Abstract
Background: Caring for someone with multiple sclerosis (MS) can be a stressful experience that requires clinical attention. We investigated the impact of caregiver stress on the emotional well-being and physical health of the MS care partner using the North American Research Committee on Multiple Sclerosis (NARCOMS) Registry.
Methods: Care partners of NARCOMS participants were invited to complete an online questionnaire that captured demographic characteristics, health status, caregiver burden as measured by the Zarit Caregiver Burden Interview, and impact of caregiving on employment.
Results: Of 1446 care partners who agreed to participate, 1333 had complete data. Most were men (n = 825, 61.9%), with a mean (SD) age of 51.1 (11.2) years. The mean (SD) Zarit total score was 24.6 (15.1), placing the overall group in the mild caregiver burden range. Compared with male care partners, female care partners reported higher levels of burden and stress and more medication use for stress/anxiety and mood disorders. Male care partners were more likely to report physical concerns. Care partners of people with primary progressive MS reported greater perceived burden than did partners of people with secondary progressive MS and relapsing-remitting MS. More than 40% of care partners (559 of 1288) had missed work during the past year owing to caregiving responsibilities.
Conclusions: Care partners of people with MS have substantial physical and psychological health concerns and experience an adverse impact on employment. Future research should evaluate how to mitigate the adverse effects of caregiving and evaluate positive aspects of the role.
Multiple sclerosis (MS) is a progressively disabling chronic disease with peak onset between ages 20 and 40 years. MS care partners constitute a growing number of individuals who voluntarily provide care for loved ones without compensation. Compared with care partners for other chronic diseases, they are more likely to be husbands, young to middle aged, parents of young children, and in the early stages of their careers.1,2 Research evaluating populations caring for those with chronic illnesses has linked caregiving to negative effects on the care partner's relationships, social life, physical health, and overall psychological well-being.3,4 Caregiving often alters career paths, causing the care partner to substitute unpaid work for paid work.5,6 Higher care partner burden is associated with an increase in caregiving hours7 and a decreased ability to maintain paid employment.8
A meta-analysis analyzing differences in health effects between care partners and noncare partners found that care partners reported an overall poorer degree of health, took more medications, had a 23% higher rate of stress hormones, and had a 15% lower rate of immune responsivity.4 Chronic stress may produce adverse physiological and psychological outcomes, such as cardiovascular disease, hypertension, eating disorders, impaired physical functioning, cognitive decline, depression, anxiety, decreased quality of life, and even death.9–11
Sex may also influence perceived care partner burden and the effect on physical and psychological health. Exposure to chronic stress is central to the development of cardiovascular disease, and observed sex differences in cardiovascular disease may be due to differing abilities to recover quickly after exposure to stress.12 Several studies have shown an increased susceptibility to stroke and cardiovascular disease in male care partners13 but not in female care partners.9 In a study evaluating elderly adults caring for spouses with Alzheimer's disease,14 female care partners reported more psychosocial problems and health concerns, whereas male care partners actually had worse physiological risk but reported better overall physical health. Additional studies also consistently report that female care partners tend to endorse higher rates of conditions such as arthritis, whereas male care partners tend to have more hospitalizations for more serious and life-threatening conditions, such as cardiovascular disease.14
We aimed to investigate the effect of caregiver stress on the emotional well-being, physical health, and employment of the MS care partner using the North American Research Committee on Multiple Sclerosis (NARCOMS) Registry. We hypothesized that male care partners would report more physical health concerns than female care partners but good overall health.
Methods
Recruitment
NARCOMS is a project of the Consortium of Multiple Sclerosis Centers. Since 1996, NARCOMS has maintained a voluntary registry consisting of participants' self-reported data obtained at enrollment and via semiannual questionnaires. At the time of data collection in 2005, the registry had demographic and clinical data for more than 29,000 individuals. We contacted NARCOMS participants by e-mail, regardless of their level of disability or whether they had previously indicated having a care partner, and requested that they refer their care partner to participate in a study assessing the effects of caregiving. Care partners who agreed to participate provided their consent electronically and then anonymously completed an online questionnaire on a secure website separate from the NARCOMS database.
Measures
Care partners provided basic demographic information about themselves, including sex, age, years of education, and years of caregiving, as well as information about the patient for whom they provided care, including age, educational level, MS course (relapsing-remitting [RRMS], secondary progressive [SPMS], primary progressive [PPMS], or unsure), and years since diagnosis.
Survey participants completed the Zarit Caregiver Burden Interview, a 22-item questionnaire designed to reflect the stresses experienced by care partners by asking questions about the impact of the patient's abilities (eg, level of mobility, fatigue, personality change, and cognitive dysfunction) on their own lives (eg, effect on health, privacy, and social life).15 For each item on the questionnaire, care partners indicated how often they felt a certain way using a 5-point Likert scale (never, rarely, sometimes, quite frequently, or nearly always). Scores from each item are summed to create a total burden score in which scores of 21 or less indicate little or no burden; 22 to 40, mild burden; 41 to 60, moderate burden; and 61 to 88, severe burden. The scale has good test-retest reliability (α = 0.71) and internal consistency (α = 0.91) and good construct validity in caregivers of people with dementia, stroke, chronic obstructive pulmonary disease, and general medical disability.16,17
Health effects were assessed by asking the care partner a series of questions developed for this study. Specifically, they were asked to indicate 1) the current stress of caregiving (on an ordinal scale from 1, indicating “not stressful,” to 10, indicating “extremely stressful”), 2) current health (on an ordinal scale from 1, indicating “very healthy,” to 10, indicating “very ill”), and 3) use of medications for conditions such as high blood pressure, high cholesterol level, diabetes, mood disorder, sleep disturbance, or headache. Additional items queried about the two most stressful disabilities for a care partner (eg, restricted mobility, bladder/bowel difficulties, inability to use hands, visual disability, cognitive dysfunction, fatigue, spasticity, personality change, or depression), number of workdays missed in the past year due to caregiving, changes in employment status (ie, from full time to part time), and whether their primary-care physicians were aware of their care partner status.
Analyses
We summarized categorical variables using frequency (percentage) and continuous variables using mean (SD) or median (interquartile range [IQR]) as appropriate. We compared categorical variables between groups using χ2 tests and continuous variables between groups using t tests or Kruskal-Wallis tests as appropriate. We compared caregiver burden by sex of the care partner and MS course using analysis of variance, with the Zarit Caregiver Burden Interview total score as the dependent variable. Statistically significant differences for MS course were evaluated further using Tukey post hoc analyses to compare the burden scores for RRMS with those for SPMS and PPMS.
We tested the hypothesis that men would report more health problems, yet overall good health, by comparing scores for the physical health items from the questionnaire using χ2 tests. We assessed the socioeconomic burden of being a care partner by reporting the need to change employment and the number of workdays missed, and we compared this by sex and course of MS using χ2 and Kruskal-Wallis tests. Statistical analyses were conducted using SPSS for Windows, version 16.0 (SPSS Inc, Chicago, IL).
Results
Participants
We contacted all 12,826 NARCOMS participants with a valid e-mail address on file. Most of those contacted were female (74.8%), had a mean (SD) age of 50.2 (10.1) years, and had a mean (SD) disease duration of 12.9 (8.5) years. The e-mail asked these registry participants to invite their adult care partner to complete a one-time anonymous survey online. A total of 1446 care partners (11.3%) agreed to participate. After survey participants with missing data points were removed, 1333 remained, of whom 825 (61.9%) were male and 508 (38.1%) were female. The mean (SD) age of the overall care partner group was 51.1 (11.2) years (range, 18–84 years).
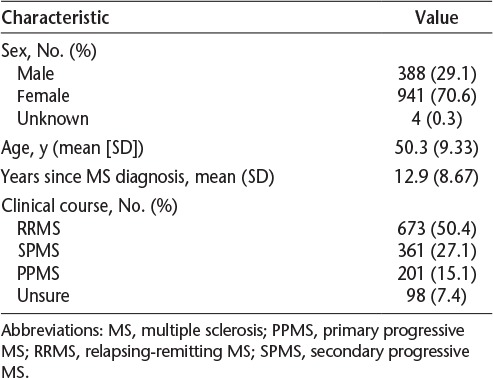
The characteristics of the 1333 care partners with complete data are shown in Table 1. Table 2 shows the descriptive statistics for the people with MS. As expected, most were female (70.6%), they ranged in age from 18 to 81 years, and time since diagnosis ranged from 1 to 50 years. Slightly more than half of the patients had relapsing-remitting MS. Due to the anonymity of the survey, the breakdown of how many registry participants perceived themselves to have a care partner and chose to invite him or her to take the study and the actual response rate among care partners is not known. However, compared with the overall registry participants receiving the study invitation, the people cared for by the study participants were similar in terms of age and disease duration (see previously herein and Table 2).
Table 1.
Characteristics of the 1333 multiple sclerosis care partners
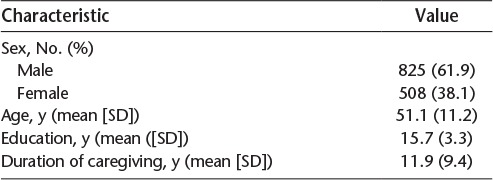
Table 2.
Characteristics of the 1333 people with MS cared for by the study participants
Care Partner Burden
The mean (SD) Zarit total score was 24.6 (15.1), placing the overall group in the mild caregiver burden range. When classified according to degree of burden, 647 care partners (48.5%) reported little or no burden; however, 475 (35.6%) reported mild burden, 183 (13.7%) reported moderate burden, and 28 (2.1%) reported severe burden.
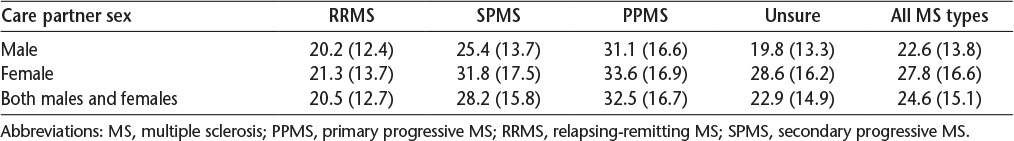
We compared level of burden according to the sex of the care partner. Mean (SD) Zarit scores are presented in Table 3. As hypothesized, women reported greater burden than men (F1,1331 = 38.9, P < .0001). When evaluated according to category of burden, a lower proportion of women reported little to no burden (39.2%) compared with men (54.3%), and women were nearly four times as likely to report severe burden (3.9% vs. 0.97%, P < .0001). Fifty-eight percent of care partners of people with RRMS reported little or no burden versus only 39.9% of care partners of people with SPMS and 30.3% of care partners of people with PPMS. Compared with care partners of people with RRMS (0.45%), care partners of people with SPMS were eight-fold more likely to report severe burden (3.88%), and care partners of people with PPMS were nearly ten-fold more likely to report severe burden (4.48%, P < .0001).
Table 3.
Mean (SD) Zarit Caregiver Burden Interview total scores stratified by care partner sex and course of MS
With respect to current health, the median (IQR) health level was 3 (2–4), and this did not differ by sex (P = .65). The median (IQR) stress level among care partners was 5 (3–7), with higher stress levels reported by women (5 [3–7]) than by men (4 [3–6], P < .0001). Overall health and stress levels correlated moderately (r = 0.35, 95% confidence interval = 0.30–0.40), with similar strengths of association when stratified by sex (data not shown).
Overall, 73.6% of respondents (918 of 1248) had informed their primary-care physicians of their role as a care partner. Men (71.8%) were slightly less likely to inform their physicians than were women (76.4%, P = .08). With respect to use of medications for specific health concerns, this was common among care partners, with the most frequent concerns being hypertension, hypercholesterolemia, and mood disorders (Table 4). Male care partners were more likely to endorse physical health concerns, such as hypertension, and women were more likely to endorse psychological symptoms, such as mood disorder and stress. Women were also more likely to endorse medication use for headaches and sleep disturbance.
Table 4.
Physical and psychological health concerns reported by care partners of people with multiple sclerosis stratified by sex
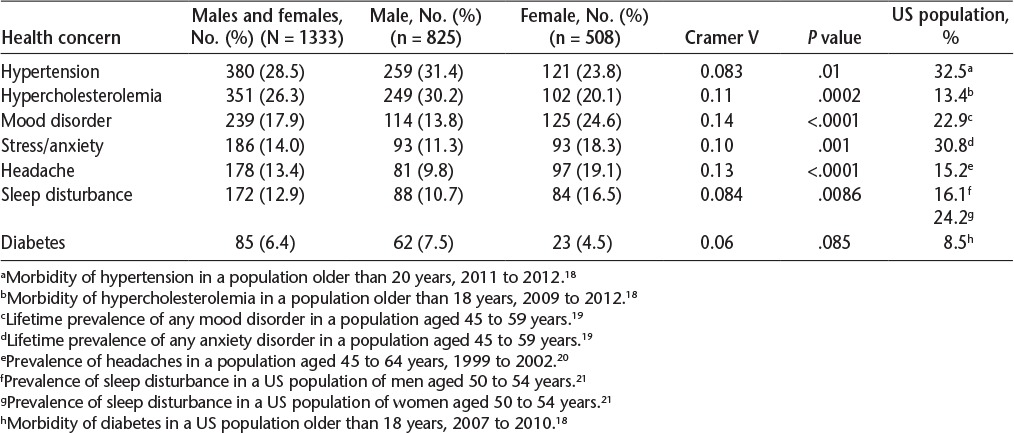
Burden, as measured by total Zarit score, did not differ between care partners who did and did not report hypertension (P = .85), hypercholesterolemia (P = .36), or diabetes (P = .41); however, Zarit scores were higher in those reporting mood disturbance (P < .0001), stress or anxiety (P < .0001), sleep disturbance (P < .0001), and headache (P = .0059) than in those who did not report these concerns.
Care Partner Burden by MS Course and Symptoms
Based on mean Zarit scores, the level of burden was highest with SPMS, followed by PPMS and then RRMS. We compared the level of burden according to the course of MS using analysis of variance and found a significant association (P < .0001) (Table 5) in which MS course accounted for 9.4% of the variance in total burden. Post hoc analyses using the Tukey honestly significant difference test showed that the unsure group and the RRMS group did not differ in level of total burden. After accounting for care partner sex, educational level, and age, the association between burden and course of MS persisted; burden was greater for PPMS and SPMS than for RRMS (both P < .0001) and for PPMS than for SPMS (P = .0023). Age and educational level were not associated with care partner burden.
Table 5.
Most stressful MS symptoms as rated by care partners, stratified by clinical course (N = 1333)
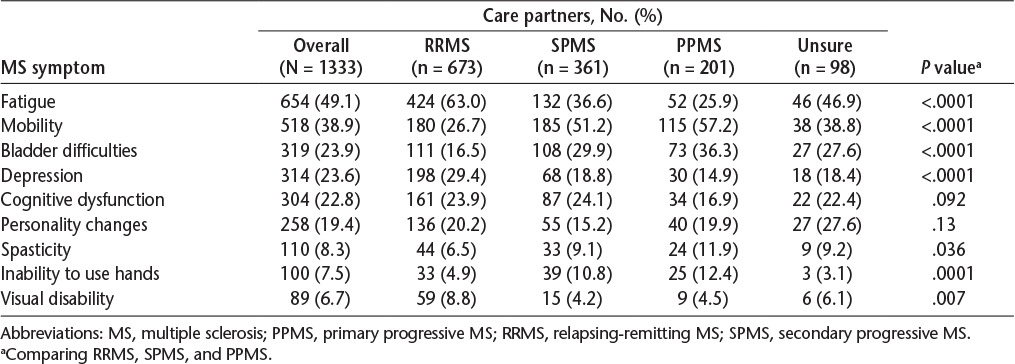
Overall, the MS symptoms most often perceived as stressful were fatigue and impaired mobility, followed by bladder difficulties, depression, cognitive dysfunction, and personality changes (Table 5). Male care partners reported that fatigue and spasticity were more stressful than did female care partners (P < .0001 and P = .002, respectively); the stress associated with other symptoms did not differ by sex. The MS symptoms deemed to be most stressful differed across MS types. Impaired mobility was the most stressful factor for care partners of people with SPMS and PPMS. Fatigue and bladder difficulties were the next most stressful factors, although in reverse order for PPMS versus SPMS. However, care partners of people with RRMS reported fatigue to be the most stressful, followed by depression and impaired mobility. Spasticity, impaired hand function, and visual impairment were less frequently rated as being stressful than other symptoms, but all were considered more of a concern for PPMS than for RRMS or SPMS.
Care Partner Socioeconomic Burden
Findings also revealed that 43.4% of MS care partners (559 of 1288) had missed work during the past year owing to caregiving responsibilities. Among those who missed work, care partners missed a mean (SD) of 18.4 (62.6) days. Eight percent of care partners (107 of 1333) reported changing their employment due to their role as a care partner. The proportion of care partners who had missed work did not differ by sex (P = .56) or course of MS (P = .14). However, among care partners who missed work, the number of days missed differed significantly by course of MS (P < .0001). Care partners of people with RRMS missed a mean (SD) of 11.8 (45.3) days, care partners of those with SPMS missed nearly twice as many days (20.9 [67.3]), and care partners of those with PPMS missed more than three times as many days (40.1 [98.8]). The number of days missed did not differ by sex.
Care partners of people with PPMS were twice as likely to change their jobs altogether due to their role as a care partner (10.9%) compared with care partners of people with RRMS (5.9%, P = .023).
Discussion
Caregiving is not generally viewed as a problem in the context of the larger society and is not viewed as a priority among public health policy lawmakers.22 However, care partners are estimated to provide 80% of the care to patients with MS,23 and this trend is expected to grow during the next 20 years.1,24–26 We aimed to understand the biopsychosocial ramifications of being an MS care partner in a sample of 1333 MS care partners. We found that physical and psychological health concerns were common. Furthermore, the effect on employment was also substantial, consistent with earlier studies.8,27
We observed differences in the health-related concerns reported by male and female care partners. Men did not perceive any problems with physical health but reported more medication use for hypertension, hypercholesterolemia, and diabetes than female care partners. This is a finding consistent with other research that found that male care partners had more chronic physical conditions than female care partners but reported better overall physical health.14 Female care partners reported greater burden and stress, as well as more medication use for stress/anxiety and mood disorders. Although we had hypothesized that men would report more headaches and sleep disturbance, as representing physical health concerns, this was not the case. An alternative hypothesis is that these are somatic concerns that mark psychological burden.28 Despite the fact that male care partners were not found to express significant emotional distress in this study, other studies have shown clinically significant psychopathology in male MS care partners.29,30 However, because the present study did not use a standardized measure of mood symptoms, it is plausible that the male MS care partners in the present study had clinically significant mood symptoms that contributed to the reported burden that we did not capture. One potential explanation for the observed gap in perceived versus actual health is male reporting style. That highlights the importance of looking at how males differ in their concept of awareness of problems, as well as their differences in communication and willingness to report them.31 These differences underscore the need for clinical attention and intervention focused on male care partners, who may not report their stress and fail to recognize the potential physiological risks associated with stress.
These findings are important given the observed association between care partner stress and the development and progression of major medical illnesses.32,33 In one such study, chronically stressed men and women caring for spouses with dementia showed a four-fold increase in interleukin-6 production compared with noncare partners. Those with the greatest interleukin-6 levels had a two-fold increased risk of death in the next 4 to 5 years compared with those with the lowest levels.34 Changes in immune function are also associated with psychiatric disorders, such as depression and anxiety.35 Negative emotions and stressful experiences collectively can lead to physiologic inflammation, which has also been associated with a variety of deleterious health effects, including cardiovascular disease, diabetes, and cancer.36–38 Chronically stressed or depressed individuals are also more likely to have poorer health habits, such as poor sleep patterns, poor nutrition, lack of exercise, and substance use, which also place them at greater risk for disease.39 This work along with ours emphasizes the need to develop and use effective stress and mood management techniques for care partners.
More than 40% of care partners missed work during the past year due to caregiving responsibilities, and nearly 10% changed their employment because of their care partner role. Although it is unknown what specifically led to job changes in the present sample, caregiver research is consistent with role conflict and time allocation theories in that increased absenteeism and work dissatisfaction is largely associated with increasing caregiver demands and inflexible work schedules (ie, lack of flextime, an inability to set one's own work hours)40; however, we do not know the effects of job changes for those care partners at or near retirement age (another well-known predictor of employment change). In addition, the amount of time spent caregiving has been viewed as a hidden economic cost because care partners lose out on days of paid work and on advanced occupational goals and opportunities.41,42 Recent studies suggest that sex differences in the economic impact of caregiving are also evident in that female care providers who remained working typically decreased their workload by 3 to 10 hours per week and faced a 3% wage cut, whereas there was very little impact of caregiving on men's working hours or wages.43 To a further extent, the American Association of Retired Persons and the National Alliance for Caregiving estimated that approximately 44 million American adults provide care to ill or disabled adults in their home and community without compensation and that the market value of this care is approximately $306 billion annually.6 Despite the pressures that many care partners experience to lessen work hours or even quit working entirely, approximately two-thirds of unpaid care partners continue to work full- or part-time jobs.6
We also found that care partners of people with PPMS reported greater burden, followed by care partners of those with SPMS and RRMS. Care partners of people with all types of MS endorsed restricted mobility and fatigue as stressful, whereas bladder difficulties were a bigger stress for PPMS and SPMS. Symptoms of depression stood out as the differential symptom endorsed significantly by the RRMS care partners. These findings concur with other studies that level of burden in MS care partners may be most related to the severity of the disease, including physically debilitating symptoms such as restricted mobility and incontinence.44,45 This is also consistent with findings in dementia, in which care partner burden is related to the severity of disease and the rapidity of progression.46 These findings also provide insights into individuals with the highest perceived care partner burden, potentially facilitating identification by physicians and consequently access to respite and other supports.
This study had several limitations. Although care partners of men were slightly more likely to respond,47 mean (SD) overall response rates were somewhat low (11% vs. 34.6% [15.7%]) compared with Internet-based response rates reported in the literature.48 This may have been affected by unsuccessful initial attempts to contact the care partner via the registry person with MS or by decisions to not participate based on the level of burden experienced by the care partner at the time because less than half of the sample was composed of those with more advanced MS. Because we used volunteers, findings may represent those of care partners who were especially motivated, uniquely stressed, or both. Generalizability may also be hindered by the use of an online questionnaire because participants with access to a computer may differ from those without such access.
Because this study was not able to randomly assign people to be care partners versus noncare partners, it is also impossible to be certain about what differences contributed to reported changes in health. Furthermore, because this study was cross-sectional, with limited knowledge of preexisting health conditions, conclusions about the causality of increased burden or physical illness are not possible; yet, increased cardiovascular risks (ie, higher cholesterol levels) in this sample are suggested compared with prevalence rates in the general population. Furthermore, mood disturbance was not assessed using a standardized measure, thus precluding our ability to rule out clinically significant mood symptoms that may have also contributed to reported burden. We also did not assess the positive aspects of the caregiving role, the number of hours spent caregiving, or the care partner's use of health-care treatments or resources that may have further affected mood, health, or employment. Indeed, recent studies reveal that a positive response to caregiving may provide indirect health benefits and maintain overall health in dementia caregivers. Despite these limitations, this study adds to the existing literature by providing additional power and generalizability, given the large study sample.
Future research on care partners of people with MS is imperative. From a health-care reform perspective, policy makers need to take into account that informal caregiving is costly and is accompanied by many physical and emotional burdens, although the “choice” to care for a loved one is typically preferred by the care partner compared with paying for medical services or having the patient leave home and is valued by both the care partner and the patient.49 Future work should evaluate positive aspects of the caregiving role in MS, as well as how care partners can be supported to minimize adverse effects on physical and psychological health. In addition, there is a great need to further address the economic effects of informal care partners to gain a better understanding about what factors affect workplace absenteeism, the decisions to change jobs or reduce workload, and the financial impact of changes in employment secondary to the sex of the caregiver.
PracticePoints.
Male MS care partners report more chronic health conditions than female care partners but tend to report overall better health; female MS care partners tend to report greater burden and emotional stress.
Many physicians and health-care providers are unaware of their patients' care partner status. Given the detrimental health effects of being a care partner, health-care professionals should regularly screen patients for care partner status and associated health risks.
Care partners of people with secondary progressive MS missed nearly twice as many workdays as care partners of people with relapsing-remitting MS, and care partners of people with primary progressive MS missed more than three times as many days and were twice as likely to change their jobs altogether due to their role as a care partner compared with relapsing-remitting MS care partners.
Acknowledgments
The authors are grateful to Dr. Janice Kiecolt-Glasser and Dr. Steven Zarit for their input during the concept development phase of this project.
Footnotes
Financial Disclosures: Dr. Marrie receives research funding from the Canadian Institutes of Health Research, Public Health Agency of Canada, Manitoba Health Research Council, Health Sciences Centre Foundation, Multiple Sclerosis Society of Canada, Multiple Sclerosis Scientific Foundation, and Rx & D Health Research Foundation and has conducted clinical trials funded by Sanofi-Aventis. Dr. Cutter is employed by the University of Alabama at Birmingham and is president of Pythagoras Inc, a private consulting company located in Birmingham, AL. He is on the editorial board of Multiple Sclerosis Journal and is statistical and contributing editor for Neurology Clinical Practice. He is funded by numerous National Institutes of Health grants and by the Department of Defense. He also participates in numerous advisory boards and data and safety monitoring committees and is engaged in consulting for companies including Alexion, Allozyne, Apotek, Ascendis, Bayer, Biogen Idec, Consortium of Multiple Sclerosis Centers, Cleveland Clinic, Genzyme, Glaxo Smith Kline Pharmaceuticals, Klein-Buendel Inc, Sanofi-Aventis, Gilead Pharmaceuticals, Medimmune, Merck/Ono Pharmaceuticals, Modigenetech/Prolor, Munck Wilson Mandala LLP, National Heart, Lung, and Blood Institute, National Institute of Neurological Disorders and Stroke, National Multiple Sclerosis Society, National Institute of Child Health and Human Development, Novartis, Nuron Biotech, PCT Bio, Receptos, Revalesio, Somahlution, Spiniflex Pharmaceuticals, Teva, Xenoport, and Vivus.
Funding/Support: Funding for this research was provided in part by an unrestricted educational grant from Serono. NARCOMS is supported in part by the Consortium of Multiple Sclerosis Centers and the Foundation of the Consortium of Multiple Sclerosis Centers.
References
- 1.Sanders S, Power J. Roles, responsibilities, and relationships among older husbands caring for wives with progressive dementia and other chronic conditions. Health Soc Work. 2009;34:41–51. doi: 10.1093/hsw/34.1.41. [DOI] [PubMed] [Google Scholar]
- 2.Sherman TE, Rapport LJ, Hanks RA et al. Predictors of well-being among significant others of persons with multiple sclerosis. Mult Scler. 2007;13:238–249. doi: 10.1177/1352458506070754. [DOI] [PubMed] [Google Scholar]
- 3.Schulz R, Sherwood PR. Physical and mental health effects of family caregiving. J Soc Work Educ. 2008;44:105–113. doi: 10.1097/01.NAJ.0000336406.45248.4c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vitaliano PP, Young HM, Zhang J. Is caregiving a risk factor for illness? Curr Dir Psychol Sci. 2004;13:13–16. [Google Scholar]
- 5.Bittman M, Hill T, Thomson C. The impact of caring on informal carers' employment, income and earnings: a longitudinal approach. Aust J Soc Issues. 2007;42:255–272. [Google Scholar]
- 6.Coghlan JG. The costs of being a caregiver. Accounting Today. July 20, 2009.
- 7.Finlayson M, Cho C. A descriptive profile of caregivers of older adults with MS and the assistance they provide. Disabil Rehabil. 2008;30:1848–1857. doi: 10.1080/09638280701707324. [DOI] [PubMed] [Google Scholar]
- 8.Buchanan RJ, Huang C, Zheng Z. Factors affecting employment among informal caregivers assisting people with multiple sclerosis. Int J MS Care. 2013;15:203–210. doi: 10.7224/1537-2073.2012-050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clark MS, Bond MJ, Hecker JR. Environmental stress, psychological stress, and allostatic load. Psychol Health Med. 2007;12:18–30. doi: 10.1080/13548500500429338. [DOI] [PubMed] [Google Scholar]
- 10.Swartz J, Keir S. Program preferences to reduce stress in caregivers of patients with brain tumors. Clin J Oncol Nurs. 2007;11:723–727. doi: 10.1188/07.CJON.723-727. [DOI] [PubMed] [Google Scholar]
- 11.Wallace EV. Managing stress: what consumers want to know from health educators. Am J Health Stud. 2007;22:56–58. [Google Scholar]
- 12.Matthews KA, Gump BB, Owens JF. Chronic stress influences cardiovascular and neuroendocrine response during acute stress and recovery, especially in men. Health Psychol. 2001;20:403–410. [PubMed] [Google Scholar]
- 13.Haley WE, Roth DL, Howard G, Safford MM. Caregiving strain and estimated risk for stroke and coronary heart disease among spouse caregivers: differential effects by race and sex. Stroke. 2010;41:331–336. doi: 10.1161/STROKEAHA.109.568279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang J, Vitaliano PP, Lin HH. Relations of caregiving stress and health depend on the health indicators used and gender. Int J Behav Med. 2006;13:173–181. doi: 10.1207/s15327558ijbm1302_9. [DOI] [PubMed] [Google Scholar]
- 15.Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: correlates of feelings of burden. The Gerontologist. 1980;20:649–655. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]
- 16.Rivera-Navarro J, Morales-González J, Benito-León J. Informal caregiving in multiple sclerosis patients: data from the Madrid demyelinating disease group. Disabil Rehabil. 2003;25:1057–1064. doi: 10.1080/0963828031000137766. [DOI] [PubMed] [Google Scholar]
- 17.Schreiner AS, Morimoto T, Arai Y, Zarit S. Assessing family caregiver's mental health using a statistically derived cut-off score for the Zarit Burden Interview. Aging Ment Health. 2006;10:107–111. doi: 10.1080/13607860500312142. [DOI] [PubMed] [Google Scholar]
- 18.FastStats. Centers for Disease Control and Prevention website. http://www.cdc.gov/nchs/fastats. Accessed October 28, 2014.
- 19.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 20.Schoenborn CA. Marital Status and Health, United States 1999–2002. Hyattsville, MD: National Center for Health Statistics; 2004. [Google Scholar]
- 21.Grandner MA, Martin JL, Patel NP et al. Age and sleep disturbances among American men and women: data from the U.S. Behavioral Risk Factor Surveillance System. Sleep. 2012;35:395–406. doi: 10.5665/sleep.1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Healy S. Caring for ethics and the politics of health care reform in the United States. Gender Place Culture. 2008;15:267–284. [Google Scholar]
- 23.Hillman L. Caregiving in multiple sclerosis. Phys Med Rehabil Clin N Am. 2013;24:619–627. doi: 10.1016/j.pmr.2013.06.007. [DOI] [PubMed] [Google Scholar]
- 24.Figved N, Myhr K-J, Larsen J-P, Aarsland D. Caregiver burden in multiple sclerosis: the impact in neuropsychiatric symptoms. J Neurol Neurosurg Psychiatry. 2007;78:1097–1102. doi: 10.1136/jnnp.2006.104216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.O'Hara L, De Souza L, Ide L. The nature of care giving in a community sample of people with multiple sclerosis. Disabil Rehabil. 2004;26:1401–1410. doi: 10.1080/09638280400007802. [DOI] [PubMed] [Google Scholar]
- 26.Patti F, Amato MP, Battaglia MA et al. Caregiver quality of life in multiple sclerosis: a multicentre Italian study. Mult Scler. 2007;13:412–419. doi: 10.1177/1352458506070707. [DOI] [PubMed] [Google Scholar]
- 27.Argyriou AA, Karanasios P, Ifanti AA et al. Quality of life and emotional burden of primary caregivers: a case–control study of multiple sclerosis patients in Greece. Qual Life Res. 2011;20:1663–1668. doi: 10.1007/s11136-011-9899-2. [DOI] [PubMed] [Google Scholar]
- 28.Argyriou AA, Karanasios P, Assimakopoulos K et al. Assessing the quality of sleep in Greek primary caregivers of patients with secondary progressive multiple sclerosis: a cross-sectional study. J Pain Symptom Manage. 2011;42:541–547. doi: 10.1016/j.jpainsymman.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 29.Buchanan RJ, Radin D, Huang C. Burden among male caregivers assisting people with multiple sclerosis. Gender Med. 2010;7:637–646. doi: 10.1016/j.genm.2010.11.009. [DOI] [PubMed] [Google Scholar]
- 30.Lehan T, Arango-Lasprilla JC, Macias MÁ, Aguayo A, Villaseñor T. Distress associated with patients' symptoms and depression in a sample of Mexican caregivers of individuals with MS. Rehabil Psychol. 2012;57:301–307. doi: 10.1037/a0030764. [DOI] [PubMed] [Google Scholar]
- 31.Chen H, Habermann B. Ready or not: planning for health declines in couples with advanced multiple sclerosis. J Neurosci Nurs. 2013;45:38–43. doi: 10.1097/JNN.0b013e318275b1f9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Graham JE, Christian LM, Kiecolt-Glaser JK. Stress, age, and immune function: toward a lifespan approach. J Behav Med. 2006;29:389–400. doi: 10.1007/s10865-006-9057-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miller G, Chen E, Cole SW. Health psychology: developing biologically plausible models linking the social world and physical health. Ann Rev Psychol. 2009;60:501–524. doi: 10.1146/annurev.psych.60.110707.163551. [DOI] [PubMed] [Google Scholar]
- 34.Kiecolt-Glaser JK, Preacher KJ, MacCallum RC, Atkinson C, Malarkey WB, Glaser R. Chronic stress and age-related increases in the proinflammatory cytokine IL-6. Proc Natl Acad Sci U S A. 2003;100:9090–9096. doi: 10.1073/pnas.1531903100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Leonard BE, Myint A. The psychoneuroimmunology of depression. Hum Psychopharmacol. 2009;24:165–175. doi: 10.1002/hup.1011. [DOI] [PubMed] [Google Scholar]
- 36.Kiecolt-Glaser JK, McGuire L, Robles TF, Glaser R. Psychoneuroimmunology and psychosomatic medicine: back to the future. Psychosom Med. 2002;64:15–28. doi: 10.1097/00006842-200201000-00004. [DOI] [PubMed] [Google Scholar]
- 37.Littrell J. The mind-body connection: not just a theory anymore. Soc Work Health Care. 2008;46:17–37. doi: 10.1300/j010v46n04_02. [DOI] [PubMed] [Google Scholar]
- 38.Reiche EMV, Nunes SOV, Morimoto HK. Stress, depression, the immune system, and cancer. Lancet Oncol. 2004;5:617–625. doi: 10.1016/S1470-2045(04)01597-9. [DOI] [PubMed] [Google Scholar]
- 39.Robles TF, Glaser R, Kiecolt-Glaser JK. Out of balance: a new look at chronic stress, depression, and immunity. Curr Directions Psychol Sci. 2005;14:111–115. [Google Scholar]
- 40.Zuba M, Schneider U. What helps working informal caregivers? the role of workplace characteristics in balancing work and adult-care responsibilities. J Fam Econom Issues. 2013;34:460–469. [Google Scholar]
- 41.Chiò A, Gauthier A, Vignola A et al. Caregiver time use in ALS. Neurology. 2006;67:901–904. doi: 10.1212/01.wnl.0000233840.41688.df. [DOI] [PubMed] [Google Scholar]
- 42.McCabe M, Firth L. Work and recreational changes among people with neurological illness and their caregivers. Disabil Rehabil. 2008;30:600–610. doi: 10.1080/09638280701400276. [DOI] [PubMed] [Google Scholar]
- 43.Van Houtven CH, Coe NB, Skira MM. The effect of informal care on work and wages. J Health Econom. 2013;32:240–252. doi: 10.1016/j.jhealeco.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 44.Ertekin Ö, Özakbaş S, İdiman E. Caregiver burden, quality of life and walking ability in different disability levels of multiple sclerosis. NeuroRehabilitation. 2014;34:313–321. doi: 10.3233/NRE-131037. [DOI] [PubMed] [Google Scholar]
- 45.Dunn J. Impact of mobility impairment on the burden of caregiving in individuals with multiple sclerosis. Exp Rev Pharmacoeconom Outcomes Res. 2010;10:433–440. doi: 10.1586/erp.10.34. [DOI] [PubMed] [Google Scholar]
- 46.Acaster S, Perard R, Chauhan D, Lloyd AJ. A forgotten aspect of the NICE reference case: an observational study of the health related quality of life impact on caregivers of people with multiple sclerosis. BMC Health Serv Res. 2013;13:346. doi: 10.1186/1472-6963-13-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Basu R, Hochhalter AK, Stevens AB. The impact of the REACH II intervention on caregivers' perceived health. J Appl Gerontol. 2015;34:590–608. doi: 10.1177/0733464813499640. [DOI] [PubMed] [Google Scholar]
- 48.Cook C, Heath F, Thompson RL. A meta-analysis of response rates in web- or internet-based surveys. Educ Psychol Meas. 2000;60:821–836. [Google Scholar]
- 49.Hollander MJ, Liu G, Chappell NL. Who cares and how much? the imputed economic contribution to the Canadian healthcare system of middle-aged and older unpaid caregivers providing care to the elderly. Healthc Q. 2009;12:42–49. doi: 10.12927/hcq.2009.20660. [DOI] [PubMed] [Google Scholar]


