Abstract
Recent advancements in virtual reality graphics and models have allowed virtual reality simulators to be incorporated into a variety of endoscopic training programmes. Use of virtual reality simulators in training programmes is thought to improve skill acquisition amongst trainees which is reflected in improved patient comfort and safety. Several studies have already been carried out to ascertain the impact that usage of virtual reality simulators may have upon trainee learning curves and how this may translate to patient comfort. This article reviews the available literature in this area of medical education which is particularly relevant to all parties involved in endoscopy training and curriculum development. Assessment of the available evidence for an optimal exposure time with virtual reality simulators and the long-term benefits of their use are also discussed.
Keywords: Virtual reality, Colonoscopy, Sigmoidoscopy, Endoscopy, Endoscopic ultrasound, Medical education, Endoscopic retrograde cholangio-pancreatography, Gastroscopy, Simulation
Core tip: There is good evidence for the use of virtual reality simulation in endoscopy training programmes, with most benefit seen amongst novice trainees. More research is needed concerning the best integration of simulators within a training programme and the optimal exposure needed. Findings are limited by the variety of simulators used and limited power of the studies. More evidence is also needed to support the benefits virtual reality simulators may have within endoscopic ultrasound and endoscopic retrograde cholangio-pancreatography training programmes.
INTRODUCTION
Endoscopy training and skill acquisition conventionally involves observation and feedback on a trainee’s performance under the supervision of an experienced endoscopist. This applies to traditional training in a variety of procedures, including oesophagogastroduodenoscopy (OGD), endoscopic retrograde cholangio-pancreatography (ERCP), endoscopic ultrasound (EUS) and colonoscopy. More recently, a variety of alternative educational tools have become available that aim to improve trainees’ endoscopy skills.
Virtual reality (VR) simulators are an educational modality that has been purposely developed to facilitate endoscopy training in a controlled environment. With improving graphics and technology, medical simulation has advanced from basic mechanical models or animal models to screen-based simulators. Their use and incorporation into endoscopy training curricula has been thought to enhance the speed of trainee skill acquisition, thus improving patients’ comfort and safety during candidates’ initial phase of learning[1].
This review article aims to evaluate existing evidence on the role of VR simulation in endoscopy training, identify if there is an evidence-based educationally optimal method of incorporating such simulators within endoscopy training programmes and to review the impact that VR simulator training may have upon patient comfort. This article will focus on the impact of virtual reality simulator training for the most common endoscopy modalities, namely OGD, ERCP, EUS and colonoscopy.
LITERATURE STUDY
An extensive bibliographical search was performed via the online databases MEDLINE and EMBASE using the following keywords: Simulation, simulator, virtual reality, endoscopy, gastroscopy, OGD, colonoscopy, sigmoidoscopy, endoscopic retrograde cholangio-pancreatography, ERCP, endoscopic ultrasound, EUS. Some of these terms (simulation, simulator, virtual reality), which were relating to simulation, were searched in combination with the remaining keywords, which were relating to endoscopy (e.g., “simulation and endoscopy”, “simulation and colonoscopy”, “virtual reality and gastroscopy”, etc.), in order to identify all relevant papers investigating the role of virtual reality simulation in endoscopy training. The results were combined before duplicates were removed and the reference lists from the selected studies were manually examined to identify further relevant reports.
All primary research papers published in full from any year of publication were considered for inclusion in this review, regardless of their design. These papers included internationally conducted studies, but only those written or translated into English were included in the full text assessment. The participants of studies considered in this review ranged from physicians, nurses and medical students and the individuals’ endoscopy experience was not taken into account in screening for studies. The intervention sought was that of VR endoscopy against traditional patient-based training methods or where there was no comparison at all.
Screening of these results removed papers which did not have an educational impact focus, as well as discussion papers, in which the title and abstract aimed to legitimise VR simulators (in comparison to traditional training) solely by expert opinion. Papers that included non-VR educational simulators which involved ex-vivo parts or mechanical models were also excluded. This demonstrated that a subset of 24 articles were relevant for this review (Figure 1).
Figure 1.
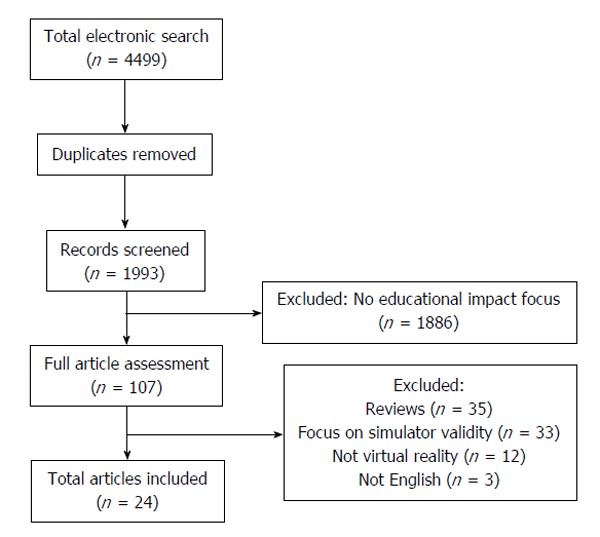
Article screening and selection process.
RESULTS
Role of VR simulation in OGD training
Table 1 shows the methodology of the eight studies that were included.
Table 1.
Summary of analysed oesophagogastroduodenoscopy studies and their design
| Ref. | No. of participants | Participants' level of training | Design | Task | Model | Primary outcome | Secondary outcomes |
| Bloom et al[6] | 35 | Novice and advanced | NRSIS | Visualisation | 5 DT gastroscope training simulator | Time to complete procedure1 | Wall visualisation1 |
| Questionnaire | Questionnaire responses | ||||||
| Clark et al[2] | 13 | Novice and advanced | NRSIS | Completion of monthly assignments over two years on simulator | GI Mentor I | Objective criteria measured by simulator1 | |
| Di Giulio et al[4] | 22 | Novice | MC RCT | Complete simulator or control training programme | GI Mentor I | Competency scores2 | Instructor assessed2 |
| Ferlitsch et al[7] | 13 | Mixed novice and advanced | RCT | Comparison of novice and expert performance in simulated endoscopy. Comparison of performance of simulation-trained and control group of novices | GI Mentor I | Competency scores from simulator1 | |
| Ferlitsch et al[3] | 28 | Novice | RCT | Training on simulator against traditional training | GI Mentor I | Competency scores from expert after 10 and 60 endoscopic examinations2 | Pain experienced by patient |
| Sedlack[9] | 8 | Novice | RCT | 6 h simulation training before 1 mo of traditional training | GI Mentor II | Mixed competency scores from expert2 | |
| Shirai et al[5] | 20 | Novice | RCT | 5 h simulation training before 2 assessed endoscopies | GI Mentor II | Mixed competency scores from expert2 | |
| Van Sickle et al[8] | 41 | Mixed novice and advanced | MC NRSIS | Baseline assessment on simulator and after 8 wk of training | GI Mentor II | Competency scores from expert1 |
Simulator-related outcome;
Patient-related outcome. MC: Multicentre; RCT: Randomised control trail; NRSIS: Non-randomised single-intervention study; GI: Gastro-intestinal; DT: Dimension technologies.
Regarding the role of VR simulators in OGD training the available evidence demonstrates that screen-based simulators have a useful role in facilitating training of novice candidates in OGD[2-7], and potentially a place in the continued professional development of more experienced trainees[2,6,8].
Multiple studies have shown that novice trainees who underwent training that included a VR simulator had significantly better performance outcomes than candidates who were traditionally trained in OGD[3-5,7] and Table 2 summarises the various outcomes of studies investigating the role of VR simulation in OGD training. Ferlitsch et al[7] furthered support for early use of the VR simulators by showing that there was a continued significant difference in VR simulator-trained candidates’ timing, diagnostic and technical accuracy at 60 d. The only study to report a negative outcome comparing simulator training against traditional training stated that the incidence of pain was reported as higher amongst those who used the simulator[9].
Table 2.
Results of studies evaluating the role of simulation in oesophagogastroduodenoscopy training
| Ref. | Primary outcome | Secondary outcome |
| Bloom et al[6] | Mean time to complete procedure was 224 ± 27.65 s for novice, 171.22 ± 25.43 s for intermediate and 106.40 ± 13.08 s for experienced candidates (P = 0.008) | Mean percentage of total surface visualised was 60.56 ± 2.56 for novice, 66.56 ± 2.80 for intermediate and 72.10 ± 0.23 for experienced candidates (P = 0.005) |
| The study demonstrated the construct validity of the simulator | Questionnaire responses suggested that novice and intermediate candidates considered VR simulation an important training tool | |
| Clark et al[2] | Efficiency scores (total time to complete procedure divided by percentage of mucosal surface examined) of senior residents were higher than those of junior residents (85% vs 59%) demonstrating improved efficiency with continued use of simulator | |
| Di Giulio et al[4] | The simulator-trained group performed a higher number of complete procedures (87.8% vs 70%, P < 0.0001) and needed less assistance (41.3% vs 97.9%, P < 0.0001) compared to control group. Length of procedure was similar in the two groups | Instructor marked performance as positive more frequently in the simulator-trained group compared to the controls (86.8% vs 56.7%, < 0.0001) |
| Ferlitsch et al[7] | Performance of expert candidates (compared to novices) was better in performance of J-manoeuvre during oesophagogastroduodenoscopy (P < 0.005), complications at colonoscopy (P < 0.02), insertion time (P < 0.001), identification of abnormal findings in gastroscopy and colonoscopy (P < 0.02) and skill performance (P < 0.01). Amongst novices, the simulation-trained group had a better performance compared to the controls in relation to complication rates at virtual endoscopy (P < 0.04), the insertion time during colonoscopy (P < 0.03) and skill performance (P < 0.01) | |
| Ferlitsch et al[3] | The simulation-trained group performed better than the control group in terms of time needed to reach the duodenum [239 s (range 50-620) vs 310 s (110-720), P < 0.0001] and technical ability (P < 0.02) in the first ten endoscopic examinations on patients. Diagnostic ability was similar in the two groups | There were no significant differences in pain scores between the groups after 10 and after 60 endoscopies |
| After 60 endoscopic examinations, investigation time was still less in the simulation-trained group. Technical and diagnostic ability improved during on-patient training in both groups and differences between groups were no longer seen at that stage | ||
| Sedlack[9] | The control group performed better than the simulation-trained group in terms of patient discomfort (5; IQR, 4-6 vs 6; IQR, 5-6; P = 0.015), sedation, independence and competence scores | |
| Shirai et al[5] | The simulator-trained group achieved significantly higher scores than the control group in the following skills: oesophageal intubation, passing from the EGJ to the antrum, pyloric intubation, and examination of the duodenum and the fundus | |
| Van Sickle et al[8] | The study group showed an improvement in endoscopic skills (e.g., Global Assessment of Gastrointestinal Endoscopic Skills scores) after 8 wk of VR simulation training |
IQR: Interquartile range; EGJ: Esophagogastric junction; VR: Virtual reality.
Another study showed that a significant proportion of trainees who utilised VR simulators felt that simulator practice would be most useful in early training, with those who were more advanced reporting that some of the modules were not very realistic for their stage of training[6].
Role of VR simulation in ERCP training
Although there have been several studies looking into the role of simulation in ERCP training, the majority of these have used mechanical models and only one has focused on the role of VR simulation. This study enrolled novice and expert endoscopists and aimed to determine the construct and face validity of the simulator. It concluded that the GI Mentor II simulator was both realistic and able to differentiate novices and experts based on their performance. In addition, most participants considered it a helpful training tool[10]. Table 3 provides a summary of the design and outcomes of this study.
Table 3.
Summary of analysed endoscopic retrograde cholangio-pancreatography study and its design
| Ref. | No. of participants | Participants' level of training | Design | Task | Model | Primary outcome | Secondary outcomes |
| Bittner et al[10] | 12 | Mixed | NRSIS | 2 simulator ERCP cases | GI Mentor II | Time to complete procedure1 | Time to papilla1 |
| Questionnaire on views |
Simulator-related outcome. NRSIS: Non-randomised single-intervention study; ERCP: Endoscopic retrograde cholangio-pancreatography; GI: Gastro-intestinal.
Role of VR simulation in EUS training
Only one study could be found that discusses the role of VR simulation in EUS training[11]. Eight experts compared an EUS VR simulator (EUS Mentor) to an animal model, a phantom (EUS FNA box) and a combination model and ranked them by realism, utility as an educational modality, ease of use and ease of incorporation into a training programme. They determined the phantom model to be easiest to use and incorporate into training, whereas animal models were marked as best for realism and utility as an educational tool[11].
Role of VR simulation in colonoscopy training
Table 4 shows the methodology of the thirteen studies that were included.
Table 4.
Summary of analysed colonoscopy studies and their design
| Ref. | No. of participants | Participants' level of training | Design | Task | Model | Primary outcome | Secondary outcomes |
| Aabakken et al[12] | 33 | Mixed | NRSIS | 1 simulated colonoscopy and questionnaire | GI Mentor | User satisfaction1 | |
| Ahlberg et al[13] | 12 | Novice3 | RCT | Completion of simulator or control training programme followed by assessment on 10 colonoscopic procedures | AccuTouch | Mixed competency scores2 | Time to caecum2 |
| Buzink et al[14] | 35 | Mixed | NRSIS | 4 training sessions | GI Mentor II | Mixed competency scores1 | |
| Cohen et al[15] | 45 | Novice | MC RCT | Completion of simulator or control training programme followed by assessment of first 200 colonoscopies | GI Mentor I | Mixed competency scores2 | Long term impact2 |
| Eversbusch et al[22] | 28 | Novice3 | RCT | 10 consecutive assessments on VR simulator | GI Mentor II | Mixed competency scores1 | |
| Gerson et al[24] | 16 | Novice | RCT | Completion of simulator or control training programme followed by assessment on 5 endoscopic procedures | AccuTouch | Mixed competency scores2 | |
| Haycock et al[16] | 36 | Novice | RCT | Completion of simulator or control training programme followed by simulator and patient-based assessment | Olympus Endo TS-1 | Mixed competency scores1,2 | |
| Kruglikova et al[21] | 30 | Mixed | NRSIS | 10 repetitions of one VR simulator task | AccuTouch | Mixed competency scores1 | |
| Park et al[17] | 24 | Novice | RCT | Completion of simulator or control training programme followed by assessment on one patient-based colonoscopy | AccuTouch | Mixed competency scores2 | |
| Sedlack et al[18] | 8 | Novice3 | RCT | Completion of simulator or control training programme followed by assessment of one endoscopic procedure | AccuTouch | Mixed competency scores2 | Patient discomfort2 |
| Sugden et al[23] | 50 | Mixed | NRSIS | Completion of modules on the VR simulator | Olympus Endo TS-1 | Mixed competency scores1 | |
| Thomas-Gibson et al[19] | 21 | Novice | NRSIS | Completion of 5 d training programme including VR simulation, with pre- and post-training assessments followed by a 9-mo follow-up assessment | AccuTouch | Mixed competency scores1,2 | Long term outcome (9 mo)1,2 |
| Thomson et al[20] | 13 | Novice | NRSIS | Completion of respective training with or without simulator use with assessments during that period | GI Mentor | Mixed competency scores2 |
Simulator-related outcome;
Patient-related outcome;
Subjects had previous oesophagogastroduodenoscopy training and knowledge. MC: Multicentre; RCT: Randomised control trail; NRSIS: Non-randomised single-intervention study; VR: Virtual reality; GI: Gastro-intestinal.
In assessing the role of VR simulators in colonoscopy training there is more evidence to support its use in training programmes[12-21]. In one survey, 91% of all participating candidates agreed that VR simulators would be useful in their training[12]. Several studies demonstrated that when VR simulator training was compared to traditional colonoscopy training alone, competency parameters were significantly greater amongst simulator trained candidates[13,15-18,20]. The majority of these studies adopted the same methodology, utilising the VR simulator model before candidates started traditional training, which supports the use of VR simulators in this way.
Some studies attempted to determine the amount of exposure with the simulator which is necessary to acquire an “expert” skill base - determined when learning curves plateaued on the simulator modules. While one study reported that the learning curve of novice candidates plateaued on the seventh consecutive attempt[22], another stated that learning curves consistently plateaued at or after the ninth attempt amongst novice candidates[23]. In a separate study which compared learning curves between novice residents and nurses with varying experience in endoscopy the learning curve did not plateau in any group by the tenth attempt[21].
In addition, several studies evaluated the effect of VR simulation training on patient discomfort. Most studies found that this was less during the procedure in simulator trained candidates[13,14,18], but few concluded that there was no significant difference between the two groups[15,24].
Better evidence that simulator training has effective translational skills can be identified by the long-term impact that simulator training has on a candidate’s skill base. It has been shown that a simulator trained candidate retains a significant advantage in competence during their first 100 colonoscopies[15] and that these skills are maintained 9 mo after the simulator intervention[19].
Such concordance advocates strong support for the use of simulators in endoscopy training. However, it is important to note the findings in Gerson et al[24] which is the only reported study to find that simulator-based training was inferior to traditional teaching methods. It concluded that simulator candidates had significantly greater difficulty with insertion of the endoscope, a lower ability to reach the splenic flexure and a lower ability for accurate retroflexion, but these findings were not replicated in other studies.
DISCUSSION
This review evaluated the evidence on the use of VR simulation endoscopy training in order to determine its role within modern educational programmes. The skill base acquired during VR simulation-supported training seems to translate into useable skills for patient-based endoscopy. In addition, learning is facilitated and skills acquisition is more effective compared to training with traditional methods alone. This applies to training in OGD (where the evidence was strongest in those who had least experience in OGD), colonoscopy and ERCP despite the small volume of literature available on this topic. There is no strong evidence for the impact of EUS VR simulator use in novice candidates when compared to traditionally trained candidates.
Integration of VR simulation in endoscopy training curricula
Our literature review did not reveal a single optimal method of integrating VR simulator use in endoscopy training programmes. This is in part due to the variety of exposures candidates had with VR simulators within each study. Whilst the majority of studies controlled candidates to a one-time formal exposure with the VR simulator[2-5,14] others allowed unlimited access[8] or optional extra-access[7,15]. The timing of this controlled exposure also varied with some being integrated within a structured training programme[14] and some randomly during a participant’s training. Despite the varied integration within the education programme, study findings were in support of VR simulator use, but further research is needed to show which approach is most effective. The main issue with the available studies is that there are significant differences in their design, in terms of sample size, candidates’ prior endoscopic experience, tasks included (e.g., some studies included therapeutic interventions or biopsies of specific lesions as additional tasks[2,6]), training time span, type of training (e.g., some studies included hard-eye co-ordination modules, such as Endobubble/Endobasket, as well as virtual endoscopies[7,14], whereas other studies included virtual endoscopies alone[13]). These differences make comparisons between studies difficult, but there was general agreement in the literature that VR simulation training was effective in improving trainees’ endoscopic skills. Therefore, despite differences in the specific interventions and differences in the endpoints of the various studies, the fact that there was an overall trend suggesting an improvement in skill level was sufficient in this review and suggests that institutions can flexibly integrate VR simulation in their endoscopy training curricula.
Optimal exposure to VR simulation
Debate still exists about the optimal exposure time needed with the VR simulator, as this was not apparent within this review. Even within those studies that controlled the exposure within a formalised teaching setting, the time which candidates had with the VR simulator varied from 5-10 h[3,5,7,22], whilst only one study stated that 20 h of exposure was needed on average to reach an expert criteria within colonoscopy[13]. However, its findings were not supported by others and more research is needed to determine the length of exposure needed with the VR simulator. There may be several explanations for the differences in the length of exposure required to achieve an improvement in performance, such as differences in the level of experience of participants, differences in simulator types, differences in the tasks (e.g., some studies included therapeutic interventions or biopsies of specific lesions as additional tasks[2,6]) and collateral learning (e.g., some studies included bedside teaching, educational videos or didactic modules, in addition to VR simulation practice as the main intervention[5,6,24]).
Long-term benefits of VR simulation
Whilst there was some evidence of the long-term benefits of VR simulator use when compared to traditional methods alone[3], the significance of long-term or continued training and the effect on outcomes remains unknown.
Effects of VR simulation on patient comfort
When looking at the reported discomfort or pain, only four studies found that VR simulator training reduced patients’ pain significantly[13,16,18,22]. Another four studies found no significant difference between VR simulator trained and traditionally trained candidates[3,15,21,24] and only one found that patients of the VR simulator trained group reported significantly more pain[25]. More evidence is needed to show the true impact that VR simulator training has on patients’ reported levels of discomfort.
LIMITATIONS
There are several issues relating to the consistency of the methodology of these studies that limits the comparison and generalisability of their findings. When looking at the studies reviewed, ten of the included studies were single-group intervention studies[2,6,8,10,12,14,19-21,23] without control groups and there were very few larger randomised control trials[15,16] (more than 30 participants). This is impacted further by the variety of different VR simulator models used, as the ability to draw accurate comparisons remains difficult.
Because of the different VR simulator models used, it is hard to accurately compare the mixed competencies used to measure candidates’ skills, as measurements made in different simulator models are not truly identical. Recognition of the overall trend suggesting an improvement or reduction in skill level was sufficient in this review, negating the technicalities of the different measures.
Despite the overall trend advocating the use of VR simulators, the power of these findings is also limited by the relatively small study size. Also, as mentioned in the discussion, not all studies actively used VR simulators as part of a structured training programme and it is difficult to assess the impact of each different approach.
Finally, one limitation across all these studies was the varied definition of who was a “novice” or “experienced” candidate and the selection criteria. It was not always clear in the selection criteria how one was defined as being novice, with some studies defining a novice candidate as having no prior endoscopy experience, some as having limited experience in the procedure, whilst others allowed candidates trained in other endoscopy modalities, providing it was not the one under investigation[13,18,21]. For example, having completed less than 200 colonoscopies was defined as being a novice candidate in one study[12] whilst in the majority of studies a novice candidate had to have done no prior colonoscopies. Other studies only excluded those who had prior simulator experience[6,8]. Similarly, there were no uniform criteria among different studies regarding the definition of advanced or expert level. For example, in some studies having done more than 1000 procedures was defined as being an expert[7,13], whereas in other studies having done more than 500 procedures[8,12] or more than 30 procedures in the past 5 years[6] were considered sufficient thresholds for entering the “advanced” group. Clearly using an arbitrary number of previous endoscopies to stratify a candidate’s ability and not standardising a candidate’s background experience may impact on the conclusions made in these studies.
CONCLUSION
Given the limitations of the studies, there is consistent evidence advocating the use of VR simulation in endoscopy teaching, stronger still in those who are least experienced. More evidence is needed to strengthen support of VR simulators in ERCP, as many of the models that currently exist to support this field of teaching rely on ex-vivo simulators not included in this review. For EUS training, more research is needed into the impact that VR simulators may have.
However, there does not appear to be a clear model in how best to integrate simulators in an educational programme. This is due to the variety of simulator models used and the lack of agreement over the length of exposure needed with any one simulator to obtain a beneficial outcome. A combined curriculum of traditional teaching supplemented with virtual reality simulators is of greater benefit than one without virtual reality simulation. Other considerations, such as the cost-benefit-analysis, although not considered here, would also influence decisions about how best to integrate VR simulators into any endoscopy curriculum.
Footnotes
P- Reviewer: de Lange T S- Editor: Tian YL L- Editor: A E- Editor: Liu SQ
Conflict-of-interest statement: None declared.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: June 11, 2015
First decision: July 29, 2015
Article in press: October 27, 2015
References
- 1.Cunningham M, Fernando B, Berlingieri P. The emerging role of screen based simulators in the training and assessment of colonoscopists. Frontline Gastroenterol. 2010;1:76–81. doi: 10.1136/fg.2009.000430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Clark JA, Volchok JA, Hazey JW, Sadighi PJ, Fanelli RD. Initial experience using an endoscopic simulator to train surgical residents in flexible endoscopy in a community medical center residency program. Curr Surg. 2005;62:59–63. doi: 10.1016/j.cursur.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 3.Ferlitsch A, Schoefl R, Puespoek A, Miehsler W, Schoeniger-Hekele M, Hofer H, Gangl A, Homoncik M. Effect of virtual endoscopy simulator training on performance of upper gastrointestinal endoscopy in patients: a randomized controlled trial. Endoscopy. 2010;42:1049–1056. doi: 10.1055/s-0030-1255818. [DOI] [PubMed] [Google Scholar]
- 4.Di Giulio E, Fregonese D, Casetti T, Cestari R, Chilovi F, D’Ambra G, Di Matteo G, Ficano L, Delle Fave G. Training with a computer-based simulator achieves basic manual skills required for upper endoscopy: a randomized controlled trial. Gastrointest Endosc. 2004;60:196–200. doi: 10.1016/s0016-5107(04)01566-4. [DOI] [PubMed] [Google Scholar]
- 5.Shirai Y, Yoshida T, Shiraishi R, Okamoto T, Nakamura H, Harada T, Nishikawa J, Sakaida I. Prospective randomized study on the use of a computer-based endoscopic simulator for training in esophagogastroduodenoscopy. J Gastroenterol Hepatol. 2008;23:1046–1050. doi: 10.1111/j.1440-1746.2008.05457.x. [DOI] [PubMed] [Google Scholar]
- 6.Bloom MB, Rawn CL, Salzberg AD, Krummel TM. Virtual reality applied to procedural testing: the next era. Ann Surg. 2003;237:442–448. doi: 10.1097/01.SLA.0000055279.50681.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ferlitsch A, Glauninger P, Gupper A, Schillinger M, Haefner M, Gangl A, Schoefl R. Evaluation of a virtual endoscopy simulator for training in gastrointestinal endoscopy. Endoscopy. 2002;34:698–702. doi: 10.1055/s-2002-33456. [DOI] [PubMed] [Google Scholar]
- 8.Van Sickle KR, Buck L, Willis R, Mangram A, Truitt MS, Shabahang M, Thomas S, Trombetta L, Dunkin B, Scott D. A multicenter, simulation-based skills training collaborative using shared GI Mentor II systems: results from the Texas Association of Surgical Skills Laboratories (TASSL) flexible endoscopy curriculum. Surg Endosc. 2011;25:2980–2986. doi: 10.1007/s00464-011-1656-7. [DOI] [PubMed] [Google Scholar]
- 9.Sedlack RE. Validation of computer simulation training for esophagogastroduodenoscopy: Pilot study. J Gastroenterol Hepatol. 2007;22:1214–1219. doi: 10.1111/j.1440-1746.2007.04841.x. [DOI] [PubMed] [Google Scholar]
- 10.Bittner JG, Mellinger JD, Imam T, Schade RR, Macfadyen BV. Face and construct validity of a computer-based virtual reality simulator for ERCP. Gastrointest Endosc. 2010;71:357–364. doi: 10.1016/j.gie.2009.08.033. [DOI] [PubMed] [Google Scholar]
- 11.Matsuda K, Hawes RH, Sahai AV, Tajiri H. The role of simulators, models, phantoms. Where’s the evidence? Endoscopy. 2006;38 Suppl 1:S61–S64. doi: 10.1055/s-2006-946656. [DOI] [PubMed] [Google Scholar]
- 12.Aabakken L, Adamsen S, Kruse A. Performance of a colonoscopy simulator: experience from a hands-on endoscopy course. Endoscopy. 2000;32:911–913. doi: 10.1055/s-2000-8092. [DOI] [PubMed] [Google Scholar]
- 13.Ahlberg G, Hultcrantz R, Jaramillo E, Lindblom A, Arvidsson D. Virtual reality colonoscopy simulation: a compulsory practice for the future colonoscopist? Endoscopy. 2005;37:1198–1204. doi: 10.1055/s-2005-921049. [DOI] [PubMed] [Google Scholar]
- 14.Buzink SN, Koch AD, Heemskerk J, Botden SM, Goossens RH, de Ridder H, Schoon EJ, Jakimowicz JJ. Acquiring basic endoscopy skills by training on the GI Mentor II. Surg Endosc. 2007;21:1996–2003. doi: 10.1007/s00464-007-9297-6. [DOI] [PubMed] [Google Scholar]
- 15.Cohen J, Cohen SA, Vora KC, Xue X, Burdick JS, Bank S, Bini EJ, Bodenheimer H, Cerulli M, Gerdes H, et al. Multicenter, randomized, controlled trial of virtual-reality simulator training in acquisition of competency in colonoscopy. Gastrointest Endosc. 2006;64:361–368. doi: 10.1016/j.gie.2005.11.062. [DOI] [PubMed] [Google Scholar]
- 16.Haycock A, Koch AD, Familiari P, van Delft F, Dekker E, Petruzziello L, Haringsma J, Thomas-Gibson S. Training and transfer of colonoscopy skills: a multinational, randomized, blinded, controlled trial of simulator versus bedside training. Gastrointest Endosc. 2010;71:298–307. doi: 10.1016/j.gie.2009.07.017. [DOI] [PubMed] [Google Scholar]
- 17.Park J, MacRae H, Musselman LJ, Rossos P, Hamstra SJ, Wolman S, Reznick RK. Randomized controlled trial of virtual reality simulator training: transfer to live patients. Am J Surg. 2007;194:205–211. doi: 10.1016/j.amjsurg.2006.11.032. [DOI] [PubMed] [Google Scholar]
- 18.Sedlack RE, Kolars JC. Computer simulator training enhances the competency of gastroenterology fellows at colonoscopy: results of a pilot study. Am J Gastroenterol. 2004;99:33–37. doi: 10.1111/j.1572-0241.2004.04007.x. [DOI] [PubMed] [Google Scholar]
- 19.Thomas-Gibson S, Bassett P, Suzuki N, Brown GJ, Williams CB, Saunders BP. Intensive training over 5 days improves colonoscopy skills long-term. Endoscopy. 2007;39:818–824. doi: 10.1055/s-2007-966763. [DOI] [PubMed] [Google Scholar]
- 20.Thomson M, Heuschkel R, Donaldson N, Murch S, Hinds R. Acquisition of competence in paediatric ileocolonoscopy with virtual endoscopy training. J Pediatr Gastroenterol Nutr. 2006;43:699–701. doi: 10.1097/01.mpg.0000243431.09216.71. [DOI] [PubMed] [Google Scholar]
- 21.Kruglikova I, Grantcharov TP, Drewes AM, Funch-Jensen P. Assessment of early learning curves among nurses and physicians using a high-fidelity virtual-reality colonoscopy simulator. Surg Endosc. 2010;24:366–370. doi: 10.1007/s00464-009-0555-7. [DOI] [PubMed] [Google Scholar]
- 22.Eversbusch A, Grantcharov TP. Learning curves and impact of psychomotor training on performance in simulated colonoscopy: a randomized trial using a virtual reality endoscopy trainer. Surg Endosc. 2004;18:1514–1518. doi: 10.1007/s00464-003-9264-9. [DOI] [PubMed] [Google Scholar]
- 23.Sugden C, Aggarwal R, Banerjee A, Haycock A, Thomas-Gibson S, Williams CB, Darzi A. The development of a virtual reality training curriculum for colonoscopy. Ann Surg. 2012;256:188–192. doi: 10.1097/SLA.0b013e31825b6e9c. [DOI] [PubMed] [Google Scholar]
- 24.Gerson LB, Van Dam J. A prospective randomized trial comparing a virtual reality simulator to bedside teaching for training in sigmoidoscopy. Endoscopy. 2003;35:569–575. doi: 10.1055/s-2003-40243. [DOI] [PubMed] [Google Scholar]
- 25.Sedlack RE, Baron TH, Downing SM, Schwartz AJ. Validation of a colonoscopy simulation model for skills assessment. Am J Gastroenterol. 2007;102:64–74. doi: 10.1111/j.1572-0241.2006.00942.x. [DOI] [PubMed] [Google Scholar]


