Abstract
This study aims to describe global health training (GHT) programs through the ethical lens suggested by the Working Group on Ethics Guidelines for Global Health Training (WEIGHT). A total of 35 GHT programs were identified, and general information was obtained online. Semi-structured telephone interviews of key members of 19 programs were then conducted and transcribed. The interview guide was constructed using WEIGHT recommendations. Transcript data were grouped according to domains: reciprocity, trainee selection and preparedness, needs assessments, and ethical questions. Many programs expressed difficulty in building reciprocal relationships due to imbalanced power structures. Eleven programs reported no formal application process for selecting trainees. Twelve (63%) programs reported only a single day of preparation. Nine (47%) programs did not conduct a formalized needs assessment of partner sites. Ethical considerations varied from concerns for safety to inadequate training for residents. This study reveals the limited preparedness curricula and lack of formalized needs assessments among several programs. Although many programs make an effort to build reciprocal exchanges with host partners, experiences for foreign trainees within the United States are limited, and U.S. residents are often tasked with duties above their training level abroad. This study demonstrates the need to restructure how GHT programs are formed and operated.
Introduction
Over the course of the past decade, medical trainees have been seeking global health experiences in unprecedented numbers.1 In response to this, the scale and number of global health training (GHT) programs in medical schools and residencies have grown exponentially, and the number of ethical challenges faced by these programs have grown as well. These challenges are highlighted by the inherent nature of GHT programs: connecting medical trainees from the developed world with health professionals and patients from the developing world.2 This power imbalance is reminiscent of colonial medicine, a system that is rooted in racial and cultural superiority and has resulted in years of exploitation and mistrust globally.3 Because of this colonial history, present global health initiatives require a specific ethically derived framework to avoid these exploitive historical trends; however GHT activities are rarely shaped by such a framework.2,4 Global health program competencies are primarily focused on the global burden of disease and health care disparities; only 3.1% of medical schools who have global health curricula focus on developing a sense of social/ethical responsibility.5
The Working Group on Ethics Guidelines for Global Health Training (WEIGHT), whose members were selected based on expertise in GHT from a range of geographic locations, developed guidelines to help assess the potential benefits and harms of GHT programs.6 The first component of the guidelines suggests that programs should be developed so that “host and sender … derive mutual, equitable benefit.”6 WEIGHT guidelines describe the need for formal training of participants in GHT programs, with a focus on professionalism, standards of practice and cultural competence.6 The guidelines stress the selection process for the trainees, and recommend that trainees are selected based on their motivation to address global health issues, their sensitivity to local priorities, their training level and clinical competence so that they are assigned to activities appropriate to their skill set, and trainees who will be “good representatives of their home institution.”6
Obstetrics and Gynecology (OB/GYN) training programs have a special interest in global health as maternal health issues are a leading cause of death among women worldwide.1 Further there is strong interest in the availability of global health electives among medical students interviewing for OB/GYN residencies. The scope of GHT programs in OB/GYN has been previously described in a study in which the authors found 41 U.S. residency programs offer 69 global health-related activities, 33 of which are 6 weeks or less, 18 with research opportunities, and 10 with greater than 6 weeks of extended field-based training.1 These programs are distributed across 64 different countries with greater density around those with high burdens of disease.1 It is unknown how these programs approach the complexities of ethical engagement in global health work. Our goal was to explore GHT programs within OB/GYN residencies through the ethical framework presented by the WEIGHT group. The WEIGHT guidelines' application to GHT within a United States-based medical specialty has not previously been described. We will attempt to frame our description within a scientific and sociocultural context and give recommendations for both existing and future GHT programs.
Methods
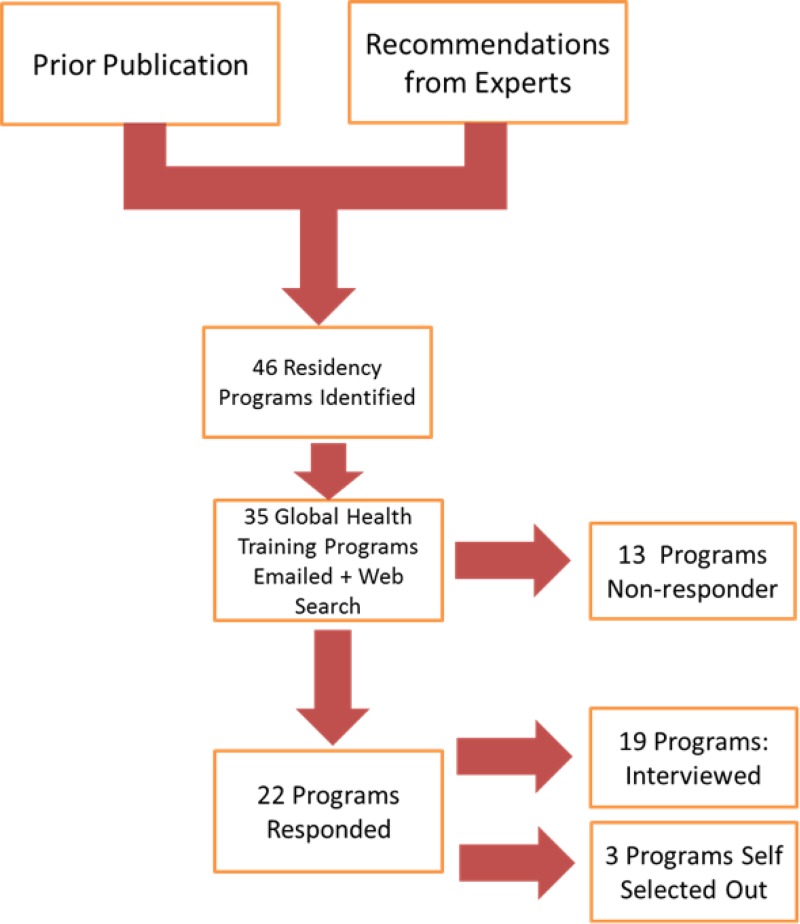
We designed a mixed method study to address our study objective. For the first part of our study, we implemented a two-part search protocol to identify OB/GYN residency programs that offered global health experiences. Programs were primarily identified through a prior publication whose methodology included a systematic website search of all the Accreditation Council for Graduate Medical Education accredited OB/GYN residency programs.1 Additional programs were identified by experts in the fields of global health and OB/GYN residency programs (Figure 1 ). A web-based search protocol was then used to identify websites that described these programs and to obtain program director contact information, program goals and objectives, trainee application requirements, trainee preparedness processes, and required deliverables from trainees. If a website for a GHT program was not identified, the OB/GYN department website was searched for program coordinator contact information.
Figure 1.
Identification and selection of global health training programs for study participation.
The second part of the study consisted of telephone interviews with faculty and staff of GHT programs. Program directors and coordinators of all programs identified from the search strategy were contacted through e-mail requesting participation in a 15–30 minute telephone interview. Two subsequent requests were sent to nonresponders over the course of 3 months. Interviews were conducted by a single researcher using the instrument shown in Figure 2 . The interview instrument was constructed using WEIGHT recommendations to assess the following areas: reciprocity, the trainee selection and preparedness process, needs assessment protocols, and ethical issues.
Figure 2.
Interview instrument for telephone interviews.
Data from the web-based search were analyzed for common themes, including published goals and objectives of GHT programs. The telephone interview responses were documented through careful note-taking during the conversation to capture values, meanings, beliefs, and experiences of the participant. These notes were then summarized immediately after the interview. Common themes from the interview summaries for each program were identified and grouped according to the following domains: general/background information, reciprocity, trainee selection, trainee preparedness, needs assessments, and ethical questions. Each domain was analyzed independently by two investigators for common themes and patterns as well as unique responses. These themes were compared for agreement and salient responses are reported. This study was deemed exempt by the Emory University institutional review board (IRB).
Results
Web-based search results.
Our search for programs found 46 residencies that offered global health rotations under 35 unique GHT programs: for example 1 residency system shared one global health program for all three of their residency sites. Overall, online information about GHT programs was very limited. Of the 35 programs identified, 10 program websites provided no specific details about programmatic activities. Of the remaining programs, 16 programs listed goals that included delivering care to underserved populations abroad and providing U.S. students, residents and faculty with international experiences to broaden their training. Three programs' goals involved facilitating an exchange with host institutions and strengthening collaborations with faculty abroad.
In-depth interview results.
Of the 35 programs requested to participate, 22 (63%) responded with 3/22 declining participation. Nineteen interviews were conducted with global health program directors, program coordinators, program faculty, and OB/GYN department chairs (Table 1). Results from the in-depth interviews are summarized below by domain evaluated.
Table 1.
Demographics of global health training programs interviewed (N = 19)
| Institution | Program name | Interviewed | OB/GYN specific | Sites | Length of program | Age of program |
|---|---|---|---|---|---|---|
| Brigham and Women's/MGH | MGH Center for Global Health | Program faculty | No | Uganda | 1 month | 2006 |
| Brigham and Women's/MGH | Harvard Humanitarian Initiative | Program director | No | Various | 1 month | 2004 |
| Brown University | Global Health Initiative | Program coordinator | No | Various | 1 month | 2009 |
| Case Western Reserve University | The Women and Newborns Didactic, Outreach, Opportunities and Research Program | Program director | Yes | Guyana | 30 months | 2009 |
| Emory University | Global Health Residency Scholars Program | Department chair, OB/GYN | No | Ethiopia | 1 year | 2012 |
| Indiana University | IU Center for Global Health | Department chair, OB/GYN | No | Kenya | 1 month/4 years | 1989 |
| Kaiser Permanente Medical Group | The KP Global Health Program | Program director | No | Various | 2 weeks–1 month | 2010 |
| Michigan State University | The Global Reproductive Health Training Program | Program director | Yes | Costa Rica | 1 month | 2010 |
| NYU School of Medicine | The NYU Division of Global Women's Health | Program director | Yes | Ghana | 1 month | 2012 |
| UCSF | Global Health Sciences Clinical Scholars Program | Program coordinator | No | Various | 2 months | 2006 |
| Upenn | Botswana-Upenn Partnership | Associate program director | No | Botswana | 1 month | 2001 |
| Yale-New Haven Medical Center | Yale/Stanford Johnson and Johnson Global Health Scholars Program | Program coordinator | No | Various | 6 weeks | 1981 |
| Greenville Health System | Department chair, OB/GYN | Yes | Columbia | 1 week | ||
| Maine Medical Center | Department chief, OB/GYN | Yes | Various | 2 weeks | 2004 | |
| Mayo Clinic | Mayo International Health Program | Program Director | No | Various | 1 month | 2000 |
| Mount Sinai University | Global Health Resident Track | Program director | Yes | Various | 4–6 weeks | 2009 |
| Stanford University | Eritrean Women's Health Project | Program director | Yes | Eritrea | 2000 | |
| University of North Carolina | Division of Global Women's Health | Program faculty | Yes | Malawi and Zambia | 4 weeks | 2008 |
| University of Michigan | Ghana Postgraduate OB/GYN Program | Program director | Yes | Ghana | 4–6 weeks | 1994 |
OB/GYN = obstetrics and gynecology; IU = Indiana University; KP = Kaiser Permanente; NYU = New York University; UCSF = University of California, San Francisco.
Reciprocity.
GHT programs reported diverse methods to promote reciprocal relationships between their own institutions and host country institutions (Table 2). The most frequently reported example of reciprocity was an exchange where host residents or staff travel to the United States for 4–6 week long “observerships” to observe care delivery or to study topics such as business administration, library management, and health facility management. Programs participating in exchanges described difficulties in obtaining licensure agreements in the United States for international residents to directly care for patients citing legal and liability concerns.
Table 2.
Reported examples of reciprocity by global health training programs per telephone interviews
| Reported examples of reciprocity | Number of programs (N = 19) |
|---|---|
| Exchange program | 9 |
| Resident deliverables: lectures, new protocols, research results | 8 |
| Clinical training programs for hosts | 6 |
| Building host research capacity | 6 |
| Sustained presence | 6 |
| Supplies/equipment | 3 |
| “Giving back” | 2 |
| “3rd world medicine experience” for U.S. Residents | 2 |
Trainee deliverables to host partner institutions were also described as examples of reciprocity, including lectures given by residents to students and residents at host sites. Two programs required residents to write, teach, and train host partners in new evidence-based protocols addressing medical issues faced by the host partners.
Several GHT programs described the commitment to build clinical and research capacity. Examples of clinical capacity building included starting a host country OB/GYN residency or OB/GYN-related fellowships, supporting scholarships for host country medical students, and developing training programs for skilled birth attendants. Research capacity building included developing and refining databases at host institutions and collaborating with host partners on research manuscripts.
Several programs described the importance of sustaining a long-term presence at host sites as a foundational aspect in building a reciprocal relationship. Three programs described the provision of consumables as part of the reciprocal relationship. One program supplies each host resident with a cryogun, while another described taking 600 lbs of equipment to the host country annually.
A few of the programs interviewed described aspects of the resident training program itself as satisfying a reciprocal relationship. Two programs stated that the programs were “giving back” to host partners by sending residents. The programs described the clinical care delivered to host country populations as the basis of a balanced and equitable partnership. One program stated that their host country gained “the clinical expertise of the [program's] faculty.” Another program also stated that the segment of the beneficiaries of their program “wouldn't have surgery if [we] weren't there.” Several programs also mentioned that the U.S. residents benefited by gaining exposure to medicine in a low resource setting through the degree and volume of various illnesses seen abroad, as well as through gaining a greater appreciation for the quality of U.S. medical care and resources.
Of the 19 programs interviewed, seven programs' initial response to the interview question addressing reciprocity was that reciprocal relationships in GHT programs are difficult to develop. One program's director stressed to residents to “do no good whatsoever,” urging residents to dispel expectations that their short engagements abroad can provide sustainable, significant impact in their host communities. Two programs mentioned that GHT programs inherently benefit U.S. residents more than host partners.
Trainee selection.
The selection process for residents who are interested in a global health experience varied among programs. Unanimously, programs reported the resident must be greater than a PGY1 and in good standing with their program directors. 11 of the 19 programs had no further application requirements. Programs with application requirements described letters of recommendation, essays, and interviews in which cultural sensitivity issues are addressed. One program required the residents to be fluent in the host country's language. No program mentioned prior global health experience as a requirement to participate. One program described host institutions' faculty as part of the process in selecting applicants.
Trainee preparedness.
GHT programs reported a varied approach to prepare residents for international electives. Twelve of the 19 programs (63%) reported a single day of orientation for residents. Single-day orientation for residents usually consisted of informal conversations with the program director and previous participants covering practical issues of living abroad. The remaining seven programs reported having some form of extended coursework that residents were required to complete before going abroad. Preparation materials reported include online courses and modules, textbooks, and case study discussions. Programs with extended curricula were more likely to cover topics of cultural competency, health and safety, standards of practice, professionalism issues, and ethical issues than programs who had a single-day orientation (Figure 3 ). Several of the programs with extended curricula give the residents a certificate in global health on completion of the course work.
Figure 3.
Frequency of topics covered in preparedness curricula volunteered by global health training programs during telephone interviews.
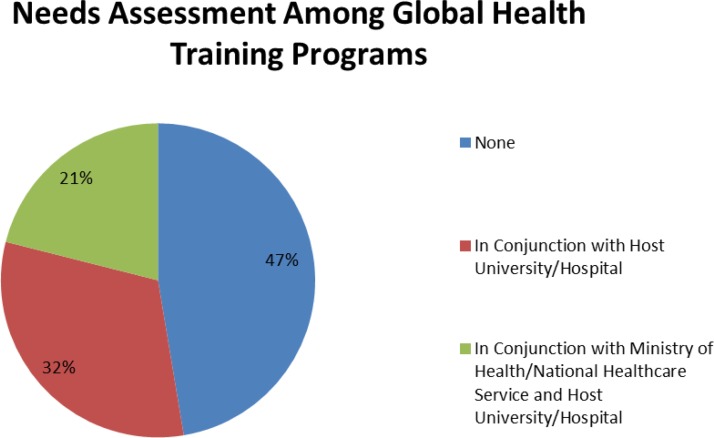
Needs assessment.
Participants reported a wide variety of approaches to completing a needs assessment to inform the structure and focus of their respective programs (Figure 4 ). Programs with no formalized needs assessment relied on host partners to assess health-care needs, and generally focused solely on delivering care to local populations. Programs that described a formal needs assessment done in conjunction with host university/hospital systems or the ministry of health described needs that were beyond simple care delivery. Almost all of these programs reported host institutions describing a need for increased medical education and training for students, residents and faculty at the host country as well as help with designing and developing research infrastructure, specifically databases and computer programs. None of these programs reported host institution need for supplies or medical equipment.
Figure 4.
Proportion of global health training programs completing formalized needs assessments per telephone interview results.
Ethical issues reported by programs.
Ethical questions and situations reported by global health programs were diverse. Multiple programs described situations in which residents and trainees were not prepared to perform certain procedures they were requested to do. In one reported example, a U.S. resident reported to a hospital and the host provider left the site for several hours with the expectation the resident could oversee the patient care. Several programs described ethical questions surrounding issues of short-term engagement. One program changed their policy to exclude surgical “hit and run” mission trips from their global health program, unless the surgical focus and cases themselves were guided by the host country's national health-care system. Another program described concern for potentially burdening an already burdened health system with residents who cannot speak the host language and could divert resources for translation or other resident-related needs away from patient care. A few programs mentioned ethical issues with the host country's medical practice. One program described having to reconcile a cultural practice where all women are “forced” to undergo tubal ligation after 2 C-sections with their own standards of practice. Two programs described concerns with the ethical conduct of research; for example, one program mentioning that a resident had been accused of taking protected research material without IRB approval from the host country. A total of 32% of the programs interviewed reported having no ethical questions or situations.
Discussion
The current landscape of GHT within residency programs is ripe for tremendous growth and development, but also fraught with complex ethical concerns. Although the vast expansion in interest in global health inequities appears to be a contemporary phenomenon, with the number of university of global health programs increasing 10-fold within the past 10 years, a critical analysis of these programs must be performed with proper sociohistorical context.7 To better understand GHT programs, it is necessary to frame their existence on a continuum with former colonial rule and colonial medicine.3 The legacy of colonial projects are rooted in exploitation of indigenous peoples, and understanding the rifts that were created in the past is imperative in analyzing current GHT projects within an ethical framework.3 All programs that participated in our study had a variety of methods to manage issues of reciprocity, needs assessments, and trainee preparedness and selection.
The importance of building reciprocity within GHT programs is both to ensure equitable benefits to all stakeholders and to fight the historical precedence of exploitation of high-income countries of low- to middle-income countries.6 As our data illustrate, the construction of truly reciprocal relationships within training programs is challenging. GHT programs inherently focus on the trainees' experiences abroad, and the benefits of participation for the resident and the sending institution.8 Residents in previous studies have reported numerous personal benefits of GHT programs that lead them to care for immigrants and underserved patients in the future.9 These good intentions however often lead to safety challenges for patients in global communities, and the global health experience can create more distrust in those communities for foreign health workers.8,10
To circumvent these potentially imbalanced training structures, many programs have focused on building research capacity and transferring skills associated with scientific research within host countries as a way to foster sustainable partnerships. Obtaining specific information about research projects associated with the programs in this article was beyond the scope of our study. Historically, however, many research projects initiated by western groups serve the objectives of the western partners rather than the host programs' objectives.11 A recent study that explored Ugandan trainees' views of global health collaborations demonstrated that only 15% of trainees felt that research projects undertaken by international groups were done in highest priority areas of Uganda.12 This demonstrates how research projects often fail to serve the needs of the host country communities. Many of the programs that were interviewed in our study also described the importance of sharing authorship of published results with host partners. Significant barriers exist, however, that prevent host partners from primary authorship including lack of guidance for ranking authors and editorial bias that favors well-known western authors.13 This is evidenced further by the previous mentioned study of Ugandan trainees where only 28% of the trainees reported participation in collaborative research with visiting groups, and none reported publishing an article as a coauthor.12 Subsequent studies are necessary to evaluate how GHT programs identify research questions and handle issues of authorship. Several participating programs identified donations of equipment and supplies to host partners as a component of reciprocity. Supplies donation to resource poor areas has a history of failure in multiple settings due to inappropriateness and lack of basic maintenance ability.14,15 Often when drugs are donated without appropriate consideration, they create additional public health issues for host communities and local economies are burdened with the cost of destruction of the excess substances.16,17 Medical supplies, without appropriately trained staff and identified needs for those items, can also be economically costly and useless to host communities.18 GHT programs that offer supplies or medications to host partners would best serve interested communities through a joint assessment to determine the priority needs for equipment as well as the host institution's capacity to appropriately store, manage, distribute, use, and maintain potential donations. Ongoing monitoring and evaluation of use and impact of donations may serve to further inform both sending and host partners.
Although imbalanced training structures, research, and supplies donation all have pitfalls in creating equitable, reciprocal relationships, a marked, problematic example of reciprocity was demonstrated by programs' descriptions of their clinical care as the sole crux of their reciprocal relationship. Many of these programs described “giving back” to host communities through the clinical work they do for the communities. Both the language of “giving back” and the attitude that the delivery of western medicine alone is a substantial contribution are reminiscent of the attitudes of missionary medicine in the colonial era.19 These attitudes reinforce patronizing and paternalistic relationships and engender mistrust among host communities of foreign workers, as they recall imperialistic pursuits of the past and present.20
To match host needs with programmatic objectives and activities, it is important to conduct a needs assessment before initiating clinical work. Nearly half of the participants in our study did not report completion of a formal needs assessment. The absence of a needs assessment can lead to misguided engagement in activities that compromise the quality and coordination of international efforts, and subsequently may bolster existing perceptions that short-term medical missions do little to address actual health needs of the community.18,21 Needs assessments done in conjunction with leaders of the host communities can help guide efforts to build local capacity and reinforce sustainable models of quality health care.10,22,23 Empowering host community leaders in this way, from the inception of GHT programs, can mitigate neocolonial trends in GHT so that the allocation of foreign expertise and skills is done in a manner that does not undermine capacity building in host communities.
Residents' experiences in health care abroad can be starkly different from their experiences within the United States, and an adequate level of preparedness is essential to mitigate the transition between cultures. Sixty-three percent of the programs interviewed in our study stated that there was a single day of orientation before going abroad, an inadequate time frame in which to address issues of cultural competency, health and safety, language, standards of practice, and ethics. This is reflective of global health electives across specialties nationally that often do not include comprehensive, country-specific preparedness.24 Insufficient preparedness can lead to unprofessional behavior, a lack of cultural awareness, and mistrust between program participants and community members, all of which can quickly unravel carefully built collaborations or stunt potential collaborations before they have had a chance to develop.10 Several of the programs interviewed, however, did have required structured and extended curricula before global health experiences. An assessment of the feasibility and effectiveness of these curricula to adequately prepare trainees was beyond the scope of this study, but could be an important area of further exploration.
Trainees who travel to host communities in GHT programs are representatives of their own U.S. institutions. Most of the programs interviewed noted there was no application requirement for trainees interested in going abroad. WEIGHT guidelines state that GHT programs should “select trainees who are adaptable, motivated to address global health issues, sensitive to local priorities, willing to listen and learn, whose abilities and experience matches the expectations of the position, and who will be good representatives of their home institution and country.”3 Although many programs described soft criteria for selecting trainees such as flexibility and good work ethic, there is no formalized method to assess how trainees will perform abroad and deal with cultural issues. Skills needed to practice medicine in resource poor settings demand a high level of clinical and surgical skill that is often profoundly different from the skill set taught and needed in the United States.25 An honest and thorough evaluation of residents' intentions, cultural sensitivity, and technical proficiency should be sought before global health experiences.
This study demonstrates the first known application of the WEIGHT guidelines to residency-based GHT programs nationally in any specialty. Although our study was focused on OB/GYN residency programs, our findings are not restricted to OB/GYN programs as many of those programs included in our study are not OB/GYN specific. Our study was limited to web-based data and interviews with sending program leaders and does not include any data on host institution or beneficiaries' experiences with and perceptions of visiting residents and sending institutions' activities. This dimension of GHT engagement will be important to study as a measure of perceived benefit, equity, and balance. Although over half of the programs we approached participated, the nonresponse rate of 37% may limit our results. Further, only one spokesperson for each program was interviewed; multiple perspectives of the same program may have added richness to our results. Most importantly, to create a full picture of ethical engagement in GHT programs, assessments of host partners', host beneficiaries' and residents' experiences and perceptions, program cost-effectiveness, and impact are all necessary. We recognize that this study comes strictly from the perspective of U.S. investigators, so host country perspectives will be crucial in shaping further research.
On the basis our data, the WEIGHT guidelines and the literature of global health ethics described above, we have developed a set of recommendations that can be used by both new and existing GHT programs (Table 3).
Table 3.
Recommendations for current and future GHT programs
| 1. Execute a needs assessment lead by host country partners at institutional and/or national levels |
| 2. Define goal, objectives, intended beneficiaries, expected impact, monitoring and evaluation plan, and expected deliverables |
| 3. Create balanced activities that form equitable relationships between counterparts that is exchanging observerships between U.S. residents and host residents |
| 4. Use a comprehensive resident selection process that takes into account cultural awareness, intentions, motivations and skills |
| 5. Use in-depth pre-departure curriculum to address: cultural issues, historical context, host country health guidelines and protocols, and how the GHT program fits within the health system landscape |
| 6. Consider if GHT activities can be accomplished with local capacity, and if not, consider how to build capacity |
| 7. Confirm that any clinical activity comply with host country licensure protocols and that residents are supervised closely by host country providers, with minimal diversion of resources away from host country learners or patients |
| 8. Verify that research efforts are led by host country partners, comply with host country IRB standards, and any published results include host country authors |
| 9. Create a culture of self-reflection and thoughtful regular critique throughout the lifetime of the program, with regular examination of the intended and unintended consequences |
GHT = global health training; IRB = institutional review board.
Conclusion
Interest in participating in GHT electives during OB/GYN residencies has grown exponentially in the past decade, and with that has grown the responsibility of both sending and host institutions to carefully design, implement, monitor, and evaluate these electives from the perspectives of all stakeholders. Our data illustrate that currently GHT programs are not, for the most part, following WEIGHT guidelines in both designing and implementing programmatic activities. Training programs can refocus their energies to build truly reciprocal relationships by completing through needs assessments with host partners. Programs can also focus on selecting residents and preparing residents for international experiences so that all work is elevated and maintained at the highest standards of ethical conduct in global health.
Footnotes
Authors' addresses: Mohammad Y. Zaidi, Emory University School of Medicine, Atlanta, GA, E-mail: mhmmd.y.zaidi@gmail.com. Lisa Haddad and Eva Lathrop, Department of Gynecology and Obstetrics, Emory University School of Medicine, Atlanta, GA, E-mails: lisa.haddad@emory.edu and elathro@emory.edu.
References
- 1.Hung KJ, Tsai AC, Johnson TR, Walensky RP, Bangsberg DR, Kerry VB. Scope of global health training in U.S. obstetrics and gynecology residency programs. Obstet Gynecol. 2013;122:1101–1109. doi: 10.1097/AOG.0b013e3182a9c1c8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pinto AD, Upshur RE. Global health ethics for students. Developing World Bioeth. 2009;9:1–10. doi: 10.1111/j.1471-8847.2007.00209.x. [DOI] [PubMed] [Google Scholar]
- 3.Farmer P, Kim JY, Kleinman A, Basilico M. Reimagining global health: an introduction. 2013;Vol. 1:15–74. [Google Scholar]
- 4.DeCamp M, Rodriguez J, Hecht S, Barry M, Sugarman J. An ethics curriculum for short-term global health trainees. Global Health. 2013;9:5. doi: 10.1186/1744-8603-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Battat R, Seidman G, Chadi N, Chanda MY, Nehme J, Hulme J, Li A, Faridi N, Brewer TF. Global health competencies and approaches in medical education: a literature review. BMC Med Educ. 2010;10:94. doi: 10.1186/1472-6920-10-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crump JA, Sugarman J, Working Group on Ethics Guidelines for Global Health Training (WEIGHT) Ethics and best practice guidelines for training experiences in global health. Am J Trop Med Hyg. 2010;83:1178–1823. doi: 10.4269/ajtmh.2010.10-0527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Merson MH. University engagement in global health. N Engl J Med. 2014;370:1676–1678. doi: 10.1056/NEJMp1401124. [DOI] [PubMed] [Google Scholar]
- 8.Sawatsky AP, Rosenman DJ, Merry SP, McDonald FS. Eight years of the Mayo International Health Program: what an international elective adds to resident education. Mayo Clin Proc. 2010;85:734–741. doi: 10.4065/mcp.2010.0107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mosepele M, Lyon S, Dine CJ. Mutually beneficial global health electives. Virtual Mentor. 2010;12:159–166. doi: 10.1001/virtualmentor.2010.12.3.ccas2-1003. [DOI] [PubMed] [Google Scholar]
- 10.Laabes EP, Desai R, Zawedde SM, Glew RH. How much longer will Africa have to depend on western nations for support of its capacity-building efforts for biomedical research? Trop Med Int Health. 2011;16:258–262. doi: 10.1111/j.1365-3156.2010.02709.x. [DOI] [PubMed] [Google Scholar]
- 11.Elobu AE, Kintu A, Galukande M, Kaggwa S, Mijjumbi C, Tindimwebwa J, Roche A, Dubowitz G, Ozgediz D, Lipnick M. Evaluating international global health collaborations: perspectives from surgery and anesthesia trainees in Uganda. Surgery. 2014;155:585–592. doi: 10.1016/j.surg.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 12.Smith E, Hunt M, Master Z. Authorship ethics in global health research partnerships between researchers from low or middle income countries and high income countries. BMC Med Ethics. 2014;15:42. doi: 10.1186/1472-6939-15-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Howie SR, Hill SE, Peel D, Sanneh M, Njie M, Hill PC, Mulholland K, Adegbola RA. Beyond good intentions: lessons on equipment donation from an African hospital. Bull World Health Organ. 2008;86:52–56. doi: 10.2471/BLT.07.042994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee PD. The role of appropriate medical technology procurement and user maintenance instructions in developing countries. J Clin Eng. 1995;20:407–413. doi: 10.1097/00004669-199509000-00016. [DOI] [PubMed] [Google Scholar]
- 15.van Dijk DP, Dinant G, Jacobs JA. Inappropriate drug donations: what has happened since the 1999 WHO guidelines? Educ Health (Abingdon) 2011;24:462. [PubMed] [Google Scholar]
- 16.World Health Organization Guidelines for drug donations. Geneva, Switzerland: WHO 1999. Report No.: WHO/EDM/PAR/99.4. Fisher D. Regulating the helping hand: improving legal preparedness for cross-border disaster medicine. Prehosp Disaster Med. 2010;25:208–212. doi: 10.1017/s1049023x00008037. [DOI] [PubMed] [Google Scholar]
- 17.Loewenberg S. Medical missionaries deliver faith and health care in Africa. Lancet. 2009;373:795–796. doi: 10.1016/s0140-6736(09)60462-1. [DOI] [PubMed] [Google Scholar]
- 18.Tropical medicine: a brittle tool of the new imperialism. Lancet. 2004;363:1087. doi: 10.1016/S0140-6736(04)15928-X. [DOI] [PubMed] [Google Scholar]
- 19.Green T, Green H, Scandlyn J, Kestler A. Perceptions of short-term medical volunteer work: a qualitative study in Guatemala. Global Health. 2009;5:4. doi: 10.1186/1744-8603-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bloom BLE. Fulfilling the Promise: How National Societies Achieve Sustainable Organizational Development: A Multi-Country Study. Geneva, Switzerland: International Federation of the Red Cross; 2011. pp. 1–42. [Google Scholar]
- 21.Baranick E, Baird A, Vinze A. An economic framework for transitioning to capacity building. Glob Public Health. 2014;10:15–27. doi: 10.1080/17441692.2014.964745. [DOI] [PubMed] [Google Scholar]
- 22.Miranda JJ, Yudkin JS, Willott C. International Health Electives: four years of experience. Travel Med Infect Dis. 2005;3:133–141. doi: 10.1016/j.tmaid.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 23.Ajayi OO, Adebamowo CA. Surgery in Nigeria. Arch Surg. 1999;134:206–211. doi: 10.1001/archsurg.134.2.206. [DOI] [PubMed] [Google Scholar]