GESTATIONAL DIABETES IN INDIA
Diabetes is a major public health problem in India with prevalence rates reported to be between 4.6% and 14% in urban areas, and 1.7% and 13.2% in rural areas.[1] India has an estimated 62 million people with Type 2 diabetes mellitus (DM); this number is expected to go up to 79.4 million by 2025.[1] Management of diabetes and its complications imposes a huge economic burden on the society; hence effective strategies are urgently needed to control this epidemic. Not surprisingly, in parallel with the increase in diabetes prevalence, there seems to be an increasing prevalence of gestational DM (GDM), that is, diabetes diagnosed during pregnancy. The prevalence of gestational diabetes has been reported to range from 3.8% in Kashmir,[2] to 6.2% in Mysore,[3] 9.5% in Western India[4] and 17.9% in Tamil Nadu.[5] In more recent studies, using different criteria, prevalence rates as high as 35% from Punjab[6] and 41% from Lucknow have been reported.[7] The geographical differences in prevalence have been attributed to differences in age and/or socioeconomic status of pregnant women in these regions. It is estimated that about 4 million women are affected by GDM in India, at any given time point.[8]
Impact of gestational diabetes mellitus
Why should we be concerned about GDM? GDM not only influences immediate maternal (preeclampsia, stillbirths, macrosomia, and need for cesarean section) and neonatal outcomes (hypoglycemia, respiratory distress), but also increases the risk of future Type 2 diabetes in mother as well as the baby. A recent meta-analysis showed that women with gestational diabetes have a greatly increased risk of developing Type 2 diabetes (relative risk 7.43, 95% confidence interval 4.79–11.51).[9] In a recent study from North India, women diagnosed to have GDM were subjected to an oral glucose tolerance test (OGTT) 6 weeks after delivery, as per standard recommendations. A disturbingly large proportion of GDM women had some persistent glucose abnormality after birth. Impaired fasting glucose (IFG) was seen in 14.5% and impaired glucose tolerance (IGT) in 4.8%, 8% had both IFG and IGT, and 6.4% had overt Type 2 diabetes.[10] These figures are a wake-up call to place GDM at the highest priority in our public health system. Global data show that children of mothers with uncontrolled diabetes – either preexisting or originating during pregnancy – are four to eight times more likely to develop diabetes in later life compared to their siblings born to the same parents in a non-GDM pregnancy.[11]
Intervention in gestational diabetes mellitus
Can we do something to improve outcomes in GDM? It is well-established that treatment of GDM reduces the risk of serious perinatal complications.[12] In addition, clinical trials now provide evidence for the impact of multiple interventions in preventing the progression to Type 2 diabetes in women with a history of GDM. Both lifestyle modification and pharmacological therapies have been shown to reduce diabetes development by 50% or more.[13,14,15] Breastfeeding can also reduce childhood obesity.[16]
SETTING STANDARDS: DEFINING DISEASE
Despite the widespread agreement among experts about the importance of diagnosing and treating GDM, the degree of glucose intolerance severe enough to warrant treatment in a pregnant woman is fraught with controversies worldwide. Leading international associations have recommended different criteria [Table 1]. The landmark trial hyperglycemia in pregnancy and adverse outcomes (HAPO) highlighted the continuous nature of the association between hyperglycemia and adverse fetal outcomes.[17] Hence, attempts to search for a dichotomous cut-off are a trade-off between creating an “epidemic” of GDM and optimizing or “rationing” resources especially in resource-constrained settings like India. The International Association of Diabetes and Pregnancy Study Groups (IADPSG) decided that a consensus would be required to translate the results of HAPO study into clinical practice.[18] The IADPSG consensus panel decided to use mean values of fasting, 1 h and 2 h blood glucose of all pregnant females as reference and chose to use odds ratio of 1.75 to define the diagnostic cut-offs for GDM, which led to the development of the widely used and accepted IADPSG criteria.
Table 1.
Definition of GDM by different criteria
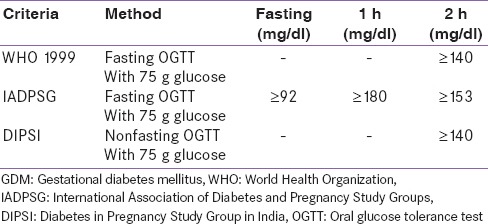
In India, pioneering work by Seshiah et al. lead to the adoption of Diabetes in Pregnancy Study Group in India (DIPSI) criteria as the norm to diagnose GDM, especially in the community setting, although these criteria were never fully adopted in specialty clinics. The DIPSI recommends a nonfasting OGTT [Table 1] based on the belief that fasting OGTT would be logistically difficult in pregnant women in the community as it required them to return to the clinic on a separate day.[19] The need for a simple screening test for GDM, is undoubtedly important, considering its relevance for the population at large. The evidence base of the DIPSI criteria is a single-center study comparing nonfasting OGTT with World Health Organization (WHO) 1999 criteria, showing 100% sensitivity and specificity.[5]
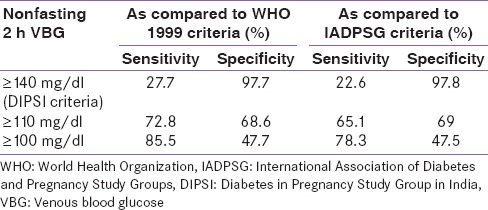
Recent studies have questioned the universal validity of DIPSI criteria. Mohan et al. compared DIPSI criteria with WHO criteria and IADPSG.[20] Definitions of GDM used in the study are shown in Table 1. The sensitivity of DIPSI criteria as compared to WHO 1999 and IADPSG criteria was very low [Table 2], and using nonfasting 2 h venous blood glucose more than 70% women with GDM would be misclassified as normal. The sensitivity improved on lowering the cut-offs, but the specificity would be lowered leading to several false positive anxious pregnant women. Another recent hospital-based study from New Delhi showed that using DIPSI criteria 22.36% women less were diagnosed with GDM than if IADPSG criteria were used.[21] The authors recommend using IADPSG criteria since the DIPSI criteria would miss a substantial number of patients.
Table 2.
Sensitivity and specificity of DIPSI criteria as compared to WHO and IADPSG
The aforementioned studies emphasize the fact that prevalence data on GDM is profoundly influenced by the criteria used for the diagnosis. It is, therefore, crucial to define “when to treat” not just for clinic based practice, but even more so for facilitating public health policy. This is only possible by conducting a large outcome based study involving multiple centers across India.
PRAGMATIC OVERVIEW
Regardless of the criteria used, it is clear that India has a very high prevalence of GDM by global standards. Conversion rates to frank Type 2 diabetes are also very high. Healthcare resources are insufficient. There is inadequate awareness among public. This results in a large population being hesitant to access healthcare system for diseases with not so “obvious” implications like GDM.
Interventions during and immediately after pregnancy provide important opportunities to improve the lives of mothers and children today and reducing diabetes in future generations. Screening and appropriate management of diabetes during pregnancy provides a unique opportunity to prevent Type 2 diabetes in two generations. Lack of awareness in society is one of the reasons that GDM is given low priority in public health delivery system in India.
PUBLIC AWARENESS: FROM WORDS TO ACTION
The need to generate awareness about GDM in society was addressed in a campaign initiated by Jagran Pehel (a social initiative by Jagran Prakashan Limited) and supported by the World Diabetes Foundation.[22] The Medanta Endocrinology and Diabetes Division was involved as the technical partner in this project. Entitled “A Multi-Media Campaign for Awareness Generation Management of Gestational Diabetes in Selected Districts in India,” the first phase of the campaign was run in 2010–2012. Launched by the then Union Health Minister, the campaign used the slogan “one test can save two lives” and sensitized more than a 100,000 adolescent girls regarding GDM through school and college based interventions across four states (http://www.worlddiabetesfoundation.org/projects/uttar-pradesh-punjab-jharkhand-and-delhi-india-wdf10-500).
This was followed by an advocacy cum capacity building project entitled “follow-up project on GDM mainstreaming in Public Health Delivery System in India” in 2012–2013. Advocacy workshops were conducted to sensitize various stakeholders including representatives from the government, government doctors, nurses and representatives from civil societies, corporate and media houses on the prevailing problem of GDM. A series of training of trainers workshops were organized where medical officers from various districts were oriented to simplified, practical guidelines on GDM. These medical officers in turn were sensitized to percolate the information to front-line workers in the public health system in a cascading manner. Handouts and training material were provided to each of these master trainers for this purpose. Furthermore, sensitization workshops were undertaken directly with the frontline health care workers in each of the districts in the four states (Bihar, Jharkhand, New Delhi and Punjab). A total of 231 doctors were trained as master trainers, and the information dissemination kit reached and sensitized 31,935 Auxiliary Nurse Midwives and 142,852 accredited social health activist workers. (http://www.jagranpehel.com/ContentPages/Events/EventsDetailsnew.aspx?newsId = 127). The impact of the project was assessed and report released in July 2015 by the incumbent Health Minister.
Efforts such as the Jagran Pehel project are much needed – their ultimate success is the translation into policy. Some policy changes that can be attributed to the Jagran campaign are that the state governments of New Delhi[23] and Punjab announced that screening for diabetes in pregnant women would become mandatory in their respective states. The government of Bihar (a nonproject state that was part of the earlier diabetes initiative) has made GDM screening mandatory in its public health facilities[24] and should be seen as a multiplier effect.
CONCLUSION
Much needs to be done to deal with the epidemic of GDM and Type 2 diabetes in India. There is a need for studying outcomes as well as cost-effectiveness of different diagnostic criteria while simultaneously creating social awareness, training manpower, and sensitizing policymakers to make GDM testing and management mandatory during pregnancy. It is hoped that the various initiatives being launched in this area, including the latest ones with the South Asian Federation of Endocrine Societies,[25] will help clarify and address this major public health problem.
REFERENCES
- 1.Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, et al. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: Phase I results of the Indian Council of Medical Research-INdia DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54:3022–7. doi: 10.1007/s00125-011-2291-5. [DOI] [PubMed] [Google Scholar]
- 2.Raja MW, Baba TA, Hanga AJ, Bilquees S, Rasheed, Haq IU, et al. A study to estimate the prevalence of gestational diabetes mellites in an urban block of Kashmir valley (North India) Int J Med Sci Public Health. 2014;3:191–5. [Google Scholar]
- 3.Swami SR, Mehetre R, Shivane V, Bandgar TR, Menon PS, Shah NS. Prevalence of carbohydrate intolerance of varying degrees in pregnant females in western India (Maharashtra) – A hospital-based study. J Indian Med Assoc. 2008;106:712–4, 735. [PubMed] [Google Scholar]
- 4.Bhatt AA, Dhore PB, Purandare VB, Sayyad MG, Mandal MK, Unnikrishnan AG. Gestational diabetes mellitus in rural population of Western India-Results of a community survey. Indian J Endocrinol Metab. 2015;19:507–10. doi: 10.4103/2230-8210.159061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seshiah V, Balaji V, Balaji MS, Sanjeevi CB, Green A. Gestational diabetes mellitus in India. J Assoc Physicians India. 2004;52:707–11. [PubMed] [Google Scholar]
- 6.Arora GP, Thaman RG, Prasad RB, Almgren P, Brøns C, Groop LC, et al. Prevalence and risk factors of gestational diabetes in Punjab, North India: Results from a population screening program. Eur J Endocrinol. 2015;173:257–67. doi: 10.1530/EJE-14-0428. [DOI] [PubMed] [Google Scholar]
- 7.Gopalakrishnan V, Singh R, Pradeep Y, Kapoor D, Rani AK, Pradhan S, et al. Evaluation of the prevalence of gestational diabetes mellitus in North Indians using the International Association of Diabetes and Pregnancy Study groups (IADPSG) criteria. J Postgrad Med. 2015;61:155–8. doi: 10.4103/0022-3859.159306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kayal A, Anjana RM, Mohan V. Gestational diabetes-An update from India, 2013. Diabetes Voice 58, 2013. [Last accessed on 2015 Aug 15]. Available from: http://www.idf.org/gestational.diabetes .
- 9.Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: A systematic review and meta-analysis. Lancet. 2009;373:1773–9. doi: 10.1016/S0140-6736(09)60731-5. [DOI] [PubMed] [Google Scholar]
- 10.Jindal R, Siddiqui MA, Gupta N, Wangnoo SK. Prevalence of glucose intolerance at 6 weeks postpartum in Indian women with gestational diabetes mellitus. Diabetes Metab Syndr. 2015;9:143–6. doi: 10.1016/j.dsx.2015.04.016. [DOI] [PubMed] [Google Scholar]
- 11.Damm P. Future risk of diabetes in mother and child after gestational diabetes mellitus. Int J Gynaecol Obstet. 2009;104:S25–6. doi: 10.1016/j.ijgo.2008.11.025. [DOI] [PubMed] [Google Scholar]
- 12.Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, Robinson JS. Australian Carbohydrate Intolerance Study in Pregnant Women (ACHOIS) Trial Group. Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med. 2005;352:2477–86. doi: 10.1056/NEJMoa042973. [DOI] [PubMed] [Google Scholar]
- 13.Ratner RE, Christophi CA, Metzger BE, Dabelea D, Bennett PH, Pi-Sunyer X, et al. Prevention of diabetes in women with a history of gestational diabetes: Effects of metformin and lifestyle interventions. J Clin Endocrinol Metab. 2008;93:4774–9. doi: 10.1210/jc.2008-0772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Azen SP, Peters RK, Berkowitz K, Kjos S, Xiang A, Buchanan TA. TRIPOD (TRoglitazone In the Prevention Of Diabetes): A randomized, placebo-controlled trial of troglitazone in women with prior gestational diabetes mellitus. Control Clin Trials. 1998;19:217–31. doi: 10.1016/s0197-2456(97)00151-7. [DOI] [PubMed] [Google Scholar]
- 15.Xiang AH, Peters RK, Kjos SL, Marroquin A, Goico J, Ochoa C, et al. Effect of pioglitazone on pancreatic beta-cell function and diabetes risk in Hispanic women with prior gestational diabetes. Diabetes. 2006;55:517–22. doi: 10.2337/diabetes.55.02.06.db05-1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gunderson EP. Breastfeeding after gestational diabetes pregnancy: Subsequent obesity and type 2 diabetes in women and their offspring. Diabetes Care. 2007;30:S161–8. doi: 10.2337/dc07-s210. [DOI] [PubMed] [Google Scholar]
- 17.Catalano PM, McIntyre HD, Cruickshank JK, McCance DR, Dyer AR, Metzger BE, et al. The hyperglycemia and adverse pregnancy outcome study: Associations of GDM and obesity with pregnancy outcomes. Diabetes Care. 2012;35:780–6. doi: 10.2337/dc11-1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.International Association of Diabetes and Pregnancy Study Groups Consensus Panel. Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA, et al. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33:676–82. doi: 10.2337/dc09-1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Seshiah V, Das AK, Balaji V, Joshi SR, Parikh MN, Gupta S. Diabetes in Pregnancy Study Group. Gestational diabetes mellitus – Guidelines. J Assoc Physicians India. 2006;54:622–8. [PubMed] [Google Scholar]
- 20.Mohan V, Mahalakshmi MM, Bhavadharini B, Maheswari K, Kalaiyarasi G, Anjana RM, et al. Comparison of screening for gestational diabetes mellitus by oral glucose tolerance tests done in the non-fasting (random) and fasting states. Acta Diabetol. 2014;51:1007–13. doi: 10.1007/s00592-014-0660-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pulkit Vij, Sujeet Jha SK, Gupta, Aneja Anjila, Mathur Rajani, Waghdhare Swati, et al. Comparison of DIPSI and IADPSG criteria for diagnosis of GDM: A study in a North Indian tertiary care center. Int J Diabetes Dev Ctries. 2015:1–4. [Google Scholar]
- 22.Madhab A, Prasad VM, Kapur A. Gestational diabetes mellitus: Advocating for policy change in India. Int J Gynaecol Obstet. 2011;115:S41–4. doi: 10.1016/S0020-7292(11)60012-X. [DOI] [PubMed] [Google Scholar]
- 23.Diabetes test a must for pregnant women in Delhi. iGovernment. 2011. Jan 10, [Last accessed on 2015 Aug 15]. Available from: http://www.igovernment.in/site/diabetes-test-must-pregnant-women-delhi-39065 .
- 24.Private firm to help state fight diabetes. The Telegraph, C., India. 2011. Mar 9, [Last accessed on 2015 Aug 15]. Available from: http://www.telegraphindia.com/1110309/jsp/bihar/story_13684554.jsp .
- 25.Mahtab H, Pathan MF, Ahmed T, Bajaj S, Sahay R, Raza SA, et al. The dhaka declaration 2015. Indian J Endocrinol Metab. 2015;19:441–2. doi: 10.4103/2230-8210.159014. [DOI] [PMC free article] [PubMed] [Google Scholar]


