Supplemental Digital Content is available in the text
Abstract
This study aimed to evaluate the association between family history and prevalence of hypertension among Chinese community elderly, and also explore the gender difference.
A population-based cross-sectional study was conducted in Miyun district of Beijing, in 2014. The family history information was obtained from each subject and was divided into 3 categories, no family history (FH0), 1 generation of first-degree relatives with hypertension (FH1), and 2 generations of first-degree relatives with hypertension (FH2).
The prevalence of hypertension was 53.0%. Participants with positive family history had a significantly higher prevalence of hypertension (67.5%, 95% CI: 63.3–71.7) than those without (47.9%, 95% CI: 45.2–50.6), and even among participants without hypertension, the blood pressure levels were higher with positive FH. Multiple logistic regression analysis showed that a significantly linear-trend increase in hypertension according to family history of first degree relative numbers was observed in both genders (P for trend < 0.001).
This study suggests that family history had not only a significant but also graded association with hypertension and with blood pressure levels, and this association exists even among those without hypertension.
INTRODUCTION
Hypertension is a major chronic noncommunicable disease which has affected nearly 1 billion people worldwide.1 Current available evidence suggests that hypertension is 1 of the most preventive risk factors for cardiovascular disease, and kidney diseases and is also at increased risk for mortality of all causes.2–4 And with the huge socioeconomic change and a succession of increases of unhealthy lifestyles, hypertension will affect even more population in the near future, especially in the developing countries.5–6 In China, the age-standardized prevalence of hypertension was 31.4% in north and 20.9% in south, and the prevalence has risen by 1.4% per year for the past decade.7 Therefore, it is important and urgent to identify the participants who have high risk of hypertension and then to prevent subsequent related cardiovascular disease (CVD).
Numerous researchers have found that genetic factors play an important role in hypertension. Patients who had family history (FH) of hypertension would have a 2 to 4 fold higher risk of getting this disease.8–9 Also, there were studies found that the prevalence of hypertension increased with the number of affected relatives.10–12 Other studies showed that mothers with hypertension contributed more than fathers,13 and first-degree relatives with hypertension were linked to higher risk of getting hypertension, compared with second-degree relatives.10
The above findings of FH and the prevalence of hypertension were mainly from the American and European countries. We did not find at the literature, any related research about Chinese people, who are undergoing huge social-economical changes and rapidly increasing prevalence of hypertension. Our study aims to examine the association of FH risk categories and prevalence of hypertension in a rural community elderly population of Beijing, China, and to provide evidence for different FH categories and its influence on prevalence of hypertension.
MATERIALS AND METHODS
Methods
The present study was a cross-sectional community-based study conducted between May and August 2014 in Jugezhuang town of Miyun district, a metropolitan area representative of the geographic and economic characteristics in rural Beijing, China. We did a 2-stage random cluster sampling was used. Five villages were randomly selected from all the 26 villages, and all the residents’ ages ≥60 years who had lived in the local district for at least 1 year were invited into the study. A total of 2122 residents’ ages 60 to 92 years were selected and invited for screening. One thousand eight hundred thirty-six residents (713 men and 1123 women) completed the survey. The response rate was 86.5% (85.7% in men and 87.1% in women). And they accounted for 20.6% of elderly residents in the Jugezhuang town.
A standardized questionnaire including marriage status, education levels, lifestyles, and use of medications was conducted face to face by trained doctors and nurses. Weights, height, and waist circumference (WC) were measured and overnight blood sampling was tested. The detailed measuring methods were reported before in our previous study.14 Two blood pressures were measured using sphygmomanometer after 30 min of rest.
Questionnaire of FH
All participants completed a standardized questionnaire including a range of demographic factors, medical history, FH of CVD, alcohol consumption, and smoking. Participants were asked by trained interviewers face to face to obtain the information. For FH of hypertension, participants selected “yes,” “no,” or “uncertain” in a table of questions about the presence of hypertension in parents (either father or mother) or siblings (either sisters or brothers). The results were classified into FH0 (no first-degree relatives had hypertension), FH1 (1 generation first-degree relatives had hypertension), and FH2 (2 generation first-degree relatives had hypertension). Also, we separate the FH1 into 2 groups: FH parents (only parents had hypertension, no siblings) and FH siblings (only siblings had hypertension, no parents). Positive FH of hypertension was defined as having at least 1 generation with hypertension.
Definition of Hypertension
Hypertension was defined according to 2010 Chinese guidelines for the management of hypertension, as following: Participants with systolic blood pressure (SBP) ≥ 140 mm Hg and/or diastolic blood pressure (DBP) ≥ 90 mm Hg as well as participants receiving treatment for hypertension.15
Statistical Analysis
Data were entered (double entry) using Epidata 3.1. All analyses were conducted using SPSS for windows (20.0, Chicago, IL, No. of Serial: 5076595).
Descriptive data were expressed as x ± s for continuous variables and percentage for categorical variables unless otherwise specified. The significance of difference between means and proportions were tested by using T test, variance analysis and Chi-squared test, and compare the prevalence of hypertension between positive FH and negative FH. The trend test was used to determine the trends in the prevalence of hypertension according to 3 FH risk categories. Finally, multivariable logistic regression was used to estimate the association between gender-specific FH risk categories and hypertension. We calculated the odds ratio (OR) and 95% confidence intervals (CIs) of FH risk categories for hypertension. Reported probabilities were 2-sided, all tests were set at the 0.05 level of statistical significance.
Ethical Consideration
All eligible participants received verbal and written information and gave their written informed consent to take part in the study. Ethics approval was obtained from the Ethics Committees of Chinese PLA General Hospital (EC0411-2001).
RESULTS
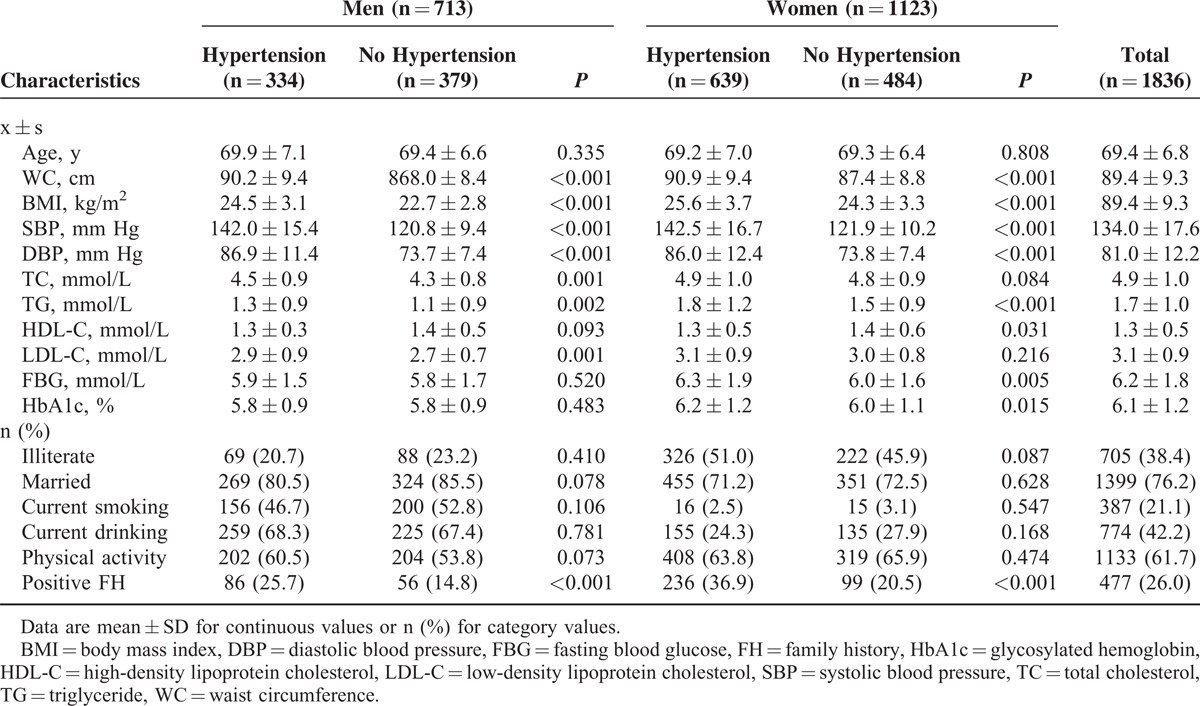
A total of 1836 participants completed the survey, with 713 (38.8%) men and 1123 (61.2%) women. The mean age were 69.4 ± 6.8 (60–92 years), older elderly (ages ≥ 80 years) accounted for 10.4%. The prevalence of hypertension in this community elderly was 53.0%, men were lower than women (46.8% vs 56.9%, P < 0.001). Baseline characteristics of participants according to gender and hypertension are presented in Table 1. Participants with hypertension had larger WC, higher BMI, higher blood pressure, glucose level, and cholesterol level. Also, participants with hypertension had a higher percentage of FH.
TABLE 1.
Characteristics of the Participants With Family History and Those Without
FH Categories of the Participants
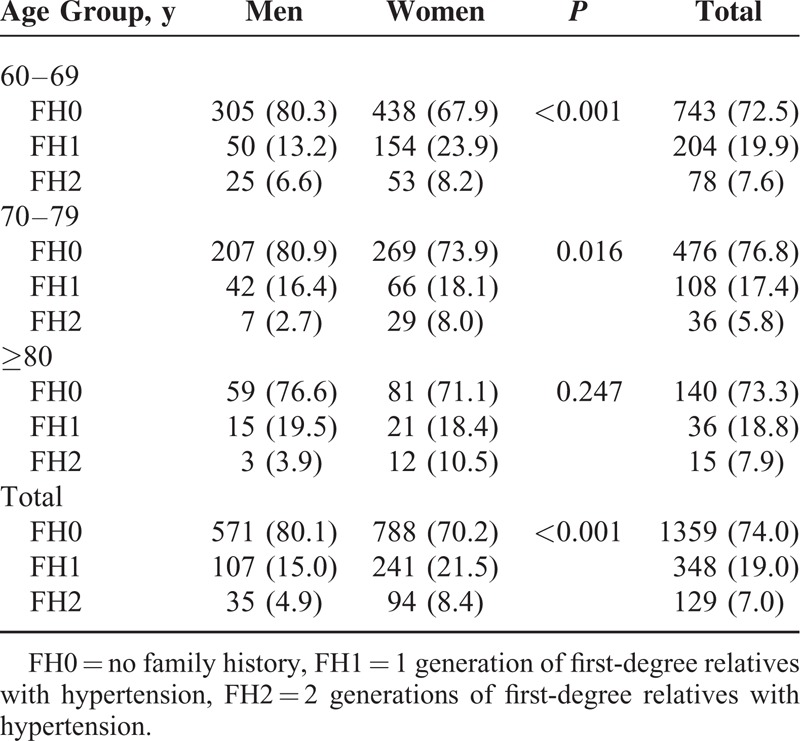
Table 2 showed the FH categories of the participants according to gender and age group. Four hundred seventy-seven participants had a positive FH, 348 were classified into FH1, accounting for 19.0%, and 129 participants were classified into FH2, accounting for 7.0% of the total sample. Among those with FH1, 161 participants were FH parents and 187 were FH siblings. Women had a higher percentage of FH1 and FH2 compared with men (P < 0.001), and this phenomenon is more obvious among younger elderly (<80 years).
TABLE 2.
Family History Categories of the Participants According to Gender and Age Group
Characteristics of Participants According to FH Categories
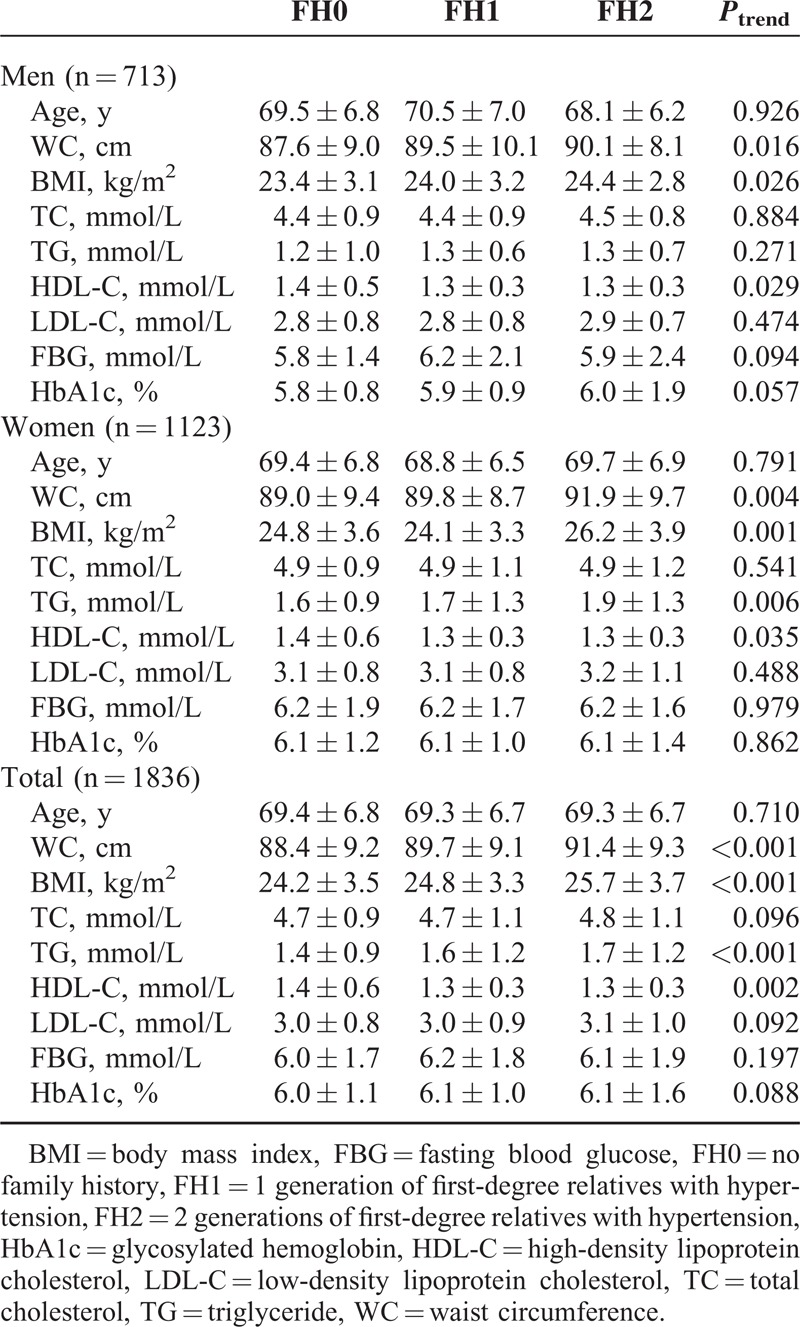
Table 3 showed the demographic characteristics and anthropometric measurements of the 1836 participants. Along with the increase of FH categories, participants had an increasing trend of main characteristics, including WC, BMI, blood pressure level, blood glucose, and cholesterol. For example, the mean WC values were 88.4 ± 9.2 cm, 89.7 ± 9.1 cm, and 91.4 ± 9.3 cm for FH0, FH1, and FH2, respectively, 3 groups, and P for trend was <0.001. However, there were no significant differences in age, total cholesterol, low-density lipoprotein cholesterol, fasting blood glucose, and glycosylated hemoglobin.
TABLE 3.
Characteristics of the Participants According to Family History Categories
Prevalence of Hypertension and Blood Pressure Level According to Different FH Risk Categories
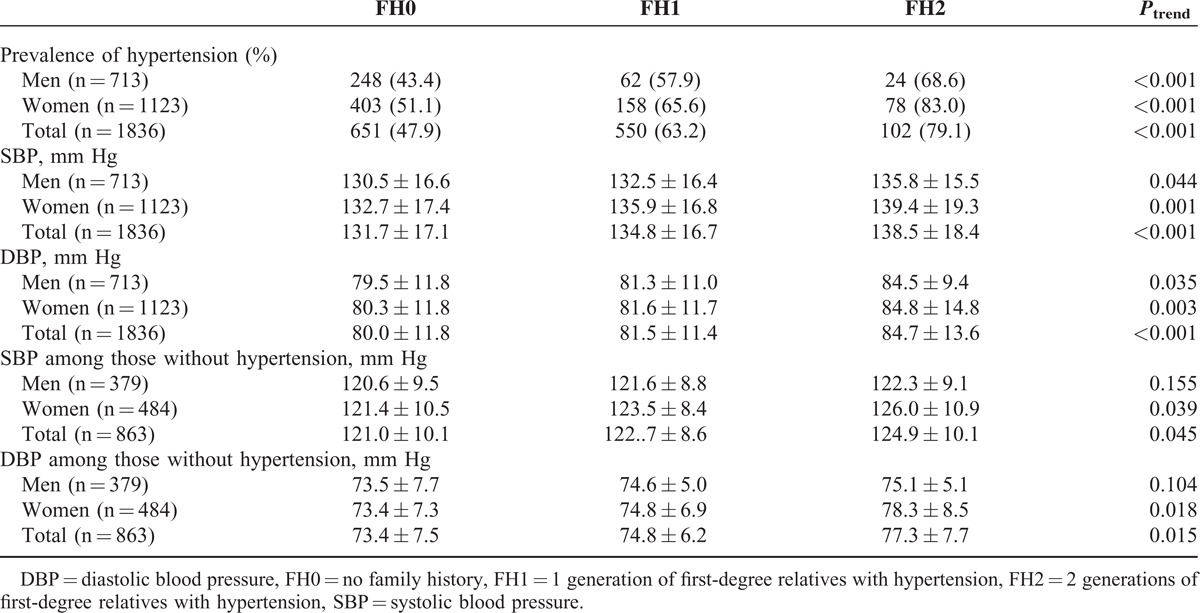
Table 4 described the prevalence of hypertension by gender and by different FH categories. The prevalence showed an increasing trend with FH categories (47.9% in FH0, 63.2% in FH1, 79.1% in FH2, P for trend < 0.001). For blood pressure levels, both SBP and DBP were increased with FH categories. Even among participants without hypertension, the blood pressures also showed the same increasing trend excluding SBP level in men (which also increased with FH categories but did not reach statistically significant levels).
TABLE 4.
Prevalence of Hypertension and Blood Pressure Level According to Different Family History Risk Categories
ORs of FH Categories and Prevalence of Hypertension
Table 5 showed the ORs of FH categories and prevalence of hypertension. After adjusted age, gender, education level, marital status, BMI, current smoking, current drinking, physical activity, participants with positive FH were at significantly elevated ORs for prevalence of hypertension compared with those without. The ORs were 1.82 (95% CI: 1.42–2.33) and 3.72 (95% CI: 2.38–5.83) for FH1 and FH 2 (P for trend < 0.001). When we separate FH1 into FH parents and FH siblings, we can see from Table 5 that FH from parents had a bigger effect than that from siblings, the ORs were 2.15 (95% CI: 1.52–3.04) and 1.68 (95% CI: 1.17–2.41).
TABLE 5.
Association Between Family History Risk Category and Prevalence of Hypertension (ORs and 95% CI)
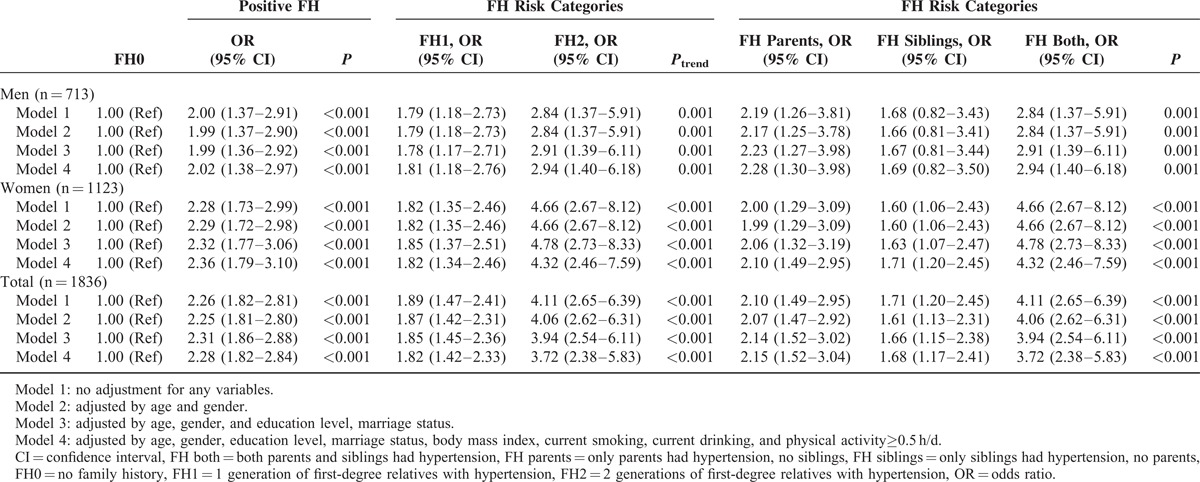
There were gender differences in the ORs for hypertension. Women had higher ORs of FH categories for hypertension than men, especially among those with FH2. The ORs of FH1 and FH2 for hypertension were 1.67 (95% CI: 1.08–2.58) and 2.49 (95% CI: 1.17–5.30) in men but 1.82 (95% CI: 1.34–2.46) and 4.32 (95% CI: 2.46–7.59) in women.
We also ascertained the association of FH categories and hypertension in the sensitivity analysis and the results were similar (Appendix Table, http://links.lww.com/MD/A548). When participants ages under 65 years old (n = 531, 28.9%) were excluded, the adjusted ORs for FH1 and FH2 associated with hypertension were 1.74 (95% CI: 1.29–2.33) and 4.09 (95% CI: 2.41–6.96), respectively.
DISCUSSION
In this study, we evaluated the association of FH and hypertension in a Chinese rural community elderly population. We found that positive FH was associated with 2.28-fold prevalence of hypertension even after adjusting for confounding factors. This association of hypertension risk by different FH categories was more robust in women than in men. Also, we found that this association showed a graded trend along with numbers of first degree relatives who had hypertension.
Hypertension and CVD are rapidly growing threats to public health worldwide, especially in economically developing countries such as China.16 Just in the past decade, prevalence of hypertension in China has increased from 23.4% to 28.6%.17 Considering the giant elderly in China and the strong associated of hypertension with the development of CVD and related disease burden, identifying high-risk asymptomatic individuals for hypertension is of critical importance and may lead to improvements in prevention and treatment of the condition and subsequent CVD events and increased disease burden.18–19
A number of studies from different countries have shown strong association between FH and hypertension or blood pressure level.8,10–11 Those with positive FH were 2 to 4 times likely to have hypertension. In this study, our study also showed the OR of FH for prevalence of hypertension was 2.28 (95% CI: 1.82–2.84), which is similar to other studies. Along with that, we also found a graded positive association between FH categories and the prevalence of hypertension among this Chinese community elderly, and even among those without hypertension, the blood pressure level also increased with FH categories.
The present study also provides evidence that elevated FH categories were more strongly associated with hypertension in women than in men. Previous studies also reported similar results. A Mexico study showed FH of hypertension in the maternal branch, was associated with hyperinsulinemia (OR 1.5, 95% CI: 1.1–5.5), high blood pressure (OR 4.0, 95% CI: 1.3–30.1), hypertriglyceridemia (OR 1.6, 95% CI: 1.1–7.2), and low high-density lipoprotein cholesterol (OR 1.3, 95% CI: 1.1–3.0).20 Data from Toyama Birth Cohort Study showed that a maternal FH of hypertension was positively associated with the risk of child overweight at age 12 (OR 1.21, 95% CI: 1.04–1.39). But there was no significant difference in the prevalence of overweight between children with a paternal FH of hypertension and those without.21 Gender is obviously an important factor in the interrelationship between hypertension and FH. However, the underlying mechanism of the gender-related difference is still unclear and needed future investigation. A study from Japan found that there is a significant partial correlation coefficient for familial disposition to hypertension only in women. This phenomenon was not observed in men.22 Some researcher came up with a hypothesis that a cardiovascular risk phenotype is transmitted on the maternal lineage with a pattern that indicates mitochondrial DNA-mediated inheritance,20 but there is still no conclusion, and require further study.
Participants with positive FH of hypertension had a series of anthropometric parameters including higher WC, BMI, and blood lipids than those without. And the related parameters showed a graded increase with the increasing number of generations who had hypertension. This is accordance with other similar studies. A Japanese study has found that the risk of obesity and overweight increased with the number of affected family members. The adjusted OR increased from 1.16 (95% CI: 0.99–1.35) to 1.42 (95% CI: 1.04–1.92) to 4.75 (95% CI: 1.35–16.69) as the number of family members with hypertension increased from 1 to 2 to 3.21 Also a France study found that parental histories of hypertension were significantly associated with cardiovascular risk.23 And there were also evidence showed that CVD and its death is increased in individuals with positive FH of hypertension.24 Therefore, the FH information could not only a tool for early prevention of hypertension but also useful for other CVDs. In addition, FH is a representative of gene variation and shared behaviors and environments, and the related information is easy to access. Considering the association between FH of hypertension and related CVDs, along with the easy accessibility and low cost, it is important and critical to identify FH of hypertension for prevention of hypertension and related diseases.
This study, which was conducted in a representative metropolitan area of rural Beijing, had strict training process and high response rate. The results showed that FH risk categories of first-degree relatives are strongly associated with the prevalence of hypertension and blood pressure level, even in the normal range. Most studies have revealed the association between FH and hypertension; our study did an in-depth study of the number of first-degree relatives affected, and showed not only positive or negative but also different FH risk categories are related with prevalence of hypertension. Third, this study explored the gender difference between the association of FH risk categories and hypertension, and a stronger association was revealed in women.
Also, this study had several limitations need to be considered. First, the nature of a cross-sectional study has its limitations on causal inference between FH risk categories and prevalence of hypertension, further cohort studies with follow-up data are necessary to strengthen the evidence. Second, the selected sample had a relatively high response rate (86.5%). There were no statistically significant differences in main characteristics (such as age, sex, education, marital status) between participants included in the study and those who did not. Third, the FH of hypertension was self-reported by participants, there were perhaps reporting bias and recall bias although a standard questionnaire was used and all the investigators were trained before involving in the field survey. Fourth, the gender difference in the association of FH risk categories and hypertension risk needs future investigations to explore the underlying mechanisms.
CONCLUSIONS
In summary, the present study showed a strong, independent association between FH risk categories of first-degree relatives of hypertension among Chinese community elderly population living in rural Beijing, even in the normal range of blood pressure level. It also provides additional evidence that FH is more closely associated with the risk of developing hypertension in women than in men. Screening and early prevention of hypertension should consider not only positive or negative but also the FH risk categories of hypertension.
Footnotes
Abbreviations: BMI = body mass index, CVD = cardiovascular disease, DBP = diastolic blood pressure, FBG = fasting blood glucose, FH = family history, HbA1c = glycerogelatin hemoglobin, HDL-C = high-density lipoprotein cholesterol, LDL-C = low-density lipoprotein cholesterol, SBP = systolic blood pressure, TC = total cholesterol, TG = triglyceride, WC = waist circumference.
ML, YH, and BJ contributed to the design of the study. All authors were involved in the analysis and interpretation of the data. JW, LW, YW, and DZ conducted the statistical analysis. ML, JZ, and YY worked on the drafting of the manuscript, which was thoroughly reviewed and approved by all the authors.
This study was supported by research grants from State Key Development Program of Basic Research of China (973 program, 2013CB530800), Beijing Municipal Science and Technology Commission (D121100004912003), Military Medicine Innovation Fund (13CXZ029), and Science Technological Innovation Nursery Fund of PLA General Hospital (13KMM26).
The authors have no conflicts of interest to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website (www.md-journal.com).
REFERENCES
- 1.Kearney PM, Whelton M, Reynolds K, et al. Global burden of hypertension: analysis of worldwide data. Lancet 2005; 36:217–223. [DOI] [PubMed] [Google Scholar]
- 2.Whelton PK. Epidemiology and the prevention of hypertension. J Clin Hypertens (Greenwich) 2004; 6:636–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weir MR. Hypertension and kidney disease. J Am Soc Hypertens 2014; 8:855–857. [DOI] [PubMed] [Google Scholar]
- 4.Lackland DT, Weber MA. Global burden of cardiovascular disease and stroke: hypertension at the core. Can J Cardiol 2015; 35:569–571. [DOI] [PubMed] [Google Scholar]
- 5.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA 2003; 290:199–206. [DOI] [PubMed] [Google Scholar]
- 6.Xi B, Liang Y, Reilly KH, et al. Trends in prevalence, awareness, treatment, and control of hypertension among Chinese adults 1991–2009. Int J Cardiol 2012; 158:326–329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang X, Bots ML, Yang F, et al. Prevalence of hypertension in China: a systematic review and meta-regression analysis of trends and regional differences. J Hypertens 2014; 32:1919–1927. [DOI] [PubMed] [Google Scholar]
- 8.Muldoon MF, Terrell DF, Bunker CH, et al. Family history studies in hypertension research. Review of the literature. Am J Hypertens 1993; 6:76–88. [DOI] [PubMed] [Google Scholar]
- 9.Winnicki M, Somers VK, Dorigatti F, et al. Lifestyle, family history and progression of hypertension. J Hypertens 2006; 24:1479–1487. [DOI] [PubMed] [Google Scholar]
- 10.Ranasinghe P, Cooray DN, Jayawardena R, et al. The influence of family history of hypertension on disease prevalence and associated metabolic risk factors among Sri Lankan adults. BMC Public Health 2015; 15:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tozawa M, Oshiro S, Iseki C, et al. Family history of hypertension and blood pressure in a screened cohort. Hypertens Res 2001; 24:93–98. [DOI] [PubMed] [Google Scholar]
- 12.Goldstein IB, Shapiro D, Weiss RE. How family history and risk factors for hypertension relate to ambulatory blood pressure in healthy adults. J Hypertens 2008; 26:276–283. [DOI] [PubMed] [Google Scholar]
- 13.Goldstein IB, Shapiro D, Guthrie D. Ambulatory blood pressure and family history of hypertension in healthy men and women. Am J Hypertens 2006; 19:486–491. [DOI] [PubMed] [Google Scholar]
- 14.Liu M, He Y, Jiang B, et al. Association between Serum Uric Acid Level and Metabolic Syndrome and Its Sex Difference in a Chinese Community Elderly Population. Int J Endocrinol 2014; 2014:754678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Writing Group of 2010 Chinese Guidelines for the Management of Hypertension. 2010 Chinese guidelines for the management of hypertension. Chin J Hypertens 2011; 19:701–743. [Google Scholar]
- 16.Li D, Lv J, Liu F, et al. Hypertension burden and control in mainland China: analysis of nationwide data. Int J Cardiol 2015; 184:637–644. [DOI] [PubMed] [Google Scholar]
- 17.Guo J, Zhu YC, Chen YP, et al. The dynamics of hypertension prevalence, awareness, treatment, control and associated factors in Chinese adults: results from CHNS. J Hypertens 2015; 33:1688–1696. [DOI] [PubMed] [Google Scholar]
- 18.Sit JW, Sijian L, Wong EM, et al. Prevalence and risk factors associated with prehypertension: identification of foci for primary prevention of hypertension. J Cardiovasc Nurs 2010; 25:461–469. [DOI] [PubMed] [Google Scholar]
- 19.Meng XJ, Dong GH, Wang D, et al. Epidemiology of prehypertension and associated risk factors in urban adults from 33 communities in China—the CHPSNE study. Circ J 2012; 76:900–906. [DOI] [PubMed] [Google Scholar]
- 20.Rodríguez-Moran M, Aradillas-García C, Simental-Mendia LE, et al. Family history of hypertension and cardiovascular risk factors in prepubertal children. Am J Hypertens 2010; 23:299–304. [DOI] [PubMed] [Google Scholar]
- 21.Liu J, Sekine M, Tatsuse T, et al. Family history of hypertension and the risk of overweight in Japanese children: results from the Toyama Birth Cohort Study. J Epidemiol 2014; 24:304–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kojima S, Murakami K, Kimura G, et al. A gender difference in the association between salt sensitivity and family history of hypertension. Am J Hypertens 1992; 5:1–7. [PubMed] [Google Scholar]
- 23.Lascaux-Lefebvre V1, Ruidavets JB, Arveiler D, et al. Influence of parental histories of cardiovascular risk factors on risk factor clusters in the offspring. Diabetes Metab 2001; 27:503–509. [PubMed] [Google Scholar]
- 24.Corvol P, Jeunemaitre X, Charru A, et al. Can the genetic factors influence the treatment of systemic hypertension? The case of the rennin–angiotensin–aldosterone system. Am J Cardiol 1992; 70:14–20. [DOI] [PubMed] [Google Scholar]


