Abstract
Background
Non-dependent alcohol and substance use patterns are prevalent among men who have sex with men (MSM), yet few effective interventions to reduce their substance use are available for these men. We evaluated whether an adapted brief counseling intervention aimed at reducing HIV risk behavior was associated with secondary benefits of reducing substance use among episodic substance-using MSM (SUMSM).
Methods
326 episodic SUMSM were randomized to brief Personalized Cognitive Counseling (PCC) intervention with rapid HIV testing or to rapid HIV testing only control. Both arms followed over 6 months. Trends in substance use were examined using GEE Poisson models with robust standard errors by arm. Reductions in frequency of use were examined using ordered logistic regression.
Results
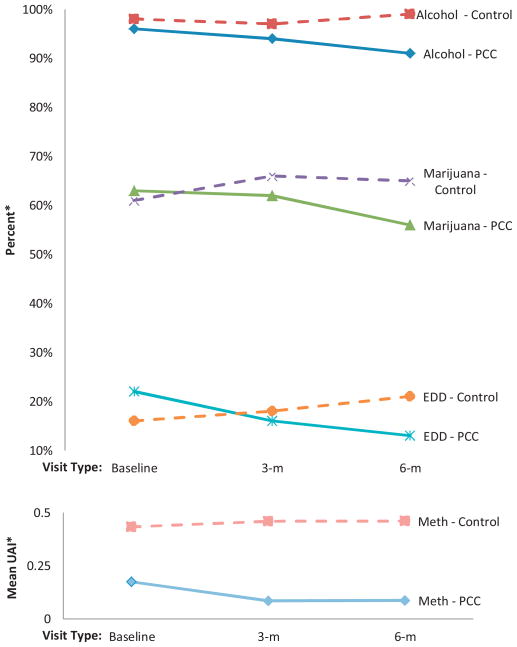
In intent-to-treat analyses, compared to men who received rapid HIV testing only, we found men randomized to PCC with rapid HIV testing were more likely to report abstaining from alcohol consumption (RR = 0.93; 95% CI = 0.89–0.97), marijuana use (RR = 0.84; 95% CI = 0.73–0.98), and erectile dysfunction drug use (EDD; RR = 0.51; 95% CI = 0.33–0.79) over the 6-month follow-up. PCC was also significantly associated with reductions in frequency of alcohol intoxication (OR = 0.58; 95% CI = 0.36–0.90) over follow-up. Furthermore, we found PCC was associated with significant reductions in number of unprotected anal intercourse events while under the influence of methamphetamine (RR = 0.26; 95% CI = 0.08–0.84).
Conclusion
The addition of adapted PCC to rapid HIV testing may have benefits in increasing abstinence from certain classes of substances previously associated with HIV risk, including alcohol and EDD; and reducing alcohol intoxication frequency and high-risk sexual behaviors concurrent with methamphetamine use.
Keywords: MSM, Behavioral interventions, Methamphetamine, Alcohol, Substance use, HIV risk, Risk reduction counseling, Personalized cognitive counseling
1. Introduction
Alcohol and substance use are prevalent among men who have sex with men (MSM). Based on National HIV Behavioral Surveillance (NHBS) data, 42% of MSM used substances recreationally in the past year (Sanchez et al., 2006). Moreover, National Household Survey on Drug Abuse (NHSDA) data show that MSM have higher lifetime prevalence of substance use and higher prevalence of “dysfunctional” use (i.e., having any symptoms of drug dependence) relative to other men in the United States (Cochran et al., 2004). NHBS data also suggest that among MSM, heavy episodic drinking (“binge-drinking”), defined as having five or more drinks on a single occasion, exceed rates reported for the general population (Finlayson et al., 2011; Centers for Disease Control and Prevention, 2012).
It is important to note, however, that most alcohol and/or substance-using MSM (SUMSM) do not meet criteria for dependence (Colfax et al., 2004; Santos et al., 2011); only 5.7% of MSM have drug dependence syndrome in NHSDA (Cochran et al., 2004). Nevertheless, alcohol and/or substance use have important public health implications in their own right: 4.8% of the global burden of disease and 2.9 million deaths attributed to alcohol and drug use in 2010 (Lim et al., 2012). Moreover, use of alcohol/substances are independently associated with HIV-related sexual risk behaviors, as well as HIV seroconversion among MSM (Drumright et al., 2006; Koblin et al., 2006; Ostrow et al., 2009; Sander et al., 2013; Vosburgh et al., 2012). This may be compounded by the limited number of evidence-based behavioral interventions for non-dependent substance users; none of which are efficacious among MSM (Centers for Disease Control and Prevention, 2013). Although brief behavioral interventions, such as motivational interviewing have shown promise in addressing substance and alcohol abuse in the general population (Baker et al., 2001, 2005; Daeppen et al., 2011; Smedslund et al., 2011), efficacy of brief interventions is less compelling among MSM (Colfax et al., 2010; Morgenstern et al., 2009). Given the high prevalence of non-dependent substance use patterns among MSM, there is a great need to develop brief interventions that may be more suitable to this population than traditional intensive treatment programs for abuse/dependence.
We previously reported that the evidence-based Personalized Cognitive Counseling (PCC) intervention (Dilley et al., 2007), adapted for episodic SUMSM (Knight et al., 2013), was associated with significant reductions in number of unprotected anal intercourse (UAI) events with most recent non-primary partners among a subgroup of non-dependent participants (Coffin et al., 2014), compared to rapid HIV testing only. As a secondary data analysis, we sought to evaluate whether PCC added to rapid HIV testing had collateral effects on alcohol/substance use outcomes among episodic SUMSM.
2. Methods
2.1. Study design
This is a secondary data analysis testing the efficacy of PCC in reducing alcohol and substance use outcomes. The study, Project ECHO, was conducted in San Francisco, CA from May, 2010 to May, 2012 (clinicaltrials.gov = NCT01279044; trial ended when target enrollment accrued and planned 6-month follow-up completed). Study procedures were approved by the institutional review board for the University of California, San Francisco.
Study methods have been reported elsewhere (Coffin et al., 2014). Briefly, 326 HIV-negative, SUMSM, ≥18 years old, were randomized 1:1 (using sequentially numbered opaque envelopes from a computer-generated allocation sequence provided by an offsite statistician) by research associates to PCC adapted for SUMSM (Knight et al., 2013) or control, and followed at 3 and 6 month visits. SUMSM were eligible if they reported no more than episodic use (defined as less than weekly use (Colfax et al., 2004)) within two hours before/during sex of one of the following target substances previously identified as drivers of HIV risk among MSM: methamphetamine, cocaine/crack, amyl nitrite (“poppers”), and binge-drinking. Sample size of 326 was determined based on parameters for primary outcomes of the trial (Coffin et al., 2014).
PCC sessions were delivered at baseline, with booster sessions at 3-month visits. PCC involved discussion of participants’ self-justifications (e.g., “Alcohol and/or drugs make it easier to have sex…”) to minimize known risks during a recent UAI event while intoxicated from alcohol/substances. Sessions were tailored to specific substances and UAI events reported. Counselors also explored strategies to avoid future similar high-risk situations (Dilley et al., 2002, 2007). Rapid HIV testing was conducted at all visits.
2.2. Data collection/analysis
Self-reported alcohol/substance use was collected using audio computer-assisted self-interview (ACASI) with a 90-day recall period for all visits. The severity of dependence scale (SDS) for our target substances was also measured (Gossop et al., 1995). Event-level data were collected on substances used within 2 h before/during UAI events (Colfax et al., 2004; Leigh and Stall, 1993). We analyzed between group differences by intention-to-treat, without any regard to adherence to study procedures, but did not impute missing outcomes. We used generalized estimating equations (GEE) models to evaluate group-specific linear trends outcomes across the three study visits, with robust standard errors to account for within-subject correlation as well as potential over-dispersion of count outcomes. Binary and count outcomes were examined using Poisson and negative binomial models, respectively, while ordinal outcomes including SDS, frequency of alcohol intoxication (i.e., being “drunk or buzzed”), and frequency of substance use were assessed using the proportional odds/ordered logistic regression model. In all models, the effect of the intervention was estimated by the interaction between the treatment assignment indicator and a linear term in time. The exponentiated coefficient for interaction in the Poisson and negative binomial models is interpretable as the ratio of the intervention and control rates of change in the mean value of the outcome, or rate-ratio (RR). We checked for imbalances at baseline, departures from linear trends, and violations of the proportional odds assumption. Analyses were conducted with STATA 12.0 (College Station, TX).
3. Results
The study recruited a diverse sample of 326 SUMSM (47% white, 26% Latino/Hispanic, 11% Asian/Pacific Islander, 10% black/African American, and 6% mixed/other race). Mean age was 33.6 years, and 71% attended some/finished college. Participant baseline characteristics in the two arms were similar (see Supplementary Table).
3.1. Alcohol and substance use prevalence
At baseline, the most common substances used were marijuana (61.7%), cocaine (32.5%), ecstasy (22.4%), erectile dysfunction drugs (EDD; 18.7%), prescription drugs (11.3%), and methamphetamine (9.5%). Nearly all participants (96.6%) consumed alcohol. Alcohol and substance use patterns between study arms presented in Table 1. There were 3 and 11 participants lost to follow-up in the control and PCC groups, respectively. In intention-to-treat analysis, 164 control and 162 PCC participants were included, regardless of adherence to group assignment. There were no study related adverse events.
Table 1.
Effects of the adapted Personalized Cognitive Counseling (PCC) intervention on various classes of substances and substance use concurrent with sexual risk among episodic substance-using MSM, Project ECHO, San Francisco, CA, 2010–2012.
| Substance use outcomes | Baselinea (%) | 3 Month (%) | 6 Month (%) | GEE Poisson regression modelsb
|
|||
|---|---|---|---|---|---|---|---|
| RR | 95% CI | p-value | |||||
| Any substance use (exclusive of alcohol) | PCC | 85 | 79 | 83 | 0.98 | 0.9–1.07 | 0.31 |
| Control | 84 | 82 | 83 | ||||
| Any alcohol | PCC | 96 | 94 | 91 | 0.93 | .89–.97 | <0.001* |
| Control | 98 | 97 | 99 | ||||
| Any ecstasy | PCC | 21 | 24 | 28 | 1.31 | .94–1.83 | 0.12 |
| Control | 24 | 23 | 22 | ||||
| Any GHB | PCC | 7 | 7 | 7 | 0.62 | .31–1.24 | 0.18 |
| Control | 8 | 7 | 12 | ||||
| Any marijuana | PCC | 63 | 62 | 56 | 0.84 | .73–.98 | 0.02* |
| Control | 61 | 66 | 65 | ||||
| Any methamphetamine | PCC | 9 | 9 | 5 | 0.72 | .36–1.42 | 0.34 |
| Control | 10 | 10 | 8 | ||||
| Any poppers | PCC | 44 | 30 | 29 | 1.04 | .74–1.46 | 0.82 |
| Control | 41 | 28 | 26 | ||||
| Any crack | PCC | 2 | 3 | 4 | 1.64 | .65–4.15 | 0.29 |
| Control | 4 | 4 | 3 | ||||
| Any cocaine | PCC | 30 | 26 | 29 | 1.05 | .77–1.43 | 0.76 |
| Control | 35 | 24 | 30 | ||||
| Any prescription drugs | PCC | 12 | 10 | 9 | 0.57 | .31–1.03 | 0.06 |
| Control | 11 | 9 | 15 | ||||
| Any erectile dysfunction drugs | PCC | 22 | 16 | 13 | 0.51 | .33–.79 | <0.001* |
| Control | 16 | 18 | 21 | ||||
| Any UAI with alcohol, methamphetamine, cocaine or poppers | PCC | 79 | 34 | 31 | 0.85 | 0.61–1.17 | 0.25 |
| Control | 74 | 41 | 33 | ||||
| Baselinea (mean) | 3 Month (mean) | 6 Month (mean) | GEE negative binomial regression modelsb
|
||||
|---|---|---|---|---|---|---|---|
| RR | 95% CI | p-value | |||||
| No. UAI events w/alcohol | PCC | 2.28 | 0.83 | 0.75 | 0.69 | .39–1.2 | 0.19 |
| Control | 2.26 | 1.13 | 1.01 | ||||
| No. UAI events w/methamphetamine | PCC | 0.17 | 0.09 | 0.09 | 0.26 | .08–.84 | 0.02* |
| Control | 0.26 | 0.37 | 0.37 | ||||
| No. UAI events w/cocaine | PCC | 0.26 | 0.16 | 0.14 | 1.07 | .35–3.27 | 0.0 |
| Control | 0.33 | 0.12 | 0.15 | ||||
| No UAI events w/poppers | PCC | 0.86 | 0.27 | 0.22 | 0.0 | .24–1.52 | 0.28 |
| Control | 0.69 | 0.41 | 0.28 | ||||
| No. binge drinking days (5+ drinks) | PCC | 8.98 | 7.55 | 7.53 | 0.87 | .64–1.19 | 0.39 |
| Control | 8.68 | 7.78 | 8.51 | ||||
| Outcomec | Ordered logistic regression modelsa,b
|
||
|---|---|---|---|
| Odds ratio | 95% CI | p-value | |
| Alcohol intoxication frequency | 0.54 | 0.34–0.85 | 0.007* |
| Methamphetamine use frequency | 0.61 | 0.25–1.52 | 0.29 |
| Cocaine use frequency | 0.89 | 0.55–1.46 | 0.65 |
| Poppers use frequency | 1.05 | 0.63–1.73 | 0.85 |
| SDS Alcohol | 0.92 | 0.59–1.42 | 0.70 |
| SDS Methamphetamine | 0.79 | 0.27–2.32 | 0.67 |
| SDS Cocaine | 0.80 | 0.40–1.60 | 0.53 |
| SDS Poppers | 0.34 | 0.09–1.27 | 0.11 |
Notes: RR indicates rate ratio (i.e., the ratio of the intervention and control rates of change in the mean value of the outcome over time, our summary measure of the intervention effect. The linearity assumption was checked); CI, confidence interval; UAI, unprotected anal intercourse; SDS, severity of dependence scale score.
No significant differences in substance use outcomes were observed between PCC and Control conditions at baseline.
No evidence of violation from proportional odds assumption in all models.
Alcohol was measured as frequency of being intoxicated (i.e., “drunk or buzzed from alcohol); categories for alcohol and substance use are based no-use and frequency of use recoded into tertiles (i.e. 1–33‰, 34–66‰, 67–100‰); categories for severity of dependence scale are based on score of 0 and scores above zero recoded into tertiles.
p-value < 0.05.
3.2. Changes in substance use
A greater proportion of men in PCC abstained from alcohol, marijuana, and EDD during follow-up (Fig. 1). Over the study period, PCC participants reported significantly greater rates of abstinence from alcohol (RR = 0.93; 95% confidence interval (CI = 0.89–0.97), marijuana (RR = 0.84; 95% CI = 0.73–0.98) and EDD (RR = 0.51; 95% CI = 0.33–0.79), than controls. In addition, PCC participants reported greater declines in mean number of UAI events while under the influence of methamphetamine (RR = 0.26; 95% CI = 0.08–0.84) and significantly greater reductions in alcohol intoxication frequency (OR = 0.54; 95% CI = 0.34–0.85).
Fig. 1.
Substance use outcomes in project ECHO study, by arm – San Francisco, 2010–2012. Note: *No significant differences between PCC and control at baseline for alcohol (p = 0.34), marijuana (p = 0.82), EDD (p = 0.20), and UAI while under the influence of methamphetamine (p = 0.65).
4. Discussion
We observed significant intervention effects for several substance use outcomes. Specifically, abstinence from alcohol, marijuana, and EDD significantly increased while frequency of alcohol intoxication, as well as UAI events while intoxicated with methamphetamine significantly decreased among men receiving PCC, compared to controls. These intervention effects occurred among episodic SUMSM not seeking treatment to stop or reduce their substance use, but interested in participating in a study to reduce HIV-related sexual risk behaviors while under the influence of alcohol/substances. To our knowledge, this is the first study to report significant reductions in alcohol/substance use associated with PCC, identified by CDC as an evidence-based intervention for HIV-related sexual risk reduction among MSM (Centers for Disease Control and Prevention, 2013). Findings from this study raise the possibility of adapted PCC to affect HIV risk by reducing alcohol/substance use.
The finding that a brief behavioral intervention can effectively reduce alcohol consumption among MSM is broadly consistent with another study that observed motivational interviewing alone can lead to significant reductions in drinking among MSM (Morgenstern et al., 2007). We observed declines in UAI while intoxicated with methamphetamine in the PCC arm, but did not find significant effects on methamphetamine use. The finding that a behavioral intervention can reduce methamphetamine-related sexual risk behaviors in the context of ongoing methamphetamine use is broadly consistent with results from prior randomized intervention trials among methamphetamine users (Mausbach et al., 2007a,b). Collectively, these data support the feasibility of harm reduction strategies among methamphetamine users who may not be willing or able to abstain from use. However, our findings remain preliminary and additional studies are needed.
Although the increase in alcohol and marijuana abstinence associated with PCC in this study were modest, given the ubiquity of these two substances among SUMSM and the low-cost/low-resource attributes of PCC (AIDS Health Project, 2011), this counseling approach may be a cost-effective, population-level intervention, if further proven effective (Dilley et al., 2002, 2007). Furthermore, the significant effect of PCC on reducing frequency of alcohol intoxication corroborates the finding on alcohol abstinence and further suggests that these findings are robust.
Additionally, it is important to note the clinical significance and public health implications of PCC’s effect on frequency of alcohol intoxication, recreational use of EDD and number of UAI events while under the influence of methamphetamine, because these behaviors have been linked to risk of HIV acquisition and transmission among MSM (Carey et al., 2009; Fisher et al., 2010; Mansergh et al., 2006; Spindler et al., 2007). In this study, PCC had medium to large effect sizes (Chen et al., 2010; Schünemann et al., 2008) on these HIV-related risk factors (46%, 49% and 74% reductions for odds of alcohol intoxication frequency, rate of EDD use and rate of UAI concurrent with methamphetamine use, respectively); the magnitude of these estimates may portend to clinically significant intervention effects on these outcomes. Given the paucity of interventions for this non-dependent population, efforts to replicate these findings and adapt PCC to directly address these target substances may also be worthwhile.
It is unclear how a brief intervention, such as PCC, resulted in significant effects in some alcohol and substance use outcomes by 6-months. PCC sessions, though brief, may facilitate meaningful explorations of the self-justifications for risky behavior and motivate SUMSM to reducing their alcohol/substance use as a strategy to reduce their HIV-risk. Indeed, as reported in the primary outcome analyses, 6 of the 15 most frequently reported self-justifications for recent UAI in this study were alcohol/substance-related (Coffin et al., 2014). However, it is unclear why the intervention was effective for some substances, but not others. We hypothesize that this may be due to the heterogeneity of the physiologic effects and the varying strengths of association with HIV-risk for the different substance classes (Santos et al., 2013). Additionally, it’s unclear why some substances increased in the control group, though this may reflect the natural history of substance use (e.g., progression from recreational use to abuse, and then to dependence). Future studies are needed to fully elucidate the mechanism that contributed to these findings, and qualitative interviews may help pin-point ways to adapt PCC further to explicitly target alcohol/substance use outcomes.
This analysis has limitations. Outcomes were assessed through self-report. Although we used ACASI, some participants may have under-reported their use due to social desirability. Our study was limited to episodic SUMSM from San Francisco, and may not be generalizable to other populations. In addition, given the exploratory nature of this secondary data analysis, we did not formally adjust for multiple comparisons; thus, findings of nominal statistical significance should be interpreted with caution.
Despite these limitations, future investigations on the effect of PCC on substance use would be of public health importance, given the paucity of brief behavioral interventions for non-dependent substances users and acceptability of PCC among MSM (Dilley et al., 2007). This study found that PCC was beneficial in stopping or reducing substance use, including alcohol, marijuana, and EDD, and concurrent use of methamphetamine with high-risk sexual behaviors. These behaviors are common and strongly associated with risk for HIV among SUMSM.
Supplementary Material
Acknowledgments
We acknowledge all of the study participants who volunteered for this project, Project ECHO facilitators and staff (Erin Antunez, Reggie Gage, Alic Shook, Rand Dadasovich, Shannon Huffaker, Deirdre Santos and Kelly R. Knight), the recruitment coordinator, John Farley, and field recruitment team.
Supported by the Centers for Disease Control and Prevention under cooperative agreement UR6PS000684 to Public Health Foundation Enterprises, City of Industry, CA.
Appendix A. Supplementary data
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.drugalcdep.2014.02.015.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering http://dx.doi.org/10.1016/j.drugalcdep.2014.02.015.
The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Conflict of interest
No conflict declared.
Role of funding source
Nothing declared.
Author contributors
Agree with the manuscript’s results and conclusions: all coauthors Designed the experiments/the study: G.C., M.D., T.M., G.M.S., J.D., E.V., J.H. Analyzed the data: G.M.S., E.V. Collected data/did experiments for the study: T.M., E.D. Enrolled patients: E.D., T.M. Managed the project: G.C., P.C., M.D., T.M. Acquired funding: G.C., M.D., T.M. Interpreted data: G.M.S., E.V., P.C., M.D., T.M., E.D., J.D., J.H., J.R., M.C. Wrote the report: G.M.S., P.C., J.H., T.M. Revised the report: G.M.S., P.C., E.D., G.C., M.D., T.M., J.D., E.V., J.R., M.C., J.H.
References
- AIDS Health Project. AIDS Health Project. University of California, San Francisco; San Francisco, CA: 2011. [Accessed on 18.10.13]. Personalized Cognitive Counseling: Implementation Manual. http://www.effectiveinterventions.org/Libraries/PCC_Docs/13-0204_PCC_Final_IM_Appendices_and_Workbook.sflb.ashx. [Google Scholar]
- Baker A, Boggs TG, Lewin TJ. Randomized controlled trial of brief cognitive-behavioural interventions among regular users of amphetamine. Addiction. 2001;96:1279–1287. doi: 10.1046/j.1360-0443.2001.96912797.x. [DOI] [PubMed] [Google Scholar]
- Baker A, Lee NK, Claire M, Lewin TJ, Grant T, Pohlman S, Saunders JB, Kay-Lambkin F, Constable P, Jenner L, Carr VJ. Brief cognitive behavioural interventions for regular amphetamine users: a step in the right direction. Addiction. 2005;100:367–378. doi: 10.1111/j.1360-0443.2005.01002.x. [DOI] [PubMed] [Google Scholar]
- Carey JW, Mejia R, Bingham T, Ciesielski C, Gelaude D, Herbst JH, Sinunu M, Sey E, Prachand N, Jenkins RA, Stall R. Drug use, high-risk sex behaviors, and increased risk for recent HIV infection among men who have sex with men in Chicago and Los Angeles. AIDS Behav. 2009;13:1084–1096. doi: 10.1007/s10461-008-9403-3. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control Prevention. Vital signs: binge drinking prevalence, frequency, and intensity among adults — United States. MMWR. 2012;61:14–16. [PubMed] [Google Scholar]
- Centers for Disease Control Prevention. [Accessed on 3.07.13];Compendium of Evidence-based HIV Behavioral Interventions. 2013 http://www.cdc.gov/hiv/prevention/research/compendium/rr/characteristics.html.
- Chen H, Cohen P, Chen S. How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Commun Stat Simul Comput. 2010;39:860–864. [Google Scholar]
- Cochran SD, Ackerman D, Mays VM, Ross MW. Prevalence of non-medical drug use and dependence among homosexually active men and women in the US population. Addiction. 2004;99:989–998. doi: 10.1111/j.1360-0443.2004.00759.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffin P, Santos GM, Das M, Matheson T, DeMicco E, Herbst JH, Raiford JL, Carry M, Dilley J, Vittinghoff E. Adapted personalized cognitive counseling for episodic substance-using men who have sex with men: a randomized controlled trial. AIDS Behav. 2014 doi: 10.1007/s10461-014-0712-4. http://dx.doi.org/10.1007/s10461-014-0712-4, Epub ahead of print. [DOI] [PMC free article] [PubMed]
- Colfax G, Santos GM, Chu P, Vittinghoff E, Pluddemann A, Kumar S, Hart C. Amphetamine-group substances and HIV. Lancet. 2010;376:458–474. doi: 10.1016/S0140-6736(10)60753-2. [DOI] [PubMed] [Google Scholar]
- Colfax G, Vittinghoff E, Husnik MJ, McKirnan D, Buchbinder S, Koblin B, Celum C, Chesney M, Huang Y, Mayer K, Bozeman S, Judson FN, Bryant KJ, Coates TJ. Substance use and sexual risk: a participant- and episode-level analysis among a cohort of men who have sex with men. Am J Epidemiol. 2004;159:1002–1012. doi: 10.1093/aje/kwh135. [DOI] [PubMed] [Google Scholar]
- Daeppen JB, Bertholet N, Gaume J, Fortini C, Faouzi M, Gmel G. Efficacy of brief motivational intervention in reducing binge drinking in young men: a randomized controlled trial. Drug Alcohol Depend. 2011;113:69–75. doi: 10.1016/j.drugalcdep.2010.07.009. [DOI] [PubMed] [Google Scholar]
- Dilley JW, Woods WJ, Loeb L, Nelson K, Sheon N, Mullan J, Adler B, Chen S, McFarland W. Brief cognitive counseling with HIV testing to reduce sexual risk among men who have sex with men: results from a randomized controlled trial using paraprofessional counselors. J Acquir Immune Defic Syndr. 2007;44:569–577. doi: 10.1097/QAI.0b013e318033ffbd. [DOI] [PubMed] [Google Scholar]
- Dilley JW, Woods WJ, Sabatino J, Lihatsh T, Adler B, Casey S, Rinaldi J, Brand R, McFarland W. Changing sexual behavior among gay male repeat testers for HIV: a randomized, controlled trial of a single-session intervention. J Acquir Immune Defic Syndr. 2002;30:177–186. doi: 10.1097/00042560-200206010-00006. [DOI] [PubMed] [Google Scholar]
- Drumright LN, Patterson TL, Strathdee SA. Club drugs as causal risk factors for HIV acquisition among men who have sex with men: a review. Subst Use Misuse. 2006;41:1551–1601. doi: 10.1080/10826080600847894. [DOI] [PubMed] [Google Scholar]
- Finlayson TJ, Le B, Smith A, Bowles K, Cribbin M, Miles I, Oster AM, Martin T, Edwards A, Dinenno E. HIV risk, prevention, and testing behaviors among men who have sex with men—National HIV Behavioral Surveillance System, 21 U.S. cities, United States 2008. MMWR Surveill Summ. 2011:1–34. [PubMed] [Google Scholar]
- Fisher DG, Reynolds GL, Napper LE. Use of crystal methamphetamine, viagra, and sexual behavior. Curr Opin Infect Dis. 2010;23:53–56. doi: 10.1097/QCO.0b013e328334de0b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gossop M, Darke S, Griffiths P, Hando J, Powis B, Hall W, Strang J. The severity of dependence scale (SDS): psychometric properties of the SDS in English and Australian samples of heroin, cocaine and amphetamine users. Addiction. 1995;90:607–614. doi: 10.1046/j.1360-0443.1995.9056072.x. [DOI] [PubMed] [Google Scholar]
- Knight KR, Das M, Demicco E, Raiford JL, Matheson T, Shook A, Antunez E, Santos GM, Dadasovich R, Dilley JW, Colfax GN, Herbst JH. A roadmap for adapting an evidence-based HIV prevention intervention: personal cognitive counseling (PCC) for episodic substance-using men who have sex with men. Prev Sci. 2013 doi: 10.1007/s11121-013-0364-z. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koblin BA, Husnik MJ, Colfax G, Huang Y, Madison M, Mayer K, Barresi PJ, Coates TJ, Chesney MA, Buchbinder S. Risk factors for HIV infection among men who have sex with men. AIDS. 2006;20:731–739. doi: 10.1097/01.aids.0000216374.61442.55. [DOI] [PubMed] [Google Scholar]
- Leigh BC, Stall R. Substance use and risky sexual behavior for exposure to HIV. Issues in methodology, interpretation, and prevention. Am Psychol. 1993;48:1035–1045. doi: 10.1037//0003-066x.48.10.1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, Amann M, Anderson HR, Andrews KG, Aryee M, Atkinson C, Bacchus LJ, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the global burden of disease study. Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansergh G, Shouse RL, Marks G, Guzman R, Rader M, Buchbinder S, Colfax GN. Methamphetamine and sildenafil (viagra) use are linked to unprotected receptive and insertive anal sex, respectively, in a sample of men who have sex with men. Sex Transm Infect. 2006;82:131–134. doi: 10.1136/sti.2005.017129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mausbach BT, Semple SJ, Strathdee SA, Zians J, Patterson TL. Efficacy of a behavioral intervention for increasing safer sex behaviors in HIV-negative, heterosexual methamphetamine users: results from the fast-lane study. Ann Behav Med. 2007a;34:263–274. doi: 10.1007/BF02874551. [DOI] [PubMed] [Google Scholar]
- Mausbach BT, Semple SJ, Strathdee SA, Zians J, Patterson TL. Efficacy of a behavioral intervention for increasing safer sex behaviors in HIV-positive MSM methamphetamine users: results from the EDGE study. Drug Alcohol Depend. 2007b;87:249–257. doi: 10.1016/j.drugalcdep.2006.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenstern J, Bux DA, Jr, Parsons J, Hagman BT, Wainberg M, Irwin T. Randomized trial to reduce club drug use and HIV risk behaviors among men who have sex with men. J Consult Clin Psychol. 2009;77:645–656. doi: 10.1037/a0015588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenstern J, Irwin TW, Wainberg ML, Parsons JT, Muench F, Bux DA, Jr, Kahler CW, Marcus S, Schulz-Heik J. A randomized controlled trial of goal choice interventions for alcohol use disorders among men who have sex with men. J Consult Clin Psychol. 2007;75:72–84. doi: 10.1037/0022-006X.75.1.72. [DOI] [PubMed] [Google Scholar]
- Ostrow DG, Plankey MW, Cox C, Li X, Shoptaw S, Jacobson LP, Stall RC. Specific sex drug combinations contribute to the majority of recent HIV seroconversions among MSM in the MACS. J Acquir Immune Defic Syndr. 2009;51:349–355. doi: 10.1097/QAI.0b013e3181a24b20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanchez T, Finlayson T, Drake A, Behel S, Cribbin M, Dinenno E, Hall T, Kramer S, Lansky A. Human immunodeficiency virus (HIV) risk, prevention, and testing behaviors—United States, National HIV Behavioral Surveillance System: men who have sex with men, November 2003–April 2005. MMWR Surveill Summ. 2006;55:1–16. [PubMed] [Google Scholar]
- Sander PM, Cole SR, Stall RD, Jacobson LP, Eron JJ, Napravnik S, Gaynes BN, Johnson-Hill LM, Bolan RK, Ostrow DG. Joint effects of alcohol consumption and high-risk sexual behavior on HIV seroconversion among men who have sex with men. AIDS. 2013;27:815–823. doi: 10.1097/QAD.0b013e32835cff4b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos GM, Coffin PO, Das M, Matheson T, Demicco E, Raiford JL, Vittinghoff E, Dilley JW, Colfax G, Herbst JH. Dose-response associations between number and frequency of substance use and high-risk sexual behaviors among HIV-negative substance-using men who have sex with men (SUMSM) in San Francisco. J Acquir Immune Defic Syndr. 2013;63:540–544. doi: 10.1097/QAI.0b013e318293f10b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos GM, Das M, Colfax GN. Interventions for non-injection substance use among US men who have sex with men: what is needed. AIDS Behav. 2011;15(Suppl 1):S51–S56. doi: 10.1007/s10461-011-9923-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schünemann HJ, Oxman AD, Vist GE, Higgins JPT, Deeks JJ, Glasziou P, Guyatt GH. Chapter 12: Interpreting results and drawing conclusions. In: Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration; 2008. Version 5.0.1 [updated September 2008] Available from www.cochrane-handbook.org. [Google Scholar]
- Smedslund G, Berg RC, Hammerstrom KT, Steiro A, Leiknes KA, Dahl HM, Karlsen K. Motivational interviewing for substance abuse. Cochrane Database Syst Rev. 2011:CD008063. doi: 10.1002/14651858.CD008063.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spindler HH, Scheer S, Chen SY, Klausner JD, Katz MH, Valleroy LA, Schwarcz SK. Viagra, methamphetamine, and HIV risk: results from a probability sample of MSM, San Francisco. Sex Transm Dis. 2007;34:586–591. doi: 10.1097/01.olq.0000258339.17325.93. [DOI] [PubMed] [Google Scholar]
- Vosburgh HW, Mansergh G, Sullivan PS, Purcell DW. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS Behav. 2012;16:1394–1410. doi: 10.1007/s10461-011-0131-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.