Abstract
Introduction:
Approximately, 33% patients with diabetes are afflicted with onychomycosis. In the past, nondermatophyte molds have been regarded as opportunistic pathogens; recently, Aspergillus species are considered as emerging pathogens of toenail infections. In Sri Lanka, the prevalence of Aspergillus species in onychomycosis among diabetics is not well documented.
Objective:
To determine the proportion of Aspergillus onychomycosis, risk factors and knowledge among diabetics.
Materials and Methods:
This was descriptive cross-sectional study. Three hundred diabetic patients were included. Clinical examinations of patients’ toenails were performed by a clinical microbiologist. Laboratory identification was done, and pathogens were identified to the species level by morpho-physiological methods. All inferential statistics were tested at P < 0.05.
Results:
Among clinically suspected patients, 85% (255/300) were mycologically confirmed to have onychomycosis. Aspergillus species were most commonly isolated n = 180 (71%) followed by dermatophytes, yeasts, and other molds n = 75 (29%). Of the patients having Aspergillus onychomycosis, 149 (83%) were in the > age group. In men, Aspergillus onycomycosis was seen in 82%. Among patients who had Aspergillus nail infection, 114 (63%) had diabetes for a period of > years. Among patients who were engaged in agricultural activities, 77% were confirmed to have infected nails due to Aspergillus species.
Conclusion:
Aspergillus niger was the most common pathogen isolated from toenail infection. Aspergillus species should be considered as an important pathogen in toenail onychomycosis in diabetic patients. Risk factors associated with Aspergillus onychomycosis were age, gender, duration of diabetes, length of exposure to fungi, and occupation.
Keywords: Aspergillus species, diabetics, onychomycosis, Sri Lanka
INTRODUCTION
Onychomycosis accounts for about a half of all nail abnormalities.[1] Approximately, 33% patients with diabetes are afflicted with onychomycosis.[2] The predisposing factors are age, gender, duration of diabetes, time of exposure, and altered host immune response.[3,4,5,6] Recently, Aspergillus species were considered as emerging pathogens of toenail infections.[7,8,9,10] The proportion of Aspergillus infection in onychomycosis has been reported as 50–60%.[11,12] In Sri Lanka, the prevalence of Aspergillus species in onychomycosis among diabetics is not well documented; therefore, we investigated the proportion of Aspergillus onychomycosis, risk factors and knowledge among diabetic patients presenting to a tertiary care hospital.
MATERIALS AND METHODS
Study design
A descriptive cross-sectional study conducted at the Diabetic Clinic at Colombo South Teaching Hospital.
Ethics
Ethical approval for the study was granted by the Ethical Committee of Colombo South Teaching Hospital (228) and University of Sri Jayewardenepura (02) Sri Lanka.
Three hundred diabetic patients attending the diabetic clinic were included in the study after obtaining their informed written consent. After taking a thorough history and demographic details, patients were asked questions on knowledge on onychomycosis, about the causative agents, risk factors, and preventive measures. Clinical examinations of patients’ toenails for onychomycosis were performed by a clinical microbiologist. Different nail abnormalities such as nail thickening, brittle nails, pitting of nails, cracking of nails, and any visible change in color of nail plate were recorded. Samples of affected toenails were collected after cleaning with 70% ethyl alcohol using sterile scissors or nail-cutters. The nail clippings were collected to black papers (5” ×5”) to form of flat packets and transported to the laboratory.
The nail clippings placed on a pre-labeled clean glass slides were immersed in a drop of 20% potassium hydroxide (KOH) and incubated at 37°C for 10–15 min. In addition, thick nail clippings processed as above were kept in humidified petri dishes overnight at room temperature. The slides were examined under a microscope. The nail samples were inoculated on quality controlled Sabouraud's dextrose agar (Oxoid, UK), with and without antimicrobials (chloramphenicol [0.05 g/l], and cycloheximide [100 mg/l]). The inoculated specimens were incubated at 25–30°C aerobically for up to 3 weeks and examined for any growth regularly. Identification of the fungi was done by examining colony morphology and microscopic examination of lactophenol blue preparation. The slides were examined for the presence of characteristic hyphae, macroconidia, and microconidia.
Statistics
Data were analyzed using SPSS version 16 (Chicago; SPSS Inc.). All inferential statistics were tested at P < 0.05. Frequency tables and cross tables were obtained to achieve the objectives of the study.
RESULTS
Three hundred diabetic patients with clinically suspected onychomycosis, comprising 92 men (31%) and 208 women (69%), aged 30–90 (mean age, 58.3) years were included in the study. Among these patients with toenail onychomycosis, 50 (16.7%) showed involvement of the first toenail alone, 80 (27%) showed involvement of two toenails and 170 (57%) showed involvement of multiple toenails.
Among clinically suspected patients, 255 patients (255/300, 85%) were mycologically confirmed to have onychomycosis: 85 men (age range 30–90 years, mean 60.05, median 61, standard deviation [SD] 11.82) and 170 women (age range 30–84 years, mean 58.05, median 58.5, SD 11.00). Male/female ratio is 1:2. All the patients with mycologically confirmed onychomycosis had type II diabetes mellitus.
Of the 255 patients with confirmed onychomycosis, culture positivity alone was seen in 28 (11%) cases, both culture and KOH positivity was seen in 226 (88.9%) cases. Aspergillus onychomycosis was confirmed after obtaining positive results from both KOH and culture. Of the fungal pathogens isolated from the mycological investigations, Aspergillus species were most commonly isolated (n = 180 [71%]). Among Aspergillus species, Aspergillus niger (76%) was predominant [Tables 1 and 2].
Table 1.
The spectrum of Aspergillus species isolated from toenails

Table 2.
Aspergillus species isolated from the toenails
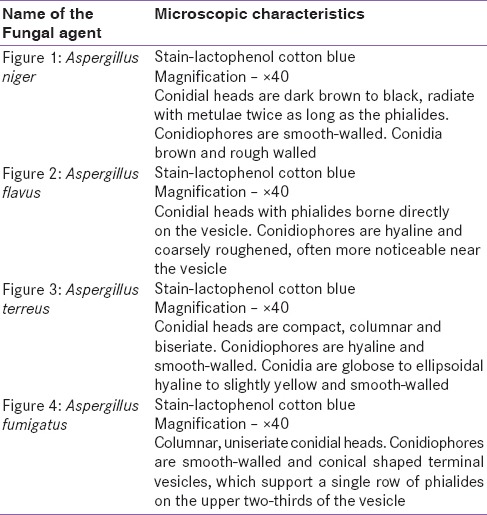
Figure 1.

Aspergillus niger
Figure 2.
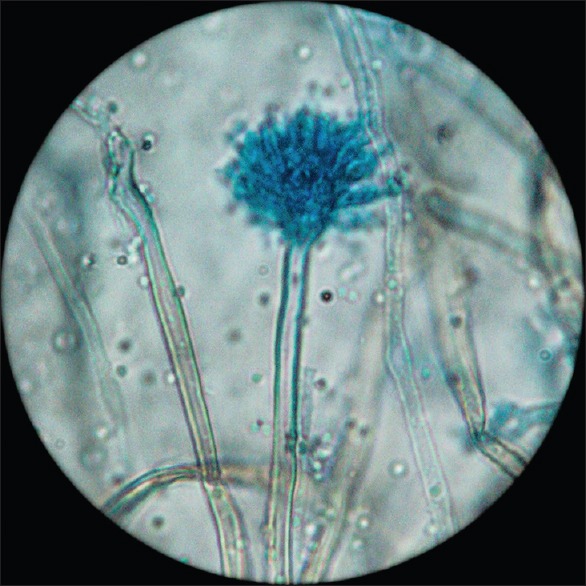
Aspergillus flavus
Figure 3.
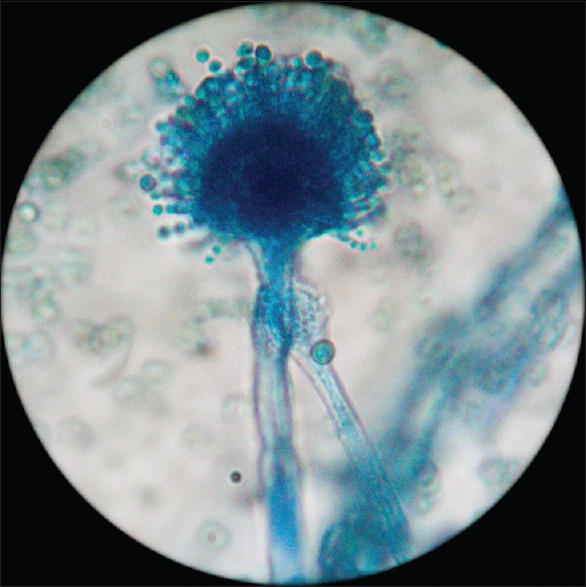
Aspergillus terreus
Figure 4.
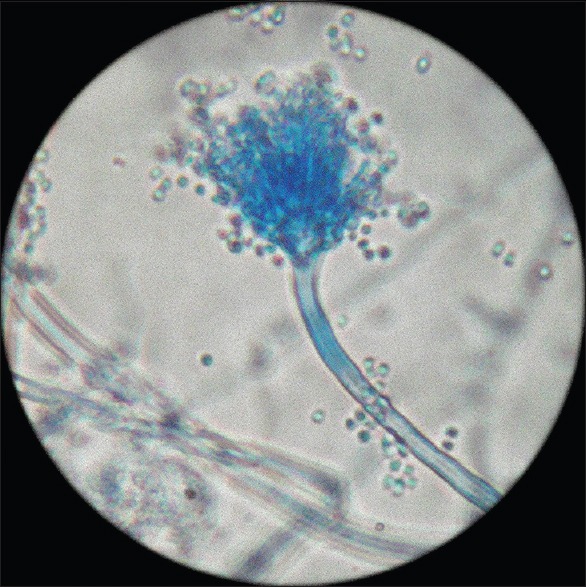
Aspergillus fumigatus
Among the women with onychomycosis, 65% and 35% cases were due to Aspergillus species and other fungal species, respectively, whereas in men 82% of onycomycosis was caused by Aspergillus species. Infection with Aspergillus species was found to correlate significantly with the male gender (P = 0.004).
Of the patients having Aspergillus onychomycosis, 149 (83%) were in the > age group. The occurrence of Aspergillus species in toenail infections was statistically significant with the increasing age (P = 0.014) and with the duration of diabetes (P < 0.05). Among patients who had Aspergillus nail infection, 66 (37%) had diabetes for a period of <15 years, and 114 (63%) had diabetes for a period of > years. There was no statistical significance with the occurrence of Aspergillus species in toenails with the family history of onychomycosis.
With regard to occupation, 162 (63%) patients were engaged in agricultural activities, including farming and gardening. Among these 77% were confirmed to have infected nails due to Aspergillus species, (P = 0.006). The majority of patients (n = 180 [71%]) were using unchlorinated water supplies for daily bathing and washing. Among these 76% were confirmed to have Aspergillus species (P = 0.003).
Sixty (20%) of the clinically suspected patients were working in offices, wearing socks and shoes. Among them, 65% were confirmed to have onycomycosis due to Aspergillus species, and all of them had previous fungal infections as well. Hard and brittle nails were the two common clinical signs observed in patients with onychomycosis due to Aspergillus species [Figure 5].
Figure 5.
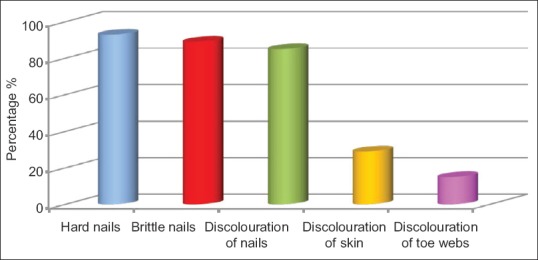
Characteristics of nails of patients confirmed to have Aspergillus onychomycosis
Among study population, only 36% of patients assumed they had an infection in their toenails. However, when the clinical toe examination was performed followed by the laboratory confirmation 85% (255/300) were found to be suffering from fungal toenail infection.
It is evident that the actual frequency of toenail infections was underestimated by the patients. Furthermore, it is clearly evident that the patients’ awareness about the pathogen which causes nail infection was very low among study population [Figure 6].
Figure 6.
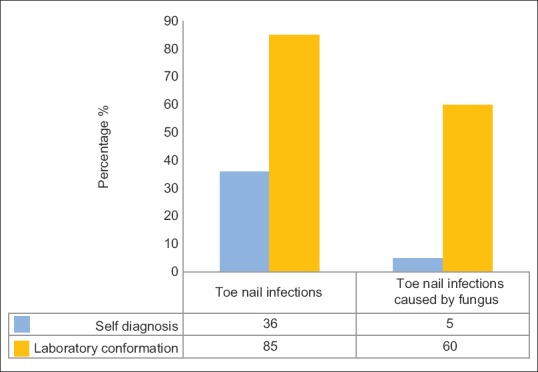
Response of volunteers regarding self-diagnosis of onychomycosis and comparison with laboratory-based mycological confirmation
DISCUSSION
Although it is reported that dermatophytes and yeasts are the most common cause for onycomycosis,[6,8] nondermatophyte molds (NDM) such as Aspergillus spp., Fusarium spp., Acremonium spp., and Scopulariopsis spp., were also found as the most common pathogens for onychomycosis in patients with diabetes.[2,5,13]
In our study, A. niger was found to be the most common (76%) cause for onycomycosis among the diabetes patients. In recent past, more than 50% of nail abnormalities are due to onychomycosis.[1] We report that 85% of diabetic patients had toenail infections, which is a significant finding when compared to the reported prevalence rates of 30–60%.[4,14] Our results were also in line with previous investigations[15,16] reporting that A. niger as the commonest cause of nail infection in diabetics.
Studies based on epidemiology have stated that Aspergillus species are emerging fungal agents of toenail onychomycosis.[9,10] Several other studies also have reported Aspergillus species as a primary cause of onychomycosis.[7,8]
Our findings of Aspergillus species as the true pathogen is consolidated as all the specimens which were positive for Aspergillus species were confirmed by both direct smear and culture positive results.
In contrast to our study, Gupta and Humke, Moreno and Arenas, have reported that Trichophyton spp., Microsporum spp. and Epidermophyton spp. were more common pathogens causing nail infections among diabetes patients.[6,8]
Even though the majority of the study population who were clinically suspected to have onychomycosis were females, the percentage of culture positive for Aspergillus species was higher in males and showed statistical significance. A global study by Sigurgeirsson and Baran in 2014 had further supported our finding.[17] Fata et al., reported that gender-related factors such as differences in lifestyle, professional activities, and sports activities can affect the nail structure of the foot.[18]
The occurrence of Aspergillus species in toenails was found to be statistically significant with the advancing age of the diabetic patients. Diabetic patients more than 50 years old are more susceptible to fungal infections in toenails due to diminished blood circulation, increased thickness of the nail plate, decreased the growth rate of the nail, and poor foot hygiene.[19]
Previous reports indicate that prolonged duration of diabetes mellitus, prolonged exposure to fungi and old age can predispose patients to onychomycosis because these patients provide a favorable environment for the growth of Aspergillus species. Therefore, early recognition and intervention is advisable because of the progressive nature of the infection.
In our study group having onychomycosis due to Aspergillus species, 93% were diagnosed with hard nails (pachyonychia), 89% with brittle nails and 85% had discolored nails. The presence of discolored skin on the feet and discolored toe webs were comparatively low than the nail deformities. This is mainly because Aspergillus species do not spread to the surrounding skin like other fungal species that cause nail infections.[20]Aspergillus onychomycosis starts at the tip of the underside of the nail, where spores get accumulated, and the infection spreads toward the cuticle and the nails become thick, discolored, and flaky.[19]
Certain factors such as barefoot walking, using open rubber slippers, low socioeconomic status, late presentation by patients, poor compliance with medical care, inadequate adherence to precautionary measures, and foot inspection contribute to this high prevalence of onychomycosis among diabetic population. Aspergillus species are a large group of common saprophytic molds which are often isolated from soil, air, and plant materials. Prolonged exposed to soil, mud, and water contaminated with fungi will increase the susceptibility of Aspergillus infection in toenails. In our study, more than half of the population was manual laborers working as farmers and gardeners’ in close contact with soil, mud, and water. The occurrence of Aspergillus infection was statistically significant with agricultural workers.
Interestingly, in our study population, only 20% were office workers, among them more than half were diagnosed with Aspergillus onychomycosis. Accumulation of sweat within a shoe: Especially when wearing socks, can generate a moist warm environment, that is, ideal for fungal growth. In 2010, Thomas et al. had reported an association between onychomycosis and the use of footwear.[21] Increased use of occlusive footwear that hinder ventilation and do not absorb perspiration may also contribute to higher incidence of onychomycosis in males.[18,22,23]
Aspergillus is normally considered as a common contaminant. Therefore, it is difficult to discern between the contaminant and the pathogen when Aspergillus spp. are identified in onychomycosis. However, according to English, in 1976, NDM can be considered as a pathogen of onychomycosis only when hyphae or spores are seen on direct microscopic examination, and the same strain is identified through cultures.[24] In our study, all the nail specimens which were confirmed to have Aspergillus showed positive direct smear as well as gave a comparable culture result.
Onychomycosis in people with diabetes increases the risk for other foot disorders and trigger for more severe complications such as foot ulcers, gangrene,[2] recurrent cellulitis, and limb amputation.[4]
The final outcome from not treating this condition can be worse in diabetics than in those without diabetes. Therefore, care should be taken for the accurate diagnosis and timely treatment of toenail onychomycosis to prevent complications.
CONCLUSION
A. niger was the most common pathogen isolated from toenail infection in this study conducted among diabetic population in Sri Lanka. Risk factors associated with Aspergillus onychomycosis were age, gender, duration of diabetes, length of exposure to fungi, and occupation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Acknowledgment
We would like to thank all the technical officers at the Department of Microbiology, University of Sri Jayewardenepura and the nursing staff at the Diabetic Clinic at Colombo South Teaching Tertiary Care Hospital, for their assistance.
REFERENCES
- 1.Leelavathi M, Noorlaily M. Onychomycosis nailed. Malays Fam Physician. 2014;9:2–7. [PMC free article] [PubMed] [Google Scholar]
- 2.Papini M, Cicoletti M, Fabrizi V, Landucci P. Skin and nail mycoses in patients with diabetic foot. G Ital Dermatol Venereol. 2013;148:603–8. [PubMed] [Google Scholar]
- 3.Mayser P, Freund V, Budihardja D. Toenail onychomycosis in diabetic patients: Issues and management. Am J Clin Dermatol. 2009;10:211–20. doi: 10.2165/00128071-200910040-00001. [DOI] [PubMed] [Google Scholar]
- 4.Cathcart S, Cantrell W, Elewski BE. Onychomycosis and diabetes. J Eur Acad Dermatol Venereol. 2009;23:1119–22. doi: 10.1111/j.1468-3083.2009.03225.x. [DOI] [PubMed] [Google Scholar]
- 5.Wijesuriya TM, Weerasekera MM, Kottahachchi J, Ranasinghe KN, Dissanayake MS, Prathapan S, et al. Proportion of lower limb fungal foot infections in patients with type 2 diabetes at a tertiary care hospital in Sri Lanka. Indian J Endocrinol Metab. 2014;18:63–9. doi: 10.4103/2230-8210.126556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta AK, Humke S. The prevalence and management of onychomycosis in diabetic patients. Eur J Dermatol. 2000;10:379–84. [PubMed] [Google Scholar]
- 7.Gupta AK, Drummond-Main C, Cooper EA, Brintnell W, Piraccini BM, Tosti A. Systematic review of nondermatophyte mold onychomycosis: Diagnosis, clinical types, epidemiology, and treatment. J Am Acad Dermatol. 2012;66:494–502. doi: 10.1016/j.jaad.2011.02.038. [DOI] [PubMed] [Google Scholar]
- 8.Moreno G, Arenas R. Other fungi causing onychomycosis. Clin Dermatol. 2010;28:160–3. doi: 10.1016/j.clindermatol.2009.12.009. [DOI] [PubMed] [Google Scholar]
- 9.Gianni C, Romano C. Clinical and histological aspects of toenail onychomycosis caused by Aspergillus spp.: 34 cases treated with weekly intermittent terbinafine. Dermatology. 2004;209:104–10. doi: 10.1159/000079593. [DOI] [PubMed] [Google Scholar]
- 10.Hilmioglu-Polat S, Metin DY, Inci R, Dereli T, Kilinç I, Tümbay E. Non-dermatophytic molds as agents of onychomycosis in Izmir, Turkey – A prospective study. Mycopathologia. 2005;160:125–8. doi: 10.1007/s11046-005-6872-z. [DOI] [PubMed] [Google Scholar]
- 11.Veer P, Patwardhan NS, Damle AS. Study of onychomycosis: Prevailing fungi and pattern of infection. Indian J Med Microbiol. 2007;25:53–6. doi: 10.4103/0255-0857.31063. [DOI] [PubMed] [Google Scholar]
- 12.Bassiri-Jahromi S, Khaksar AA. Nondermatophytic moulds as a causative agent of onychomycosis in tehran. Indian J Dermatol. 2010;55:140–3. doi: 10.4103/0019-5154.62743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Farwa U, Abbasi SA, Mirza IA, Amjad A, Ikram A, Malik N, et al. Non-dermatophyte moulds as pathogens of onychomycosis. J Coll Physicians Surg Pak. 2011;21:597–600. doi: 10.2011/JCPSP.597600. [DOI] [PubMed] [Google Scholar]
- 14.Nasreen S, Ahmed I, Jahangir MU. Cutaneous manifestations of diabetic foot. J Pak Assoc Dermatologists. 2009;19:13–7. [Google Scholar]
- 15.Nair S, Peter S, Sasidharan A, Sistla S, Unni AK. Incidence of mycotic infections in diabetic foot tissue. J Cult Collect. 2006-2007;5:85–9. [Google Scholar]
- 16.Eckhard M, Lengler A, Liersch J, Bretzel RG, Mayser P. Fungal foot infections in patients with diabetes mellitus – Results of two independent investigations. Mycoses. 2007;50(Suppl 2):14–9. doi: 10.1111/j.1439-0507.2007.01425.x. [DOI] [PubMed] [Google Scholar]
- 17.Sigurgeirsson B, Baran R. The prevalence of onychomycosis in the global population: A literature study. J Eur Acad Dermatol Venereol. 2014;28:1480–91. doi: 10.1111/jdv.12323. [DOI] [PubMed] [Google Scholar]
- 18.Fata S, Saeed-Modaghegh MH, Faizi R, Najafzadeh MJ, Afzalaghee M, Ghasemi M. Mycotic infections in diabetic foot ulcers in Emam Reza hospital, Mashhad, 2006-2008. Jundishapur J Microbiol. 2011;4:11–6. [Google Scholar]
- 19.Zaias N, Escovar SX, Rebell G. Opportunistic toenail onychomycosis. The fungal colonization of an available nail unit space by non-dermatophytes is produced by the trauma of the closed shoe by an asymmetric gait or other trauma. A plausible theory. J Eur Acad Dermatol Venereol. 2014;28:1002–6. doi: 10.1111/jdv.12458. [DOI] [PubMed] [Google Scholar]
- 20.Banu A, Anand M, Eswari L. A rare case of onychomycosis in all 10 fingers of an immunocompetent patient. Indian Dermatol Online J. 2013;4:302–4. doi: 10.4103/2229-5178.120649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thomas J, Jacobson GA, Narkowicz CK, Peterson GM, Burnet H, Sharpe C. Toenail onychomycosis: An important global disease burden. J Clin Pharm Ther. 2010;35:497–519. doi: 10.1111/j.1365-2710.2009.01107.x. [DOI] [PubMed] [Google Scholar]
- 22.Araujo AJ, Bastos OM, Souza MA, Oliveira JC. Occurrence of onychomycosis among patients attended in dermatology offices in the city of Rio de Janeiro, Brazil. An Bras Dermatol. 2003;78:299–308. [Google Scholar]
- 23.Kafaie P, Noorbala MT. Evaluation of onychomycosis among diabetic patients of Yazd diabetic center. J Pak Assoc Dermatologists. 2010;20:217–21. [Google Scholar]
- 24.English MP. Nails and fungi. Br J Dermatol. 1976;94:697–701. doi: 10.1111/j.1365-2133.1976.tb05171.x. [DOI] [PubMed] [Google Scholar]


