Abstract
Objectives:
To investigate the effectiveness of topical anesthetic, 20% benzocaine in relieving pain and stress in patients following deep cavity restoration and extraction of teeth under local anesthesia (LA).
Methods:
A prospective clinical trial was conducted from October 2014 until April 2015 at Taibah University, Al Madinah Al Munawarah, Kingdom of Saudi Arabia. Forty-five patients were included in the 20% benzocaine group, and 46 in the normal saline group. Evaluation of the dental stress was made pre-operatively and immediately post-operative treatment using the visual analogue scale (VAS). Furthermore, discomfort of the injections were recorded by the patients after each treatment on standard 100 mm VAS, tagged at the endpoints with “no pain” (0 mm) and “unbearable pain” (100 mm).
Results:
There were statistically significant differences between the mean stress scores for patients in the benzocaine and normal saline groups post-operatively (p=0.002). There were significant differences between the mean pain scores for patients in the post buccal injection (p=0.001), post palatal injection (p=0.01), and the post inferior alveolar nerve block groups (p=0.02). Buccal, palatal, and inferior alveolar nerve block injections were more painful for patients in the normal saline group than the benzocaine group.
Conclusion:
This investigation has demonstrated that post-operative stress associated with deep cavity restoration and dental extractions under LA can be reduced by the application of topical anesthetic (20% benzocaine) at the operative site for intra-oral injections.
Anxiety is one of the most common causes of dental fear.1 There have been 3 stable and reliable factors, which contribute to dental fear. The first factor is related to patterns of dental avoidance and anticipatory anxiety, the second, related to fear, which is associated to specific dental stimuli and procedures, and the third is concerned with physiologic arousal during dental treatment.2 Fear develops through the interaction of 3 phenomena, those which are instinctive, dependent on maturation, and developed through learning from individual and social experience.3 It is unusual for modern local anesthetics to fail completely unless they have been injected incorrectly, but it is common for patients to retain some sensation of pressure around the tooth. Dental stress and anxiety may lead them to interpret this as pain, and cooperation is lost.4,5 Application of topical anesthetic for post-operative pain relief has not usually been considered as a part of routine clinical dental practice. However, infiltration local anesthesia (LA) has been used in other surgical disciplines with good effect.6,7 The field of anesthesia has witnessed many developments throughout the last century, and a number of different techniques and agents have been developed. Anesthesia has become an essential procedure in every surgical operation and treatment. In practice, topical anesthesia including cocaine, amethocaine, lignocaine, and prilocaine is applied to skin, eye, ear, nose, and mouth. Their application was reported to be useful and effective for reducing pain sensation.8 When used to produce topical anesthesia, they usually have a rapid onset of action (5-10 minutes [mins]), and a moderate duration of action (30-60 mins). A rapid onset of action of 5 mins or less has also been reported for 10% and 20% benzocaine gels for the relief of spontaneous toothache pain.9 Various preparations of lignocaine are available as aqueous solutions (4%), or in water-miscible bases, such as gels, ointments, creams, and sprays (2-10%). Intact skin works as a barrier preventing the diffusion of local anesthetics so high concentrations of anesthetic agents (for example, 20% benzocaine or 4% lignocaine) are required.8 The use of LA in dentistry is standard practice. No studies were found in the literature, which looked at the possibility of using benzocaine soaked rolls/swabs to reduce the post operative stress in adult patients following simple dental extractions, or deep cavity restoration. This study concentrated on the effectiveness of topical anesthetic 20% benzocaine for relieving pain of local anesthetic injection, and post-operative stress in patients following extraction of teeth, or deep restoration under LA.
Methods
This prospective study was conducted from October 2014 to April 2015 after obtaining the approval from the ethical committee. Patients who attended Taibah University, College of Dentistry (TUCoD), Al Madinah Al Munawarah, Kingdom of Saudi Arabia scheduled for extraction of teeth or deep cavity restoration under LA were considered for inclusion in the study. Using convenience-sampling pattern, 100 patients were selected to one of the 2 groups. Patients who fulfilled the following criteria were eligible for inclusion into the study: 1) male, aged 16-70 years of age. 2) scheduled for extraction of between 1-2 teeth or one deep cavity restoration. 3) American Society of Anesthesiologists I or II patients. 4) where the patient was able to understand and cooperate with the requirements of the protocol, and were able and willing to provide an appropriate written informed consent. Patients who were excluded from the study were hypersensitive or allergic to topical anesthesia, needed more than 3 teeth extraction, disliked the taste of the anesthetic, and refused to continue, or had vomiting reflex. Prior to the study, a researcher allocated the sequence of patient identity numbers to either the test or control group. Slips of paper with the test group or the control group were placed in opaque envelopes, and sealed by a secretary who was not associated with the study. These envelopes had been numbered sequentially on their outside with the patient identity number and was attached to the patient’s dental hospital treatment record.
On the dental chair, once the patient signed the consent a dental assistant placed the swab over the site of injection in the mouth for 20 second. If the slip in the envelope said that the patient was in the study group, small swabs were painted with topical anesthetic paste 20% benzocaine (Sky-Caine Gel, Skydent Inc., NY, USA). If the slip in the envelope said control group, the patient had the swab impregnated with cold normal saline mixed with one lozenge honey and lemon flavored Strepsils (Reckitt Benckiser Healthcare International Ltd., Nottingham, England). The slip was placed back in the envelope, which was placed back into the patients’ records. This ensured that the patient and the dentist carrying out the assessment were blind. Once the swabs were removed, the patient received 1.8 ml mepivacaine 2% with epinephrine 1:100,000. For the upper teeth, patients received buccal and palatal infiltrations. For lower teeth, they had either buccal and lingual infiltrations, or inferior alveolar nerve block additional to buccal injections. This was the usual clinical practice. Standard extraction techniques using elevators and dental forceps were employed. For deep caries, cavities prepared with high-speed contra angle hand piece.
The researcher was just an observer. Each patient was assessed for levels of stress, and these assessments were recorded using the visual analogue scale (VAS). The scores given were 0 if no sign of stress, or 100 for very severe stress. Evaluation of stress was made pre-operatively and immediately post-extraction. The discomfort of the injections were recorded by the patients after each treatment on standard 100 mm VAS, tagged at the endpoints with “no pain” (0 mm) and “unbearable pain” (100 mm). The researcher who made all the stress and pain observation was completely independent of the whole process. Statistical analysis was performed using Statistical Package for Social Sciences, version 21 (IBM Corp., Chicago, IL, USA). T-test was carried out to know significance level and p-value was adjusted to p<0.05. Sample size calculation was made for this study based on a study by Gazal and Mackie.10
Results
Out of the 100 patients, 6 were excluded because they fall into the exclusion criteria. Ninety-four patients were randomly allocated to one of the 2 groups. However, at the end of the study there were missing data for 3 patients (one in the normal saline group who fainted after local anesthetic injection, and 2 in the benzocaine group because their teeth extraction was performed surgically), giving 45 in the benzocaine group (study) and 46 in the normal saline group (control). Thus, the final sample size included 91 patients aged between 16-66 years (mean 37.70 years, standard deviation 14.50). The teeth had deep caries for restoration, or it was extracted due to gross caries, which could not be restored.
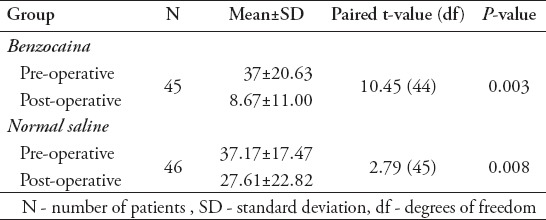
There were no statistically significant differences between the mean stress scores for the treatment (20% benzocaine) and control (normal saline) groups at the baseline assessment pre-operatively (p=0.97) (Table 1). However, there were statistically significant differences between the mean stress scores for the benzocaine and normal saline groups post-operatively (p=0.002) (Table 1). For both benzocaine and normal saline groups, changes in stress scores from the pre-operative score to the post-operative score were made using the paired sample t-test. There were significant decreases in stress scores between the pre-operative (p=0.003), and post-operative scores (p=0.008) (Table 2).
Table 1.
Comparisons between mean stresses scores for the benzocaine and normal saline groups pre-operatively and post-operatively.
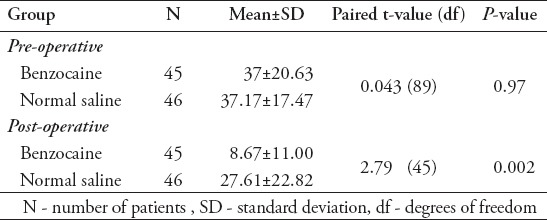
Table 2.
Comparisons between mean pre-operative stress scores and post-operative for patients in the benzocaine and normal saline groups.
The discomfort of the injections was recorded by the patients after each treatment on standard 100 mm VAS, tagged at the endpoints with “no pain” (0 mm) and “unbearable pain” (100 mm). There were significant differences between the mean pain scores for patients in the post buccal injection (p=0.001), post palatal injection (p=0.01), and the post inferior alveolar nerve block groups (p=0.02). These figures are illustrated in Table 3, Figures 1 A & B, and Figure 2 A & B.
Table 3.
Comparisons between mean post injections pain scores for patients in the benzocaine and normal saline groups.
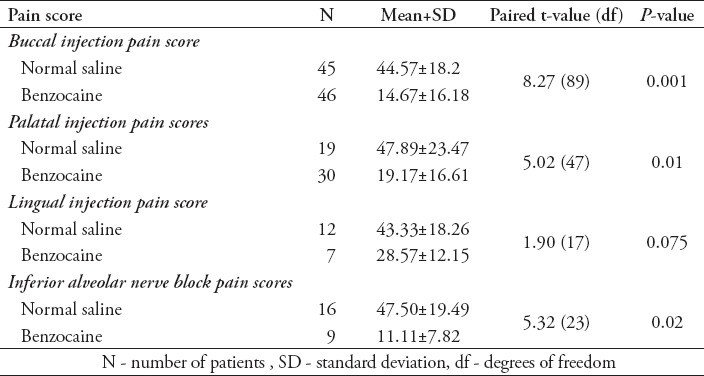
Figure 1.
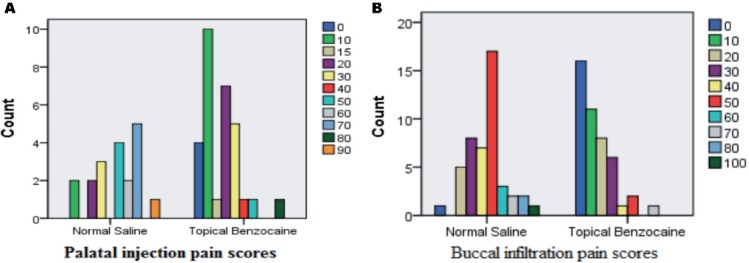
Pain scores compared between patients in benzocaine and normal saline groups regarding post buccal and palatal injections (A & B).
Figure 2.
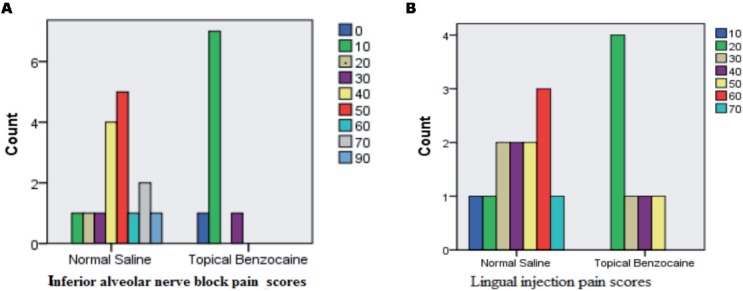
Pain scores compared between patients in benzocaine and normal saline groups regarding post lingual injection inferior alveolar nerve block.
Patients in the benzocaine group were more comfortable during administration of local anesthetic than the normal saline group. However, there were no significant differences between the mean pain scores for the patients in benzocaine and normal saline groups post lingual injection (p=0.075) (Table 3). Clinically, lingual injections were more painful for patients in the normal saline group than in the benzocaine group. This finding did not achieve a statistical significance because the number of patients who received lingual injections was small. Thus, a large sample size of patients in the lingual injection group might have significant differences in pain injection scores.
Discussion
Injection of LA is considered one of the main reasons for dental fear and dental visiting avoidance. Efforts have been performed to reduce pain perception of needle injection.11,12 Dental treatment fear and anxiety gradually builds up during childhood as results of a bad experience caused by dentist misbehavior, painful tooth preparation, or needle injection.13 Local anesthesia is necessary for a painless dental treatment. However, patients sometimes feel the needle puncturing the mucosa, or the pressure of depositing the local anesthetic solutions is painful. Different techniques have been employed in dentistry to minimize the pain on injection. Use of topical anesthesia, low-pressure injection, narrow, sharp needles, and a slow injection rate were not enough to achieve a completely painless injection under all circumstances.14 A large number of dentists believe that fearful patients are difficult and more stressful to treat, and they are most likely to attend appointments irregularly.15
The result of this study showed that there was a statistically significant difference in mean pain and stress scores between the patients in the topical benzocaine and those in the normal saline groups (p<0.05). The application of 20% benzocaine as a topical anesthetic for intraoral injections did reduce the pain of needle insertion, post-operative stress, and uneasiness connected with dental extractions under LA. The results of the current study are consistent with earlier findings of previous studies.16-18 All topical anesthetics are similarly reducing pain associated with needle puncture. When EMLA-60 was applied on oral mucosa, it seemed to have longer duration of action.15 Hodosh et al16 conducted a double-blind randomized control trial on 100 patients to investigate the effectiveness of a combination of different types of topical local an anesthetic for reducing pain during maintenance visits. A 35% potassium nitrate; 20% benzocaine; 10% tetracaine/aqueous hydroxyethyl cellulose gel was applied to the teeth and gingiva prior to hygienist-administered maintenance treatments. The outcome of this study revealed that the application effectively anesthetized the teeth and gingiva, so the dental work was performed with comfort. A study19 demonstrated that the combination of EMLA cream with propofol is beneficial and providing safe and effective pain management for lumbar punctures.
On the contrary, a study20 was conducted to evaluate the patient’s perceived pain response to the injection and anesthetic deposition for the greater palatine nerve block. Their findings revealed that the use of pressure and topical analgesia (20% benzocaine) did not reduce posterior palatal injection pain. However, in the current study, the patients in the benzocaine group reported less pain scores following palatal injection compared with those that are in the control group. From the clinical point of view, the palatal infiltration technique used in this study is more comfortable than the greater palatine nerve block because it minimizes the risk of direct contact of the needle with greater palatine nerve.
In this study, it was noticed by the dental surgeon who carried out all teeth extractions, that there was a group of patients who recorded a high level of dental stress at the baseline assessment; they scored less after completing the tooth extraction, or deep cavity preparation procedure. One possible explanation was given by these patients is that their needle phobia was eased off by having painless dental injections. Similarly, psychological processes, such as social appearance, anxiety, and blood injection phobia may affect the phobia of dental procedures. Targeting these points related psychological constructs may improve the management of dental anxiety among adult patients.21 Despite using topical benzocaine there was a group of patient who scored mild stress scores pre-operatively, they reported high level of stress post-operatively. These patients stated that seeing blood on the dental gauze and hearing the noise of surgical instruments during extraction procedure scared them and they became stressful post-operatively. However, dental injection pain can sometimes be a result of too rapid administration of local anesthetic, or due to the difference in pH value between the local anesthetic solution and the soft tissues in the mouth. Rapid injection can tear the tissue and result in immediate pain followed by soreness. The duration of discomfort varies a lot between different injections sites and techniques.22,23 Administration of oral ibuprofen pre-operatively in patients with irreversible pulpitis increased the success rates of inferior alveolar nerve block anesthesia and eased needle pain.24
In conclusion, this investigation has demonstrated that the post-operative stress associated with dental extractions and deep cavity restoration under LA can be reduced by the application of topical anesthetic (20% benzocaine) at the surgical site for intraoral injections. Topical anesthetic can be of value to help patients with needle phobia and reduce their level of fear. It is strongly recommended for all dental clinics and institutions to administer topical anesthetic before giving local anesthetic injections. In the study sample only males were included as only male patients are treated in TUCoD, so females should be included in future studies for more valid and stronger results.
Acknowledgment
The authors would like to thank all dentists, dental assistants, receptionists of the Oral and Maxillofacial, and the Restorative Units of College of Dentistry, Taibah University, Al Madinah Al Munawarah, Kingdom of Saudi Arabia for their help and advice.
Footnotes
Ethical Consent.
All manuscripts reporting the results of experimental investigations involving human subjects should include a statement confirming that informed consent was obtained from each subject or subject’s guardian, after receiving approval of the experimental protocol by a local human ethics committee, or institutional review board. When reporting experiments on animals, authors should indicate whether the institutional and national guide for the care and use of laboratory animals was followed.
References
- 1.Gazal G. Comparison of speed of action and injection discomfort of 4% articaine and 2% mepivacaine for pulpal anesthesia in mandibular teeth: A randomized, double-blind cross-over trial. Eur J Dent. 2015;9:201–206. doi: 10.4103/1305-7456.156811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goodwin M, Pretty IA. Estimating the need for dental sedation. 3. Analysis of factors contributing to non-attendance for dental treatment in the general population, across 12 English primary care trusts. Br Dent J. 2011;211:599–603. doi: 10.1038/sj.bdj.2011.1053. [DOI] [PubMed] [Google Scholar]
- 3.Wilson TD, McNeil DW, Kyle BN, Weaver BD, Graves RW. Effects of conscious sedation on patient recall of anxiety and pain after oral surgery. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;117:277–282. doi: 10.1016/j.oooo.2013.11.489. [DOI] [PubMed] [Google Scholar]
- 4.Spindler H, Staugaard SR, Nicolaisen C, Poulsen R. A. randomized controlled trial of the effect of a brief cognitive-behavioral intervention on dental fear. J Public Health Dent. 2015;75:64–73. doi: 10.1111/jphd.12074. [DOI] [PubMed] [Google Scholar]
- 5.Muschik S, Kallow J. The impact of dental phobia on patient consent. Br Dent J. 2015;219:183–185. doi: 10.1038/sj.bdj.2015.648. [DOI] [PubMed] [Google Scholar]
- 6.Yu C, Li S, Deng F, Yao Y, Qian L. Comparison of dexmedetomidine/fentanyl with midazolam/fentanyl combination for sedation and analgesia during tooth extraction. Int J Oral Maxillofac Surg. 2014;43:1148–1153. doi: 10.1016/j.ijom.2014.03.019. [DOI] [PubMed] [Google Scholar]
- 7.Banerjee P, Rogers BA. Systematic review of high-volume multimodal wound infiltration in total knee arthroplasty. Orthopedics. 2014;37:403–412. doi: 10.3928/01477447-20140528-07. [DOI] [PubMed] [Google Scholar]
- 8.Calvey TN, Williams NE. Principles and Practice of Pharmacology for Anaesthesia. 3rd ed. Oxford (UK): Blackwell Science; 1997. pp. 284–312. [Google Scholar]
- 9.Hersh EV, Ciancio SG, Kuperstein AS, Stoopler ET, Moore PA, Boynes SG, et al. An evaluation of 10 percent and 20 percent benzocaine gels in patients with acute toothaches: efficacy, tolerability and compliance with label dose administration directions. J Am Dent Assoc. 2013;144:517–526. doi: 10.14219/jada.archive.2013.0154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gazal G, Mackie IC. A comparison of paracetamol, ibuprofen or their combination for pain relief following extractions in children under general anaesthesia: a randomized controlled trial. Int J Paediatr Dent. 2007;17:169–177. doi: 10.1111/j.1365-263X.2006.00806.x. [DOI] [PubMed] [Google Scholar]
- 11.Gazal G, Fareed WM, Zafar MS, Al-Samadani KH. Pain and anxiety management for pediatric dental procedures using various combinations of sedative drugs: A review. Saudi Pharmaceutical Journal. 2014 doi: 10.1016/j.jsps.2014.04.004. [Published online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gazal G, Fareed WM, Zafar MS. Effectiveness of gaseous and intravenous inductions on children’s anxiety and distress during extraction of teeth under general anesthesia. Saudi J Anaesth. 2015;9:33–36. doi: 10.4103/1658-354X.146282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Frencken JE, Flohil KA, de Baat C. [Atraumatic restorative treatment in relation to pain, discomfort and dental treatment anxiety] Ned Tijdschr Tandheelkd. 2014;121:388–393. Dutch. [PubMed] [Google Scholar]
- 14.Yesilyurt C, Bulut G, Taşdemir T. Pain perception during inferior alveolar injection administered with the Wand or conventional syringe. Br Dent J. 2008;205:E10. doi: 10.1038/sj.bdj.2008.757. [DOI] [PubMed] [Google Scholar]
- 15.Armfield JM. The extent and nature of dental fear and phobia in Australia. Aust Dent J. 2010;55:368–377. doi: 10.1111/j.1834-7819.2010.01256.x. [DOI] [PubMed] [Google Scholar]
- 16.Al-Melh MA, Andersson L. Reducing pain from palatal needle stick by topical anesthetics: a comparative study between two lidocaine/prilocaine substances. J Clin Dent. 2008;19:43–47. [PubMed] [Google Scholar]
- 17.Franz-Montan M, Silva AL, Cogo K, Bergamaschi C, Volpato MC, Ranali J, et al. Efficacy of 1% ropivacaine gel for topical anesthesia of human oral mucosa. Quintessence Int. 2007;38:601–606. [PubMed] [Google Scholar]
- 18.Hodosh M, Hodosh SH, Hodosh AJ. KNO3/benzocaine/tetracaine gel use for maintenance visit pain control. Gen Dent. 2007;55:312–315. [PubMed] [Google Scholar]
- 19.Whitlow PG, Saboda K, Roe DJ, Bazzell S, Wilson C. Topical analgesia treats pain and decreases propofol use during lumbar punctures in a randomized pediatric leukemia trial. Pediatr Blood Cancer. 2015;62:85–90. doi: 10.1002/pbc.25236. [DOI] [PubMed] [Google Scholar]
- 20.Wiswall AT, Bowles WR, Lunos S, McClanahan SB, Harris S. Palatal anesthesia: comparison of four techniques for decreasing injection discomfort. Northwest Dent. 2014;93:25–29. [PubMed] [Google Scholar]
- 21.Tellez M, Kinner DG, Heimberg RG, Lim S, Ismail AI. Prevalence and correlates of dental anxiety in patients seeking dental care. Community Dent Oral Epidemiol. 2015;43:135–142. doi: 10.1111/cdoe.12132. [DOI] [PubMed] [Google Scholar]
- 22.Armfield JM, Ketting M. Predictors of dental avoidance among Australian adults with different levels of dental anxiety. Health Psychol. 2015;34:929–940. doi: 10.1037/hea0000186. [DOI] [PubMed] [Google Scholar]
- 23.Gazal G, Alharbi AM, Al-samadani KH, Kanaa MD. Articaine and mepivacaine buccal infiltration in securing mandibular first molar pulp anesthesia following mepivacaine inferior alveolar nerve block: A randomized, double-blind crossover study. Saudi Journal of Anaesthesia. 2015;9:397–403. doi: 10.4103/1658-354X.159463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kandreli MG, Vadachkoriia NR, Gumberidze NSh, Mandzhavidze NA. [Pain management in dentistry] Georgian Med News. 2013;(225):44–49. Russian. [PubMed] [Google Scholar]


