Abstract
The term splenosis describes autotransplantation or implantation of ectopic splenic tissue within the abdominal cavity or in any other unusual body compartment. In addition to the diagnostic dilemma it causes, splenosis may also lead to persistence or recurrence of hematologic dysfunctions by its preserved immune activity especially in cases of splenectomy due to hematologic indications. Herein, we present a 40-year-old female who had splenectomy for idiopatic thrombocytopenic purpura, and was identified to have splenic tissue within left lobe of the liver during further assessment of ongoing thrombocytopenia.
Keywords: Splenosis, intrahepatic splenosis, idiopatic thrombocytopenic purpura
INTRODUCTION
The term splenosis refers to heterotopic autotransplantation or implantation of splenic tissue following splenectomy or spleen trauma. Buchbinder and Lipkopf described this entity for the first time in 1939. Splenic implants usually are multiple (1). Splenosis is reported to occur in 16–67% of patients after splenic surgery or traumatic rupture of the spleen. The incidence of splenosis following elective splenectomy in patients with non-traumatic causes is low (2). Hepatic splenosis is rare, and its differential diagnosis with hepatic adenoma, focal nodular hyperplasia, lymphoma, hemangioma and hepatocellular carcinoma can be difficult (3). It may appear in any part of the peritoneal cavity, and often in the bowel and mesentery, serosal surfaces, omentum, the diaphragm and pelvis. Unusual locations include the pleural cavity, pelvis, and subcutaneous tissue (4). Most patients are asymptomatic and are diagnosed incidentally. However, abdominal pain and hematologic dysfunction may rarely be seen (5).
This article aimed to present a patient who had splenectomy for idiopathic thrombocytopenic purpura (ITP), and was identified to have intrahepatic splenosis after development of thrombocytopenia.
CASE PRESENTATION
A 40-year-old female patient with persistent low platelet count (<20 thousand) who had splenectomy 7 years ago for ITP underwent ultrasound (USG) and contrast enhanced abdominopelvic computed tomography (CT) scan. The USG revealed a 68 × 31 mm in size, lobulated mass located in the left upper quadrant that was isodense with the spleen. On CT examination, there was a 7 × 3 cm in size, regular bordered mass with minimal lobulation, which was isodense with the spleen (Figure 1). The patient was diagnosed with a possible postoperative accessory splenic hypertrophy, and the persistent ITP was accepted as an indication for surgery. She was taken to surgery following the required hematologic preparations. Intraoperatively, a solid lesion that was 7 × 3 cm in size was observed in the posterior aspect of the left lobe (segments 2–3) and within the liver parenchyma. The intrahepatic lesion was resected in a way that partially included segments 2–3 (Figure 2, 3). Macroscopically the nodular lesion was 7 × 4 × 3 cm in dimension, sharply demarcated from surrounding liver tissue, and had a solid red color on the cut surface. Histopathologic examination revealed features of a normal liver tissue separated by fibrous septa and marked sinusoidal expansions resembling hemangioma, along with splenic tissue mainly composed of red pulp (Figure 4) and a number of lymphoid follicles (Figure 5); thus the case was reported as intrahepatic splenosis.
Figure 1.
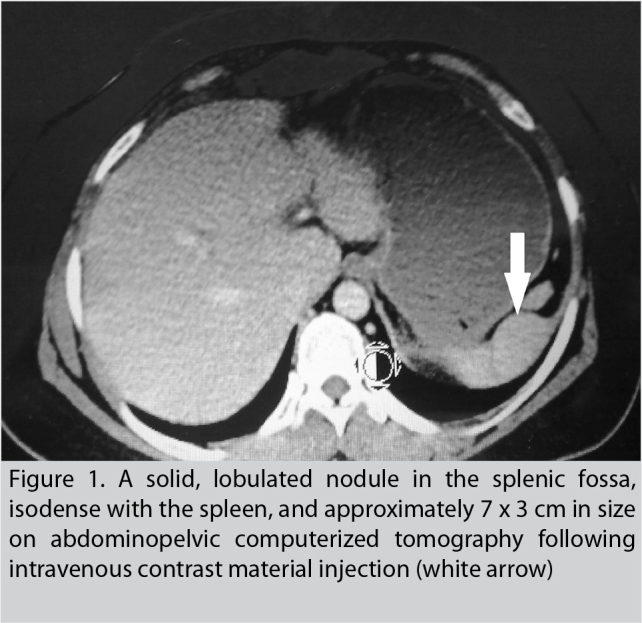
A solid, lobulated nodule in the splenic fossa, isodense with the spleen, and approximately 7 × 3 cm in size on abdominopelvic computerized tomography following intravenous contrast material injection (white arrow)
Figure 2.
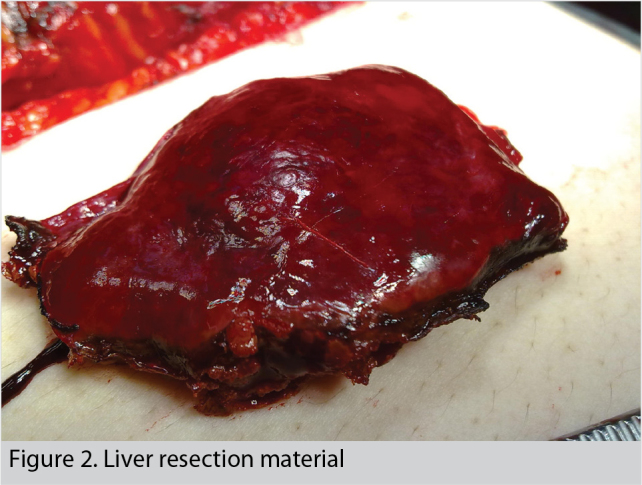
Liver resection material
Figure 3.
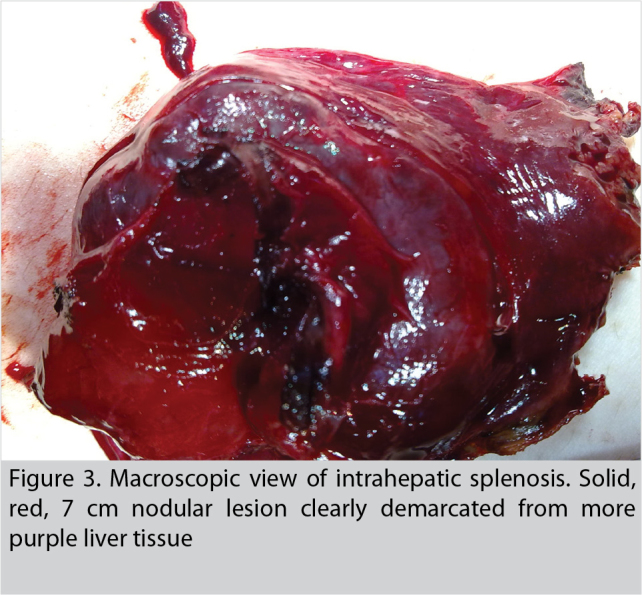
Macroscopic view of intrahepatic splenosis. Solid, red, 7 cm nodular lesion clearly demarcated from more purple liver tissue
Figure 4.
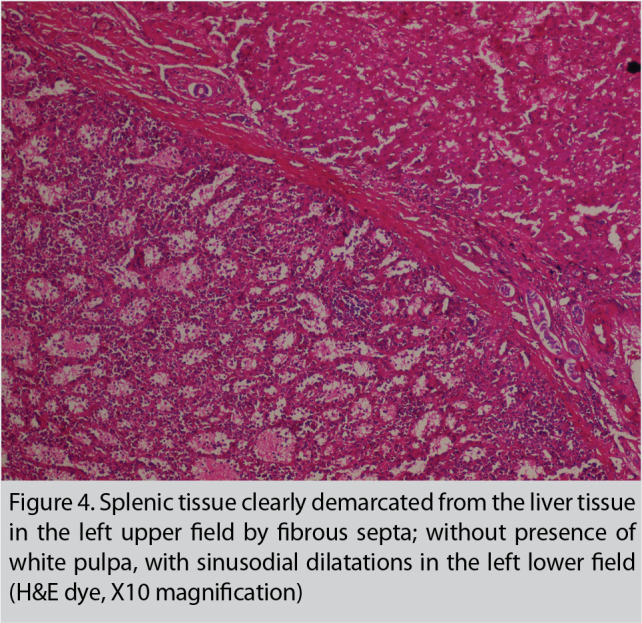
Splenic tissue clearly demarcated from the liver tissue in the left upper field by fibrous septa; without presence of white pulpa, with sinusodial dilatations in the left lower field (H&E dye, X10 magnification)
Figure 5.
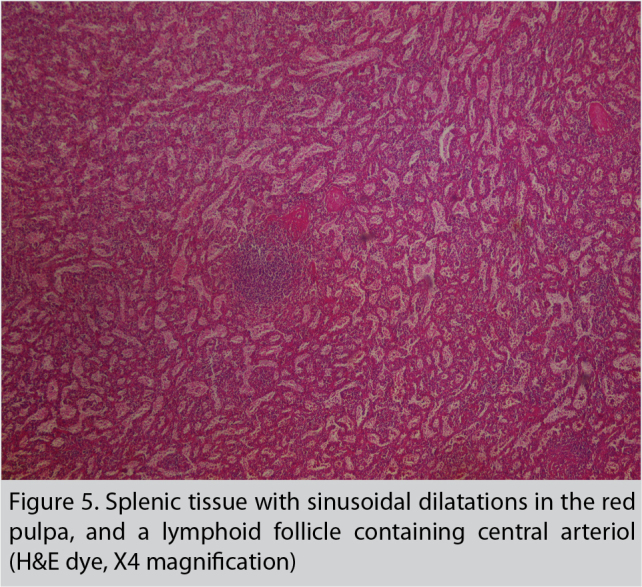
Splenic tissue with sinusoidal dilatations in the red pulpa, and a lymphoid follicle containing central arteriol (H&E dye, X4 magnification)
DISCUSSION
Splenosis is caused by spillage of splenic pulp within the abdominal cavity following splenic trauma or splenectomy (4). Another mechanism of splenic tissue transplantation is hematogenous dissemination of splenic pulp that is thought to be responsible for intracranial and intrahepatic splenosis. Splenosis has been shown by transplantation of the splenic pulp experimentally in dogs, rats, rabbits and monkeys (5). It was also suggested that splenic erythroid progenitor cells could access the liver via the portal vein, proliferate in response to tissue hypoxia and create splenosis (6). The location of splenic implants is closely related to the type of trauma and/or operative approach. Since the spleen is an intra-abdominal organ, splenosis is usually detected within the peritoneal cavity. Usually it is localized in the left upper abdomen and splenic fossa (7). However, with widespread dissemination due to more extensive injuries, splenosis can be seen in the serosal surfaces of the small intestine, great omentum, parietal peritoneum, over the large intestine, the lower surface of the diaphragm and the Douglas cavity. Thoracic splenosis cases have also been reported in patients with accompanying diaphragm rupture (8). Splenic implants have an advanced transplantation ability along with lack of tissue selectivity, thus, splenosis cases that mimic intrabronchial, pericardial, subcutaneous, or even stomach, kidney and liver tumors have been reported (9, 10). The size of intrahepatic splenosis may vary from a few millimeters up to 12 centimeters (11). In our patient, the splenosis focus was isolated and 7 × 3 cm in size. Intrahepatic splenosis can be clinically and radiologically misdiagnosed as intrahepatic nodular lesions such as hepatic adenoma, focal nodular hyperplasia, lymphoma, hemangioma and hepatocellular carcinoma. The vast majority of patients with splenosis are asymptomatic. Recurrence of symptoms in patients who underwent splenectomy for hematologic indications indicates the presence of splenosis (3). The hematologic symptoms have recurred in our patient, and have not improved despite treatment. The diagnosis of splenosis or ectopic splenic tissue is usually made by USG, CT or MRI scans. Tc-99m sulfur colloid scintigraphy is also extremely sensitive in the detection of ectopic splenic tissue; it enables the identification of small sized splenosis or those in the form of multiple nodules that may be overlooked on CT or MRI. Intrahepatic splenosis is usually observed as well-bordered, hypo-isoechoic solid lesions on USG examination with no specific color or spectral Doppler USG findings. The lesions appear as hypodense areas in un-enhanced CT, while being hyperdense in the arterial phase in dynamic contrast-enhanced CT series following intravenous contrast material injection, isodense in the portal phase, and hypodense in the equilibrium phase (11). In our case, the hepatobiliary USG planned after splenectomy revealed a hypoechoic nodular mass in the abdomen, in the splenic fossa, and this lesion was interpreted as splenic tissue on CT examination. These findings were confirmed by postoperative histopathologic evaluation. Additional scintigraphic evaluation was not performed since sufficient diagnostic evaluation could be done with USG and CT examinations, and since this modality cannot be performed at our institution.
CONCLUSION
Splenosis should be kept in mind as part of differential diagnosis of liver masses in patients with a history of splenic trauma or splenectomy, and if thrombocytopenia persists after therapeutic splenectomy for hematologic diseases.
Footnotes
Informed Consent: Written informed consent was obtained from patient who participated in this case.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - O.T.; Design - O.T.; Supervision - A.Y., İ.B.; Funding - O.T.; Materials - Ü.İ., D.Y.; Data Collection and/or Processing - O.T., D.Y., İ.B.; Literature Review - O.T., A.Y., İ.B.; Writer - O.T., A.Y.; Critical Review - O.T., A.Y.; Other - Ü.İ., D.Y., İ.B.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
REFERENCES
- 1.Tsitouridis I, Michaelides M, Sotiriadis C, Arvaniti M. CT and MRI of intraperitoneal splenosis. Diagn Interv Radiol. 2010;16:145–149. doi: 10.4261/1305-3825.DIR.1855-08.1. [DOI] [PubMed] [Google Scholar]
- 2.Menth M, Herrmann K, Haug A, Raziorrouh B, Zachoval R, Jung CM, et al. Intra-hepatic splenosis as an unexpected cause of a focal liver lesion in a patient with hepatitis C and liver cirrhosis: a case report. Cases J. 2009;2:8335. doi: 10.4076/1757-1626-2-8335. http://dx.doi.org/10.4076/1757-1626-2-8335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khosravi MR, Margulies DR, Alsabeh R, Nissen N, Phillips EH, Morgenstern L. Consider the diagnosis of splenosis for soft tissue masses long after any splenic injury. Am Surg. 2004;70:967–970. [PubMed] [Google Scholar]
- 4.Kang KC, Cho GS, Chung GA, Kang GH, Kim YJ, Lee MS, et al. Intrahepatic splenosis mimicking liver metastasis in a patient with gastric cancer. J Gastric Cancer. 2011;11:64–68. doi: 10.5230/jgc.2011.11.1.64. http://dx.doi.org/10.5230/jgc.2011.11.1.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nakajima T, Fujiwara A, Yamaguchi M, Makiyama A, Wakae T, Fujita K, et al. Intrahepatic splenosis with severe iron deposition presenting with atypical magnetic resonance images. Intern Med. 2008;47:743–746. doi: 10.2169/internalmedicine.47.0689. http://dx.doi.org/10.2169/internalmedicine.47.0689. [DOI] [PubMed] [Google Scholar]
- 6.De Vuysere S, Van Steenbergen W, Aerts R, Van Hauwaert H, Van Beckevoort D, Van Hoe L. Intrahepatic splenosis: imaging features. Abdom Imaging. 2000;25:187–189. doi: 10.1007/s002619910042. http://dx.doi.org/10.1007/s002619910042. [DOI] [PubMed] [Google Scholar]
- 7.Gruen DR, Gollub MJ. Intrahepatic splenosis mimicking hepatic adenoma. AJR Am J Roentgenol. 1997;168:725–726. doi: 10.2214/ajr.168.3.9057523. http://dx.doi.org/10.2214/ajr.168.3.9057523. [DOI] [PubMed] [Google Scholar]
- 8.Kumbasar U, Döner E, Enön S, Akal M, Öztürk C. Thoracic splenosis. Turk J Hematol. 2005;22:147–149. [PubMed] [Google Scholar]
- 9.Kwok CM, Chen YT, Lin HT, Su CH, Liu YS, Chiu YC. Portal vein entrance of splenic erythrocytic progenitor cells and local hypoxia of liver, two events cause intrahepatic splenosis. Med Hypotheses. 2006;67:1330–1332. doi: 10.1016/j.mehy.2006.04.064. http://dx.doi.org/10.1016/j.mehy.2006.04.064. [DOI] [PubMed] [Google Scholar]
- 10.Yananlı ZD, Uçmaklı E, Öztürk A, Akıncı OF. A case of splenosis mimicking a gastric tumor. J Kartal TR. 2015;26:182–184. [Google Scholar]
- 11.Ufuk F, Karabulut N. İntraabdominal splenozis: BT bulguları. Pam Tıp Derg. 2013;6:37–40. [Google Scholar]


