Abstract
Objective
To describe the clinical epidemiology of extubation failure in a multicenter cohort of patients treated in pediatric cardiac ICUs.
Design
Retrospective cohort study using prospectively collected clinical registry data.
Setting
Pediatric Cardiac Critical Care Consortium registry.
Patients
All patients admitted to the CICU at Pediatric Cardiac Critical Care Consortium hospitals.
Interventions
None.
Measurements and Main Results
Analysis of all mechanical ventilation episodes in the registry from October 1, 2013, to July 31, 2014. The primary outcome of extubation failure was reintubation less than 48 hours after planned extubation. Repeated-measures analysis using generalized estimating equations to account for within patient and center correlation was performed to identify risk factors for extubation failure. Adjusted extubation failure rates for each hospital were calculated using logistic regression controlling for patient factors. Of 1,734 mechanical ventilation episodes (1,478 patients at eight hospitals) ending in a planned extubation, there were 100 extubation failures (5.8%). In multivariable analysis, only longer duration of mechanical ventilation was significantly associated with extubation failure (p = 0.01); the failure rate was 4% when ventilated less than 24 hours, 9% after 24 hours, and 13% after 7 days. For 503 patients intubated and extubated in the cardiac operating room, 15 patients (3%) failed extubation within 48 hours (12 within 24 hr). Case-mix-adjusted extubation failure rates ranged from 1.1% to 9.8% across hospitals. Patients failing extubation had greater median cardiac ICU length of stay (15 vs 3 d; p < 0.001) and in-hospital mortality (7.9 vs 1.2%; p < 0.001).
Conclusions
Though extubation failure is uncommon overall, there may be opportunities to improve extubation readiness assessment in patients ventilated more than 24 hours. These data suggest that extubation in the operating room after cardiac surgery can be done with a low failure rate. We observed variation in extubation failure rates across hospitals, and future investigation must elucidate the optimal strategies of high-performing centers to reduce ventilation time while limiting extubation failures.
Keywords: cardiac, cardiac surgery, extubation failure, mechanical ventilation
Greater than half of all patients treated in pediatric cardiac ICUs (CICUs) require mechanical ventilation immediately prior to admission (e.g., in a procedural suite) or during the CICU encounter (1). Assessment of extubation readiness in ventilated patients and choosing an approach to periextubation care represent two important decisions pediatric cardiac critical care clinicians must make on a routine basis. Previous single-center reports suggest that the rate of extubation failure in the CICU—defined as need for reintubation after a planned extubation—ranges from 3% to 10% (2–4). Failed trials of extubation associate with longer mechanical ventilation and intensive care duration and increased mortality among children mechanically ventilated in general PICUs (5, 6). As such, efforts to reduce the rate of extubation failure may represent an opportunity to improve outcomes for critically ill children with cardiovascular disease.
However, several questions remain unanswered surrounding extubation failure in the pediatric CICU. Extubation practices have changed over the last decade, with a move toward earlier extubation after cardiac surgery, and few descriptive data exist from a contemporary cohort of patients. Previous literature identifying risk factors for extubation failure in the CICU largely comes from single institution studies focused on a subset of patients, thus limiting the generalizability of the findings across centers and populations. Finally, the current literature offers no insight into the degree of variation in extubation failure across hospitals. Filling these and other knowledge gaps will be crucial to inform quality improvement initiatives for ventilated patients in the CICU.
In this context, we performed an analysis of the Pediatric Cardiac Critical Care Consortium (PC4) registry to describe the clinical epidemiology of extubation failure in a multicenter cohort of patients treated in pediatric CICUs. We aimed to characterize the rate and timing of extubation failure, to identify risk factors for extubation failure in a multi-institutional database, and to describe differences in rates of extubation failure across hospitals.
MATERIALS AND METHODS
Data Infrastructure
PC4 is a quality improvement collaborative currently including hospitals from North America who participate voluntarily (7). Data are submitted on all patients with primary cardiac disease admitted to the CICU under the care of a cardiac critical care attending physician. At the time of this data analysis, nine hospitals were submitting cases to the clinical registry. The registry collects patient demographics, CICU encounter characteristics, surgical data, critical care practices, and outcomes. Specific to the study, the date and time of initiation and endpoint of each mechanical ventilation episode is recorded, as is the type of airway, mode of ventilation, and whether an extubation is planned or unplanned. PC4 data entry for surgical variables uses common data definitions and terminology and is integrated with site’s local data collection for the Society of Thoracic Surgery Congenital Heart Surgery Database as previously described (7).
Trained data managers who pass an annual certification exam enter data into the registry. All data fields are defined according to standardized definitions in a data definitions manual that is available to all participants on the PC4 internal website. PC4 conducts weekly data collection team teleconferences to review variable definitions and resolve questions related to data entry. Cases cannot be submitted to the registry unless all mandatory data fields are complete, and approximately 90% of fields are required for submission. There were no missing data in the study cohort on variables necessary for the analysis.
The PC4 Data Coordinating Center audits every participating center on a regular schedule using a combined method of blind chart abstraction by auditors and source data verification. Each center contributing data to this analysis was audited for data integrity and accuracy; the audit included cases from the time period of the study. In addition, CICU census records are reviewed during the audit to be sure all cases that meet criteria are in the database. The results of the audit demonstrated a major discrepancy rate less than 1% across greater than 29,000 fields reviewed (M. Gaies, personal communication, 2015).
Participation in PC4 is considered quality improvement by the local institutional review board (IRB) at each site who participated in this study, and as such, the local IRB waived the need for approval. Data used for this analysis were deidentified prior to analysis.
Case Selection
We analyzed all hospitalizations with at least one CICU encounter that started on or after October 1, 2013, and were submitted by July 31, 2014. All courses of mechanical ventilation were reviewed, including those commencing in the cardiac operating room. Data collectors do not specifically record whether mechanical ventilation occurs in the operating room, but it was assumed that patients who had cardiovascular surgery with or without bypass had an endotracheal tube and were mechanically ventilated during the procedure.
We excluded data from one center that had submitted only 20 cases at the time of analysis because of small sample size. For patient-level analyses, we only used data from a patient’s initial hospitalization during the study period if there were multiple episodes. For ventilation episode-level analyses, we included each course of mechanical ventilation from every CICU encounter. The records of 10 patients (< 1% of all cases) were excluded either because of duplicate records of mechanical ventilation episodes that could not be resolved by the time of the analysis (n = 9) or because there was no mechanical ventilation recorded for a patient who was on extracorporeal membrane oxygenation (ECMO) for the entire duration of their CICU encounter (n = 1). Individual courses of mechanical ventilation were also excluded from the analysis for any one of the following criteria: 1) patient remained mechanically ventilated at CICU discharge/transfer, 2) tracheostomy in situ, or 3) extubation during withdrawal of support. Episodes where patients were previously intubated in any location other than the cardiac operating room (e.g., MRI, noncardiac operating room, and catheterization laboratory) and came to the CICU with a natural airway were not included because periprocedural intubation in these locations is not recorded in the registry.
Data Variables and Outcomes
Patient, preoperative, operative, and postoperative clinical variables were chosen a priori as potential risk factors of extubation failure. Weight-for-age z-score was calculated using World Health Organization or Centers for Disease Control standards, according to patient age (8). Airway anomalies known at the time of hospital admission were recorded. A patient was classified as having an airway anomaly if they had any of the following, based on International Pediatric and Congenital Cardiac Code definitions (9): major abnormality of the larynx-trachea-bronchus, congenital tracheal stenosis, laryngomalacia, tracheomalacia, bronchomalacia, or other major abnormality of the larynx-trachea-bronchus. We recorded newly acquired diaphragm paralysis and vocal cord dysfunction and included these variables in the analyses. Hospitalizations were classified as surgical if the patient had surgery at any time during the admission. The Society of Thoracic Surgeons-European Association for Cardiothoracic Surgery (STAT) mortality categories were used to classify surgical complexity (10). Finally, for nonsurgical hospitalizations, we recorded the reason for the initial CICU encounter and the primary medical diagnosis at admission (if applicable).
The primary outcome was extubation failure defined as need for reintubation within 48 hours after a planned extubation. Though other authors use variable time periods to define extubation failure (3, 11, 12), this investigative team believes that 48 hours is the most appropriate in the current era given the increasing use of noninvasive ventilation techniques that can decelerate the progression of respiratory failure. If a patient was extubated in the cardiac operating room and was subsequently reintubated in the CICU, this was recorded as an extubation failure. If a previously extubated patient was reintubated to go to the cardiac operating room for cardiovascular surgery this event was not included as an extubation failure. We further assessed the impact of failed extubation on in-hospital mortality, CICU and hospital length of stay (LOS), total duration of mechanical ventilation, and cardiac arrest or ECMO cannulation within 48 hours of a planned extubation.
Statistical Analysis
Data are presented as frequency (percentage) for categorical variables and median with interquartile range for continuous variables. Rates of extubation failure in the overall cohort and a subgroup of patients extubated in the operating room were also described as percentage. To identify patient and clinical characteristics associated with extubation failure, repeated-measures analysis using generalized estimating equations with a logit function was used to account for within-subject correlation when a patient had multiple ventilation episodes and correlation between outcomes of patients at the same center.
Factors associated with extubation failure in unadjusted analysis (p < 0.1) were subsequently included in the multivariable analysis to determine independent association with the primary outcome: neonatal status, airway anomaly, STAT category in surgical patients, reason for the initial CICU encounter, duration of mechanical ventilation, extubation in CICU, and vocal cord dysfunction. Unadjusted and adjusted odds ratios and their 95% CIs were reported. Due to the low number of failure events in the subgroup of patients who were extubated in the operating room and lack of intraoperative data around the time extubation, we did not pursue further analysis to identify risk factors in this subgroup. Clinical outcomes were compared between patients with and without extubation failure using Fisher exact test for categorical variables and Wilcoxon rank-sum test for continuous variables.
To describe rates of extubation failure across hospitals, we identified patient factors (present at admission and not influenced by intensive care practice) associated with the outcome at p value of less than 0.1 in the analysis described above, which included neonate status, STAT score 4–5 and nonsurgical status, and preexisting airway anomaly. We then calculated case-mix-adjusted rates of extubation failure by center using logistic regression controlling for these variables. All analyses were performed using SAS Version 9.4 (SAS Institute, Cary, NC), with statistical significance at a p value of less than 0.05.
RESULTS
Patient Characteristics
A total of 1,478 patients and 1,734 episodes of mechanical ventilation met inclusion criteria. Table 1 displays patient characteristics (patient diagnoses are presented in Supplemental Appendix A, Supplemental Digital Content 1, http://links.lww.com/PCC/A187). Infants comprised 55% of the cohort (n = 812), and 92% (n = 1,357) underwent cardiothoracic surgery at some point during their hospitalization with 20% in STAT categories 4 or 5. For nonsurgical patients, the primary diagnosis at CICU admission was either cardiovascular dysfunction or respiratory insufficiency (37/121, 31%); another 30% of nonsurgical patients were admitted directly from the catheterization laboratory or noncardiothoracic operating room and had no medical diagnosis as the reason for admission coded. Characteristics of patients extubated in the operating room after cardiothoracic surgery are shown in Table 2.
TABLE 1.
Patient Characteristics (n = 1,478 Patients)
| Male | 842 (57.0) |
|
| |
| Age at hospital admission, yr | 0.6 (0.2–5.1) |
| Neonate (< 30 d) | 327 (22.1) |
| Infant (30 d to 1 yr) | 485 (32.8) |
| Child (1–18 yr) | 568 (38.4) |
| Adult (> 18 yr) | 98 (6.6) |
|
| |
| Weight-for-age z-score at hospital admission | –0.9 (–2.1 to –0.2) |
|
| |
| Any chromosomal anomaly, syndrome, or extracardiac anomaly | 420 (28.4) |
|
| |
| Airway anomaly | 24 (1.6) |
|
| |
| Hospitalization type | |
| Surgical | 1,357 (91.8) |
| Medical | 121 (8.2) |
|
| |
| STAT category (for surgical patients) | |
| 1 | 479 (35.3) |
| 2 | 397 (29.3) |
| 3 | 170 (12.5) |
| 4 | 209 (15.4) |
| 5 | 62 (4.6) |
| Not assigned | 40 (2.9) |
|
| |
| Reason for first cardiac ICU encounter (medical patients) | |
| Preoperative cardiac surgery | 14 (11.6) |
| Medical condition | 70 (57.9) |
| Noncardiac postsurgery | 11 (9.1) |
| Post–cardiac catheterization | 26 (21.5) |
STAT = Society of Thoracic Surgeons-European Association for Cardiothoracic Surgery.
Data is presented as n (%) or median (interquartile range) as appropriate.
TABLE 2.
Patient Characteristics of Patients Extubated in the Operating Room After Cardiothoracic Surgery (n = 503 Patients)
| Characteristics | Extubation Failure
|
|
|---|---|---|
| Yes (n = 15) |
No (n = 488) |
|
| Male sex | 10 (66.7) | 281 (57.6) |
|
| ||
| Neonate (< 30 d) at hospital admission | 2 (13.3) | 30 (6.1) |
|
| ||
| Weight-for-age z-score at hospital admission | −1.1 (−2.5 to −0.4) | −0.7 (−1.7 to −0.4) |
|
| ||
| Weight-for-age percentile at hospital admission | 14.2 (0.6–33.4) | 24.8 (4.5–63.3) |
|
| ||
| Race (not mutually exclusive) | ||
| Caucasian | 10 (66.7) | 328 (67.2) |
| African American | 1 (6.7) | 63 (12.9) |
| Asian/Pacific islander/Native American | 1 (6.7) | 23 (4.7) |
| Other | 3 (20.0) | 102 (20.9) |
|
| ||
| Any chromosomal anomaly, syndrome, or extracardiac anomaly | 2 (13.3) | 106 (21.7) |
|
| ||
| Airway anomaly | 0 (0.0) | 3 (0.6) |
|
| ||
| STAT category | ||
| 1–3 | 11 (73.3) | 449 (92.0) |
| 4 or 5 | 4 (26.7) | 29 (5.9) |
| Unknown | 0 (0.0) | 10 (2.0) |
STAT = Society of Thoracic Surgeons-European Association for Cardiothoracic Surgery.
Data is presented as n (%) or median (interquartile range) as appropriate.
Epidemiology of Extubation Failure
Extubation failure occurred 100 times among the 1,734 mechanical ventilation episodes ending in a planned extubation (5.8%). The time to extubation failure is shown in Figure 1; 71% of failures transpired in the first 24 hours with 34% in the first 6 hours. Table 3 shows the clinical characteristics of all mechanical ventilation episodes comparing those with and without extubation failure. At the patient-level, 94% of patients (n = 1,387) were not reintubated within 48 hours of any planned extubation, 5% (n = 79) had one failure event, and 1% (n = 12) experienced multiple extubation failures. Including all events (i.e., those beyond 48 hr), 9% of patients required at least one reintubation after planned extubation. Among patients extubated in the cardiac operating room after cardiothoracic surgery (n = 503), 15 (3%) required reintubation in the CICU within 48 hours of admission.
Figure 1.
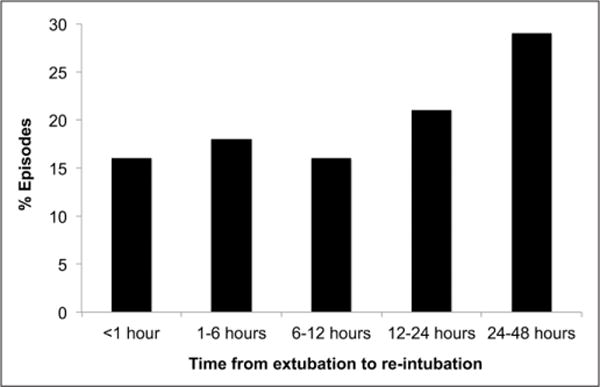
Time to extubation failure (n = 100 episodes). Values are expressed as the percentage of extubation failures within each time period.
TABLE 3.
Clinical Characteristics of Ventilation Episodes by Extubation Failure Status (n = 1,734 Ventilation Episodes)
| Characteristics | Overall (n = 1,734) |
Extubation Failure
|
|
|---|---|---|---|
| Yes (n = 100) |
No (n = 1,634) |
||
| Previous episodes of mechanical ventilation | 259 (14.9) | 25 (25.0) | 234 (14.3) |
|
| |||
| Time of the day of the extubation | |||
| Daytime (7:00 AM–5:00 PM) | 1,211 (69.8) | 71 (71.0) | 1,140 (69.8) |
| Off hours (5:01 AM–6:59PM) | 523 (30.2) | 29 (29.0) | 494 (30.2) |
|
| |||
| Day of the week of the extubation | |||
| Weekday (Monday–Friday) | 1,499 (86.4) | 82 (82.0) | 1,417 (86.7) |
| Weekend (Saturday/Sunday) | 235 (13.6) | 18 (18.0) | 217 (13.3) |
|
| |||
| Duration of mechanical ventilation, hr | 9.6 (4.0–44.1) | 32.8 (10.1–80.3) | 9.0 (4.0–41.4) |
| < 9.6 hr (median) | 869 (50.1) | 24 (24.0) | 845 (51.7) |
| 9.6–44.1 hr | 432 (24.9) | 33 (33.0) | 399 (24.4) |
| ≥ 44.1 hr (75th percentile) | 433 (25.0) | 43 (43.0) | 390 (23.9) |
|
| |||
| Extubation in cardiac ICU | 1,225 (70.6) | 85 (85.0) | 1,140 (69.8) |
|
| |||
| Final airway type used during mechanical ventilation course | |||
| Oral | 1,261 (72.7) | 78 (78.0) | 1,183 (72.4) |
| Nasal | 466 (26.9) | 21 (21.0) | 445 (27.2) |
| Unknown | 7 (0.4) | 1 (1.0) | 6 (0.4) |
|
| |||
| Diaphragm paralysis during the hospitalization | 21 (1.2) | 2 (2.0) | 19 (1.2) |
|
| |||
| Vocal cord dysfunction during the hospitalization | 52 (3.0) | 9 (9.0) | 43 (2.6) |
Data is presented as n (%) or median (interquartile range) as appropriate.
At the hospital level, we observed variation in the frequency of extubation failure. Adjusted and unadjusted rates of extubation failure by center are shown in Figure 2. Case-mix-adjusted rates ranged from 1.1% to 9.8% across the participating hospitals.
Figure 2.
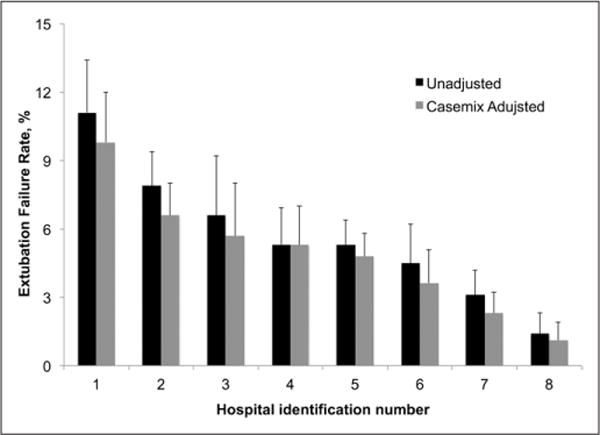
Extubation failure rates by center. Values are expressed as the percentage of ventilation episodes ending in extubation failure at a hospital. Dark bars represent the unadjusted rates, and the light bars represent the rates adjusted for patient factors (neonate, surgical complexity, and airway anomalies).
Assessing Risk Factors for Extubation Failure
Table 4 includes the results from unadjusted analysis of patient and episode factors associated with extubation failure after a planned extubation in the overall cohort, accounting for within-center correlations. Neonate status, greater surgical procedure complexity, nonsurgical status, admission for any reason other than postoperative cardiothoracic surgery, new vocal cord dysfunction, and duration of ventilation were all significantly associated with the primary outcome. Of note, chromosomal and extracardiac anomalies, weight-for-age z-score, time of day and day of week of extubation, and airway type (oral vs nasotracheal) were not associated with the likelihood of extubation failure.
TABLE 4.
Factors Associated With Reintubation Within 48 Hours After a Planned Extubation
| Characteristics | Unadjusteda
|
Adjustedb
|
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | AOR | 95% CI | p | |
| Male sex | 1.06 | 0.69, 1.62 | 0.79 | |||
|
| ||||||
| Neonate (< 30 d) at hospital admission | 3.36 | 2.21, 5.12 | < 0.0001 | 1.64 | 0.82, 3.31 | 0.16 |
|
| ||||||
| Weight-for-age z-score at hospital admission | 1.01 | 0.96, 1.07 | 0.65 | |||
|
| ||||||
| Any chromosomal anomaly, syndrome, or extracardiac anomaly | 1.25 | 0.80, 1.97 | 0.33 | |||
|
| ||||||
| Airway anomaly | 2.76 | 0.83, 9.22 | 0.098 | 2.74 | 0.90, 8.39 | 0.08 |
|
| ||||||
| Hospitalization type | ||||||
| Surgical | 0.58 | 0.30, 1.12 | 0.11 | |||
| Medical | Ref | |||||
|
| ||||||
| STAT category | 0.0003 | 0.51 | ||||
| Nonsurgical (i.e., medical) | 2.33 | 1.16, 4.65 | 0.02 | 1.41 | 0.62, 3.23 | 0.42 |
| 1–3 | Ref | Ref | ||||
| 4 or 5 | 2.82 | 1.81, 4.40 | < 0.0001 | 1.35 | 0.73, 2.47 | 0.34 |
|
| ||||||
| Reason for the initial CICU encounter | ||||||
| Postoperative cardiac surgery | Ref | Ref | ||||
| All others | 3.42 | 2.21, 5.30 | < 0.0001 | 1.56 | 0.74, 3.27 | 0.24 |
|
| ||||||
| Time of the day of the extubation | ||||||
| Daytime (7:00 AM–5:00 PM) | 0.96 | 0.56, 1.67 | 0.90 | |||
| Off hours (5:01 AM–6:59PM) | Ref | |||||
|
| ||||||
| Day of the week of the extubation | ||||||
| Weekday (Monday–Friday) | Ref | |||||
| Weekend (Saturday/Sunday) | 1.13 | 0.53, 2.39 | 0.75 | |||
|
| ||||||
| Duration of mechanical ventilation, hr | 0.001 | 0.01 | ||||
| < 9.6 hr (median) | Ref | Ref | ||||
| 9.6–44.1 hr | 3.22 | 1.89, 5.49 | < 0.0001 | 2.81 | 1.32, 6.00 | 0.01 |
| ≥ 44.1 hr (75th percentile) | 4.54 | 2.70, 7.64 | < 0.0001 | 2.54 | 1.14, 5.64 | 0.02 |
|
| ||||||
| Extubation in CICU | 1.97 | 0.97, 4.00 | 0.06 | 0.54 | 0.20, 1.47 | 0.23 |
|
| ||||||
| Final airway type used during mechanical ventilation course | ||||||
| Oral | 1.58 | 0.61, 4.14 | 0.35 | |||
| Nasal | Ref | |||||
|
| ||||||
| Diaphragm paralysis during the hospitalization | 2.13 | 0.54, 8.36 | 0.28 | |||
|
| ||||||
| Vocal cord dysfunction during the hospitalization | 3.49 | 1.77, 6.90 | 0.0003 | 1.92 | 0.89, 4.15 | 0.096 |
OR = (unadjusted) odds ratio, AOR = adjusted odds ratio, Ref = reference category, STAT = Society of Thoracic Surgeons-European association for cardiothoracic surgery, CICU = cardiac ICU.
p value from a repeated-measures analysis using generalized estimating equations accounting for within-center correlations only.
p value from a repeated-measures analysis using generalized estimating equations accounting for within-center correlations, age at hospital admission, airway anomaly, STAT category, reason for the initial CICU encounter, duration of mechanical ventilation, extubation in CICU, and vocal cord dysfunction during hospitalization.
In multivariable analysis including potential risk factors of extubation failure identified in univariate analyses, again accounting for center effects, only increasing duration of mechanical ventilation prior to extubation remained independently associated with extubation failure (Table 4). The rate of extubation failure by length of ventilation is illustrated in Figure 3.
Figure 3.
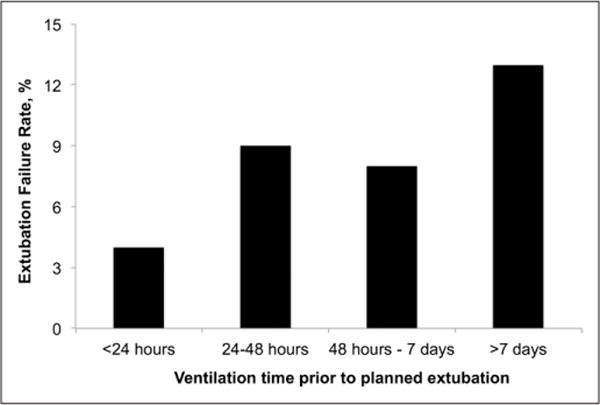
Extubation failure rate by length of ventilation. Values are expressed as the percentage of extubation failures based on length of mechanical ventilation prior planned extubation.
Impact of Extubation Failure on Patient Outcomes
Supplemental Table 1 (Supplemental Digital Content 2, http://links.lww.com/PCC/A188) displays outcomes for patients experiencing at least one extubation failure episode. Patients with extubation failure had significantly longer CICU LOS (median, 15 vs 3 d), hospital LOS (24 vs 7 d), and higher in-hospital mortality (7.9% vs 1.2%) compared with those that did not (all p < 0.001).
DISCUSSION
This study from a multi-institutional dataset describes the epidemiology of extubation failure in the largest cohort of CICU patients yet reported. Our analysis demonstrated that approximately 6% of planned extubations result in the need for reintubation within 48 hours. Of these, 71% of events occurred in the first 24 hours. We identified duration of ventilation prior to extubation as the only independent risk factor predictive of extubation failure, with the rate of failure increasing two-fold after only 24 hours of ventilation.
We also observed nine-fold variation in extubation failure rates across centers. These findings remain preliminary, and several areas must be explored before comparing hospitals using this outcome as a metric of hospital quality. Obtaining larger sample sizes and refining the method of adjusting for differences in case-mix across hospitals will be necessary in order to draw actionable conclusions. Patient and clinical characteristics associated with extubation failure are likely unique to the different subgroups of patients within the CICU population, such as neonates, nonsurgical patients, and those extubated in the operating room, among others. Ongoing data collection in the PC4 registry will support such analyses. These data do suggest that differences in extubation failure rates across hospitals are not solely due to differences in case-mix; it is likely that hospital perioperative and intensive care practices meaningfully impact the likelihood of extubation failure. The overarching goal of future work will be to identify high-performing centers and elucidate the key practices and resources that lead to lower extubation failure rates.
In this context, future research efforts to interpret extubation failure rates and compare hospitals to one another must evaluate duration of mechanical ventilation concomitantly. Defining an “acceptable” extubation failure rate remains an unresolved debate within the pediatric cardiac critical care community. Prevailing beliefs suggest that a goal of zero extubation failures would result in many patients being ventilated longer than necessary. Further, for patients with known or suspected critical airway anomalies that might require tracheostomy or another surgical procedure, it is often necessary to perform a trial of extubation, despite the high likelihood of failure, in order to progress to definitive treatment. For these and other reasons, the “best” approach to managing mechanical ventilation and extubation practices may be that which is aggressive enough to limit ventilation times in the majority of patients, but which also results in some extubation failures. Thoughtful, detailed analyses of hospital-level outcomes in both domains will provide the greatest opportunity to define best practice in the CICU.
The data from the present study illustrate increasing extubation failure rates for patients ventilated greater than 24 hours. Patient factors and disease severity are likely closely tied to the need for ventilation beyond 24 hours. We were able to control for some of these factors in our analysis, but there are no doubt unmeasured covariates that we could not include. Our findings mirror those of Kurachek et al (6) who showed that the rate of extubation failure goes up markedly after 48 hours (8.2%) and 10 days (17.5%) of ventilation in a general PICU cohort. Several previous investigations demonstrate the limitations of spontaneous breathing trials in critically ill children (13, 14) to predict successful transition from mechanical ventilation. Patients ventilated for prolonged periods in the CICU are more likely to suffer from clinically significant cardiovascular dysfunction compared with the general PICU population, which may also limit successful unassisted respiration. Taken together these data suggest a need for re-examination of extubation readiness assessment in patients with prolonged mechanical ventilation.
Our analysis of extubation failure in patients who are extubated in the operating room after cardiothoracic surgery provides important data around a practice gaining adoption across surgical centers (2, 4, 15–17). These single-center studies collectively report extubation failure rates in the CICU from 0% to 12% (4, 15, 16) and the patient populations assessed included neonates and other infants with complex procedures, as did ours. We were limited to measurement of extubation failure in patients who entered the CICU postoperatively with a natural airway; we could not determine extubation failures that occurred in the operating room. Ongoing research initiatives exist to study and promote the practice of extubation in the operating room and assess the costs and benefits of this strategy (W. Mahle, personal communication, 2015), and PC4 will continue to evaluate the perioperative extubation outcomes in this subgroup of high interest.
Comparison of our findings to previously reported data is complicated by differing definitions for extubation failure. Some authors (3, 11) used a different time period to define extubation failure (< 24 or for up to 96 hr after extubation), while others include use of noninvasive positive pressure ventilation as a criterion for failure (12, 18, 19). Our definition of extubation failure as need for reintubation within 48 hours is consistent with that in several other previous studies from both cardiac and general pediatric critical care populations (4–6). We did not include use of noninvasive ventilation in the definition because cardiac intensivists increasingly use these therapies at the time of transition to allow extubation of patients earlier than would otherwise be possible, and as such, this may not represent an extubation failure. Use of these therapies may also lengthen the time to reintubation in a patient ultimately destined for respiratory failure, and this influenced the choice of a 48-hour window to define extubation failure.
Common limitations associated with use of observational data also apply to our analysis. No clinical registry contains all the variables that may impact outcomes assessment through confounding or another mechanism. We could not evaluate the reasons for extubation failure; the registry does not include this field as it is not likely to be captured accurately through chart abstraction. The number of nonsurgical patients who receive mechanical ventilation in the CICU is small, and therefore, we were only able to include nonsurgical status as a categorical exposure variable in the final multivariable model. Future analyses of this subgroup are warranted as the risk factors for extubation failure may differ importantly from surgical patients. We do not capture newly diagnosed airway abnormalities and therefore clinically important tracheal or bronchial anomalies identified during the CICU encounter could not be assessed as a potential risk factor in the analysis. Though previously identified airway anomalies were not significantly associated with the primary outcome in multivariable analysis, the point estimate of the odds ratio suggests what would be clinically expected: that children with airway anomalies are at higher risk of failure.
CONCLUSIONS
Our analysis suggests that extubation failure in the CICU remains uncommon overall but is associated with important morbidities and increased hospital LOS. Opportunities may exist to improve assessment for extubation readiness in patients ventilated more than 24 hours. Future study must determine optimal strategies to reduce ventilation times while limiting extubation failures. This includes efforts to identify patients at low risk of harm, initiatives aimed at extubating them more consistently when ready early in the course of ventilation, and more accurately assessing those who are likely to fail so that they can be optimized prior to extubation. Assessment of variation in extubation failure rates between centers would allow identification of high-performing hospitals and the care processes underlying performance differences including general ventilation techniques, protocols for extubation readiness, and periextubation use of noninvasive ventilation strategies. Sharing best practices discovered through a collaborative learning model will likely reduce ventilation times and extubation failure and lead to improved outcomes across hospitals.
Supplementary Material
Acknowledgments
We acknowledge the data collection teams at the University of Michigan C.S. Mott Children’s Hospital, University of California-San Francisco Benioff Children’s Hospital, Medical University of South Carolina Children’s Hospital, Children’s Hospital of Philadelphia, Miami Children’s Hospital, Cincinnati Children’s Hospital and Medical Center, Children’s Hospital of Alabama, and Children’s National Medical Center for their efforts to provide the data for this investigation.
Footnotes
Listen to the iCritical Care podcasts for an in-depth interview on this article. Visit www.sccm.org/iCriticalCare or search “SCCM” at iTunes.
Analysis was performed at the Pediatric Cardiac Critical Care Consortium Data Coordinating Center within the Michigan Congenital Heart Outcomes Research and Discovery Program at the University of Michigan.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/pccmjournal).
Dr. Gaies receives support from the National Heart, Lung, and Blood Institute (K08HL116639, Principal Investigator) that indirectly supports this research. Dr. Gaies received support for article research from the National Institutes of Health (NIH). His institution received grant support from the NIH (K08 award from NHLBI [PI: Gaies]). Dr. Shekerdemian disclosed other support from Pediatric Research (Editorial Board Honorarium, $125 for 2014). Dr. Thiagarajan’s institution consulted for Bristol Myers Squibb (Events Adjudication Committee). Dr. Pasquali’s institution received grant support from the NHLBI and the Children’s Heart Foundation. Dr. Cooper lectured for Cadence and MedImmune and provided expert testimony for Keith L Davidson Law Offices. His institution received grant support from Grifols. The remaining authors have disclosed that they do not have any potential conflicts of interest.
References
- 1.Pediatric Cardiac Critical Care Consortium (PC4). Available at: http://pc4quality.org. Accessed February 28, 2015
- 2.Harris KC, Holowachuk S, Pitfield S, et al. Should early extubation be the goal for children after congenital cardiac surgery? J Thorac Cardiovasc Surg. 2014;148:2642–2647. doi: 10.1016/j.jtcvs.2014.06.093. [DOI] [PubMed] [Google Scholar]
- 3.Manrique AM, Feingold B, Di Filippo S, et al. Extubation after cardiothoracic surgery in neonates, children, and young adults: One year of institutional experience. Pediatr Crit Care Med. 2007;8:552–555. [PubMed] [Google Scholar]
- 4.Miller JW, Vu D, Chai PJ, et al. Patient and procedural characteristics for successful and failed immediate tracheal extubation in the operating room following cardiac surgery in infancy. Paediatr Anaesth. 2014;24:830–839. doi: 10.1111/pan.12413. [DOI] [PubMed] [Google Scholar]
- 5.Baisch SD, Wheeler WB, Kurachek SC, et al. Extubation failure in pediatric intensive care incidence and outcomes. Pediatr Crit Care Med. 2005;6:312–318. doi: 10.1097/01.PCC.0000161119.05076.91. [DOI] [PubMed] [Google Scholar]
- 6.Kurachek SC, Newth CJ, Quasney MW, et al. Extubation failure in pediatric intensive care: A multiple-center study of risk factors and outcomes. Crit Care Med. 2003;31:2657–2664. doi: 10.1097/01.CCM.0000094228.90557.85. [DOI] [PubMed] [Google Scholar]
- 7.Gaies M, Cooper DS, Tabbutt S, et al. Collaborative quality improvement in the cardiac intensive care unit: Development of the Paediatric Cardiac Critical Care Consortium (PC4) Cardiol Young. 2015;25:951–957. doi: 10.1017/S1047951114001450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control website. Available at: http://www.cdc.gov/growthcharts/. Accessed October 10, 2014
- 9.Jacobs JP, Jacobs ML, Mavroudis C, et al. Nomenclature and databases for the surgical treatment of congenital cardiac disease–An updated primer and an analysis of opportunities for improvement. Cardiol Young. 2008;18(Suppl 2):38–62. doi: 10.1017/S1047951108003028. [DOI] [PubMed] [Google Scholar]
- 10.Jacobs JP, Jacobs ML, Maruszewski B, et al. Initial application in the EACTS and STS Congenital Heart Surgery Databases of an empirically derived methodology of complexity adjustment to evaluate surgical case mix and results. Eur J Cardiothorac Surg. 2012;42:775–779. doi: 10.1093/ejcts/ezs026. discussion 779–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Edmunds S, Weiss I, Harrison R. Extubation failure in a large pediatric ICU population. Chest. 2001;119:897–900. doi: 10.1378/chest.119.3.897. [DOI] [PubMed] [Google Scholar]
- 12.Dodgen AL, Dodgen AC, Swearingen CJ, et al. Characteristics and hemodynamic effects of extubation failure in children undergoing complete repair for tetralogy of Fallot. Pediatr Cardiol. 2013;34:1455–1462. doi: 10.1007/s00246-013-0670-z. [DOI] [PubMed] [Google Scholar]
- 13.Randolph AG, Wypij D, Venkataraman ST, et al. Pediatric Acute Lung Injury and Sepsis Investigators (PALISI) Network: Effect of mechanical ventilator weaning protocols on respiratory outcomes in infants and children: A randomized controlled trial. JAMA. 2002;288:2561–2568. doi: 10.1001/jama.288.20.2561. [DOI] [PubMed] [Google Scholar]
- 14.Ferguson LP, Walsh BK, Munhall D, et al. A spontaneous breathing trial with pressure support overestimates readiness for extubation in children. Pediatr Crit Care Med. 2011;12:e330–e335. doi: 10.1097/PCC.0b013e3182231220. [DOI] [PubMed] [Google Scholar]
- 15.Mittnacht AJ, Thanjan M, Srivastava S, et al. Extubation in the operating room after congenital heart surgery in children. J Thorac Cardiovasc Surg. 2008;136:88–93. doi: 10.1016/j.jtcvs.2007.11.042. [DOI] [PubMed] [Google Scholar]
- 16.Garg R, Rao S, John C, et al. Extubation in the operating room after cardiac surgery in children: A prospective observational study with multidisciplinary coordinated approach. J Cardiothorac Vasc Anesth. 2014;28:479–487. doi: 10.1053/j.jvca.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 17.Hamilton BC, Honjo O, Alghamdi AA, et al. Efficacy of evolving earlyextubation strategy on early postoperative functional recovery in pediatric open-heart surgery: A matched case-control study. Semin Cardiothorac Vasc Anesth. 2014;18:290–296. doi: 10.1177/1089253213519291. [DOI] [PubMed] [Google Scholar]
- 18.Gupta P, McDonald R, Goyal S, et al. Extubation failure in infants with shunt-dependent pulmonary blood flow and univentricular physiology. Cardiol Young. 2014;24:64–72. doi: 10.1017/S1047951112002181. [DOI] [PubMed] [Google Scholar]
- 19.Gupta P, Chow V, Gossett JM, et al. Incidence, predictors, and outcomes of extubation failure in children after orthotopic heart transplantation: A single-center experience. Pediatr Cardiol. 2015;36:300–307. doi: 10.1007/s00246-014-1003-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


