Abstract
Background
In 2010, the reported overall HIV prevalence in Liangshan China (1.14%) was 19.7 times of the overall estimated prevalence in China (0.058%), and injection drug use contributed to 60.0% of overall HIV infections in Xichang, the Capital city of Liangshan. With one national methadone clinic and three outpatient service sites, and three NEP sites, the HIV prevalence among people who inject drugs (PWID) in Xichang was estimated as 18.0 %(2.8 times of national HIV prevalence among PWID) in 2012.
Methods
Face-to-face questionnaire interviews were used in a cross-sectional study to assess experience, attitudes, possibility and acceptability of implementing 8 pharmacy-delivered services among PWID (n=403). The concordance of attitudes, possibility and acceptability between PWID and pharmacy staff (n=50) was examined.
Results
Rather than medical facility (23.1%), and NEP (8.9%), pharmacies were the main source of syringes for PWID in the last 12 months (82.1%), PWID (63.5%) reported syringes could be bought in single piece and at the price of $0.16 USD (59.3%). In the last 30 days, only 1 PWID brought used syringes back to a pharmacy. Pharmacy staff’s attitudes were generally negative but nearly neutral (average score −0.18), discrimination/business concerns against pharmacy-delivered services existed, and 4 of 5 compared attitude questions between PWID and pharmacy staff were statistically different (P<0.01). 5 of 8 pharmacy-delivered services were available for PWID at low level (≤ 16.9%). Pharmacy staff’s supportive perception for pharmacy-delivered services focused on pharmacies’ initiate roles targeting on general population more than on PWID.PWID were more supportive and optimistic than pharmacy staff toward potential usage of pharmacy-delivered services (p<0.05).
Conclusion
Pharmacy-delivered services for PWID in Xichang were partly in reality, and could be feasible. It is urgently needed to address the legal requirements and remuneration for pharmacies. Pharmacy staff should receive additional training on services related knowledge and skills, cultural sensitivity toward PWID. Successful pharmacy-delivered services would benefit from identifying mutual interest and benefit between pharmacies and PWID.
Keywords: PWID, Pharmacies, China, Services, HIV, Yi ethnic group
Graphical Abstract
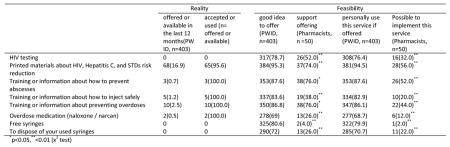
Reality and Feasibility of potential pharmacy-Delivered Services (No. (%))
INTRODUCTION
The first reported acquired immune deficiency syndrome (AIDS) in China was a dying tourist in 1985(Settle E. 2003). In 1989, the first indigenous cases in China were reported as first national large human immunodeficiency virus (HIV) outbreak among 146 infected heroin users in Yunnan province(Ma Y, Li ZZ, &Zhang KX,1990). People who inject drugs (PWID) had accounted for 44.2% of the total reported HIV/AIDS Between 1985 and 2005, and 34.1% in 2006. Since 2007, sexual transmission has overtaken injection drug use and became the first route of HIV infection. In 2011, the estimated number of HIV infections in China was about 780,000 and 154,000 had AIDS, with an estimated 46.5% infected through heterosexual transmission, 28.4% through injection drug use . The overall prevalence (0.058%) remains low, but pockets of high prevalence among specific subpopulations exist (China MOH, UNAIDS,& WHO, 2011).
Systematic review showed that in 2005, mid-estimates of HIV prevalence among PWID in China were 12.0 %( Mathers et al., 2008). With an estimated national prevalence of PWID as 0.19% in 2012(UNODC, 2014), China accounts for approximately 20.2% of the global numbers of PWID (UNODC, 2014; China National bureau of statistics, 2013). Sichuan province in China ranked 5 in the number of PWID (China MOH, UNAIDS, &WHO, 2011); most are from Liangshan Yi Autonomous Prefecture (Liangshan). Adjacent to Yunnan province, Liangshan has been part of the major drug trafficking routes in China for more than 100 years and heroin use had been socially acceptable among Yi ethnic group. With a total population of 4.9 million (6.1% of the total population in Sichuan), among whom 50.0% were Yi ethnic group, 3.5% were other ethnic groups(Liangshan Bureau of Statistics, 2012 ), HIV incidence in Liangshan increased dramatically, accounting for 81.5% of the total HIV/AIDS cases in the past 5 years(Dai et al.,2012 ). In 2010, the reported overall HIV prevalence in Liangshan was 1.14%, 19.7 times of the national estimated prevalence, and as the first transmission route, PWID accounted for 48.6% of the cases. According to Asian Epidemic Model (AEM), PWID accounted for 52.3% of the HIV infection in Liangshan in 2013, and 39.1% by 2020(Liu et al., 2013).
To cut the HIV transmission among PWID through syringes sharing, methadone maintenance treatment (MMT) has been also scaled up in China (Mathers et al, 2010; China MOH, 2012; Zhou et al., 2014). By the end of 2011, there established 738 methadone clinics in 623 counties (districts) within 28 provinces/autonomous regions/municipalities in China providing MMT for a cumulative more than 344,000 PWID(China MOH, 2012), 13.3% of the total PWID. Providing sterile syringes to PWID is cost effective for HIV prevention (Holtgrave et al., 1998). Over 900 needle exchange program (NEP) sites in China have been established delivering more than 12 million clean needle and syringes annually (China MOH, 2012). Due to country-wide responses (Ruan et al., 2007; Mathers et al, 2010; China MOH, 2012; Ruan et al., 2013), the overall levels (per IDU per year) of syringes distribution in China were greater than the global average and of the US and Russia(Mathers et al, 2010) . With the expanded harm reduction programs HIV, prevalence among PWID in China fell from 9.3% in 2009 to 6.4% in 2011(China MOH, 2012), but high risk behaviors such sharing syringes and other equipment still exist in Liangshan(Ruan et al., 2007; Zhang et al, 2010; Ruan et al., 2013). HIV prevalence among PWID from 11 national methadone clinics in Liangshan between March 2004 and December 2012 was 25.4 %( Zhou et al., 2014).
Perceived discrimination (Wilson et al., 2014), internalized stigma (Rivera et al., 2014), lack of stigma management strategies (Mateu-Gelabert et al.,2014) by PWID may reduce uptake of services from formal health services, such as NEP use(Lang et.al, 2013; Rivera et al., 2014; Hammett, 2014). Pharmacies are considered as supplementary organization sources of obtaining sterile syringes (Busza et al., 2013). In the world, community pharmacies have been involved in providing services to PWID for many years (Glanz, Byrne, & Jackson, 1989; Sheridan et al, 1997; Myers et al., 1998; Matheson et al., 1999; Coffin et al., 2000; Koester et al.,2002; Fuller et al.,2004;Cooper et al., 2007; Mackridge&Scott., 2009; Rudolph et al.,2010; Torre, Lucas&Barros, 2010; Janulis, 2011; Zaller et al, 2012; Crawford et al, 2013; Busza et al., 2013; Pollini et al., 2014; Rose et al., 2014). Pharmacies are seen as not only feasible in nonprescription syringes sales(NPSS) to PWID, but also as public health venues to provide HIV-testing and vaccination, educational material, coupon syringe program. Moreover pharmacies have the potential to provide methadone, and Naloxone for overdose prevention, safer injection and overdose prevention training programs, and containers to dispose syringes, on-site disposal, clinical testing for hepatitis and pregnancy, directly observed therapy and so on.
In the early year of community pharmacy-delivered services, the coverage of a sharps box for used equipment was low (Glanz, Byrne, & Jackson, 1989; Coffin et al., 2000). Supporting attitude among pharmacists were less than half. Pharmacists who provided services to PWID held more positive attitudes than who did not provide. Pharmacists were more supportive than pharmacy staff (Sheridan et al, 1997; Myers et al., 1998; Matheson et al., 1999; Coffin et al., 2000). Pharmacists’ most comfortable services were counselling, advices and literature, and environmental and technological interventions, and they gave least support toward providing services as part of program and legalization of drugs or methadone prescription. They worried about staff safety (Myers et al., 1998). Some pharmacists who did not provided services suspected that pharmacy-delivered services would increase the percentage of injection drug use. Lack of sufficient training for how to provide services to PWID was common. In addition, concerns about the financial impact on business were also barriers against effective services for PWID (Sheridan et al, 1997; Koester et al.,2002; Fuller et al.,2004;Janulis, 2011; Zaller et al, 2012;Busza et al., 2013; Pollini et al., 2014). With time, pharmacies have been involved in providing clean syringes as well as opiod substitution. Pharmacist’s attitudes have been generally positive. Lack of time and training, insufficient remuneration are common barriers against pharmacy-delivered-services, as well as fear of attracting unruly clients and inadequate communication with health providers (Watson & Hughes, 2012).
As services receivers, PWID have reported problems (such as declined, or asked for picture identification and/or prescription) in obtaining syringes from a pharmacy even when legally available (Koester et al.,2002; Fuller et al.,2004;Janulis, 2011; Zaller et al, 2012;Busza et al., 2013; Pollini et al., 2014).Pharmacists sold nonprescription syringes less frequently than they claimed( Zaller et al, 2012). PWID considered syringes access and disposal, clinical testing, vaccinations, and methadone provision as priorities. For PWID, pharmacists’ and pharmacy staff attitudes were a major barrier to comfort with pharmacy-delivered services (Lutnick, Case&Kral, 2012). Hostile service environments increased the odds of improper syringe disposal (Quinn et al., 2014).
In Guangxi Province, China, besides direct distribution, vouchers redeemable for new syringes, ampoules of sterile water for injection, and condoms in pharmacies have been used as alternative provision of sterile syringes for PWIDI (Hammett et al., 2006). In Yunnan and Beijing, pharmacies have been perceived as health care facilities, especially for STI/HIV treatment (Wong et al., 2006; Zhao et al., 2008). A survey among 324 PWID from addiction treatment centers in Yunnan showed that their major resource of syringes were pharmacies and clinics (SHA et al., 2008). Between 2008 and 2011, NEP among 19 counties in Yunnan had implemented at pharmacies as well as at NSP center, clinics, and from peer educators (Xue, LIU &Sun, 2013)
NPSS to PWID in Liangshan were not reported in previous literatures, there were no study to show the willingness of pharmacy staff to expanding their roles in providing services to PWID besides syringes sales. It was not clear to what extent PWID would like to utilize potential pharmacy-delivered services. Pharmacy staff were the direct providers for pharmacies-delivered services; hence, their attitudes are likely to have a major impact on the successful provision of services. As receivers of services, if PWID were reluctant to utilize pharmacies-delivered services, these services could not likely to be successful. In the current study, we were interested in examining whether pharmacies-delivered services for PWID would be acceptable and feasible in Liangshan, and what trainings and interventions were needed to facilitate these services. The specific aim of this paper was to examine both PWID and pharmacy staff attitudes and experience in harm reduction services and the concordance between PWID as receivers and pharmacists as providers.
Methods
Study site
Xichang, with a population of more than 600,000(Ruan et al., 2013), is the Capital city of Liangshan. The estimated number of PWID in Xichang was 2250, and drug use contributed to 60% of HIV infections (Hammett et al., 2014). The HIV prevalence among PWID in Xichang was 11.3 %(Ruan et al., 2004) in 2002, 17.8% in 2004(Yin et al., 2007), and 18.0% in 2012(Hammett et al., 2014). There was one national methadone clinic, three MMT outpatient service sites, and three NEP sites in Xichang. In 2012, there were more than 400 pharmacies in Xichang.
Study procedure and PWID recruitment
This study was a cross-sectional study, and the protocols were approved both by institutional review board (IRB)s from Johns Hopkins Bloomberg School of Public Health (JHSPH) and from the West China School of Public Health (WCSPH). After initial piloting, the surveys were face-to-face structure interviews. Only the one eligible to inclusion criteria were recruited. The protocol and questionnaires were written in English and the questionnaires were translated into Chinese and reviewed by the US and Chinese study team. Investigators from WCSPH and governmental staff from Xichang Skin Disease and Prevention Center (XSDPC), which is in the charge of HIV/AIDS prevention and control in Xichang, were trained as interviewers and face-to-face collected the data. From April to May, 2012, staff from XSDPC recruited eligible participants in Xichang City through purposive and snowball sampling. The study inclusion criteria for PWID were: 1) 18 years of age or over and 2) had injected drugs within the past 30 days. Most (>80.0%) PWID in China are registered (National Narcotics Control Commission, 2013). In order to approach PWID easily, in the beginning, according to their working experiences, staff from XSDPC selected Xichang methadone clinic and Xichang addiction treatment center to recruit eligible PWID as purposive sampling. After completing their interviews, PWID were encouraged to inform other PWID to take part in the study as snowball sampling. Finally, 403 PWID were recruited from addiction treatment center (66.7 %,), methadone clinic (15.6 %), communities (7.4%), MMT outpatient service sites (6.7%), and rehabilitation center (3.5%). Before completing a face-to-face structure interview, eligible participants completed an informed consent form and 50 yuan (~USD 8) compensation was paid for their participation. Condoms and safe injection supplies were also provided to PWID along with appropriate referrals. The survey for the PWID included demographic characteristics, experiences of syringe services in pharmacies, attitudes toward pharmacy-delivered services, and supporting perception and potential usage toward the 8 pharmacy-delivered services. The syringes getting experiences were recalled in the past 30 days, and pharmacy experiences were recalled in the past 12 months. The answers categories for attitudes were ‘strongly agree’, ‘agree’, ‘don’t know’, ‘disagree’, and ‘strongly disagree’. 2 questions were asked toward each pharmacy-delivered service: 1) Do you think it would be a good idea to offer [this] in pharmacies? 2) Would you personally use this service if offered? The answers were three categories: ‘no’, yes,’ ‘don’t know’.
Pharmacy participants and instruments
In China, there are three types of pharmacies: a chain pharmacy, an independent pharmacy, and a government run pharmacy. All pharmacies are directly supervised by local the food and drug administration (FDA). Single-use syringes are considered as medical devices. Pharmacies that sell syringes are required to obtain “Medical Devices Operation Enterprises permit” which is ensured by provincial bureau of FDA and supervised by Prefecture FDA for NPSS (China FDA, 2004–2014). This study was designed as baseline survey for future pharmacy-delivered services trials, to find out potential capability and level of interest among pharmacies which currently provided NPSS. Therefore, only pharmacies both with “medical devices Operation Enterprises permit” and where pharmacy policy permit syringes sales to PWID were approached. The surveys were highly accepted. Before the formal survey, according to their work experiences, staff from XSDPC approached pharmacies, and asked managers or senior staff whether their pharmacy policies permit NPSS to PWID or not. If yes, the study was explained to pharmacy managers or senior staff, and they were invited to ask for one eligible staff(including them) from each pharmacy to take part in the study later on, the criteria were: a) 18 years or older; 2) working at a pharmacy for at least one year; 3) current working in the pharmacy. Therefore in the formal survey, all the approached pharmacies took part in the study. In total, fifty pharmacies were recruited: 86.0% were chain pharmacies, 12.0% as independent pharmacy, and 2.0% government–run pharmacy. Finally, there were 92.0% pharmacy staff and 8.0% licensed pharmacists were recruited. The 50 pharmacies represented about 12% of all pharmacies in Xichang. Due to small proportion of pharmacists, in this article, we called all the participants pharmacy staff. The surveys were face-to-face structure interviews, and included their pharmacy work experiences and perceptions of illegal drug activity and other crime in the neighborhood of the pharmacies. Attitudes toward pharmacy-delivered services were assessed with 9 questions, such as ‘pharmacy staff and pharmacists care about the health of customers who inject illicit drugs’. The answers categories were ‘strongly agree’,’ agree ‘,’not applicable ‘,’disagree’, and ‘strongly disagree’(valued as 2, 1, 0, −1, −2) and reverse coded for negative questions (such as ‘PWID are a disruption in this pharmacy’). Sum of the scores for each question was the total attitude score, and the range was −18 to 18. A sum greater than zero was considered a positive attitude, less than zero negative, and zero as neutral. There were 8 potential pharmacy-delivered services, and 2 questions were asked toward each service: 1) would you support offering ……? 2) Would it be possible to implement this service in this pharmacy? The answers were three categories: ‘no’, ‘yes,’ ‘maybe’.
Statistics
SPSS 22.0 (IBM, USA) was used for descriptive statics. In order to examine differences between pharmacy staff and PWID in terms of the attitude, supporting ideas, potential usage / provision of pharmacy-delivered service, nonparametric cross-tabulation (χ2 and Fisher’s exact test) were used. The group comparison was run by Stata 13.0(StataCorp LP, USA).
Results
The characteristics of participants are shown in table1.
Table 1.
Characteristics of Participants Enrolled in the Study (n, (%))
| pharmacy staff(n=50)
|
PWID(n=403)
|
||
|---|---|---|---|
| Licensed pharmacist(s) employed in the pharmacy | Male Sex | 353(87.6) | |
| 1 | 42(84.0) | Employed | 234(58.1) |
| 2 | 7(14.0) | Ethnic group | |
| 3 | 1(2.0) | Han | 213(52.9) |
| Managed the pharmacy | 9(18.0) | Yi | 180(44.7) |
| Worked in the sample pharmacy(years) | others | 10(2.5) | |
| <1 | 16(32.0) | Currently enrolled in any kinds of school, college, a vocational or training program | 3(0.7) |
| =1 | 13(26.0) | Stable housing | 367(91.1) |
| >1 | 20(40.0) | Martial statues | |
| Involved with setting practice policies at the pharmacy | 28(56.0) | Single | 116(28.8) |
| On a scale of illegal drug activity (from 1 = no activity to 6 = very high activity) | Married | 187(46.4) | |
| 1 | 17(34.0) | Divorced | 86(21.3) |
| 2 | 7(14.0) | Separated | 6(1.5) |
| 3 | 8(16.0) | widowed | 7(1.7) |
| 4 | 3(6.0) | Others | 1(0.2) |
| 5 | 1(2.0) | Live | |
| 6 | 2(4.0) | Alone | 87(21.6) |
| Don’t know the situation | 12(24.0) | With parents | 173(42.9) |
| On a scale of crime (robbery, car theft, etc…) activity in the neighborhood (from 1 = no activity to 6 = very high activity) | With sex partners | 117(29) | |
| 1 | 18(36.0) | Others | 25(6.2) |
| 2 | 12(24.0) | Having a cell phone were age, median(range), y living in Xichang, median(range), y | 336(83.4) |
| 3 | 9(18.0) | 35(17–55) | |
| 4 | 5(10.0) | 28(1–51) | |
| 5 | 3(6.0) | Education, median(range), y | 8(0–16) |
| 6 | 2(4.0) | income in last month, median(range), Chinese Yuan | 2000(0–30000) |
| Don’t know the situation | 1(2.0) | ||
In the last 30 days, the major self-reported sources of obtaining syringes for PWID were from pharmacy (81.1%), medical facility (23.1%), someone else who obtained them from pharmacy (11.9%), and NEP (8.9%). 49.1% of PWID reported used a syringe for only one time, and the median times for a single syringe among all PWID were 2(1–50). There were 2.7% PWID reported ‘always’, 19.4% ‘at least once’, and 77.9% ‘never’ using a syringe that they knew someone had used before them. The respective percentages of ‘always,’ ‘at least once’ and ‘never’ passing their syringe to somebody else to use after they had used it were 3.5%, 25.3%, and 71.2 %( p<0.01). It is interesting to note that PWID reported giving more used syringes out than they received.
Pharmacy-delivered Services
In the last 12 months, 82.1% PWID reported having purchased a syringe in a pharmacy. Most (63.5%) PWID reported that the minimum number of syringes that they could buy in a pharmacy in Xichang was 1 during the past 12 months. The mostly common (59.3%) price for the minimum number was 1 Chinese Yuan (~$0.16); 65.2% PWID preferred to buy syringes at a pharmacy where they buy OTC or prescription drugs; 43.8% chose pharmacies in the same neighborhood/region where they live. When buying syringes in pharmacies, 18.6% PWID reported that some of their requests were declined, and 12.2% were treated poorly at the pharmacy.
Among the 8 identified services in the pharmacies, printed materials about HIV, Hepatitis C, and STIs risk reduction, was offered by 16.9%, but other 4 provided services were offered less than 3% in the last 12 months. As long as the services were offered, the percentages of acceptance were high. HIV testing, free syringes and used syringes disposal was not offered in pharmacies (table 2).
Table 2.
current pharmacy-Delivered Services in the last 12 months (PWID, n=403, No. (%))
| Offered/available | accepted or used (n=offered or available) | |
|---|---|---|
| Printed materials about HIV, Hepatitis C, and STIs risk reduction | 68(16.9) | 65(95.6) |
| Training or information about preventing overdoses | 10(2.5) | 10(100.0) |
| Training or information about how to inject safely | 5(1.2) | 5(100.0) |
| Training or information about how to prevent abscesses | 3(0.7) | 3(100.0) |
| Overdose medication (naloxone / narcan) | 2(0.5) | 2(100.0) |
| HIV testing | 0 | 0 |
| Free syringes | 0 | 0 |
| To dispose of your used syringes | 0 | 0 |
In the last 30 days, 74.7% of PWID reported throwing used syringes away, 24.3% left syringes where they shot up, and 17.9% buried or burned syringes. Only 1 PWID brought used syringes to a pharmacy.
Attitudes towards services from pharmacies
Of the 50 pharmacy staff, 64% and 4.0% agreed and strongly agreed that their views on these issues were the same as other pharmacy staff in city. In general, pharmacy staff’s attitudes were more inconsistent than PWID, pharmacy staff gave the answer of ‘no applicable/don’t know’ toward many questions, especially the questions about ‘PWID make other customers in the pharmacy uncomfortable’ with 32% reporting …’ Overall, pharmacy staff held positive attitude only toward 3 of 8 questions. The average attitude score for pharmacy staff was −0.18(range: −7 to 5).
Among the 5 comparison questions, there were 4 statistically significant differences between PWID and pharmacy staff (P<0.01, table3). 65.3% PWID agreed the statement that pharmacy staff should sell sterile syringes to PWID, on the contrary, only 6% pharmacy staff agreed that PWID should always be allowed to buy syringes in this pharmacy. Most (84%) pharmacy staff agreed with the statement that pharmacy staff and pharmacy staff care about the health of PWID; however only 40.7% PWID agreed that pharmacy staff and pharmacy staff care about their health and wellbeing.
Table 3.
attitude toward services in pharmacies (No. (%))
| PWID(N=403)
|
Pharmacy staff(n=50)
|
|||||||
|---|---|---|---|---|---|---|---|---|
| item | agree(incl uding strongly agree) |
disagree(i ncluding strongly disagree) |
missing data | item | agree(incl uding strongly agree) |
disagree(i ncluding strongly disagree) |
not applicabl e/don’t know |
χ2 |
| Pharmacists should sell sterile syringes to PWID | 263(65.3) | 132(32.8) | 8(2.0) | PWID should always be allowed to buy syringes in this pharmacy | 3(6.0) | 47(94.0) | 0(0.0) | 69.8**, α |
| Pharmacists and pharmacists care about my health and well being | 164(40.7) | 229(56.8) | 10(2.5) | Pharmacists and pharmacists care about the health of PWID | 42(84.0) | 6(12.0) | 2(4.0) | 34.0** |
| It bothers me if people know why I’m buying syringes at the pharmacy. | 369(91.6) | 29(7.2) | 5(1.2) | Customers purchasing syringes would feel uncomfortable if we were to give them HIV related information | 25(50.0) | 12(24.0) | 13(26.0) | 91.3** |
| It’s generally hard for me to go to the pharmacy during the hours they are open | 258(64) | 140(34.7) | 5(1.2) | I usually have the time to provide information or resources to customers who purchase syringes in this pharmacy & | 11(22.0) | 28(56.0) | 11(22.0) | 56.9** |
| It wouldn’t matter to me if people saw me walk into a pharmacy | 204(50.6) | 195(48.4) | 4(1.0) | Customers who inject illicit drugs are a disruption in this pharmacy & | 28(56.0) | 20(40.0) | 2(4.0) | 4.6 |
| Police will take notice if I go to a pharmacy to buy syringes | 325(80.6) | 72(17.9) | 6(1.5) | It is the role of pharmacists or pharmacists to provide customers with HIV prevention services | 44(88.0) | 4(8.0) | 2(4.0) | - |
| I know which pharmacies to go to for syringes | 308(76.4) | 87(21.6) | 8(2.0) | Pharmacists are an important point of contact for health care information for PWID | 27(54.0) | 15(30.0) | 8(16.0) | - |
| I feel comfortable trying to buy a syringe at any pharmacy | 177(43.9) | 222(55.1) | 4(1.0) | PWID make other customers in the pharmacy uncomfortable | 27(54.0) | 7(14.0) | 16(32.0) | - |
| Pharmacies are sometimes too far for me to get to easily. | 264(65.5) | 136(33.7) | 3(0.7) | My views on these issues are the same as other pharmacists in <city> | 34(68.0) | 6(12.0) | 10(20.0) | - |
Notes: - means not compared, &: in the comparison, ‘agree (including strongly agree)’ attitude among PWID were compared with ‘disagree (including strongly disagree)’ among pharmacy staff.
:fisher exact test,
<0.01
Feasibility for Pharmacy-Delivered Services
For every potential pharmacy-delivered service, PWID were more likely to endorse providing the services as compare to the pharmacy staff. The most extreme example was that 80.6% PWID thought it is good idea to offer free syringes at pharmacies, but only 4% of pharmacy staff agreed. In general, pharmacy staff was less supportive in offering services directly related with inject drug use (such as proving free syringes and disposing of used syringes). When comparing the feasibility for implementing new services, PWID were more favorable than pharmacy staff. The most extreme example was that 79.9% PWID said that they would personally use free syringe if offered, but only 1 of 50 pharmacy staff thought it is possible to implement the provision of free syringes (table 4).
Table 4.
Feasibility of potential pharmacy-Delivered Services (No. (%))
| good idea to offer (PWID,n=403) | support offering (Pharmacy staff, n =50) | personally use this service if offered (PWID,n=403) | Possible to implement this service (Pharmacy staff, n=50) | |
|---|---|---|---|---|
| HIV testing | 317(78.7) | 26(52.0)** | 308(76.4) | 16(32.0)** |
| Printed materials about HIV, Hepatitis C, and STDs risk reduction | 384(95.3) | 37(74.0)** | 381(94.5) | 28(56.0)** |
| Training or information about how to prevent abscesses | 353(87.6) | 38(76.0)* | 353(87.6) | 26(52.0)** |
| Training or information about how to inject safely | 337(83.6) | 19(38.0)** | 334(82.9) | 10(20.0)** |
| Training or information about preventing overdoses | 350(86.8) | 38(76.0)* | 347(86.1) | 22(44.0)** |
| Overdose medication (naloxone / narcan) | 278(69) | 13(26.0)** | 277(68.7) | 6(12.0)** |
| Free syringes | 325(80.6) | 2(4.0)** | 322(79.9) | 1(2.0)** |
| To dispose of used syringes | 290(72) | 13(26.0)** | 285(70.7) | 11(22.0)** |
p<0.05,
<0.01 (χ2 test)
Discussion
This study showed that pharmacies were the main source of syringes for PWID with some reports of harassment and unfair treatment from pharmacy staff. PWID disposed their used syringes mainly by throwing them away. There were 5 of 8 pharmacy-delivered services available for PWID at low level (<20%). Pharmacy staff’s attitudes toward pharmacy-delivered services for PWID were generally negative but nearly neutral. PWID were more optimistic than pharmacy staff toward potential usage of pharmacy-delivered services.
NPSS are legally available at qualified pharmacies, and carrying a syringe for individuals is legal. PWID reported syringes could be bought in single piece and with low price from pharmacies. Nearly half of the PWID reported used a syringe for only one time. ‘At least once’ syringes sharing were lower than previously reported (Zhang et al., 2010), and the prevalence of ‘always’ sharing syringes were < 4%. Though free syringes from pharmacies were not offered, yet pharmacies were the main source (>80%) of buying syringes for PWID. We found that 3 of 8 pharmacy-delivered services were unavailable for PWID. HIV testing in China are legally restricted within medical institutes which exclude pharmacies (China State Council, 1994&2006), and HIV test kits are not approved by China FDA yet. When ‘giving out’ syringes from pharmacies became easy, ‘receiving’ used syringes back need more attention under the background of highly improper syringes disposal (74.7% throwing used syringes away) to reduce harm. According to ‘Management Regulation of the People’s Republic of China on Medical waste’ (China State Council, 2003), only in rural areas, single used syringes could be sterilized-destroyed-burned or buried. In urban areas, single used syringes should be first collected and then transported to the local medical waste disposition centers within 2 days after use. Medical institutions are supervised by bureaus of health for medical waste disposal, but pharmacies are not categorized as ‘medical institutions ’. Therefore syringes disposal in pharmacies may have potential problems as there was little support from pharmacy staff for disposal at pharmacies. Remuneration is important for successful pharmacy-delivered-services (Watson & Hughes, 2012). At the time of investigation, there were no programs in Xichang to support ‘free syringes’ and related services from pharmacies, ‘free syringes’ were unavailable from pharmacies, and other harm reduction services were available at low level.
As the direct providers, pharmacy staff’s attitudes toward pharmacy-delivered services for PWID were generally negative but nearly neutral. On one hand, they viewed their role more than just providing OTC or prescription drugs, which could be evidenced by the 88% supporting for the statement that ‘It is the role of pharmacists or pharmacy staff to provide customers with HIV prevention services’. On other hand, 54.0% considered themselves as an important point of contact for health care information for PWID. ‘Lack of time’ was their explanation for not providing more services to PWID. In this study, though all the pharmacies had a policy for selling syringes to PWID, only 6% pharmacy staff agreed that PWID should ‘always’ be allowed to buy syringes in this pharmacy. Pharmacy staff may have their own prejudices towards NPSS regardless of pharmacy policy. Pharmacy staff have been found to be less supportive than pharmacists (Sheridan et al, 1997; Myers et al., 1998; Matheson et al., 1999; Coffin et al., 2000). Pharmacy staff had their own judgments toward NPSS and other services. Pharmacy staff’s supportive perception for pharmacy-delivered services focused on pharmacies’ initiate roles as health facilities providing services targeted on general population (HIV testing; Printed materials about HIV, Hepatitis C, and STIs risk reduction; training or information about how to prevent abscesses) more than on PWID, especially the ideas of ‘free syringes’, ‘disposal of used syringes’, and ‘training or information about how to inject safely’ which are directly related with the harm reduction goal of reducing syringes sharing.
PWID endorsed the perception and potential usage of different kinds of ‘training or information’ similarly, but pharmacy staff’s endorsement showed more ambivalence. For example, pharmacy staff gave less support for ‘training or information about how to inject safely’ than for abscesses prevention and overdose ‘trainings or information’. In addition, pharmacy staff were more pessimistic in possibility for implementation toward these services than PWID in their potential use.
Though harassment and badly treatment from pharmacy staff was infrequent, discrimination towards PWID did exist in part to pharmacy staff viewing PWID as a disruption(56.0%) and claiming that ‘PWID make other customers uncomfortable in the pharmacy’ (54.0%). These claims could also be concerns about the financial impact on business (Sheridan et al, 1997; Koester et al., 2002; Fuller et al., 2004; Janulis, 2011; Watson & Hughes, 2012; Zaller et al, 2012; Busza et al., 2013; Pollini et al., 2014). As services receivers, many PWID perceived discrimination, and felt uncomfortable when trying to buy a syringe at any pharmacy (55.1%), and worried about people knowing the reasons for their syringe buying (91.6%). Although most (84%) pharmacy staff reported that they cared about the health of PWID, less than half (40.7%) PWID agreed that pharmacy staff cared about their health. Perceived discrimination could held PWID back from purchasing syringes from pharmacies (Fuller et al., 2004). Most PWID (65.2%) would like to buy syringes from well-known pharmacies where they buy OTC or prescription drugs without disclosing their PWID identities(less than half (43.8%) PWID chose pharmacies at the same neighborhood/region where they live).
At the time of investigation, pharmacies spontaneously provided NPSS and 5 of 8 harm reduction services. Most PWID supported and would like to use these services. In another word, the ‘markets’ existed, and ‘clients’-PWID as receivers was ready. Though their attitude were generally negative but neutral, most pharmacy staff views them as an important point of contact for health care information for PWID, and supported half of the potential services. Pharmacy staff as providers were at the point to be pulled into being involved in harm reduction services. Experiences in Yunnan showed though facing challenges, pharmacy-delivered services had their own advantages as 1) Pharmacies could integrate pharmacy-delivered services with other business. 2) Pretending buying OCT drugs, PWID could avoid disclosing their identities in pharmacies so as to avoid discrimination from society. 3) Normally, pharmacies had long service time, it was easy for PWID to get service during the nighttime. (SHA et al., 2008; Xue, LIU &Sun, 2013). Therefore, harm reduction programs could be implemented at pharmacies as the following being conducted. Firstly, pharmacies should be expanded to attain the legal requirements. Secondly, redeemable/coupon syringe program could be used to provide free syringes and used syringes disposal, sufficient remuneration for other services should be paid. Thirdly, training was important, especially among pharmacy staff who were less supportive than pharmacists (Sheridan et al, 1997; Myers et al., 1998; Matheson et al., 1999; Coffin et al., 2000). Trainings for pharmacy staff should include services related knowledge and skills, sensitive attitudes toward PWID, willingness for services provision. Misunderstandings such as that pharmacy-delivered services would increase the percentage of injection drug use should be eradicated.
Limitation and Future Direction
Qualitative sampling were used to recruit PWID and might not be representative of the population. In the future, respondent driven sampling (Heckathorn, 1997) could be utilized. Only 8% of the pharmacy participants were pharmacists, the results showed their attitude were generally negative but nearly neutral. Pharmacists’ attitude were considered more supportive than pharmacy staff (Sheridan et al, 1997; Myers et al., 1998; Matheson et al., 1999; Coffin et al., 2000). In future study, pharmacists’ attitude need be investigated to evaluate the feasibility for harm reduction services. Moreover, some statements in the questionnaire should be adjusted. For example, in terms of attitude, only 6% pharmacy staff agreed ‘always’ allowing PWID to buy syringes. Under the background that pharmacies policy permitted NPSS to PWID, instead of against “allowing PWID to buy syringes”, the disagreement probably were against “always” as pharmacy staff had their own judgment for suitable sales. In this study, staff only from pharmacies where NPSS were available were investigated. Prior studies have found that pharmacists who provided services to PWID held more positive attitudes than who did not provide (Sheridan et al, 1997; Myers et al., 1998; Matheson et al., 1999; Coffin et al., 2000). In the future, pharmacists and pharmacy staff from pharmacies where policy do not permit NPSS should also be studied.
In this paper, we documented that discrimination/business concerns were against pharmacy-delivered services, but we did not have sufficient information to disentangle the business concerns from discrimination and stigma against drug use. For the business concern, it may be useful to work with both PWID and pharmacy staff to find areas of mutual interest and benefit. For stigma, it may be useful to educate pharmacy staff on the science of drug addiction as well as foster positive interactions with PWID. Future studies to disentangle the business concerns from stigma of drug use are needed.
In this paper, we focused on the comparisons between PWID and pharmacy staff. Both perspectives are critical for improving pharmacy based harm reduction services. We only include questions where both perspectives are available.
Highlights (for review).
Pharmacies were the main sources of syringes sales in single piece at $0.16 USD for PWID, but not used syringe disposal.
Pharmacists’ attitudes were generally negative, discrimination towards PWID did exist.
3 of 8 pharmacy-delivered services were unavailable for PWID due to legal considerations and business concerns.
For every pharmacy-delivered service, PWID were more likely to endorse provision and to accept than the pharmacists.
Pharmacy-delivered services for PWID in Xichang were partly in reality, and could be feasible.
Acknowledgments
This study was supported by the National Institute on Drug Abuse (NIDA; R21 DA024971; Principal Investigator: Carl Latkin) and has been supported by the Johns Hopkins Center for AIDS Research (1P30AI094189). Yi Yang is supported by China Scholarship Council for her postdoctoral fellow study in JHSPH. We thank the individuals, who made this research possible, particularly Qi Luo, Ting Huang, Shou Liu, Si Qin from WCSPH and Qianping Liu, Zhengqing Jiang from XSDPC.
Footnotes
Conflict of Interest
We have no actual or potential financial, personal or other conflicts of interest related to the materials in the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Yi Yang, Email: yyang96@jhu.edu.
Carl Latkin, Email: carl.latkin@jhu.edu.
Rongsheng Luan, Email: luan_rs@scu.edu.cn.
Cui Yang, Email: cyang29@jhu.edu.
References
- 1.Settle E. AIDS in China: an annotated chronology: 1985–2003. Montreal: China AIDS Survey; 2003. [Google Scholar]
- 2.Ma Y, Li ZZ, Zhang KX. Identification of HIV infection among drug users in China. Zhonghua Liu Xing Bing Xue Za Zhi. 1990;11:184–185. (in Chinese) [Google Scholar]
- 3.China Ministry of Health, UNAIDS, WHO. Estimate for the HIV/AIDS epidemic in china. Beijing: China Ministry of Health; 2011. [Google Scholar]
- 4.Mathers BM, Degenhardt L, Phillips B, Wiessing L, Hickman M, Strathdee SA, Mattick RP. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. The Lancet. 2008;372(9651):1733–1745. doi: 10.1016/S0140-6736(08)61311-2. [DOI] [PubMed] [Google Scholar]
- 5.United Nations Office on Drugs and Crime. World Drug Report. 2014. (United Nations publication, Sales No. E.14.XI.7) [Google Scholar]
- 6.National bureau of statistics of the people’s republic of China. Total Population (201 year-end)(10000 persons) http://data.stats.gov.cn/english/easyquery.htm?cn=C01.
- 7.2011 Annual bulletin of financial and social development in Liangshan Prefecture. Bureau of Statistics of Liangshan Yi autonomous prefecture. 2012 http://www.lsz.gov.cn/lszrmzf/gmjjhshfztjgb/780375/index.html. Chinese.
- 8.2011 Annual bulletin of financial and social development in Sichuan Province. Bureau of Statistics of Liangshan Yi autonomous prefecture and Sichuan General Survey Group of National Bureau of Statistics of China. 2012 http://www.sc.stats.gov.cn/sjfb/tjgb/201203/t20120307_2577.html. Chinese.
- 9.Dai S, Shen Z, Zha Z, et al. Seroprevalence of HIV, syphilis, and hepatitis C virus in the general population of the Liangshan Prefecture, Sichuan Province, China[J] Journal of medical virology. 2012;84(1):1–5. doi: 10.1002/jmv.22214. [DOI] [PubMed] [Google Scholar]
- 10.LIU S, WANG QX, NAN L, et al. The changing trends of HIV/AIDS in an ethnic minority region of China: modeling the epidemic in Liangshan prefecture, Sichuan Province[J] Biomedical and Environmental Sciences. 2013;26(7):562–570. doi: 10.3967/0895-3988.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 11.Mathers BM, Degenhardt L, Ali H, Wiessing L, Hickman M, Mattick RP, Strathdee SA. HIV prevention, treatment, and care services for people who inject drugs: a systematic review of global, regional, and national coverage. The Lancet. 2010;375(9719):1014–1028. doi: 10.1016/S0140-6736(10)60232-2. [DOI] [PubMed] [Google Scholar]
- 12.Press Office of Ministry of Health. 2012 China AIDS Response Progress Report. Beijing: Ministry of Health the People’s Republic China; 2012. [Google Scholar]
- 13.Zhou Y-B, Wang Q-X, Liang S, Gong Y-H, Yang M-x, et al. HIV-, HCV-, and Co-Infections and Associated Risk Factors among Drug Users in Southwestern China: A Township-Level Ecological Study Incorporating Spatial Regression. PLoS ONE. 2014;9(3):e93157. doi: 10.1371/journal.pone.0093157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holtgrave DR, Pinkerton SD, Jones TS, et al. Cost and cost-effectiveness of increasing access to sterile syringes and needles as an HIV prevention intervention in the United States[J] JAIDS Journal of Acquired Immune Deficiency Syndromes. 1998;18:S133–S138. doi: 10.1097/00042560-199802001-00022. [DOI] [PubMed] [Google Scholar]
- 15.Ruan Y, Qin G, Yin L, Chen K, Qian H-Z, Hao C, et al. Incidence of HIV, hepatitis C and hepatitis B viruses among injection drug users in southwestern China: a 3-year follow-up study. Aids. 2007;21:S39–S46. doi: 10.1097/01.aids.0000304695.54884.4f. [DOI] [PubMed] [Google Scholar]
- 16.Ruan Y, Liang S, Zhu J, Li X, Pan SW, Liu Q, et al. Evaluation of harm reduction programs on seroincidence of HIV, hepatitis B and C, and syphilis among intravenous drug users in southwest China. Sexually transmitted diseases. 2013;40(4):323–8. doi: 10.1097/OLQ.0b013e31827fd4d4. [DOI] [PubMed] [Google Scholar]
- 17.Zhang L, Li J, Lai W, et al. Prevalence and correlates of needle-sharing among new and long-term injection drug users in southwest China [J] Substance use & misuse. 2010;45(14):2503–2523. doi: 10.3109/10826084.2010.487234. [DOI] [PubMed] [Google Scholar]
- 18.Wilson H, Brener L, Mao L, Treloar C. Perceived discrimination and injecting risk among people who inject drugs attending Needle and Syringe Programmes in Sydney, Australia. Drug Alcohol Depend. 2014 Sep 6; doi: 10.1016/j.drugalcdep.2014.08.018. pii: S0376–8716(14)01060-6 Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 19.Rivera AV, DeCuir J, Crawford ND, Amesty S, Lewis CF. Internalized stigma and sterile syringe use among people who inject drugs in New York City, 2010–2012. Drug Alcohol Depend. 2014 Oct 2; doi: 10.1016/j.drugalcdep.2014.09.778. pii: S0376–8716(14)01840-7 Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mateu-Gelabert P, Gwadz MV, Guarino H, Sandoval M, Cleland CM, Jordan A, Hagan H, Lune H, Friedman SR. The staying safe intervention: training people who inject drugs in strategies to avoid injection-related HCV and HIV infection. AIDS Educ Prev. 2014 Apr;26(2):144–57. doi: 10.1521/aeap.2014.26.2.144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hammett TM, Phan S, Gaggin J, et al. Pharmacies as providers of expanded health services for people who inject drugs: a review of laws, policies, and barriers in six countries[J] BMC health services research. 2014;14(1):261. doi: 10.1186/1472-6963-14-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lang K, Neil J, Wright J, Dell CA, Berenbaum S, El-Aneed A. Qualitative investigation of barriers to accessing care by people who inject drugs in Saskatoon, Canada: perspectives of service providers. Subst Abuse Treat Prev Policy. 2013 Oct 1;8:35. doi: 10.1186/1747-597X-8-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Glanz A, Byrne C, Jackson P. Role of community pharmacies in prevention of AIDS among injecting drug misusers: Findings of a survey in England and Wales. British Medical Journal. 1989;299(6707):1076–1079. doi: 10.1136/bmj.299.6707.1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sheridan J, Strang J, Taylor C, et al. HIV prevention and drug treatment services for drug misusers: a national study of community pharmacists’ attitudes and their involvement in service specific training[J] Addiction. 1997;92(12):1737–1748. [PubMed] [Google Scholar]
- 25.MYERS T, COCKERILL R, WORTHINGTON C, MILLSON M, RANKIN J. Community pharmacist perspectives on HIV/AIDS and interventions for injection drug users in Canada. AIDS Care: Psychological and Socio-medical Aspects of AIDS/HIV. 1998;10(6):689–700. doi: 10.1080/09540129848316. [DOI] [PubMed] [Google Scholar]
- 26.Matheson C, Bond CM, Mollison J. Attitudinal factors associated with community pharmacists’ involvement in services for drug misusers[J] Addiction. 1999;94(9):1349–1359. doi: 10.1046/j.1360-0443.1999.94913497.x. [DOI] [PubMed] [Google Scholar]
- 27.Coffin MPO, Linas BP, Factor SH, et al. New York City pharmacists’ attitudes toward sale of needles/syringes to injection drug users before implementation of law expanding syringe access[J] Journal of Urban Health. 2000;77(4):781–793. doi: 10.1007/BF02344038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koester SK, Lewis BA, Bush TW. Limited access to syringes for injection drug users in pharmacies in Denver, Colorado [J] Journal of the American Pharmacists Association. 2002;42(6s2):S88–S91. doi: 10.1331/1086-5802.42.0.s88.koester. [DOI] [PubMed] [Google Scholar]
- 29.Fuller CM, Galea S, Blaney S, et al. explaining the relationship between race/ethnicity and pharmacy purchased syringes among injection drug users in New York City [J] Ethnicity and Disease. 2004;14:589–596. [PubMed] [Google Scholar]
- 30.Mackridge AJ, Scott J. Experiences, attitudes and training needs of pharmacy support staff providing services to drug users in Great Britain: A qualitative study[J] Journal of Substance Use. 2009;14(6):375–384. [Google Scholar]
- 31.Scott J, Mackridge AJ. Pharmacy support staff involvement in, and attitudes towards, pharmacy- based services for drug misusers[J] International Journal of Pharmacy Practice. 2009;17(6):325–332. [Google Scholar]
- 32.Cooper EN, Dodson C, Stopka TJ, et al. Pharmacy participation in non-prescription syringe sales in Los Angeles and San Francisco counties, 2007[J] Journal of Urban Health. 2010;87(4):543–552. doi: 10.1007/s11524-010-9483-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rudolph AE, Standish K, Amesty S, et al. A community based approach to linking injection drug users with needed services through pharmacies: An evaluation of a pilot intervention in New York City[J] AIDS education and prevention: official publication of the International Society for AIDS Education. 2010;22(3):238. doi: 10.1521/aeap.2010.22.3.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zaller N, Jeronimo A, Bratberg J, et al. Pharmacist and pharmacy staff experiences with non-prescription (NP) sale of syringes and attitudes toward providing HIV prevention services for injection drug users (IDUs) in Providence, RI[J] Journal of Urban Health. 2010;87(6):942–953. doi: 10.1007/s11524-010-9503-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Torre C, Lucas R, Barros H. Syringe exchange in community pharmacies—The Portuguese experience [J] International Journal of Drug Policy. 2010;21(6):514–517. doi: 10.1016/j.drugpo.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 36.Janulis P. Pharmacy nonprescription syringe distribution and HIV/AIDS: a review[J] Journal of the American Pharmacists Association: JAPhA. 2011;52(6):787–797. doi: 10.1331/JAPhA.2012.11136. [DOI] [PubMed] [Google Scholar]
- 37.Zaller ND, Yokell MA, Apeakorang N, et al. Reported Experiences During Syringe Purchases in Providence, Rhode Island: Implications for HIV Prevention [J] Journal of health care for the poor and underserved. 2012;23(3):1310–1326. doi: 10.1353/hpu.2012.0094. [DOI] [PubMed] [Google Scholar]
- 38.Crawford ND, Amesty S, Rivera AV, et al. Randomized, community-based pharmacy intervention to expand services beyond sale of sterile syringes to injection drug users in pharmacies in New York City[J] American journal of public health. 2013;103(9):1579–1582. doi: 10.2105/AJPH.2012.301178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Busza J, Douthwaite M, Bani R, et al. Injecting behaviour and service use among young injectors in Albania, Moldova, Romania and Serbia[J] International Journal of Drug Policy. 2013;24(5):423–431. doi: 10.1016/j.drugpo.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 40.Pollini RA, Gallardo M, Ruiz S, et al. Over-the-Counter But Out of Reach: A Pharmacy-Based Survey of OTC Syringe Sales in Tijuana, Mexico[J] Journal of health care for the poor and underserved. 2014;25(2):637–651. doi: 10.1353/hpu.2014.0090. [DOI] [PubMed] [Google Scholar]
- 41.Rose VJ, Lutnick A, Kral AH. Feasibility of Providing Interventions for Injection Drug Users in Pharmacy Settings: A Case Study among San Francisco Pharmacists [J] Journal of psychoactive drugs. 2014;46(3):226–232. doi: 10.1080/02791072.2014.921745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Quinn B, Chu D, Wenger L, Bluthenthal RN, Kral AH. Syringe disposal among people who inject drugs in Los Angeles: the role of sterile syringe source. Int J Drug Policy. 2014 Sep;25(5):905–10. doi: 10.1016/j.drugpo.2014.05.008. Epub 2014 May 21. [DOI] [PubMed] [Google Scholar]
- 43.Watson T, Hughes C. Pharmacists and harm reduction: a review of current practices and attitudes[J] Canadian Pharmacists Journal/Revue des Pharmaciens du Canada. 2012;145(3):124–127. e2. doi: 10.3821/145.3.cpj124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lutnick A, Case P, Kral AH. Injection drug users’ perspectives on placing HIV prevention and other clinical services in pharmacy settings[J] Journal of Urban Health. 2012;89(2):354–364. doi: 10.1007/s11524-011-9651-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hammett TM, Kling R, Johnston P, et al. Patterns of HIV prevalence and HIV risk behaviors among injection drug users prior to and 24 months following implementation of cross-border HIV prevention interventions in northern Vietnam and southern China[J] AIDS Education & Prevention. 2006;18(2):97–115. doi: 10.1521/aeap.2006.18.2.97. [DOI] [PubMed] [Google Scholar]
- 46.Zhao G, Detels R, Gu F, et al. The distribution of people seeking STD services in the various types of health care facilities in Chao Yang District, Beijing, China. Sex Transm Dis. 2008;35:65–67. doi: 10.1097/OLQ.0b013e318148b4dc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wong WC, Zhang J, Wu SC, et al. The HIV related risks among men having sex with men in rural Yunnan, China: A qualitative study. Sex Transm Infect. 2006;82:127–30. doi: 10.1136/sti.2005.016790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.SHA L, LI Y, ZHU Y. A sampling survey on syringe exchange and methadone maintenance treatment (MMT) among drug abusers in Yunnan province [J][J] Chinese Journal of AIDS & STD. 2008;3:015. [Google Scholar]
- 49.XUE H, LIU H, SUN J. An analysis of service model and cost of needle and syringe exchange in 19 counties of Yunnan[J] Chinese Journal of AIDS & STD. 2013;5:011. [Google Scholar]
- 50.Hammett TM, Phan S, Gaggin J, et al. Pharmacies as providers of expanded health services for people who inject drugs: a review of laws, policies, and barriers in six countries[J] BMC health services research. 2014;14(1):261. doi: 10.1186/1472-6963-14-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ruan Y, Chen K, Hong K, He Y, Liu S, Zhou F, et al. Community-based survey of HIV transmission modes among intravenous drug users in Sichuan, China. Sexually transmitted diseases. 2004;31(10):623–7. doi: 10.1097/01.olq.0000140018.24262.4a. [DOI] [PubMed] [Google Scholar]
- 52.Yin L, Qin G, Qian HZ, Zhu Y, Hu W, Zhang L, Shao Y. Continued spread of HIV among injecting drug users in southern Sichuan Province, China. Harm Reduct J. 2007;4(6) doi: 10.1186/1477-7517-4-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.China, National Narcotics Control Commission. Annual Report on Drug Control in China 2013. Beijing: 2013. [Google Scholar]
- 54.China food and drug administration. Measures for the Administration of Permits for Medical Device Operation Enterprises. 2004–2014. [Google Scholar]
- 55.The state Council of China. Regulation of the People’s Republic of China on HIV/AIDS prevention and control. 2006. [Google Scholar]
- 56.The state Council of China. Regulations of the People’s Republic of China on Medical institutions management. 1994. [Google Scholar]
- 57.China Ministry of Health. Regulations of the People’s Republic of China on Medical institutions management, implementing rules. 1994. [Google Scholar]
- 58.The state Council of China. Management Regulation of the People’s Republic of China on Medical waste. 2003. [Google Scholar]
- 59.Standing committee of national congress of China. The Drug Administration Law of People’s Republic of China. 2001. [Google Scholar]
- 60.The state Council of China. Regulation of the people’s Republic of China on narcotic drugs and psychotropic drugs. 2005. [Google Scholar]
- 61.Standing committee of national congress of China. Law of the People’s Republic of China on Medical Practitioners. 1998. [Google Scholar]
- 62.Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations[J] Social problems. 1997;44(2):174–199. [Google Scholar]


