Abstract
Background:
Pneumonia due to ventilator is a prevalent nosocomial infection associated with high morbidity and mortality. This study aimed to determine the change in serum levels of precalcitonin (PCT) and C-reactive protein (CRP) in response to antibiotic treatment in patients hospitalized in intense care unit (ICU) suffering from ventilator-associated pneumonia (VAP).
Materials and Methods:
This is an analytical and descriptive study performed in 2013 in Ayatollah Kashani Medical Training Center, Isfahan, Iran. The statistical sample includes patients hospitalized in ICU in 2013 suffering from VAP. In this study, 50 patients suffering from VAP were selected, and PCT and CRP levels were measured in them before antibiotic therapy and every 48 h until the end of therapy. The collected data were analyzed by SPSS software.
Results:
CRP and PCT levels were high before the beginning of antibiotic therapy in all patients suffering from VAP and their CRP level had an increasing trend until 4 days after the beginning of therapy; however, from the 4th day, it turned into decreasing trend. PCT serum level was higher than normal before the treatment and until 48 h after the therapy, and then it was found to have a decreasing trend. According to variance analysis test with repetition of observations, the mean level of mentioned markers had a meaningful difference before the beginning of antibiotic therapy until the end of antibiotic therapy (P < 0.001).
Conclusion:
CRP and PCT serum levels can be used as an instrument for determining the effect of antibiotic therapy in patients with VAP.
Keywords: C-reactive protein, precalcitonin, ventilator pneumonia
INTRODUCTION
Nowadays, the nosocomial infections are one of the most common disorders in hospitalized patients, and despite the fact that intensive care units (ICUs) include just 5–15% of hospital beds, more than 30% of nosocomial infections are due to these units.[1]
Pneumonia is considered a prevalent, serious, and costly symptom in hospitalized patients due to the use of ventilator in ICU; it allocates the first rank concerning hospital-induced infections.[2] Ventilator-associated pneumonia (VAP) is usually created after 48 h from endotracheal intubation and mechanical ventilation[3] and since its prevalence varies from 9% to 27% and its resulting death varies from 30% to 70%, its epidemiological care has been seriously considered.[4] VAP risk increases from 1% to 3% daily in patients with mechanical ventilation.
Clinical and microbiological diagnoses of VAP, its risk factors, prevention indices, and its experimental treatment are still controversial. VAP depends on the statistical sample, ICU type, and diagnostic criteria.[5] Some of the predisposing factors of VAP include age, consciousness level, trauma, and burning, and the severity of underlying disease leads to increased incidence of VAP. Despite this, the history of antibiotic consumption and mechanical ventilation are considered as the main factors. The highest rate of VAP happens in the 5th day of mechanical ventilation.[6]
In most studies, enteric Gram-negative bacilli, Pseudomonas and Staphylococcus aureus, have been reported as three main factors of VAP. Knowledge of VAP and its antibiotic resistance patterns seem to be necessary for improvement and promotion of nosocomial infection control and the use of effective methods of prevention and control.[7]
Using sensitive methods, it becomes clear that C-reactive protein (CRP) is present in very low amounts in normal individuals and its rate might increase several times immediately after excitement. Compared to other factors of cute phase, an increase in CRP is rapid and can be evaluated between 6 and 12 h from the beginning of inflammatory stages. In the case of lack of disease control or incidence of the problem, its rate increases or remains high. Evaluation of CRP for diagnosis of bacterial meningitis, septicemia, pneumonia, and aspiration pneumonia has a critical value. Thus, significant variations of CRP with respect to the disease can effectively indicate improvement and efficiency of the treatment.[8] In serum of healthy kids and adults, CRP values are very low, and the normal rate is 0.8–4 mg/dl.[8,9]
Precalcitonin (PCT) serum level has direct relation with diseases; however, its values differ in different individuals. PCT levels increase in infections, emergency patients, patients in ICU, and after surgery in patients suffering from respiratory tract infection, meningitis, and abdominal infections. This index can be used in diagnosis, prognosis, and the effect of antibiotic therapy in acute diseases.[8] Serum level of PCT is < 0.05μg/L in normal individuals.[10]
There was no study in this field in Iran and Asian countries due to different bacterial etiology of VAP in various areas; on the other hand, because of drug resistance and treatment failure of different strains, it seems necessary to evaluate the CRP and PCT levels in ICU patients suffering from VAP. PCT and CRP are two laboratorial markers whose values are supposed to increase during suffering from VAP,[7] however a few studies have been done in this area and the obtained results are contradictory. Thus, concerning high incidence of VAP in ICU, the present study has been done with the aim of determining the value of PCT and CRP in diagnosis of pneumonia due to ventilator in 2013 in Ayatollah Kashani Medical Center of Isfahan.
MATERIALS AND METHODS
This analytical and descriptive study was performed in Ayatollah Kashani Medical Training Center, Isfahan, Iran in 2013. The inclusion criteria included ICU patients suffering from VAP, connected to ventilator at least for 48 h, and not suffering from chronic lung diseases.
VAP diagnosis was done according to Center for Disease Control instructions.[7] According to the mentioned criteria, for diagnosis of VAP, at least one of the following criteria should be observed in patients:
Fever (T >38°C) without other recognized cause
White blood cells <4000/mm or 12,000/mm
For adults >70 years, altered mental status without other recognized cause.
Plusradiographic criteria:
At least two serial X-rays with new or progressive and persistent infiltrate, consolidate, or cavitation that develops >48 h after initiation of mechanical ventilation.
And at least two of the following:
New-onset purulent sputum or change in the character of sputum or increased respiratory secretions
New-onset or worsening of a cough, dyspnea, or tachypnea
Rales or bronchial breath sounds
Worsening ventilation or oxygenation.
The occurrence of heart failure and death in the first 48 h of hospitalization are exclusion criteria.
The required sample size for this study has been estimated to be 48, through sample size estimation for comparison of ratios and by (1) consideration of reliability level of 95%, (2) a VAP prevalence of 15% as estimated in previous studies, and (3) error acceptance of 0.1. For more reliability, 50 patients were included.
Demographic information of patients including age, gender, the reason for hospitalization, duration of hospitalization in ICU, duration of being connected to ventilator, and suffering from underlying diseases were collected through the profile of the patient and registered in the special form that was prepared for this end.
Patients’ PCT and CRP serum levels were measured before antibiotic therapy and every 48 h until 10 days.
Sequential organ failure assessment (SOFA) score is a mortality prediction score, that is, based on the degree of dysfunction of 6 organ systems.
The SOFA was designed to focus on organ dysfunction and morbidity, with less of an emphasis on mortality prediction. The authors designed the system with an emphasis on bedside applicability and simplicity using widely available Var.[8] SOFA score was daily checked.
The obtained data were entered into the computer and analyzed through SPSS (version 22) and repeated-measures ANOVA and t-test.
RESULTS
In this study, 50 patients suffering from VAP were studied and investigated. The average age of patients was 45.7 ± 17.8 years, ranging from 22 to 78. Twenty-nine patients (58%) were male, and 21 (42%) were female. The mean age of men and women was 44.8 ± 18 and 47.1 ± 17.9 years, respectively, and according to t-test, there was no meaningful difference between men and women (P = 0.65).
Twenty-one individuals (42%) were hospitalized in ICU due to trauma, seven individuals (14%) due to intracerebral hemorrhage, 16 individuals (32%) due to stroke, two individuals (4%) due to brain tumor, and two individuals (4%) due to lung contusion.
The average hospitalization duration in ICU was 16.3 ± 5 days, ranging from 8 to 25 days. Average duration of connection to ventilator was 14.4 ± 5.4 days, ranging from 6 to 25 days and average interval of entrance to ICU to suffering from VAP was 4.36 ± 2.03 days, ranging from 2 to 12 days.
According to the results, CRP and PCT serum levels were high before beginning of antibiotic therapy in all individuals suffering from VAP, and CRP level had an increasing trend until 4 days after the beginning of treatment; however, from the 4th day onward, it had a decreasing trend but it was high until the end of the 10th day. PCT serum level was higher than normal in all patients before the treatment and then it had a decreasing trend after the beginning of therapy; however, the level of this marker was still high after 10 days of beginning the treatment. Moreover, the mean of the mentioned markers had a meaningful difference before the beginning of antibiotic therapy to the end of it according to variance analysis test with repetition of observations (P < 0.001). The PCT-CRP ratio reached its highest value in the fourth 48 h, and then it decreased.
It is worth noting that SOFA index had a meaningful decreasing trend compared to the entrance to ICU (P < 0.001).
Table 1 shows the mean and standard deviation of CRP and PCT serum levels and SOFA score index from the beginning of antibiotic therapy until 10 days after it.
Table 1.
Mean and SD of CRP serum level, PCT, PCT-CRP ratio, and SOFA
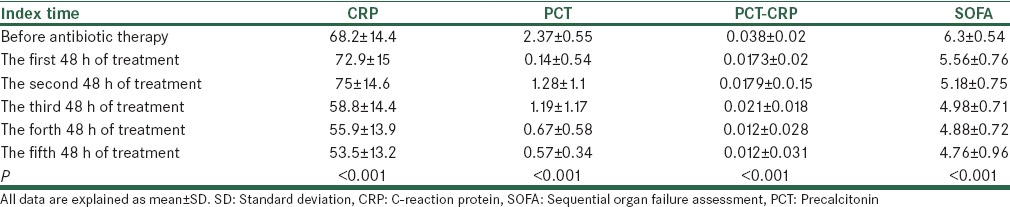
In Figures 1–4, the variation trend of mentioned parameters is presented.
Figure 1.
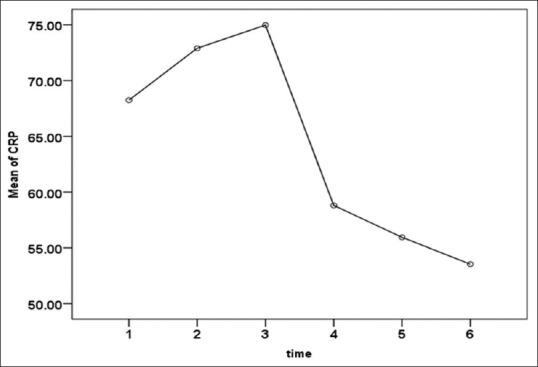
C-reactive protein serum level before antibiotic treatment until the 10th day
Figure 4.
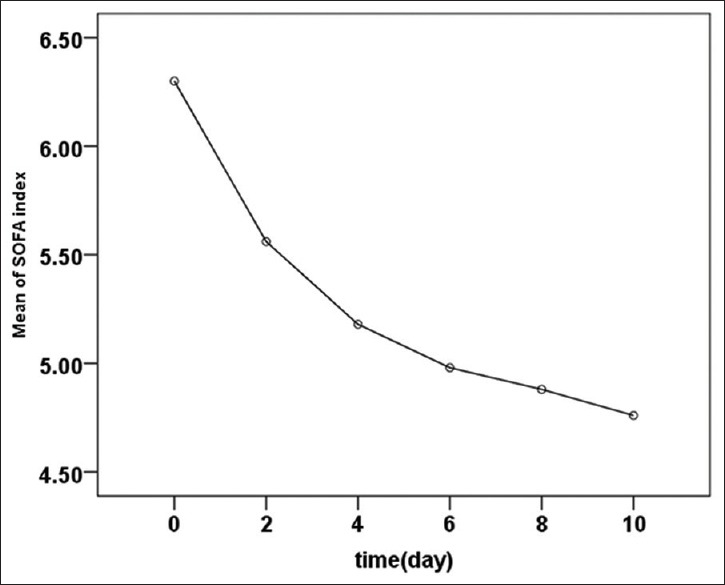
Sequential organ failure assessment index mean from the beginning of antibiotic therapy to the 10th day
Figure 2.
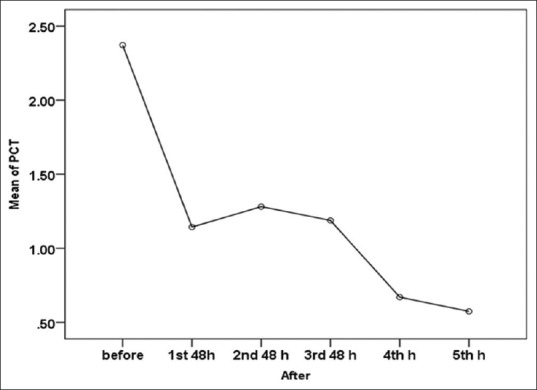
Precalcitonin serum level before the beginning of antibiotic therapy until the 10th day
Figure 3.
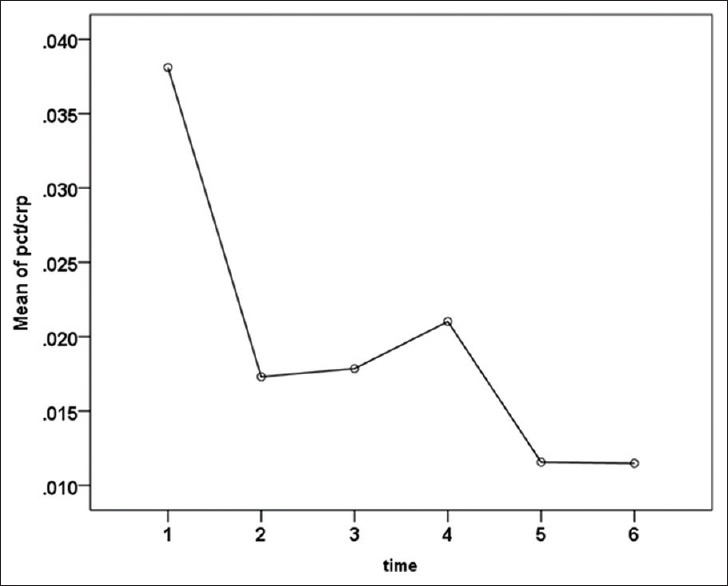
Precalcitonin and C-reactive protein ratio before antibiotic treatment until the 10th day
During the study, 4 individuals (8%) did not respond to antibiotic therapy. In Table 2, demographic and clinical characteristics of expired and treated patients are shown. According to this table, the duration of connection to ventilator was significantly higher in expired (after the first 48 h of hospitalization) group than the treated group (P = 0.029) and other variables had not meaningful difference between the two groups (P > 0.05). In Figures 5 and 6, the variation of serum levels of CRP and PCT in live and expired groups has been shown from the beginning of antibiotic therapy to the 10th day. According to repeated-measures ANOVA, the mean variation of CRP in two groups had a meaningful difference (P = 0.048); however, the variation of PCT in the two groups was not different (P = 0.18).
Table 2.
Frequency distribution of demographic and clinical specification of died and treated patients
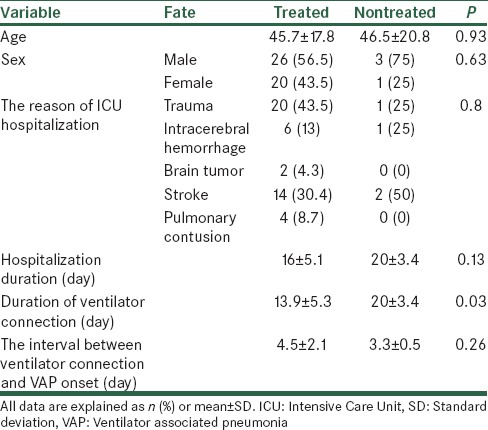
Figure 5.
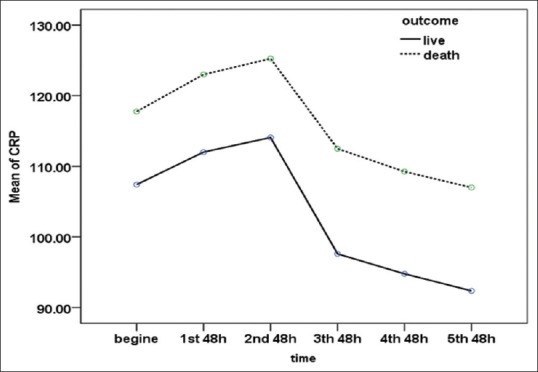
Mean of C-reactive protein serum level from beginning of therapy until the 10th day in treated and died groups (P = 0.046)
Figure 6.
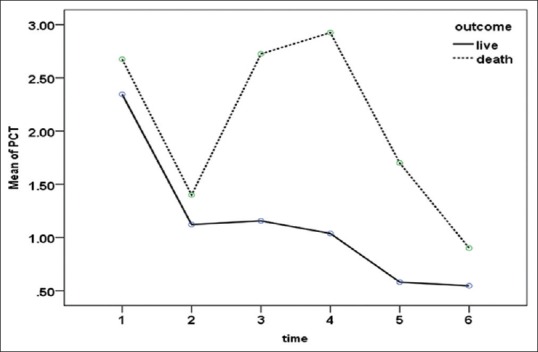
Mean of precalcitonin serum level from beginning of therapy until the 10th day in treated and died groups (P = 0.18)
DISCUSSION
The aim of this study is to determine PCT and CRP variations as a marker in responding to antibiotic therapy in patients suffering from VAP hospitalized in ICU.
According to our study, mean hospitalization time was 16 ± 5.1 days. In Saberi's study in Shahid Beheshti Kashani Hospital, the average hospitalization duration in ICU was 16.3 ± 5 days and the mean duration of connection to ventilator was 14.4 ± 5.4 days and the mean time interval between entrance to ICU to suffering from VAP was 4.36 ± 2.03 days.[11] In Zadeh et al.'s study in Sanandaj, the average hospitalization duration in patients suffering from VAP was 23.4 ± 10.2 days that was higher than that of ours.[12]
CRP serum level has been reported as a sensitive index in the evaluation of anti-bacterial trial treatment and follow-up of bacterial infection and control of postsurgical infections.[9] Thus, meaningful changes in CRP compared to disease condition can effectively show improvement and efficiency of the treatment. Concerning PCT, as previously mentioned, this index can be used in diagnosis, prognosis, and effect of antibiotic therapy in acute diseases.[8]
In Hillas et al. study on 45 patients suffering from VAP, serum levels of CRP and PCT were significantly higher than those of survived individuals. This study concluded that the mentioned markers can acceptably determine VAP prognosis in patients hospitalized in ICU.[8]
In Póvoa et al. study, the CRP serum level in patients suffering from VAP was higher than normal value after until 4 days of the beginning of antibiotic therapy; however, the CRP level in died individuals and treated people had not meaningful difference with VAP. In this study, a daily measurement of CRP level for determining the effect of antibiotic therapy has been evaluated as a beneficial marker.[13]
Thus, concerning the obtained results of this study and its comparison with other studies, the overall conclusion of this study is that CRP and PCT serum levels in patients suffering from VAP were high; however, by beginning of antibiotic treatment and its continuance, their levels gradually decreases. Thus, these two markers can be used as an instrument for determining the effect of antibiotic therapy in VAP patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ghazvini K, Ghanaat J, Jafarian MM, Yazdan Panah M, Irani N. Incidence of nosocomial pneumonia and bacterial agents causing this infection in intensive care unit in Qaem university hospital in Mashhad. J Ilam Univ Med Sci. 2005;13:55–61. [Google Scholar]
- 2.Nassaji M, Mousavi SH, Ghorbani R. Incidences of nosocomial pneumonia in patients above 15 years in intensive care units of university hospital in Semnan. Koomesh J Semnan Univ Med Sci. 2003;2:87–92. [Google Scholar]
- 3.Joseph NM, Sistla S, Dutta TK, Badhe AS, Parija SC. Ventilator-associated pneumonia in a tertiary care hospital in India: Incidence and risk factors. J Infect Dev Ctries. 2009;3:771–7. doi: 10.3855/jidc.396. [DOI] [PubMed] [Google Scholar]
- 4.Gopal Katherason S, Naing L, Jaalam K, Imran Musa K, Nik Mohamad NA, Aiyar S, et al. Ventilator-associated nosocomial pneumonia in intensive care units in Malaysia. J Infect Dev Ctries. 2009;3:704–10. doi: 10.3855/jidc.115. [DOI] [PubMed] [Google Scholar]
- 5.Apostolopoulou E, Bakakos P, Katostaras T, Gregorakos L. Incidence and risk factors for ventilator-associated pneumonia in 4 multidisciplinary intensive care units in Athens, Greece. Respir Care. 2003;48:681–8. [PubMed] [Google Scholar]
- 6.da Silva JM, Jr, Rezende E, Guimarães T, dos Campos EV, Magno LA, Consorti L, et al. Epidemiological and microbiological analysis of ventilator-associated pneumonia patients in a public teaching hospital. Braz J Infect Dis. 2007;11:482–8. doi: 10.1590/s1413-86702007000500009. [DOI] [PubMed] [Google Scholar]
- 7.Sadeghi M, Asghazadeh SA, Baratlu AR, Montazeri M. Antibiotic resistance pattern of gram negative bacillus isolated from respiratory culture in Intensive Care Unit's patients of Yahyanejad hospital. J Infect Dis Trop Med. 2009;14:39–43. [Google Scholar]
- 8.Hillas G, Vassilakopoulos T, Plantza P, Rasidakis A, Bakakos P. C-reactive protein and procalcitonin as predictors of survival and septic shock in ventilator-associated pneumonia. Eur Respir J. 2010;35:805–11. doi: 10.1183/09031936.00051309. [DOI] [PubMed] [Google Scholar]
- 9.Ramirez P, Garcia MA, Ferrer M, Aznar J, Valencia M, Sahuquillo JM, et al. Sequential measurements of procalcitonin levels in diagnosing ventilator-associated pneumonia. Eur Respir J. 2008;31:356–62. doi: 10.1183/09031936.00086707. [DOI] [PubMed] [Google Scholar]
- 10.Luyt CE, Guérin V, Combes A, Trouillet JL, Ayed SB, Bernard M, et al. Procalcitonin kinetics as a prognostic marker of ventilator-associated pneumonia. Am J Respir Crit Care Med. 2005;171:48–53. doi: 10.1164/rccm.200406-746OC. [DOI] [PubMed] [Google Scholar]
- 11.Saberi M, Shiri H, Moradians V, Taqadosi M. The investigation of the frequency of risk factors of early ventilator-associated pneumonia in ICU of Shahid Beheshti Hospital during 2009- 2010. J Feiz Sci Res. 2012;16:560–9. [Google Scholar]
- 12.Zadeh AA, Pour FL, Delpisheh A, Janmardi R. The investigation of the incidence of ventilator associated pneumonia and its bacterial resistance in ICU for adults hospitalized in Besat hospital of Sanandaj. J Med Sci Kurdistan. 2011;16:20–206. [Google Scholar]
- 13.Póvoa P, Coelho L, Almeida E, Fernandes A, Mealha R, Moreira P, et al. C-reactive protein as a marker of ventilator-associated pneumonia resolution: A pilot study. Eur Respir J. 2005;25:804–12. doi: 10.1183/09031936.05.00071704. [DOI] [PubMed] [Google Scholar]


