Abstract
Background:
Post cardiac surgery routine chest radiographs (CXRs), ordered without any clinical and laboratory indications, is a standard obligatory practice in many cardiothoracic centers. Routine CXRs incur cost, manpower, and radiation. The objective of this study is to assess early outcome in off-pump coronary artery bypass (OPCAB) patients with postoperative routine versus clinically indicated CXR protocols.
Materials and Methods:
This study is a randomized clinical trial conducted on 231 OPCAB candidates in Afshar Cardiac Center, Yazd, Iran. Patients were categorized into two groups. All 118 patients in group A had routine postoperative CXRs. The 113 patients in group B were selectively exposed to CXR only on clinical indications. All patients were postoperatively followed up for 30 days. Data gathered from both groups were statistically analyzed.
Results:
Routine postoperative CXRs obtained in 118 OPCAB group A candidates showed abnormal findings in 20 patients that did not require new intervention. One month follow-up of these patients showed no complications. In 113 OPCAB candidates of group B, 7 on-demand CXRs were obtained on clinical evaluation that required added intervention. In a 1-month follow-up of this group, five patients presented with symptomatic complaints. On re-examination, none needed readmission, intervention, or paraclinical evaluation. No complications were observed due to CXR elimination.
Conclusion:
The study suggests that postoperative CXR selected on clinical grounds in place of routine CXR does not change early postoperative outcome of OPCAB procedure.
Keywords: Chest radiograph, off-pump coronary artery bypass, outcome
INTRODUCTION
Coronary artery bypass grafting (CABG), a landmark procedure in cardiovascular history, is today a leading cardiac operation.[1] The time-honored on-pump CABG has often been replaced by an equally effective, alternative, comparatively economical off-pump coronary artery bypass (OPCAB) procedure particularly performed in patients with co-morbid conditions including renal impairment and increased risk of cardiovascular accident.[2] Pre- and postoperative orders for a frequently practiced procedure may need revision.
Postoperative routine chest radiograph (CXR) is a conventional protocol, practiced in most cardiothoracic centers, undertaken without any clinical or laboratory indications. Although postoperative CXR has been broadly evaluated in cardiac surgeries, in general, however, different cardiac procedures merit selective postoperative protocols as in OPCAB. Clinical cardiopulmonary findings are not always revealed on CXR.[3] Its accuracy in visualizing and defining etiology of pulmonary opacity is moderate.[4] Not all abnormal cardiopulmonary CXR findings after OPCAB are unexpected or require change of management.[5,6] In addition, cost, manpower resources, radiation, and manipulation of the critically ill patients that may induce transient hemodynamic instability and endotracheal tube (ETT) and vascular catheter displacement make routine CXR debatable.[6,7]
MATERIALS AND METHODS
This clinical trial was conducted at Afshar Cardiac Center, a university hospital in Yazd, Iran. The study was approved by the Hospital Research Ethics Committee. A total of 231 patients over a period of 6 months from March to September 2011 were subjected to the OPCAB procedure. Patients were randomized into two groups using simple randomization: Group A included 118 patients and group B 113 patients. Routine CXR was obtained for all 118 patients in group A. On-demand CXR was advised for selective patients in group B. All patients were carefully monitored postoperatively for cardiopulmonary complications. Hemodynamics, pulse oximetry, arterial blood gas analysis, frequent auscultation of lungs and control of chest tube drains, and position of ETT and vascular lines were among the critical care protocol.
Routine CXR was obtained without any clinical indication. On-demand CXR was obtained on clinical findings, either to confirm or clarify clinical diagnosis. Selection on clinical evaluation was based on findings of fever, dyspnea, abnormal pulmonary sounds, signs and symptoms of cardiac tamponade, lower extremity edema, abnormal chest tube bleed or air leak, and doubtful position of ETT and vascular lines. Final clinical evaluation for on-demand CXR rested on the cardiovascular surgeon and X-ray findings were reported by the radiologist. All patients were discharged 5-7 days after surgery. A 30-day follow-up included at least two visits. Patients were in constant contact with the cardiac clinic. Symptomatic patients were selectively re-examined to rule out complications.
A detailed questionnaire was completed for each patient. Clinical indication resulting in on-demand CXR, X-ray findings, and new intervention were recorded. Data obtained from both groups were statistically analyzed by SPSS 11.5 (SPSS Inc, Chicago, IL) using Chi-square and Fisher's exact test. P value of 0.05 was considered statistically significant [Figure 1].
Figure 1.
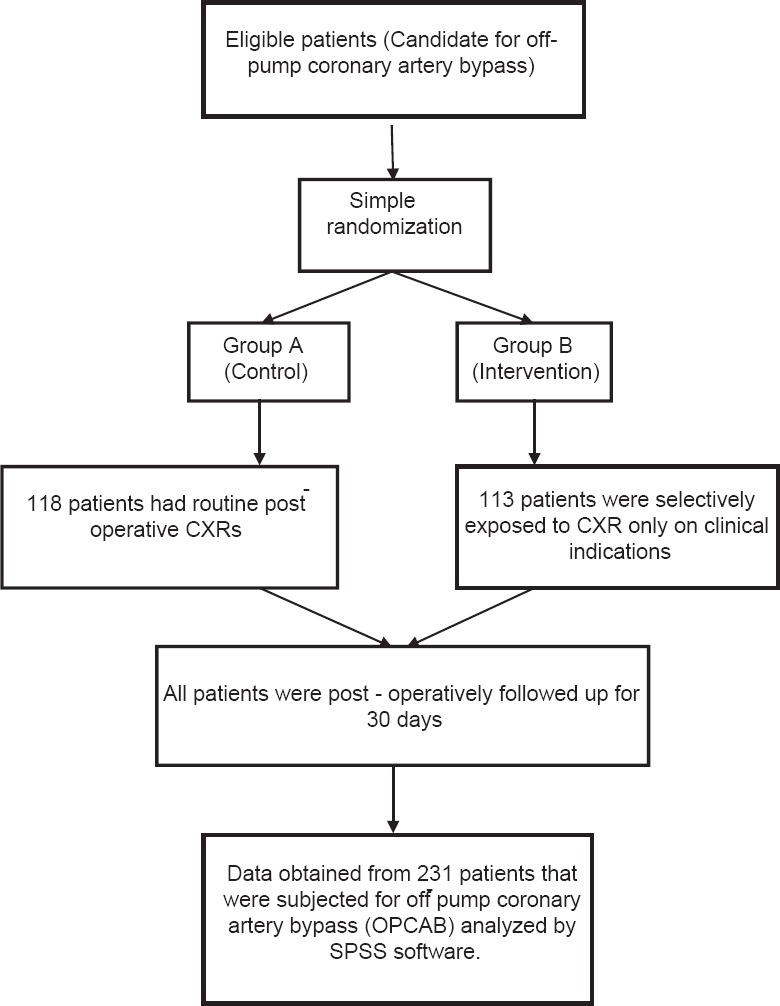
The flowchart of study groups
RESULTS
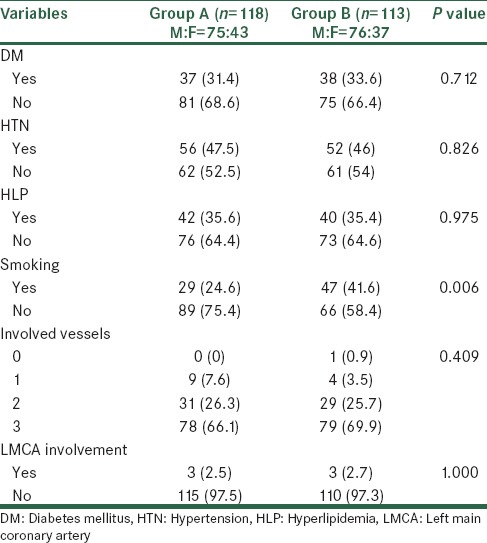
A total of 231 OPCAB candidates including 151 males (65.4%) and 80 females (34.6%) with ages ranging from 31 to 83 years (average 60.2) were categorized into two groups. Although efforts were made to balance the two groups, age and tobacco smoke exposure were greater and statistically significant in group B. These variables were not critical for the study. However, no significant differences were observed between preoperative variables of gender, diabetes mellitus, hypertension, hyperlipidemia, number of coronary vessels involved and, in particular, left main coronary artery (LMCA) lesion [Table 1].
Table 1.
Preoperative variables in groups A and B
All 118 patients of group A obtained CXR as a routine protocol. Twenty abnormal CXRs were observed including five atelectasis, five pulmonary opacities, nine mild pleural effusion, and one abnormal position of diaphragm. The remaining 98 group A patients had normal CXRs. None of the 20 patients with positive CXR findings required new intervention.
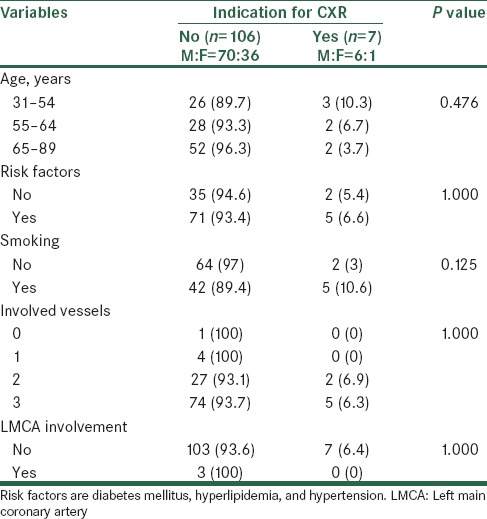
On-demand CXRs were obtained in seven group B patients on clinical grounds. These included three patients with abnormal pulmonary sounds, three patients with chest tube air leak, and one case with subcutaneous emphysema. Positive X-ray findings included pneumothorax, hydropneumothorax, massive pleural effusion, lobar atelectasis, and pulmonary congestion, clarifying or confirming clinical findings in each case. All seven on-demand CXRs prompted change in management. There was no statistically significant relationship between preoperative variables and indication for CXR in group B patients [Table 2].
Table 2.
Relationship between preoperative variables and indication for CXR in group B
A 30-day follow-up was undertaken for both groups. Group A had a normal follow-up. In group B, 5 patients presented with symptomatic complaints including three cases of dyspnea, one with fever and rigor, and one with chest pain. On re-examination, none needed readmission, intervention, or paraclinical evaluation. No complications were observed due to CXR elimination.
DISCUSSION
Routine postoperative CXR is a standard of care in many centers all over the world. However, the protocol has been often questioned by some authors. These include Roa et al., Silverstein et al., O’Brien et al., and of recent, Ganapathy et al. and Tolsma et al., who favor the elimination of routine CXR.[8,9,10,11,12,13,14]
Most current literatures refer to routine CXR evaluation after cardiac surgeries in general. Protocols in elective cardiac operations differ from emergency post-traumatic cardiac operations wherein postoperative CXR would be mandatory. Accompanying trivial lung injuries in post-traumatic cases are often missed and may flare up in course of time, emphasizing postoperative screening with CXR.[15]
Likewise, clinical settings may influence the rule of CXR. Pediatric examination, particularly in ICU, is more complex and less informative.[16] CXR in these settings mostly reveal malposition of devise. The effect of a minor intervention, performed on CXR findings, can be significant in the critically ill children.[17] Also, each elective cardiac surgery would require a selective postoperative protocol. This is a study for routine and clinically indicated postoperative CXR in exclusively OPCAB candidates with regards to early postoperative outcome.
Findings on routine CXR may not always influence management. Several postoperative radiological findings, including minor atelectasis and minimal-to-moderate pleural effusion, usually resolve spontaneously.[5,6] In our study, all 20 abnormal routine CXR findings in group A did not prompt new intervention. On the other hand, clinically it indicated on-demand CXR changed management status.
In contrast to group A candidates, 106 patients in group B who were closely clinically followed did not require CXR, thus saving on cost, manpower, and avoiding unnecessary maneuver and cumulative radiation, both to attending staff and patients.[6,7] No differences were observed in 30-day postoperative outcome between the both groups.
The use of CXR to confirm position of ETT and vascular lines remains controversial. O’Brien and colleagues demonstrated that clinical evaluation of ETT proved to be more sensitive than CXR.[12] Palesty et al. and Gray et al. concluded that CXR was unnecessary for vascular line position;[18,19] however, Gladwin et al. had contradictory thoughts, emphasizing the need for CXR.[20]
Post cardiac surgery echocardiography in cardiac tamponade is a more reliable diagnostic tool than CXR. Since the pericardium is left open after surgery, the cardiac silhouette stands abnormal on CXR. A series of CXRs would be needed to detect changes in the abnormal cardiac shadow. In addition, cardiac dilatation cannot be ruled out from pericardial effusion. In contrast, even a 20-50 ml pericardial effusion is detected by echocardiography.[21] Likewise, sonography more accurately detects diaphragmatic motility than CXR.[22] Routine postoperative CXR shows limited reliability in these complications. The application of a more sensitive alternative method for evaluation in these situations is recommended.
CONCLUSION
Clinically indicated CXR in place of routine CXR after OPCAB procedure significantly reduced the number of CXRs without affecting the length of hospital stay, readmission rate, and mortality rate. Thus, it seems that postoperative on-demand CXR on clinical evaluation is an efficacious, cost-effective, and comparatively safe protocol than routine CXR.
In order to eliminate limitations of this study, greater number of patients sampling, evaluation at different cardiothoracic centers, and a postoperative follow-up beyond 30 days are recommended for future studies.
ACKNOWLEDGMENT
We would like to express our appreciation to the nursing staff of Afshar Cardiac Center for their invaluable assistance during the study. This study is an extract from a thesis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Shekar PS. On-pump and off-pump coronary artery bypass grafting. Circulation. 2006;113:e51–2. doi: 10.1161/CIRCULATIONAHA.105.566737. [DOI] [PubMed] [Google Scholar]
- 2.Nwaejike N, Mansha M, Bonde P, Campalani G. Myocardial revascularization by off-pump coronary bypass surgery (OPCABG): A ten year review. Ulster Med J. 2008;77:106–9. [PMC free article] [PubMed] [Google Scholar]
- 3.Wiener-Kronish JP. Postoperative pleural and pulmonary abnormalities in patients undergoing coronary artery bypass grafts. Chest. 1992;102:1313–4. doi: 10.1378/chest.102.5.1313. [DOI] [PubMed] [Google Scholar]
- 4.Rubenfield GD, Caldwell E, Granton J, Hudson LD, Matthay MA. Interobserver variability in applying a radiographic definition for ARDS. Chest. 1999;116:1347–53. doi: 10.1378/chest.116.5.1347. [DOI] [PubMed] [Google Scholar]
- 5.Labidi M, Baillot R, Dionne B, Lacasse Y, Maltais F, Boulet LP. Pleural effusions following cardiac surgery: Prevelance, risk factors, and clinical features. Chest. 2009;136:1604–11. doi: 10.1378/chest.09-0689. [DOI] [PubMed] [Google Scholar]
- 6.Roa PS, Abid Q, Khan KJ, Meikle RJ, Natarajan KM, Morritt GN, et al. Evaluation of routine postoperative chest X-rays in the management of cardiac surgical patient. Eur J Cardiothorac Surg. 1997;12:724–9. doi: 10.1016/s1010-7940(97)00132-2. [DOI] [PubMed] [Google Scholar]
- 7.Chahine-Malus N, Stewart T, Lapinsky SE, Marras T, Dancey D, Leung R, et al. Utility of routine chest radiographs in a medical-surgical intensive care unit: A quality assurance survey. Crit Care. 2001;5:271–5. doi: 10.1186/cc1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chong JL, Pillai R, Fisher A, Grebenik C, Sinclair M, Westaby S. Cardiac surgery: Moving away from intensive care. Br Heart J. 1992;68:430–3. doi: 10.1136/hrt.68.10.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hornick PI, Harris P, Cousins C, Taylor KM, Keogh BE. Assessment of the value of the immediate postoperative chest radiograph after cardiac operation. Ann Thorac Surg. 1995;59:1150–4. doi: 10.1016/0003-4975(95)00087-2. [DOI] [PubMed] [Google Scholar]
- 10.Stevens JJ, Booth JV, Little J, Gopinath S, Ghosh S, Kneeshaw JD, et al. The value of immediate postoperative chest radiography in adult cardiac surgery. Br J Anaesth. 1995;A110:56. [Google Scholar]
- 11.Silverstein DS, Livingston DH, Elcavage J, Kovar L, Kelly KM. The utility of routine chest radiography in the surgical intensive care unit. J Trauma. 1993;35:643–6. doi: 10.1097/00005373-199310000-00022. [DOI] [PubMed] [Google Scholar]
- 12.O’Brien W, Karski J, Cheng D, Sandler A. Does the immediate postoperative chest x-ray help in the clinical management of patients following cardiac surgery. Can J Anaesth. 1995;42:A3–76. [Google Scholar]
- 13.Tolsma M, Rijpstra TA, Schultz MJ, Mulder PG, van der Meer NJ. Significant changes in the practice of chest radiography in Dutch intensive care units: A web-based survey. Ann Intensive Care. 2014;4:10. doi: 10.1186/2110-5820-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ganapathy A, Adhikari NK, Spiegelman J, Scales DC. Routine chest x-rays in intensive care units: A systemic review and meta-analysis. Crit Care. 2012;16:R68. doi: 10.1186/cc11321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahangar AG, Dar AM, Mir IA, Bhat MA, Lone GN, Shah SH. Role of routine chest roentgenography in patients with open heart operation. J K Science. 2003;5:104–6. [Google Scholar]
- 16.Hauser GJ, Pollack MM, Sivit CJ, Taylor GA, Balas DI, Guion CJ. Routine chest radiographs in pediatric intensive care: A prospective study. Pediatrics. 1989;83:465–70. [PubMed] [Google Scholar]
- 17.Quasney MW, Goodman DM, Billow M, Chiu H, Easterling L, Frankel L, et al. Routine chest radiographs in pediatric intensive care units. Pediatrics. 2001;107:241–8. doi: 10.1542/peds.107.2.241. [DOI] [PubMed] [Google Scholar]
- 18.Palesty JA, Amshel CE, Dudrick SJ. Routine chest radiographs following central venous recatheterization over a wire are not justified. Am J Surg. 1998;176:618–21. doi: 10.1016/s0002-9610(98)00283-9. [DOI] [PubMed] [Google Scholar]
- 19.Gray P, Sullivan G, Ostryzniuk P, McEwen TA, Rigby M, Roberts DE. Value of postprocedural chest radiographs in adult intensive care unit. Crit Care Med. 1992;20:1513–8. doi: 10.1097/00003246-199211000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Gladwin MT, Slonim A, Landucci DL, Gutierrez DC, Cunnion RE. Canulation of the internal jugular vein: Is postprocedural chest radiography always necessary? Crit Care Med. 1999;27:1819–23. doi: 10.1097/00003246-199909000-00019. [DOI] [PubMed] [Google Scholar]
- 21.Hamid M, Khan MU, Bashour AC. Diagnostic value of chest x-ray and echocardiography for cardiac tamponade in post cardiac surgery patients. J Pak Med Assoc. 2006;56:104–7. [PubMed] [Google Scholar]
- 22.Fedulla AJ, Lerner RM, Gibson J, Shayne DS. Sonographic measurement of diaphragmatic motion after coronary artery bypass surgery. Chest. 1992;102:1683–6. doi: 10.1378/chest.102.6.1683. [DOI] [PubMed] [Google Scholar]


