Abstract
Paraneoplastic neurological syndromes belong to the most enigmatic and fascinating disorders. Their remarkable clinical spectrum ranges from sensory neuronopathy to cerebellar degeneration or limbic encephalitis. We retrace the clinical and pathological description of a forgotten case published by Hermann Oppenheim in 1888, which to our knowledge represents the first report of a paraneoplastic neurological syndrome. The young Oppenheim used thorough observation and good clinical judgment to suggest a causal link between the seemingly mere association of an underlying malignancy and a neurological syndrome, decades before Denny-Brown’s identification of sensory neuronopathy in 1948 and a century before the discovery of “anti-Hu” antibodies. Oppenheim anticipated that scientific progress was required to prove this link, and he indicated his finding as “a pointer for future observers.” In this way, he leaves the reader with the fascinating question of which observations during our current neurology practice could be the next “pointers” in medical research.
Keywords: paraneoplastic neurological syndrome, Hermann Oppenheim, cancer, encephalitis
Although being rare, paraneoplastic neurological syndromes attract much attention for at least two reasons. First, the distant immunological effects stimulated by the presence of an often undetected tumor represent a challenging and enigmatic disease mechanism. Discovery of antineuronal antibodies has facilitated diagnosis so that patients may be treated earlier and more effectively. Second, the new era of pathogenic antibodies directed against neuronal surfaces has resulted in reclassification of brain diseases that are now known to be autoimmune encephalitides. The best established and most prevalent member of this new group is the encephalitis with NMDAR (N-methyl-D-aspartate receptor) antibodies, frequently occurring in the context of a teratoma. Anti-NMDAR encephalitis is a severe encephalitis with psychiatric features, epileptic seizures, and movement disorders; many of these patients require intensive care unit treatment for hypoventilation and autonomic dysfunction. Despite the disease severity, rapid and sufficiently aggressive immunotherapy results in profound improvement, and most patients can eventually return to school or work.
Historical Background
However, diagnosis and treatment have not always been so clear.
In fact, the categorization and the research on autoimmune-mediated neurologic symptoms, often in combination with a primary cancerous disease, did not start until the 1950s, since it required certain equipment and knowledge to collect evidence. Three contributions are generally cited as seminal papers highlighting the history of the discovery of the paraneoplastic neurological syndrome.
One of them was by Derek Denny-Brown in 1948, who documented two patients suffering from rapidly progressive sensory neuropathy. Autopsy revealed not only severe neuronal loss in the dorsal root ganglia but also a previously unidentified lung cancer. Denny-Brown concluded that the “close similarity of the condition suggests that the coincidence of carcinoma was more than a chance association” (Denny-Brown, 1948). He inferred that “metabolic studies on similar cases in the future are indicated” (1948). Further reports followed, and the term “paraneoplastic” was used by Guichard and Vignon to describe the development of neuropathies in the context of a neoplasm of the uterus (Guichard and Vignon, 1949).
The second important paper was that of Brierley and colleagues in 1960, reporting three adult patients with an inflammatory reaction of the hemispheres of the brain in association with a carcinoma, occasionally cited as the first description of a paraneoplastic neurological syndrome involving the brain (Brierley et al., 1960).
In 1985, Graus et al. presented the discovery of a neuronal antinuclear antibody associated with sensory neuropathy and lung cancer (Graus et al., 1985). Whereas the antigen was still unknown, the following years of research allowed classification of this antibody amongst others. It is well known as “Anti-Hu” mostly occurring in the context of encephalitis and sensory neuropathy, often in presence of small-cell lung cancer, neuroblastoma, or prostate cancer.
Nevertheless, research has not revealed the complete pathogenic mechanisms between the onset of cancer, the development of auto-antibodies, and neuronal inflammation so that it still remains a field of current scientific efforts (Darnell and Posner, 2011).
Perhaps more surprising, it seems that the first documentation of a paraneoplastic neurological syndrome might have already been described a long time before the research around that particular diagnosis had even started.
Over 125 years ago in 1888, the Berlin-based neurologist Hermann Oppenheim (1858–1919) published an interesting case under the descriptive title “Über Hirnsymptome bei Carcinomatose ohne nachweisbare Veränderungen im Gehirn” [On Brain Symptoms Associated with Carcinomatosis without Detectable Changes in the Brain] in the Charité Annalen — an annual collection of clinical cases and observations at the Charité Hospital in Berlin (Oppenheim, 1888; see Fig. 1).
Figure 1.
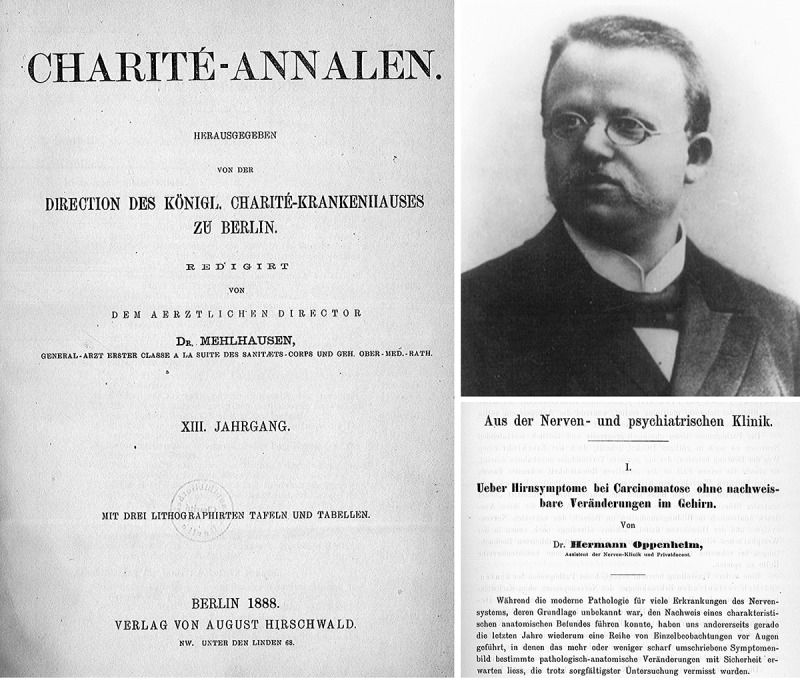
Hermann Oppenheim, the famous neurologist of the late-nineteenth and early-twentieth centuries, published his remarkable case “On Brain Symptoms Associated with Carcinomatosis without Detectable Changes in the Brain” in the 1888 issue of the Charité Annalen, at that time a renowned annual collection of clinical cases and observations at the Charité Hospital in Berlin.
Source: Institut für Geschichte der Medizin, Charité – Universitätsmedizin Berlin.
At that time, Oppenheim, habilitated in 1886, worked as clinical assistant to Carl Friedrich Otto Westphal (who is still known for his many discoveries in the field of neurology, such as the Edinger-Westphal nucleus or the Westphal variant of Huntington’s disease) at the Clinic of Neurology at the Charité Hospital where he had started his academic career only a few years before.
Neurology had just emerged as a clinical discipline in the nineteenth century, with still a broad number of diseases and syndromes not yet identified, so it seemed the ideal field of research for a young and ambitious scientist such as Oppenheim, who spread his attention widely from the impact of syphilis on the nervous system through poliomyelitis, multiple sclerosis even to “neurosis.” The knowledge he gained through his clinical experience and research, Oppenheim later summed up in a textbook about nervous diseases titled Lehrbuch der Nervenkrankheiten für Ärzte und Studierende in 1894, which became one of the most recommended textbooks at his time and was published in multiple languages. Meanwhile, after being denied the head of the Neurology Clinic of Charité Hospital, probably due to his Jewish background, he had just opened his own private outpatient institution (Poliklinik) in Berlin where he successfully spent the remaining years of his career, before he died in 1919.
So taking a look back at his scarcely cited (Darnell and Posner, 2011) and, at that time, rather overlooked publication in 1888, Oppenheim describes the case and its challenging circumstances as follows.
Case Presentation
Oppenheim opens the article with a discussion about the phenomenon of focal neurologic symptoms devoid of any correlating macroscopical or microscopical findings. He presents common hypotheses, such as infectious or toxic processes (see Fig. 2) and discusses their probability only to reference to a case at his clinic where he sees the chance of another possible explanation for the incongruity of symptoms and pathologic findings.
Figure 2.
Pathomechanistic hypotheses for fatal diseases of the nervous system in the absence of anatomical changes, suspecting infectious or toxic causes.
Ernestine Maetschke is her name — a 54-year-old housemaid presenting with various neurologic deficits when she initially arrived in the Charité Clinic of Neurology on the 4th of June in 1887. Her deficits included agnosia, mood changes, and aphasia, leaving the patient unable to answer or to communicate other than in primitive gestures, but also a strong deficit in processing given information. Furthermore, Oppenheim portrays her as fully conscious while looking for help entreatingly with the expression of grief (see Fig. 3). To complete the image, Oppenheim sums up the results of the physical examination that was comprised of cachexia, anemia, dysphagia, a rapid pulse, and a greyish skin color. Relatives reported that the woman complained about nausea, vomiting, and weight loss for several months.
Figure 3.
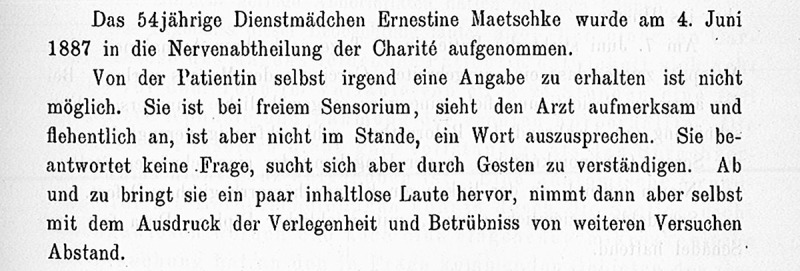
Description of the initial clinical presentation of the index case, the 54-year-old housemaid Ernestine Maetschke.
The patient died a few days later and autopsy revealed a large gastric cancer as sufficient explanation for the patient’s death. Strangely, the neurological symptoms could not be explained through the autopsy since there were no macroscopically visible pathological changes of either the brain or meningeal tissue or the brain vessels.
Subsequently, Oppenheim prepared the brain for histological examination (see Fig. 4), which was at that time still routinely conducted by the treating physician himself, and explored the brain microscopically only to be left surprised again; not even in this closer observation was he able to detect any significant change explaining the patient’s neurologic deficits — no signs of metastasis, of nervous vasopathy, or of any other explanatory pathology (see Fig. 5).
Figure 4.

Microscopic analysis of the brain did not reveal abnormalities.
Figure 5.
Oppenheim states that he has not found similar cases of ‘carcinomatosis’ patients in the literature in whom brain symptoms occurred in the absence of macroscopical and microscopical changes.
Hence, Oppenheim searched for similar cases describing nervous symptoms in conjunction with a cancerous disease, but without anatomical brain findings. Research did not reveal any related descriptions but one other observation made at the Charité Hospital one year earlier in 1887.
At the day of her admission to the Charité Hospital, Ms. Irrgang suffered from a progressive stage of breast cancer with numerous local metastases. Only two weeks later, she suddenly developed jerks in the flexor muscles of the lower leg that transitioned into tonic movements spreading first to the upper leg then also to the right arm as well as her neck and her face, while her pupils were without reaction. This seizure lasted for half a minute and left the patient in a state of unconsciousness. Throughout the following day, seizures recurred several times and eventually the patient died in the evening. The autopsy showed various metastases in the patient’s breasts and thoracic region without any pathological findings in the brain.
With these two cases on the one side and with a lack of publications explaining sufficiently the phenomenon of cancer with distant nervous symptoms on the other side, Oppenheim finally — although very carefully — drew a conclusion: “After acknowledging all moments, the conclusion — whose hypothetical nature I certainly accept — proved to be the most likely, that the toxic focal neurological symptoms of the brain are in fact caused by the presence of a carcinoma” (see Fig. 6; Oppenheim, 1888, p. 342). He further felt it very plausible that “toxic products” can have very focal effects only in specific parts of the brain, as was known already from work on ergotin intoxication.
Figure 6.
Most likely, the toxic focal neurological symptoms of the brain are in fact caused by the presence of a carcinoma.
In the 1888 article, Oppenheim eventually mentioned another case that he remembered from his own experience — a patient suffering from uterine cancer with progressive paralysis of the upper and lower limbs without pathological findings in the spine, spinal cord, or pelvine nerve plexus at autopsy. But being aware of its vague nature, he mentioned that “due to an insufficient microscopical examination this case can only be considered as a valuable pointer, indicating the right direction for future observers” (see Fig. 7; Oppenheim, 1888, p. 344).
Figure 7.
The case was not seen as definite proof, but rather as a valuable pointer, indicating the right direction for future observers.
Discussion
Oppenheim thoroughly documented the cases of three patients suffering from cancer with anatomically distant symptoms in the nervous system, lacking macroscopical and microscopical signs of tumor infiltration or neuronal death in the brain. He concluded that the underlying cancerous disease could cause the neurological symptoms, an idea that modern neurology would call paraneoplastic neurological syndromes (Darnell and Posner, 2011).
Nowadays a diagnostic panel of onconeuronal antibodies would have been ordered that would likely return with positive results. Although gastric cancer rarely causes paraneoplastic neurological syndromes such as encephalomyelitis, it is much clearer in the other two cases. Based on Oppenheim’s descriptions, one patient could have suffered from breast-cancer-associated limbic encephalitis with refractory seizures and reduced levels of consciousness. The other likely had uterus-cancer-associated myelitis with progressive paralysis. Encephalomyelitis, myelitis, and limbic encephalitis all belong to the “classical” paraneoplastic syndromes, and Oppenheim’s patients might have had anti-Ri (ANNA-2) and anti-Yo (PCA-1) antibodies, respectively.
From a current perspective, Oppenheim’s observations and conclusions are remarkable for two reasons. First, his description is a fascinating early documentation of a connection between neurological deficits and an underlying malignancy, strongly suggestive of a paraneoplastic syndrome. Second, he proved far-sightedness by calling his findings “a valuable pointer, indicating the right direction for future observers” (Oppenheim, 1888, p. 344). Oppenheim seemed to know that science someday will reach a point where medical research can go beyond macroscopical as well as microscopical examination — and it has. But still it took another 60 years to move on into this direction (Denny-Brown, 1948), leading to the concept of paraneoplastic syndromes as we know it now in modern clinical practice. In this way, Oppenheim lines up with the many physicians in medical history whose initial observations and anticipations became confirmed with advanced knowledge and scientific progress.
From our position, although we cannot guarantee that Oppenheim’s cases were in fact examples of paraneoplastic neurological symptoms, we conclude that it is very likely. It has been discussed that Oppenheim could have overlooked metastatic tumor (Darnell and Posner, 2011). However, his documented careful microscopic analysis and the presence of a multisystem brain disorder (including aphasia, personality changes, cognitive deficits, hemiparesis) do not support this hypothesis. Furthermore, we cannot exclude that similar reports were made in the nineteenth century. However, Oppenheim was a thorough scientist who failed to find any comparable cases through his research, thus we assume that Oppenheim’s article remains a singularity at that time.
Nonetheless, we strongly acknowledge Oppenheim’s observation as the initial “pointer” into the direction of paraneoplastic research. The fact that Oppenheim carefully documented his cases of the unknown — hereby enabling further progress in this field — should leave us with the question of which current clinical observations could be the next “pointers” in medical research.
ORCID
Harald Prüss

References
- Brierley JB, Corsellis JAN, Hierons R, Nevin S. Subacute encephalitis of later adult life mainly affecting the limbic areas. Brain. 1960;83:357–368. [Google Scholar]
- Darnell RB, Posner JB. Paraneoplastic Syndromes. New York: Oxford University Press; 2011. [Google Scholar]
- Denny-Brown D. Primary sensory neuropathy with muscular changes associated with carcinoma. Journal of Neurology, Neurosurgery and Psychiatry. 1948;11(2):73–87. doi: 10.1136/jnnp.11.2.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graus F, Cordon-Cardo C, Posner JB. Neuronal antinuclear antibody in sensory neuronopathy from lung cancer. Neurology. 1985;35(4):538–543. doi: 10.1212/wnl.35.4.538. [DOI] [PubMed] [Google Scholar]
- Guichard MMA, Vignon G. Le Journal de Médecine de Lyon 30: 1949. La Polyradiculonéurite cancéreuse métastatique; pp. 197–207. [PubMed] [Google Scholar]
- Oppenheim H. Über Hirnsymptome bei Carcinomatose ohne nachweisbare Veränderungen im Gehirn. Charité Annalen. 1888;13:335–344. [Google Scholar]
- Oppenheim H. Berlin, S. Karger. 1894. Lehrbuch der Nervenkrankheiten für Ärzte und Studierende . [Google Scholar]


