS were involved in study design and reviewing the protocol. All authors have read and approved the final version of the manuscript.
Competing interests: All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author). None of the participating authors has a conflicting financial or other interest related to the work detailed in this manuscript.
REFERENCES
- 1.International Diabetes Federation. IDF Diabetes Atlas, 6th ed. Brussels: International Diabetes Federation, 2013. [Google Scholar]
- 2.Egede LE, Ellis C. Diabetes and depression: global perspectives. Diabetes Res Clin Pract. 2010;87:302–12. doi: 10.1016/j.diabres.2010.01.024. [DOI] [PubMed] [Google Scholar]
- 3.Islam SM, Purnat TD, Phuong NTA, Mwingira U, Schacht K, Fröschl G, et al. Non‐Communicable Diseases (NCDs) in developing countries: a symposium report. Global Health. 2014;10:81. doi: 10.1186/s12992-014-0081-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. The global burden of disease: 2004 update. Geneva: World Health Organization; 2008. Annex C, Analysis Categories and mortality data sources, 2009, pp.120–31. [Google Scholar]
- 5.Holt RI, de Groot M, Lucki I, Hunter CM, Sartorius N, Golden S, et al. NIDDK international conference report on diabetes and depression: current understanding and future directions. Diabetes Care. 2014;37:2067–77. doi: 10.2337/dc13-2134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet. 2007;370:851–8. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 7.Golden SH, Lazo M, Carnethon M, Bertoni AG, Schreiner PJ, Roux AVD, et al. Examining a bidirectional association between depressive symptoms and diabetes. JAMA. 2008;299:2751–9. doi: 10.1001/jama.299.23.2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160:3278–85. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- 9.Egede LE, Zheng D, Simpson K. Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care. 2002;25:464–70. doi: 10.2337/diacare.25.3.464. [DOI] [PubMed] [Google Scholar]
- 10.Leone T, Coast E, Narayanan S, de Graft Aikins A. Diabetes and depression comorbidity and socio–economic status in low and middle income countries (LMICs): a mapping of the evidence. Global Health. 2012;8:39. doi: 10.1186/1744-8603-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghaffar A, Reddy KS, Singhi M. Burden of non–communicable diseases in South Asia. BMJ. 2004;328:807–10. doi: 10.1136/bmj.328.7443.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Asghar S, Hussain A, Ali SM, Khan KAK, Magnusson A. Prevalence of depression and diabetes: A population‐based study from rural Bangladesh. Diabet Med. 2007;24:872–7. doi: 10.1111/j.1464-5491.2007.02136.x. [DOI] [PubMed] [Google Scholar]
- 13.Roy T, Parvin M, Mohiuddin KGB, Rahman M. Prevalence of co–morbid depression in out–patients with type 2 diabetes mellitus in Bangladesh. BMC Psychiatry. 2012;12:123. doi: 10.1186/1471-244X-12-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bhowmik B, Binte Munir S, Ara Hossain I, Siddiquee T, Diep LM, Mahmood S, et al. Prevalence of type 2 diabetes and impaired glucose regulation with associated cardiometabolic risk factors and depression in an urbanizing rural community in Bangladesh: a population–based cross–sectional study. Diabetes & Metabolism Journal. 2012;36:422–32. doi: 10.4093/dmj.2012.36.6.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rahman M, Rahman MA, Flora MS, Rakibuz-Zaman M. Depression and associated factors in diabetic patients attending an urban hospital of Bangladesh. Int J Collab Res Intern Med Public Health. 2011;3:65–76. [Google Scholar]
- 16.Shariful Islam SM, Lechner A, Ferrari U, Froeschl G, Niessen LW, Seissler J, et al. Social and economic impact of diabetics in Bangladesh: protocol for a case–control study. BMC Public Health. 2013;13:1217. doi: 10.1186/1471-2458-13-1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM–IV–TR Fourth Edition (Text Revision). Washington, DC: APA, 2000. [Google Scholar]
- 18.Kroenke K, Spitzer RL, Williams JB. The Phq‐9. J Gen Intern Med. 2001;16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kroenke K, Spitzer RL. The PHQ–9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002;32:509–15. doi: 10.3928/0048-5713-20020901-06. [DOI] [Google Scholar]
- 20.Carnethon MR, Biggs ML, Barzilay JI, Smith NL, Vaccarino V, Bertoni AG, et al. Longitudinal association between depressive symptoms and incident type 2 diabetes mellitus in older adults: the cardiovascular health study. Arch Intern Med. 2007;167:802–7. doi: 10.1001/archinte.167.8.802. [DOI] [PubMed] [Google Scholar]
- 21.Engum A. The role of depression and anxiety in onset of diabetes in a large population–based study. J Psychosom Res. 2007;62:31–8. doi: 10.1016/j.jpsychores.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 22.Knol MJ, Twisk J, Beekman WR, Heine ATF, Snoek RJ, Pouwer FJ. Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta–analysis. Diabetologia. 2006;49:837–45. doi: 10.1007/s00125-006-0159-x. [DOI] [PubMed] [Google Scholar]
- 23.Kinder LS, Katon WJ, Ludman E, Russo J, Simon G, Lin EH, et al. Improving depression care in patients with diabetes and multiple complications. J Gen Intern Med. 2006;21:1036–41. doi: 10.1111/j.1525-1497.2006.00552.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ciechanowski PS, Katon WJ, Russo JE, Hirsch IB. The relationship of depressive symptoms to symptom reporting, self–care and glucose control in diabetes. Gen Hosp Psychiatry. 2003;25:246–52. doi: 10.1016/S0163-8343(03)00055-0. [DOI] [PubMed] [Google Scholar]
- 25.Ludman EJ, Katon W, Russo J, Von Korff M, Simon G, Ciechanowski P, et al. Depression and diabetes symptom burden. Gen Hosp Psychiatry. 2004;26:430–6. doi: 10.1016/j.genhosppsych.2004.08.010. [DOI] [PubMed] [Google Scholar]
- 26.Lustman PJ, Clouse RE. Depression in diabetic patients: the relationship between mood and glycemic control. J Diabetes Complications. 2005;19:113–22. doi: 10.1016/j.jdiacomp.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 27.Lerman I, Lozano L, Villa AR, Hernández-Jiménez S, Weinger K, Caballero AE, et al. Psychosocial factors associated with poor diabetes self–care management in a specialized center in Mexico City. Biomed Pharmacother. 2004;58:566–70. doi: 10.1016/j.biopha.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 28.Park H, Hong Y, Lee H, Ha E, Sung Y. Individuals with type 2 diabetes and depressive symptoms exhibited lower adherence with self–care. J Clin Epidemiol. 2004;57:978–84. doi: 10.1016/j.jclinepi.2004.01.015. [DOI] [PubMed] [Google Scholar]
- 29.Black SA, Markides KS, Ray LA. Depression predicts increased incidence of adverse health outcomes in older Mexican Americans with type 2 diabetes. Diabetes Care. 2003;26:2822–8. doi: 10.2337/diacare.26.10.2822. [DOI] [PubMed] [Google Scholar]
- 30.Katon WJ, Rutter C, Simon G, Lin EH, Ludman E, Ciechanowski P, et al. The association of comorbid depression with mortality in patients with type 2 diabetes. Diabetes Care. 2005;28:2668–72. doi: 10.2337/diacare.28.11.2668. [DOI] [PubMed] [Google Scholar]
- 31.Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: a meta–analysis. Psychosom Med. 2001;63:619–30. doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 32.de Jonge P, Roy JF, Saz P, Marcos G, Lobo A. Prevalent and incident depression in community–dwelling elderly persons with diabetes mellitus: results from the ZARADEMP project. Diabetologia. 2006;49:2627–33. doi: 10.1007/s00125-006-0442-x. [DOI] [PubMed] [Google Scholar]
- 33.Maraldi C, Volpato S, Penninx BW, Yaffe K, Simonsick EM, Strotmeyer ES, et al. Diabetes mellitus, glycemic control, and incident depressive symptoms among 70–to 79–year–old persons: the health, aging, and body composition study. Arch Intern Med. 2007;167:1137–44. doi: 10.1001/archinte.167.11.1137. [DOI] [PubMed] [Google Scholar]
- 34.Islam SM, Rawal LB, Niessen LW. Prevalence of depression and its associated factors among patients with type 2 diabetes: A cross–sectional study in Dhaka, Bangladesh. Asian J Psychiatr. 2015 doi: 10.1016/j.ajp.2015.07.008. pii: S1876-2018(15)00166-5. [DOI] [PubMed] [Google Scholar]
- 35.Nouwen A, Winkley K, Twisk J, Lloyd CE, Peyrot M, Ismail K, et al. Type 2 diabetes mellitus as a risk factor for the onset of depression: a systematic review and meta–analysis. Diabetologia. 2010;53:2480–6. doi: 10.1007/s00125-010-1874-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhao W, Chen Y, Lin M, Sigal RJ. Association between diabetes and depression: sex and age differences. Public Health. 2006;120:696–704. doi: 10.1016/j.puhe.2006.04.012. [DOI] [PubMed] [Google Scholar]
- 37.Ahmed SM, Hossain MA, Raja Chowdhury AM, Bhuiya AU. The health workforce crisis in Bangladesh: shortage, inappropriate skill–mix and inequitable distribution. Hum Resour Health. 2011;9:3–91. doi: 10.1186/1478-4491-9-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Islam SM, Alam DS, Wahiduzzaman M, Niessen LW, Froeschl G, Ferrari U, et al. Clinical characteristics and complications of patients with type 2 diabetes attending an urban hospital in Bangladesh. Diabetes Metab Syndr. 2015;9:7–13. doi: 10.1016/j.dsx.2014.09.014. [DOI] [PubMed] [Google Scholar]
- 39.Islam SMS, Lechner A, Ferrari U, Froesch G, Alam DS, Holle R, et al. Mobile phone intervention for increasing adherence to treatment for type 2 diabetes in an urban area of Bangladesh: protocol for a randomized controlled trial. BMC Health Serv Res. 2014;14:586. doi: 10.1186/s12913-014-0586-1. [DOI] [PMC free article] [PubMed] [Google Scholar]


