Abstract
The Amazon is responsible for approximately 40% of the American tegumentary leishmaniasis (ATL) in Brazil. Herein the sustained presence of ATL in Manaus, the largest settlement in the Amazon, was investigated. Records of notification of historic cases, and data from cases prospectively enrolled in the Tropical Medicine Foundation of the Amazonas State were used. Geographic coordinates of prospective patients' living sites were used to detect inner-city clusters of ATL. Infecting Leishmania species was determined by polymerase chain reaction. Among prospectively enrolled subjects, 94.8% were infected with Leishmania (Viannia) guyanensis, 76.7% were male, 30.2% were 0–20 years old, and 69.8% had an urban residence. Historic cases showed a profile similar to that of prospectively enrolled subjects. Several clusters of ATL, widely distributed within the city of Manaus, could be detected. In conclusion, there was a high frequency of disease in young age groups and cases clustered in urban neighborhoods. It cannot be determined from these data whether transmission of these cases occurred within or outside the city of Manaus.
Introduction
The burden of leishmaniasis accounts for about 2 million disability-adjusted life years worldwide.1 Of all cases of tegumentary forms of leishmaniasis, 90% concentrate in five countries including Brazil,2 where the number of new cases notified per year varied from 18,226 to 28,737 in the decade of 2004 to 2013.3,4
American visceral leishmaniasis (AVL) reportedly is more likely to occur in urban areas than the tegumentary form of the disease (ATL).5 Major urban centers in Brazil such as the capital cities of Fortaleza, Natal, and Belo Horizonte have well-documented endemicity of AVL.6–8 It has been assumed that ATL more commonly affects rural populations, small towns of the countryside, or the periphery of larger settlements.
The Amazon is responsible for approximately 40% of the ATL cases in Brazil. In 2013, roughly 12,000 of 18,000 Brazilian cases of ATL occurred in that region.4 Leishmania (Viannia) guyanensis is the most prevalent parasite in the region.9 The city of Manaus is the largest human settlement located within the Amazon rain forest, with a population of approximately 1.7 million inhabitants. Early descriptions indicated that ATL is transmitted to human beings either within or in regions surrounding rain forest10 or in the peridomiciles of those individuals living in the outskirts of the city.11
In the large population of Manaus, an average of 700–800 cases of ATL are reported every year.12 The purpose of this study was to investigate the location of ATL cases within Manaus to determine whether there was localized clustering that might provide clues to the mode of transmission.
Materials and Methods
Study site.
The research was conducted at the Tropical Medicine Foundation of the Amazonas state (FMTAM) in Manaus. FMTAM diagnoses and treats 1,000 cases of ATL, on average, per year.
Patients.
A total of 185 consecutive cases of ATL, attending the outpatient dermatology clinics in FMTAM between January 2008 and August 2010, were enrolled. ATL was confirmed in all cases by direct microscopic examination and histopathology of Giemsa-stained specimens from skin lesions, followed by parasite identification in biopsies with L. (Viannia)-specific polymerase chain reaction restriction fragment length polymorphism (PCR-RFLP).13,14
Inclusion criteria consisted of any individual that had microscopically confirmed infection with Leishmania spp., who consented to participate in the study. Subjects with Leishmania spp. infection but negative L. (Viannia) PCR-RFLP were presumed to be infected with an alternate species, and thus were dropped from the study. After inclusion/exclusion criteria were applied, the study sample consisted of 172 subjects infected with L. Viannia spp. parasites.
ATL cases were classified into urban or rural according to their residence (i.e., their home addresses). Cases whose homes were within the official city limits were defined as urban, whereas those living outside these borders were defined as rural.
Discrimination of Leishmania species by PCR-RFLP of the HSP-70 locus.
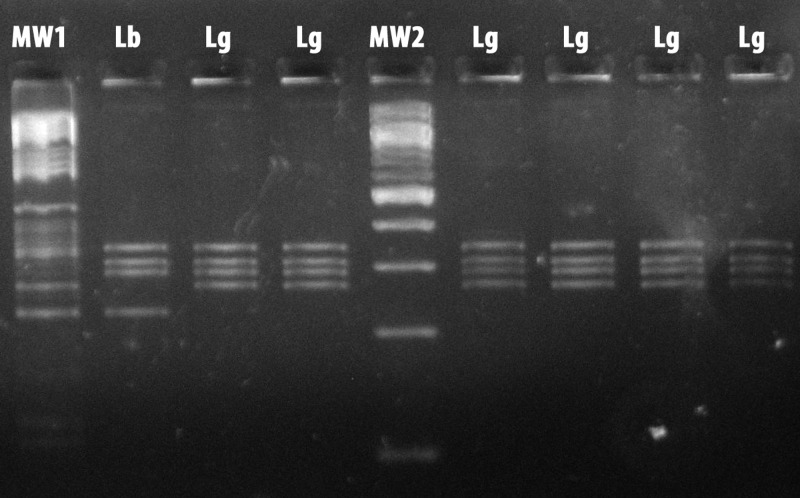
Discrimination between Leishmania (Viannia) braziliensis and L. (V.) guyanensis used PCR-RFLP, targeting the genomic HSP-70 locus. PCR-RFLP was performed on skin biopsy specimens from all subjects, following previously reported protocols.13,14 A representative picture of a gel containing electrophoretic patterns of L. (V.) guyanensis and L. (V.) braziliensis DNA samples submitted to this PCR-RFLP protocol is shown in Figure 1 .
Figure 1.
Representative photograph of an agarose gel showing electrophoretic patterns of Leishmania (Viannia) guyanensis and Leishmania (Viannia) braziliensis HSP-70 polymerase chain reaction restriction fragment length polymorphism (PCR-RFLP). Reactions were performed as described in references.13,14 MW = molecular weight markers; Lg = L. (V.) guyanensis; Lb = L. (V.) braziliensis.
Geographic positioning of ATL cases.
High-resolution spatial positioning of urban ATL cases enrolled at FMTAM was determined by acquisition of geographic coordinates of patients' residences, using a Brunton Multi-Navigator global positioning system apparatus (The Brunton Co., Louisville, CO). This apparatus has a range of precision of 15 m. Collected data were plotted onto a high-definition satellite photograph of Manaus (INPA, Brazil) with the geographic information system (GIS) ArcInfo Version 8.3 (Environmental Systems Research Institute Inc., Redlands, CA) for visual inspection.
Clustering of cases within neighborhoods of Manaus was detected by Kernel analyses with software built into the GIS package. Kernel analysis was performed overlaying the shape file containing the population densities of different neighborhoods onto the raster file with the geo-referenced photograph of the city, to reflect the diverse population densities found in Manaus.
To compare the frequency of ATL cases occurring close to forests with the frequency of cases from individuals living in non-forested areas of the city, we used the GIS measurement tool. We determined the distance from the living site of each patient to the closest forest patch. Then the patients were classified as living within or beyond 500 m from the forest.
Additional ATL case information was derived from historic data from patients diagnosed with the disease in Manaus between 2001 and 2009. The age and geographic distribution of these historic cases of ATL were evaluated from health records from Manaus between 2001 and 2009. These public health records are maintained in the Brazilian Ministry of Health SINAN database.15 Historic cases were classified according to their rural or urban residence and the age divided into intervals: 01–10, 11–20, 21–30, 31–40, 41–50, 51–60, 61–70, and > 70 years of age. The number of ATL cases among age intervals was compared by Student's t test.
Human study approval.
The research was approved by FMTAM Institutional Review Board.
Results
Characterization of the ATL patients enrolled at FMTAM, Manaus.
Among the 185 enrolled patients, the distribution of ATL caused by different L. Viannia species (PCR+ plus PCR−), consisted of 88.6% (N = 163) L. (V.) guyanensis, 4.9% (N = 9) L. (V.) braziliensis, and 6.5% (N = 13) of non-Viannia infected individuals or individuals with non-detectable parasites. Liver infusion tryptose/Novy, McNeal and Nicolle (LIT/NNN) culturing was positive in lesion biopsy specimens from 59% (N = 97) of L. (V.) guyanensis, 66% (N = 6) of L. (V.) braziliensis, and 0% of L. (Viannia) PCR-negative patients.
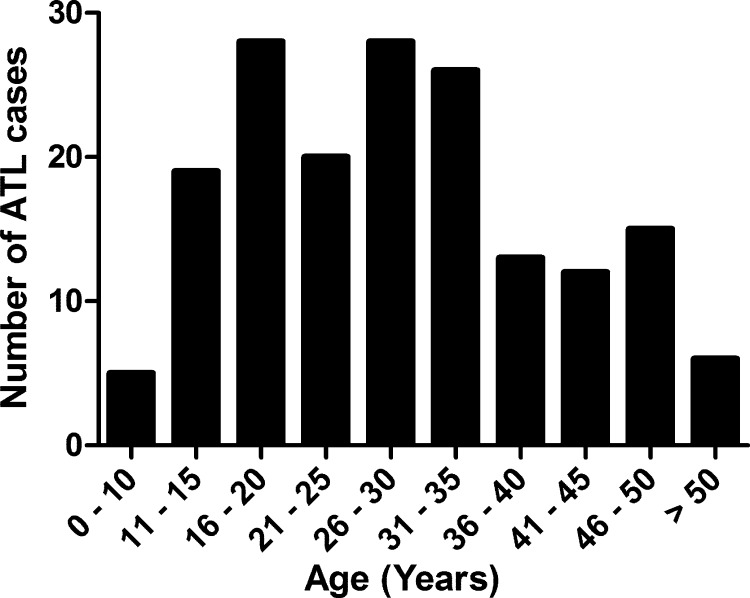
Of the 172 subjects effectively included in the study, nine (5.2%) were infected with L. (V.) braziliensis and 163 (94.8%) were infected with L. guyanensis; 132 (76.7%) were male; and 120 (69.8%) lived within the city of Manaus (herein defined as urban cases). Ages varied from 5 to 65 years (mean 29). Of note, a large proportion of these ATL cases belonged to the age stratum 0–20 years (N = 52; 30.2%). About half of these subjects were 15 years old or younger (N = 24) (Figure 2 ).
Figure 2.
Age distribution of 172 cases of American tegumentary leishmaniasis (ATL) diagnosed in the dermatology clinic of Tropical Medicine Foundation of the Amazonas State (FMTAM), Manaus, between January 2008 and August 2010.
Historic profiles of ATL patients diagnosed in Manaus.
To verify that the cross-section of prospectively enrolled study subjects reflected the actual profile of tegumentary leishmaniasis cases seeking health care in the region, we analyzed historic cases of ATL diagnosed in Manaus between 2001 and 2009, reported to the Brazilian Ministry of Health, and listed in the SINAN database.15
A total of 9,510 cases were reported during this period; 67% lived within the city of Manaus (urban cases) and 76% were male. Their detailed distribution stratified by age and place of residence are described in Table 1. Urban and rural cases had similar age distributions, with 35% (3,344 of 9,510 cases) occurring in the youngest (1–20 year) age group. Furthermore, the majority of urban residents that were diagnosed with ATL were consistently distributed across all age groups.
Table 1.
ATL cases notified in the city of Manaus and listed in the SINAN database of the Brazilian Ministry of Health between 2001 and 2009, stratified by place of residence
| Age strata | Number of ATL cases notified between 2001 and 2009 | |
|---|---|---|
| Urban | Rural | |
| 0–10 | 782 | 477 |
| 11–20 | 1,416 | 669 |
| 21–30 | 1,647 | 771 |
| 31–40 | 1,123 | 553 |
| 41–50 | 776 | 401 |
| 51–60 | 410 | 187 |
| 61–70 | 154 | 81 |
| > 70 | 45 | 18 |
ATL = American tegumentary leishmaniasis.
The yearly incidence of urban ATL in Manaus from 2001 to 2009 in the 0–20 or 21–40 age intervals is shown in Table 2. There were 244 ± 45 or 308 ± 37 (mean ± standard deviation) cases in the 0–20 or 21–40 age groups, respectively. Interestingly, the difference between the two groups was not significant (Student's t test P = 0.3).
Table 2.
Urban ATL cases notified in the city of Manaus and listed in the SINAN database of the Brazilian Ministry of Health between 2001 and 2009, stratified by age groups
| Year | Number of ATL cases notified per age group* | |
|---|---|---|
| 0–20 years | 21–40 years | |
| 2001 | 333 | 345 |
| 2002 | 301 | 349 |
| 2003 | 539 | 562 |
| 2004 | 185 | 245 |
| 2005 | 178 | 274 |
| 2006 | 229 | 299 |
| 2007 | 226 | 313 |
| 2008 | 111 | 207 |
| 2009 | 96 | 176 |
| Total | 2,198 | 2,770 |
ATL = American tegumentary leishmaniasis.
Student's t test P > 0.05 for the comparison of average number of ATL cases between the two age groups.
Overall, the profile displayed by historic cases of ATL is in rough agreement with that of the subjects prospectively enrolled at FMTAM.
Geographic distribution of ATL in Manaus.
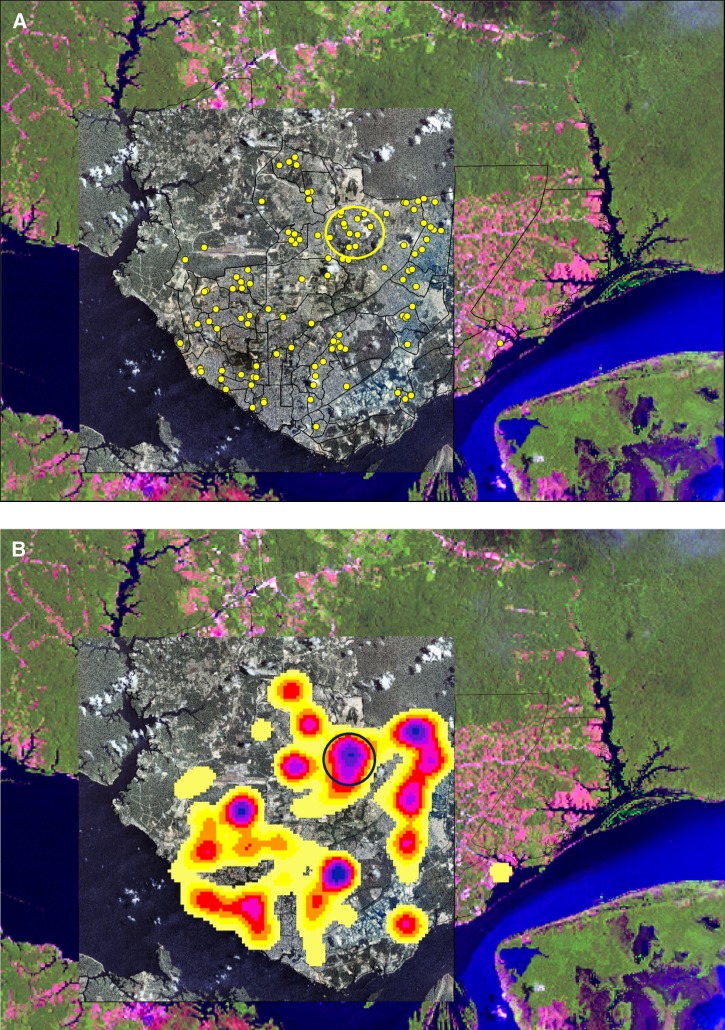
The spatial distribution of ATL within the city of Manaus was evaluated after acquisition of geographic coordinates of the living sites of the 120 urban cases enrolled at FMTAM. Positioning of the cases onto a geo-referenced photograph (Figure 3A ) revealed that ATL is distributed widely throughout several neighborhoods of Manaus (polygons outlined with black lines). Contrary to the notion that ATL is a rural disease, it was not confined to the outskirts adjacent to the Amazon forest.
Figure 3.
Distribution of American tegumentary leishmaniasis (ATL) cases within the city of Manaus. (A) Composite image showing the distribution of urban ATL cases diagnosed in the dermatology clinic of Tropical Medicine Foundation of the Amazonas State (FMTAM) between January 2008 and August 2010. Polygons outlined by black lines in the satellite photograph correspond to neighborhoods of Manaus. Green areas in color picture and dark gray areas in the black and white geo-referenced image correspond to vegetation. Red, light gray, and white areas correspond to populated districts. Yellow dots represent the homes of ATL patients. Yellow circle surrounds the major cluster of observed ATL cases, located in the Cidade Nova neighborhood. (B) Kernel analysis identifying clusters of cases represented by shades of yellow, red, and purple. Progression of shading from yellow to red to purple represents increasing density of clustered cases. Yellow circle surrounds the major cluster of ATL cases in the Cidade Nova neighborhood.
Kernel analysis identified several clusters of ATL cases, suggesting that certain areas of the city may expose the residents to a greater risk of disease acquisition than others (Figure 3B). Even neighborhoods of older settlement, which are closer to the Negro river and away from boundaries with the forest, displayed major aggregates of cases (Figure 3B).
Inspection of the major ATL clusters detected in Manaus (clusters with red and purple centers in Figure 3B) revealed that the majority of the patients' homes were located in close vicinity to forest patches occurring inside the city. For example, of the seven patients shown (yellow dots) in the representative photograph of the major ATL cluster identified (Figure 4 , encircled in Figure 3), five lived right next to forest patches and the other two lived only two blocks away from these areas. Reflecting this observation, 76% (N = 91) of all mapped patients lived within 500 m from forested areas, against only 24% (N = 29) living beyond 500 m of the closest forest.
Figure 4.
Distribution of seven representative cases found at the center of the major cluster of American tegumentary leishmaniasis (ATL) patients in Cidade Nova neighborhood within the yellow circle from Figure 3A. Green areas correspond to vegetation. Yellow dots represent the homes of ATL patients.
Discussion
Because of increasing urbanization, 70% of the residents of the Brazilian Amazon live within cities.16 This study is an investigation of the positioning of cutaneous leishmaniasis cases within Manaus, the largest settlement within the Amazon.
Data from prospectively enrolled cases and recorded databases of the Ministry of Health were analyzed. Patients with ATL were distributed widely throughout Manaus. Their homes were frequently located close to residual forest inside the city, and younger age groups were frequently affected. Altogether these findings suggest that either localized populations within the city have a higher risk of acquiring vector-borne diseases outside the borders of Manaus or there may be transmission of L. (V.) guyanensis occurring close to inhabitants' homes within the city of Manaus. To properly address these possibilities, careful case–control studies comparing affected individuals with non-affected individuals, and comparing the distribution of other diseases within the city of Manaus will be required.
Although reports on the sand fly fauna within Manaus are still scarce, a fairly recent study was performed in the community of São João, which is located in the outskirts of the city.17 The study reported that the local phlebotomine fly population is composed of almost 50 different species of sand flies. Fewer than 2% of the species could be found in peridomiciles, in contrast to 98.5% that could be found within the forested area. Of note, the predominant species detected, both within forested areas and peridomiciles, was Lutzomyia (Nyssomyia) umbratilis. This is the major vector transmitting L. (V.) guyanensis to human beings in the Amazon.18
We speculate that Lu. (N.) umbratilis is a component of the phlebotomine fly population within the forest preservation areas and parks distributed throughout Manaus, as well as of the peridomiciles and urbanized areas found near to these green reserves. Thus the local population could be exposed to this vector, and thus have the risk of acquiring L. (V.) guyanensis infection, particularly at dawn, night, and/or dusk because of the biting habits of this phlebotomine species.17
Ironically, an early report in 1989 raised the concern that there might be urbanization of leishmaniasis in (then) recent settlements built along the northern edge of Manaus. These neighborhoods housed the rapidly growing population of migrants, which were incoming to fulfill the developing industrial district of Manaus.11 That study described 1) the presence of Lu. (N.) umbratilis within inhabitants' domiciles and nearby primary forests, 2) that five percent of these sand flies were infected with L. (V.) guyanensis, and 3) that disease due to this Leishmania species occurred among residents of these neighborhoods. The authors further concluded on the possible existence of an intra-domiciliary component in the local transmission cycle of the parasite, given the detection of disease among young children.
To a large extent, exposure to Leishmania spp. among individuals younger than 20 years of age most likely occurs within or close to the home (i.e., peridomiciliary). Individuals in the age range of 21–40 years would be at greatest risk of occupational acquisition of the infection, for example, during farming or harvesting, since this is one of the most economically active age groups. In this study, there was no difference in the number of ATL cases between the 0–20 and 20–40 age groups. Furthermore, about half of the patients in the 0–20 age group enrolled at FMTAM were 15 years old or less. Although these findings are supportive of a local transmission cycle, they do not represent formal proof.
The use of historic and prospective data to correlate subject residence with disease acquisition site was certainly a limitation in this study. A more accurate approach would be to delineate the “personal activity space” of each enrolled subject, then perform the geographic analyses. The estimation of personal activity space is based on questionnaires administered to the study participants, asking for current and past place of residence, travel within and outside the city, work-related and other habitual activities, and the location of these activities. Acquisition and analysis of these data is a laborious task that is not routinely performed by the Ministry of Health. Questionnaires therefore must be designed and administered as part of a prospective study on a large sample of individuals to achieve power to detect case clustering, given the assortment of places each individual will list as possible Leishmania spp. exposure sites.
An extension of this research would include vector surveillance, both in and surrounding patients' homes and at nearby forested patches. Such work would use vector capture and identification of a large sample of collected insects, and specific molecular methods to assess sand fly infection rates with Leishmania spp. Such an approach could be designed as part of a prospective study, based on the findings reported herein.
This report shows the sustained presence of ATL in the largest human settlement within the Amazon rain forest. These findings describe the current distribution of this vector-borne disease in Brazil, in a region where human settlements encroach upon the Amazon forest; it raises questions that must be studied in future follow-up research. Such studies would address whether transmission of ATL occurs within the city of Manaus itself or, due to exposure of residents to parasite-infected sand flies outside the city, in the surrounding forest. It will be also important to identify other risk factors for ATL detection in Manaus.
Despite the above limitations, this report underscores the need for local public health authorities to design effective and/or reinforce measures for residents' protection against the sand fly vectors transmitting leishmaniasis in large urban centers, to control the spread of disease.
ACKNOWLEDGMENTS
We are deeply indebted to Lee W. Riley and Mary E. Wilson for careful revision of this article.
Disclaimer: This study was part of Ednelza Benício's master's degree dissertation at the Programa de Pós-Graduação em Medicina Tropical, Universidade Estadual do Amazonas/Fundação de Medicina Tropical Doutor Heitor Vieira Dourado.
Footnotes
Financial support: This work was funded by the Fundação de Amparo à Pesquisa do Estado do Amazonas–FAPEAM, Brazil and by the NIH grant P50AI030639. Albert Schriefer and Marcelo Távora Mira were recipients of research scholarships from FAPEAM. Ednelza Benício, Mayara Cordeiro, and Hannah Monteiro were recipients of PAIC scholarships from FAPEAM.
Authors' addresses: Ednelza Benício, Mayara Cordeiro, Hannah Monteiro, and Cintia Oliveira, Departamento de Ensino e Pesquisa, Fundação de Medicina Tropical do Amazonas, Amazonas, Brazil, E-mails: ednelza.benicio@hotmail.com, mayara.cord89@gmail.com, nanahhg@hotmail.com, and cmaraoliveira@hotmail.com. Marco Antônio Saboia Moura, Departamento de Tecnologia da Informação, Fundação de Medicina Tropical do Amazonas, Amazonas, Brazil, E-mail: marco@fmt.am.gov.br. Ellen Pricilla Nunes Gadelha, Anette Chrusciak-Talhari, and Sinésio Talhari, Gerência de Dermatologia, Fundação de Medicina Tropical do Amazonas, Amazonas, Brazil, E-mails: ellenpriscilla@ig.com.br, anette@dermatologiatalhari.com.br, and sinesio@dermatologiatalhari.com.br. Carolina Talhari, Diretoria de Ensino e Pesquisa, Fundação de Dermatologia Tropical e Venereologia Alfredo da Mata, Amazonas, Brazil, E-mail: carolinatalhari@gmail.com. Luiz Carlos de Lima Ferreira, Gerência de Patologia, Fundação de Medicina Tropical do Amazonas, Amazonas, Brazil, E-mail: ferreira@fmt.am.gov.br. Marcelo Távora Mira, PPGCS/CCBS, Pontificia Universidade Católica do Paraná, Paraná, Brazil, E-mail: m.mira@pucpr.br. Paulo Roberto Lima Machado and Albert Schriefer, Serviço de Imunologia, Hospital Universitário Professor Edgard Santos, Bahia, Brazil, E-mails: prlmachado@uol.com.br and aschriefer@globo.com.
References
- 1.Mathers CD, Ezzati M, Lopez AD. Measuring the burden of neglected tropical diseases: the global burden of disease framework. PLoS Negl Trop Dis. 2007;1:e114. doi: 10.1371/journal.pntd.0000114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reithinger R, Dujardin JC, Louzir H, Pirmez C, Alexander B, Brooker S. Cutaneous leishmaniasis. Lancet Infect Dis. 2007;7:581–596. doi: 10.1016/S1473-3099(07)70209-8. [DOI] [PubMed] [Google Scholar]
- 3.Hotez PJ, Bottazzi ME, Franco-Paredes C, Ault SK, Periago MR. The neglected tropical diseases of Latin America and the Caribbean: a review of disease burden and distribution and a roadmap for control and elimination. PLoS Negl Trop Dis. 2008;2:e300. doi: 10.1371/journal.pntd.0000300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brazil Ministry of Health Portal da Saúde. 2014. http://portalsaude.saude.gov.br/images/pdf/2014/setembro/09/LT-Casos.pdf Available at. Accessed July 1, 2015.
- 5.Harhay MO, Olliaro PL, Costa DL, Costa CH. Urban parasitology: visceral leishmaniasis in Brazil. Trends Parasitol. 2011;27:403–409. doi: 10.1016/j.pt.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 6.Albuquerque PL, Silva Junior GB, Freire CC, Oliveira SB, Almeida DM, Silva HF, Cavalcante Mdo S, Sousa Ade Q. Urbanization of visceral leishmaniasis (kala-azar) in Fortaleza, Ceara, Brazil. Rev Panam Salud Publica. 2009;26:330–333. doi: 10.1590/s1020-49892009001000007. [DOI] [PubMed] [Google Scholar]
- 7.Silva ES, Gontijo CM, Pacheco RS, Fiuza VO, Brazil RP. Visceral leishmaniasis in the metropolitan region of Belo Horizonte, State of Minas Gerais, Brazil. Mem Inst Oswaldo Cruz. 2001;96:285–291. doi: 10.1590/s0074-02762001000300002. [DOI] [PubMed] [Google Scholar]
- 8.Jeronimo SM, Duggal P, Braz RF, Cheng C, Monteiro GR, Nascimento ET, Martins DR, Karplus TM, Ximenes MF, Oliveira CC, Pinheiro VG, Pereira W, Peralta JM, Sousa J, Medeiros IM, Pearsoni RD, Burns TL, Pugh EW, Wilson ME. An emerging peri-urban pattern of infection with Leishmania chagasi, the protozoan causing visceral leishmaniasis in northeast Brazil. Scand J Infect Dis. 2004;36:443–449. doi: 10.1080/00365540410020451. [DOI] [PubMed] [Google Scholar]
- 9.Penna G, Pinto LF, Soranz D, Glatt R. High incidence of diseases endemic to the Amazon region of Brazil, 2001–2006. Emerg Infect Dis. 2009;15:626–632. doi: 10.3201/eid1504.081329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guerra JA, Ribeiro JA, Coelho LI, Barbosa MG, Paes MG. Epidemiology of tegumentary leishmaniasis in Sao Joao, Manaus, Amazonas, Brazil [in Portuguese] Cad Saude Publica. 2006;22:2319–2327. doi: 10.1590/s0102-311x2006001100006. [DOI] [PubMed] [Google Scholar]
- 11.Barrett TV, Senra MS. Leishmaniasis in Manaus, Brazil. Parasitol Today. 1989;5:255–257. doi: 10.1016/0169-4758(89)90258-5. [DOI] [PubMed] [Google Scholar]
- 12.Brazil Ministry of Health DATASUS. 2011. http://www.datasus.gov.br Available at. Accessed July 1, 2015.
- 13.Garcia L, Kindt A, Bermudez H, Llanos-Cuentas A, De Doncker S, Arevalo J, Wilber Quispe Tintaya K, Dujardin JC. Culture-independent species typing of neotropical Leishmania for clinical validation of a PCR-based assay targeting heat shock protein 70 genes. J Clin Microbiol. 2004;42:2294–2297. doi: 10.1128/JCM.42.5.2294-2297.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Montalvo AM, Fraga J, Monzote L, Montano I, De Doncker S, Dujardin JC, Van der Auwera G. Heat-shock protein 70 PCR-RFLP: a universal simple tool for Leishmania species discrimination in the New and Old World. Parasitology. 2010;137:1159–1168. doi: 10.1017/S0031182010000089. [DOI] [PubMed] [Google Scholar]
- 15.Brazil Ministry of Health SINAN. 2011. http://dtr2004.saude.gov.br/sinanweb/ Available at. Accessed July 1, 2015.
- 16.SUDAM Amazônia Legal Demografia. 2014. http://www.sudam.gov.br/amazonia-legal/demografia Available at. Accessed July 1, 2015.
- 17.Barbosa MGV, Fé NF, Marcião AHR, Silva APT, Monteiro WM, Guerra JAO. Fauna de flebotomíneos (Diptera: Psychodidae) em um foco de leishmaniose tegumentar americana na área periurbana de Manaus, Estado do Amazonas. Rev Soc Bras Med Trop. 2008;41:485–491. doi: 10.1590/s0037-86822008000500010. [DOI] [PubMed] [Google Scholar]
- 18.Lainson R, Shaw JJ, Silveira FT, de Souza AA, Braga RR, Ishikawa EA. The dermal leishmaniases of Brazil, with special reference to the eco-epidemiology of the disease in Amazonia. Mem Inst Oswaldo Cruz. 1994;89:435–443. doi: 10.1590/s0074-02761994000300027. [DOI] [PubMed] [Google Scholar]