Abstract
Background
The aim of this study was to evaluate the feasibility of single-port video-assisted thoracic surgery (VATS) in the treatment of secondary spontaneous pneumothorax (SSP).
Methods
Twenty-four patients who were scheduled to undergo single-port VATS for SSP were studied. The medical records of the patients were retrospectively reviewed. The mean follow-up duration was 26.1±19.8 months. In order to evaluate the feasibility of single-port VATS for SSP, the postoperative results of single-port VATS (n=15) in patients with emphysema were compared with those of emphysematous patients who underwent three-port VATS (n=15) during the study period.
Results
Single-port VATS was feasible in 19 of 24 patients (79.2%), while an additional port was needed in five patients. In the single-port VATS patients, the median operation time, duration of chest tube drainage, and hospital stay were 84.0 minutes, one day, and two days, respectively. Postoperative complications included prolonged chest tube drainage for more than five days (n=1), wound infection (n=1), and vocal fold palsy (n=1). No recurrence of pneumothorax was observed during the follow-up period. The median operation time, duration of chest tube drainage, and hospital stay of the emphysematous patients who underwent single-port VATS were shorter than those who underwent three-port VATS group (p<0.05 for all parameters).
Conclusion
Single-port VATS proved to be a feasible procedure in the treatment of patients with secondary spontaneous pneumothorax.
Keywords: Video-assisted thoracic surgery (VATS), Secondary spontaneous pneumothorax, Lung wedge resections
INTRODUCTION
Secondary spontaneous pneumothorax (SSP) is associated with underlying pulmonary pathologies, such as chronic obstructive pulmonary disease, in contrast to primary spontaneous pneumothorax (PSP), which occurs in the absence of underlying lung disease [1]. Patients with SSP tend to exhibit more severe symptoms due to their underlying lung disease and frequently require active intervention, because the air leakage is less likely to stop spontaneously than in patients with PSP [2,3].
Since its introduction, video-assisted thoracic surgery (VATS) has proven to be as effective as thoracotomy in the treatment of pneumothorax, with an acceptable recurrence rate and few complications [4]. Recently, the single-port approach has been introduced as an alternative to conventional multi-port VATS for the treatment of PSP [5]. Single-port VATS has shown to have advantages over three-port VATS, including lower complication rates, shorter hospital stays, and less postoperative pain and paresthesia, and does not lead to increased recurrence rates [6–8]. Although single-port VATS is currently accepted as a treatment modality for PSP, its application to SSP is still limited due to the nature and clinical characteristics of the underlying disease processes. The aim of this study was to evaluate the feasibility of single-port VATS in the treatment of SSP.
METHODS
The study protocol was reviewed by our institutional review board and approved as a minimal-risk retrospective study (approval number, H-1212-002-445) that did not require individual consent based on the institutional guidelines for waiving consent.
Twenty-four SSP patients who were initially scheduled to undergo single-port VATS from July 2011 to December 2013 were enrolled. The etiologies of SSP were emphysema (n=18), catamenial pneumothoraces (n=4), and lymphangioleiomyomatosis (n=2) (Table 1). A high-resolution computed tomography scan of the chest was performed preoperatively in each case to examine the location and extent of bullae and blebs. The indications for surgery were recurrent pneumothorax, massive air leakage with a collapsed lung or increasing subcutaneous emphysema, and persistent air leakage for more than 48 hours despite chest tube drainage. The postoperative management protocol included the application of thoracic suction (−15 cm H2O) until the morning of postoperative day 1, a change to water-sealed drainage of the chest tube if no air leak existed, removal of the chest tube in the afternoon of postoperative day 1, and discharge of the patient. The perioperative pain management protocol included a preemptive intercostal nerve block using bupivacaine (20 mL of 0.5% bupivacaine), and oral medications every six hours postoperatively. If the regular oral medication was not sufficient for postoperative analgesic purposes, intravenous analgesics were administered. Epidural or intravenous patient-controlled analgesia was not used during the study period. Pain scores were evaluated using the visual analog scale, ranging from 0 (no pain) to 10 (worst pain ever experienced). Pain scores were obtained every eight hours by the assigned nurse. Patients underwent regular postoperative follow-up at our outpatient clinic at three- or four-month intervals. A retrospective review of their medical records was performed, including sex, age, underlying etiology, site of the pneumothorax, number of episodes, operation time, the duration of chest tube drainage, the length of their hospital stay, postoperative complications, postoperative pain, and whether recurrences took place. Operation time was defined as the time from the skin incision to the end of skin closure.
Table 1.
Characteristics of patients scheduled for single-port surgery (N=24)
| Variable | Value |
|---|---|
| Age (yr) | 50.8±16.8 |
| Sex (male:female) | 19:5 |
| Smoking history (pack-year) | 20.0±20.4 |
| Etiology | |
| Emphysema | 18 |
| Catamenial | 4 |
| Others | 2 |
| Site | |
| Right | 12 |
| Left | 11 |
| Bilateral | 1 |
| Previous episodes of pneumothorax | |
| None | 9 |
| One | 13 |
| Two or more | 2 |
| Follow-up duration (mo) | 16.2±6.8 |
Values are presented as mean±standard deviation or number.
In addition, the perioperative parameters of emphysematous SSP patients who underwent single-port VATS (n=15) were compared with those who underwent three-port VATS (n=15) during the same study period, in order to demonstrate the feasibility of single-port VATS for the treatment of SSP. The operations were all performed by a single surgeon, and the surgical method was determined according to the surgeon’s preference. The indications for surgery, postoperative management protocols, and perioperative pain management protocols were similar between the single-port VATS and the three-port VATS groups.
The patients underwent postoperative follow-up examinations, including a chest X-ray, at our outpatient clinic at one week and three months after discharge, and every six to 12 months postoperatively thereafter. Patients were interviewed by telephone to determine their condition if the last clinical visit had not been conducted at the scheduled time. The clinical and radiographic follow-up examinations were completed on June 30, 2014. Follow-up was complete in 100% (19 of 19) of patients, with a mean follow-up duration of 16.9±7.4 months.
1) Surgical technique
All operations were performed under general anesthesia using a double-lumen endotracheal tube and one-lung ventilation. The patient was placed in the lateral decubitus position. The single-port VATS technique was performed using a 2.5-cm skin incision made through the fifth intercostal space on the mid-axillary line. If the patient had a chest tube inserted anywhere other than the fifth intercostal space, the previous chest tube insertion site was used as the single port after extending the skin incision to 2.5 cm. The three-port VATS technique included the standard inverted-triangle positioning of the ports. An 11-mm trocar (Endopath XCEL bladeless trocar; Ethicon Endo-Surgery, Cincinnati, OH, USA) for the thoracoscope was placed through the seventh or eighth intercostal space on the mid-axillary line, the 2-cm working port for the stapler was placed through the fourth or fifth intercostal space on the anterior axillary line, and the 5-mm Thoracoport (United States Surgical Co., Norwalk, CT, USA) for the endograsper was placed through the sixth or seventh intercostal space on the posterior axillary line. Our operative strategy for SSP involved performing pulmonary wedge resection of the bullous lesion with the endoscopic stapler equipped with a bovine pericardial strip (Peri-Strips Dry; Synovis, St. Paul, MN, USA), and using absorbable polyglycolic acid felt (Neoveil; Gunze, Kyoto, Japan) and fibrin glue to reinforce staple lines in most cases, instead of performing mechanical pleurodesis.
2) Statistical analysis
Statistical analysis was performed with the IBM SPSS software package ver. 20.0 (IBM Co., Armonk, NY, USA). Data were expressed as mean±standard deviation, or median and interquartile range. Comparisons between groups were performed using the Student t-test or the Mann-Whitney test for continuous variables, and the chi-square test, Fisher’s exact test, or the linear-by-linear association method for categorical variables. Pain score changes between groups were compared using repeated-measures analysis of variance. All p-values <0.05 were considered to indicate statistical significance.
RESULTS
Single-port VATS was feasible in 19 of 24 patients (79.2%). An additional port was needed in five patients, due to a previous chest tube insertion site inappropriate for single-port VATS (n=1), an extremely small intercostal space (n=1), or severe pleural adhesion (n=3). The median operation time, duration of chest tube drainage, and hospital stay were 84.0 minutes, one day, and two days, respectively. The median visual analog pain scales on postoperative days 0 and 1 were 4 and 3, respectively. The postoperative complications were prolonged chest tube drainage for more than five days (n=1), wound infection (n=1), and vocal fold palsy (n=1). No recurrence of pneumothorax was observed during the follow-up period.
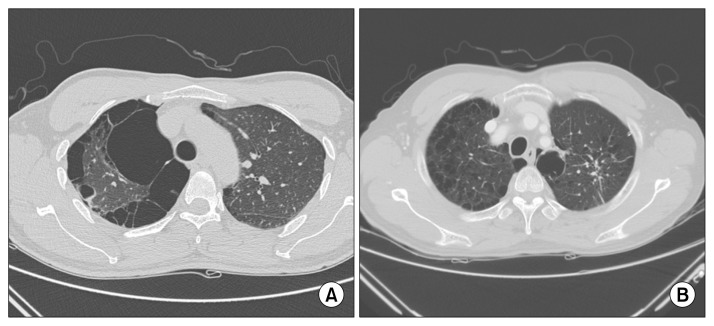
In order to demonstrate the feasibility of single-port VATS for the treatment of SSP, the patient characteristics and perioperative parameters were also compared between single-port VATS and three-port VATS within the subgroup of emphysematous SSP patients (Table 2). The severity of underlying emphysema was similar between the two groups, as shown in the typical findings of a chest computed tomography scan (Fig. 1). The median operation time (84.0 minutes vs. 114.0 minutes, p=0.023), the duration of chest tube drainage (one day vs. two days, p=0.045), and hospital stay (two days vs. three days, p=0.029) were shorter in the single-port group than in the three-port group, although the number of wedge resections during surgery was similar between the two groups (1.0 vs. 1.0, p=0.539). No significant differences were observed in the median postoperative pain score (visual analog score) on postoperative days 0 and 1 between the two groups (4 and 3 in the single-port group vs. 4 and 3 in the three-port group; p=0.935 and p=0.713, respectively). When the differences in changes in the pain score between the two groups were analyzed using repeated-measures analysis of variance, no statistically significant difference was found (p=0.882). Postoperative complications did not show a statistical difference between the two groups (p=0.539) (Table 2).
Table 2.
Operative outcomes of the single-port VATS and three-port VATS groups
| Variable | Single-port VATS, overall (n=19) | Single-port VATS, emphysema patients (n=15) | Three-port VATS, emphysema patients (n=15) | p-valuea) |
|---|---|---|---|---|
| Age (yr) | 49.8±17.9 | 54.9±15.7 | 65.8±4.8 | 0.056 |
| Smoking history (pack-year) | 19.2±19.4 | 24.3±18.7 | 35.9±22.1 | 0.161 |
| Operation time (min) | 84.0 (77.0–103.0) | 84.0 (77.0–103.0) | 114.0 (98.0–151.0) | 0.023 |
| No. of wedge resections | 1.0 (1.0–2.0) | 1.0 (1.0–1.0) | 1.0 (1.0–1.0) | 0.539 |
| Chest tube drainage (day) | 1.0 (1.0–2.0) | 1.0 (1.0–2.0) | 2.0 (2.0–4.0) | 0.045 |
| Hospital stay (day) | 2.0 (2.0–2.0) | 2.0 (2.0–2.0) | 3.0 (2.0–5.0) | 0.029 |
| Postoperative complications | 3 | 3 | 0 | 0.539 |
| Prolonged chest tube drainage (>5 day) | 1 | 1 | 1 | |
| Wound infection | 1 | 1 | 0 | |
| Vocal fold palsy | 1 | 1 | 0 | |
| Pain score | ||||
| Postoperative day 0 | 4.0 (3.0–5.0) | 4.0 (3.0–5.0) | 4.0 (2.0–6.0) | 0.935 |
| Postoperative day 1 | 3.0 (3.0–4.0) | 3.0 (2.0–3.0) | 3.0 (2.0–4.0) | 0.713 |
| Recurrence | 0 | 0 | 0 | 1.000 |
Values are reported as mean±standard deviation or as median (interquartile range).
VATS, video-assisted thoracic surgery.
Obtained by comparing the outcomes of single-port VATS (n=15) with three-port VATS (n=15) in the subgroup of patients whose etiology was emphysema.
Fig. 1.
Typical preoperative computed tomography scan findings of patients in (A) the single-port VATS and (B) the three-port VATS groups. VATS, video-assisted thoracic surgery.
DISCUSSION
The present study had two main findings. First, the majority of patients with secondary pneumothorax were managed by single-port VATS, although five patients (20.8%) required additional port insertion. Second, single-port VATS was feasible in the treatment of SSP, with a shorter operation time, duration of chest tube drainage, and hospital stay than was observed for three-port VATS.
In some studies of PSP, single-port VATS has been found to show better results than three-port VATS with regard to hospital stay, complication rates, and postoperative pain [6–8]. However, its application to SSP remains controversial. A previous study found that VATS did not demonstrate advantages over thoracotomy when used for SSP [9]. Both single-port and three-port VATS might be impossible to perform in SSP if all bullae and areas of severe adhesion must be removed and dissected. However, single-port VATS has been used to treat SSP because it in most cases of SSP, it would be sufficient to remove the bulla that was the origin of the air leakage. In the present study, single-port VATS was feasible in 19 of 24 patients (79.2%). An additional port was needed in five patients due to an inappropriate previous chest tube insertion site for single-port VATS, an extremely small intercostal space, or severe pleural adhesion.
Since this study was a retrospective observational study of our initial experiences with this surgical technique, it is inevitable that some degree of selection bias might exist. More severe and difficult cases may have been treated with three-port VATS, while less complicated and easier cases may have been preferentially treated with single-port VATS. The single-port VATS patients for SSP were younger and had a shorter history of smoking than the three-port VATS patients during the same study period. Therefore, it would be meaningless to compare the results of single-port VATS with those of three-port VATS in the overall sample included in the present study. Instead, the perioperative parameters of emphysematous SSP patients who underwent single-port VATS (n=15) were compared with those of emphysematous patients who underwent three-port VATS (n=15) in order to demonstrate the feasibility of single-port VATS for the treatment of SSP. The traditional thoracoscopic principle of triangulation is not applicable in single-port VATS, and it is not a naturally ergonomic technique [10]. Therefore, single-port VATS has limitations in surgical exposure and technical feasibility, and the operation time may be longer than is necessary for three-port VATS. In the present study, however, the median operation time, the duration of chest tube drainage, and the length of the hospital stay were no longer in the single-port group than in the three-port group, although the number of wedge resections was similar in both groups. These results suggest that single-port VATS is feasible, although selection bias still cannot be ruled out. One of the advantages of VATS in the treatment of pneumothorax is reduced postoperative pain in comparison with open thoracotomy [11]. Single-port VATS has been found to lead to a further decrease in postoperative pain and neurological symptoms in comparison to three-port VATS [7,12–14]. Previous studies have demonstrated that single-port VATS using a single-incision laparoscopic surgery port reduced postoperative pain due to its flexibility and the way in which pressure was absorbed [13,14]. The current study, however, failed to show the benefit of reduced postoperative pain in the single-port VATS group. This discrepancy may have arisen from the fact that a specialized instrument was not used and the pain scores were examined only on postoperative days 0 and 1. Longer follow-up of postoperative pain needs to be performed. Regarding the prevention of recurrent pneumothorax, VATS has been shown to have a similar recurrence rate to thoracotomy [15]. Another study found no difference in the recurrence rates between single-port VATS and three-port VATS in the treatment of PSP [6]. The present study suggested that no difference in recurrence rates exists between single-port VATS and three-port VATS in the treatment of SSP. No instances of recurrence occurred in either group during the follow-up period, which may have partially been due to the reinforcement materials used during surgery. An endoscopic stapler equipped with bovine pericardial strips was used, and absorbable polyglycolic acid felt and fibrin glue were also applied in most cases analyzed in this study.
In conclusion, single-port VATS proved to be a feasible procedure in most SSP patients. In order to improve the power of the study and to further demonstrate the feasibility and efficacy of single-port VATS in the treatment of SSP, further research involving a prospective randomized controlled trial should be carried out.
ACKNOWLEDGMENTS
This study was supported by a Grant of the Samsung Vein Clinic Network (Daejeon, Anyang, Cheongju, Cheonan; Fund No. KTCS04-039).
Footnotes
This paper was presented at the 46th Annual Meeting of the Korean Society for Thoracic and Cardiovascular Surgery, Yeosu, Oct 23rd–25th, 2015.
CONFLICT OF INTEREST
No potential conflict of interest relevant to this article was reported.
REFERENCES
- 1.Schramel FM, Postmus PE, Vanderschueren RG. Current aspects of spontaneous pneumothorax. Eur Respir J. 1997;10:1372–9. doi: 10.1183/09031936.97.10061372. [DOI] [PubMed] [Google Scholar]
- 2.MacDuff A, Arnold A, Harvey J BTS Pleural Disease Guideline Group. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010;65(Suppl 2):ii18–31. doi: 10.1136/thx.2010.136986. [DOI] [PubMed] [Google Scholar]
- 3.Schoenenberger RA, Haefeli WE, Weiss P, Ritz RF. Timing of invasive procedures in therapy for primary and secondary spontaneous pneumothorax. Arch Surg. 1991;126:764–6. doi: 10.1001/archsurg.1991.01410300110017. [DOI] [PubMed] [Google Scholar]
- 4.Lang-Lazdunski L, Chapuis O, Bonnet PM, Pons F, Jancovici R. Videothoracoscopic bleb excision and pleural abrasion for the treatment of primary spontaneous pneumothorax: long-term results. Ann Thorac Surg. 2003;75:960–5. doi: 10.1016/S0003-4975(02)04544-7. [DOI] [PubMed] [Google Scholar]
- 5.Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg. 2004;77:726–8. doi: 10.1016/S0003-4975(03)01219-0. [DOI] [PubMed] [Google Scholar]
- 6.Salati M, Brunelli A, Xiume F, et al. Uniportal video-assisted thoracic surgery for primary spontaneous pneumothorax: clinical and economic analysis in comparison to the traditional approach. Interact Cardiovasc Thorac Surg. 2008;7:63–6. doi: 10.1510/icvts.2007.165712. [DOI] [PubMed] [Google Scholar]
- 7.Jutley RS, Khalil MW, Rocco G. Uniportal vs standard three-port VATS technique for spontaneous pneumothorax: comparison of post-operative pain and residual paraesthesia. Eur J Cardiothorac Surg. 2005;28:43–6. doi: 10.1016/j.ejcts.2005.02.039. [DOI] [PubMed] [Google Scholar]
- 8.Yang HC, Cho S, Jheon S. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax using the SILS port compared with conventional three-port surgery. Surg Endosc. 2013;27:139–45. doi: 10.1007/s00464-012-2381-6. [DOI] [PubMed] [Google Scholar]
- 9.Passlick B, Born C, Haussinger K, Thetter O. Efficiency of video-assisted thoracic surgery for primary and secondary spontaneous pneumothorax. Ann Thorac Surg. 1998;65:324–7. doi: 10.1016/S0003-4975(97)01128-4. [DOI] [PubMed] [Google Scholar]
- 10.Chen PR, Chen CK, Lin YS, et al. Single-incision thoracoscopic surgery for primary spontaneous pneumothorax. J Cardiothorac Surg. 2011;6:58. doi: 10.1186/1749-8090-6-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Massard G, Thomas P, Wihlm JM. Minimally invasive management for first and recurrent pneumothorax. Ann Thorac Surg. 1998;66:592–9. doi: 10.1016/S0003-4975(98)00621-3. [DOI] [PubMed] [Google Scholar]
- 12.Rocco G. One-port (uniportal) video-assisted thoracic surgical resections: a clear advance. J Thorac Cardiovasc Surg. 2012;144:S27–31. doi: 10.1016/j.jtcvs.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 13.Gigirey Castro O, Berlanga Gonzalez L, Sanchez Gomez E. Single port thorascopic surgery using the SILS tool as a novel method in the surgical treatment of pneumothorax. Arch Bronconeumol. 2010;46:439–41. doi: 10.1016/j.arbres.2009.11.013. [DOI] [PubMed] [Google Scholar]
- 14.Berlanga LA, Gigirey O. Uniportal video-assisted thoracic surgery for primary spontaneous pneumothorax using a single-incision laparoscopic surgery port: a feasible and safe procedure. Surg Endosc. 2011;25:2044–7. doi: 10.1007/s00464-010-1470-7. [DOI] [PubMed] [Google Scholar]
- 15.Barker A, Maratos EC, Edmonds L, Lim E. Recurrence rates of video-assisted thoracoscopic versus open surgery in the prevention of recurrent pneumothoraces: a systematic review of randomised and non-randomised trials. Lancet. 2007;370:329–35. doi: 10.1016/S0140-6736(07)61163-5. [DOI] [PubMed] [Google Scholar]