Abstract
Background:
A pre-packaged mixture of areca nut, tobacco, slaked lime, catechu, and flavoring agents is popularly known as Gutkha. Aim of study is to analyze the addiction biology of Gutkha chewing and to assess efficacy of a cessation program based on nicotine replacement therapy (NRT).
Materials and Methods:
Patterns of addiction of 400 Gutkha chewers were analyzed with a questionnaire-based survey. Urine cotinine levels of 60 subjects undergoing NRT were periodically estimated using gas chromatography.
Results:
Mean urine cotinine levels of relapse and relapse-free cases were 5800.38 µg/g of creatine and 5622.16 µg/g of creatine. The difference was not found to be statistically significant. A 83.3% of the subjects associated their chewing habit with day to day activities. Overall relapse rate was found to be 79%. The most common reported reason for relapse was unacceptable taste and form of nicotine chewing gums.
Conclusion:
Repetitive coexistence in time of an indifferent act and the act of chewing Gutkha where, the act of chewing is almost always preceded by the indifferent act sets in a conditioned reflex. Gutkha addiction can be considered as a form of conditioned reflex, rather than actual craving for nicotine.
Keywords: Conditioned reflex, Gutkha, nicotine replacement therapy, urine cotinine
Introduction
The history of tobacco use in India can be traced back to almost 400 years. The etiologic role of Gutkha, a prepackaged mixture of areca nut, Tobacco, slaked lime and flavoring agents in oral precancer and cancer is well documented.1 Currently, available nicotine replacement therapy (NRT) products like chewing gums, transdermal patches have achieved considerable success in smoking cessation. There are basic differences in the addiction of smoked and smokeless form of tobacco.2 So, there is a need to understand the biologic basis of Gutkha addiction to successfully achieve Gutkha cessation. Very few studies have been done to assess the exact nature of Gutkha addiction and to evaluate the efficacy of NRT products.2-4 The present study was aimed to analyze the addiction biology of Gutkha chewing and to evaluate the efficacy of cessation program based on NRT and psychological counseling.
Materials and Methods
A total of 400 male Gutkha chewers in the age group of 25-30 years with a minimum habit history of 5 years and employed in heavy industries were randomly selected for the study. They were enrolled in a preliminary questionnaire- based survey to analyze the pattern of addiction after obtaining written consent in accordance with the declaration of Helsinki (1975). All the 400 subjects underwent psychological counseling and were motivated to quit the habit. 60 subjects who consented for enrollment in the cessation program were divided into three groups. Subjects who chewed 1-5 Gutkha per day (n = 20) (Group A), subjects who chewed 6-10 Gutkha per day (n = 20) (Group B) and more than 10 Gutkha per day (n = 20) (Group C). Urine cotinine levels of subjects were determined by using capillary Gas chromatography (Shimadzu) on the 1st day of enrollment into the study. Among 400 subjects, 60 subjects were enrolled in a two armed cessation program after obtaining physicians consent. Arm one was pharmacological arm consisting of 4 mg nicotine polacrilex chewits 4-15 times per day for 1st week. Then depending on the compliance of subjects, dosage was altered to 2 mg Chewets 4-15 times per day for 2nd week. Relapse cases were immediately reported and divided into three groups. Group RA, RB, and RC were designated for the number of relapsed cases from Groups A, B, and C, respectively. Relapsed cases were excluded from the cessation program after estimating the urine cotinine levels. Comparison of mean urine cotinine levels of relapse cases and relapse-free cases was made within the same subgroups made on the basis of frequency of chewing. Arm two of the study comprised of periodic psychological counseling which was specifically designed on the basis of outcomes of questionnaire and involved explaining the patient about the degree of dependence, possible reasons for relapse and means of dealing with withdrawal symptoms.
Results
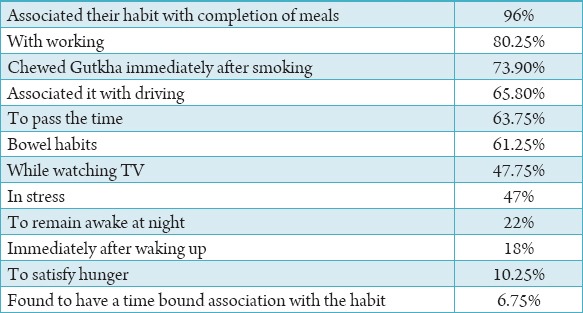
Among 400 randomly selected subjects, average frequency of Gutkha chewing was 4-15 times per day. 73.5% of Gutkha chewers were from lower socio-economic strata, 25.5% were from middle strata while only 1% subjects were from higher socio-economic strata. Close coexistence in time of chewing habit and day to day activities was observed (Table 1). The mean urinary cotinine level of Group A was 4680.91 µg/g creatine, Group B was 5898.22 µg/g creatine and Group C was 6287.35 ±3198 µg/g creatine.
Table 1.
Association of chewing habits and day to day activities.
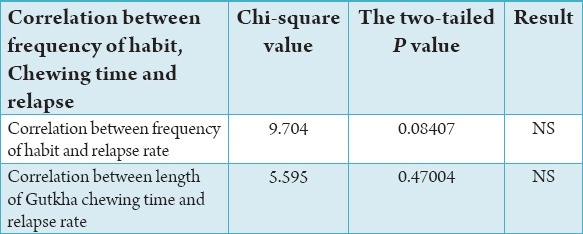
Among 60 subjects who underwent NRT, total relapse rate was found to be 79% at the end of 8th week. Relapse rate was higher in the first (41.6%) and second (37.9%) week of NRT. No relapse was found in the last week of therapy. The most common reported reason for relapse was unacceptable taste and form of nicotine chewing gums. Other factors reported for relapse were an adverse effect of NRT, gastrointestinal problems, and unsatisfactory effect of tobacco (Table 2). Chi-square analysis was done to check the correlation between frequency of habit and relapse, as well as chewing time and relapse. But, results were not statistically significant (Table 3). The intensity of craving was reported to be highest in the morning within 30 min after waking up. This finding was constant in all the subjects throughout 8 weeks. Results have showed that the relapse was more in lower (85.7%) and middle (83.3%) socio-economic class as compare to higher (33.3%) socio-economic class. Relapse was higher in illiterate persons (90%) than literate (80%). A mean urinary cotinine level of relapsed group (RA) was 5891.68 µg/g creatine, group (RB) was 6018.18 µg/g creatine, and group (RC) was 6001.28 µg/g creatine.
Table 2.
Reasons for relapse.
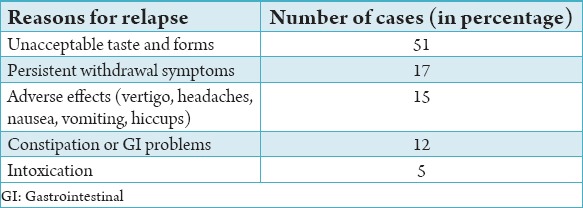
Table 3.
Correlation between the frequency of habit and relapse; chewing time and relapse.
Discussion
Various studies have shown a significant correlation between relapse and age, frequency of smoking, duration of habit, withdrawal symptoms such as craving and depressed mood in smokers.5-7 However, in the present study no statistically significant correlation was found between relapse rate and age, frequency, gender or time of chew. This shows that pattern of addiction of smoking and Gutkha chewing is different. Patients who abruptly stop using smokeless tobacco may experience withdrawal symptoms similar to that observed in smokers.8 The time course of withdrawal symptoms varied among individuals of all three study groups, but withdrawal symptoms were at its peak within a few days and then began to subside over the next several weeks. NRT does not appear to shorten the course of the symptoms but can reduce symptom severity to the generally more tolerable levels.9 In this study, 20% of subjects reported withdrawal symptoms even after taking NRT. NRT had no impact on the circadian rhythm of cravings. Intensity of craving was found to be highest in the morning. The differences between the urine cotinine levels of relapse-free and relapsed cases were not found to be statistically significant. This fact indicates that nicotine probably plays a minor role in Gutkha addiction. At present, there are very few NRT products specific to Gutkha cessation. These products do not take into account the pathways of addiction related to the oral sense of gratification caused by physical form and flavoring agents in Gutkha. This finding is suggestive of withdrawals being sustained by pathways other than nicotine. Thus, NRT could influence only a selected component of Gutkha. Arecoline present in Areca nut is reported to have profound effect on the cholinergic nervous system and has considerable addiction potential.10 The observations made in the present study probably suggest that in the absence of free of cost NRT products, motivational support, and periodic counseling, relapse rate would have been higher than that found in the present study.
Conclusion
There are basic differences in the addiction biology of Gutkha chewing and smoking. A Gutkha chewer relates the habit to daily activities. Gutkha addiction can be considered as a form of conditioned reflex, rather than actual craving for nicotine, which probably plays a minor role in addiction. However, addiction potential of nicotine cannot be completely ruled out. Further development of NRT products with similar physical form and flavor to Gutkha would probably aid in similar oral gratification and might lower the rates of relapse.
Footnotes
Conflicts of Interest: None
Source of Support: Nil
References
- 1.Nair U, Bartsch H, Nair J. Alert for an epidemic of oral cancer due to use of the betel quid substitutes gutkha and pan masala: A review of agents and causative mechanisms. Mutagenesis. 2004;19(4):251–62. doi: 10.1093/mutage/geh036. [DOI] [PubMed] [Google Scholar]
- 2.Arabi Z. How smokeless tobacco differs from smoking and nicotine replacement therapy. Curr Cardiovasc Risk Rep. 2008;2:439–45. [Google Scholar]
- 3.Ahmad MS, Ali SA, Ali AS, Chaubey KK. Epidemiological and etiological study of oral submucous fibrosis among gutkha chewers of Patna, Bihar, India. J Indian Soc Pedod Prev Dent. 2006;24(2):84–9. doi: 10.4103/0970-4388.26022. [DOI] [PubMed] [Google Scholar]
- 4.Benegal V, Rajkumar RP, Muralidharan K. Does areca nut use lead to dependence? Drug Alcohol Depend. 2008;97(1-2):114–21. doi: 10.1016/j.drugalcdep.2008.03.016. [DOI] [PubMed] [Google Scholar]
- 5.Burns EK, Levinson AH. Discontinuation of nicotine replacement therapy among smoking-cessation attempters. Am J Prev Med. 2008;34(3):212–5. doi: 10.1016/j.amepre.2007.11.010. [DOI] [PubMed] [Google Scholar]
- 6.Fortmann SP, Killen JD. Nicotine gum and self-help behavioral treatment for smoking relapse prevention: Results from a trial using population-based recruitment. J Consult Clin Psychol. 1995;63(3):460–8. doi: 10.1037//0022-006x.63.3.460. [DOI] [PubMed] [Google Scholar]
- 7.Yadav VK. Pharmacotherapy of smoking cessation and the Indian scenario. Indian J Pharmacol. 2006;38:320–9. [Google Scholar]
- 8.Mills EJ, Wu P, Lockhart I, Wilson K, Ebbert JO. Adverse events associated with nicotine replacement therapy (NRT) for smoking cessation. A systematic review and meta-analysis of one hundred and twenty studies involving 177,390 individuals. Tob Induc Dis. 2010;8:8. doi: 10.1186/1617-9625-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lerman C, Kaufmann V, Rukstalis M, Patterson F, Perkins K, Audrain-McGovern J, et al. Individualizing nicotine replacement therapy for the treatment of tobacco dependence: A randomized trial. Ann Intern Med. 2004;140(6):426–33. doi: 10.7326/0003-4819-140-6-200403160-00009. [DOI] [PubMed] [Google Scholar]
- 10.Winstock AR, Trivedy CR, Warnakulasuriya KA, Peters TJ. A dependency syndrome related to areca nut use: Some medical and psychological aspects among areca nut users in the Gujarat community in the UK. Addict Biol. 2000;5(2):173–9. doi: 10.1080/13556210050003766. [DOI] [PubMed] [Google Scholar]


