Abstract
New densitometer installation requires cross-calibration for accurate longitudinal assessment. When replacing a unit with the same model, ISCD recommends cross-calibrating by scanning phantoms 10 times on each instrument and states spine BMD should be within 1%, while total body lean, fat and %fat mass should be within 2% of the prior instrument. However, there is limited validation that these recommendations provide adequate total body cross-calibration. Here we report a total body cross-calibration experience with phantoms and humans.
Cross-calibration between an existing and new Lunar iDXA was performed using three encapsulated spine phantoms (GE-Lunar, BioClinica and Hologic), one total body composition phantom (BioClinica) and 30 human volunteers. Thirty scans of each phantom and a total body scan of human volunteers were obtained on each instrument.
All spine phantom BMD means were similar (within 1%; < −0.010 g/cm2 bias) between the existing and new DXA unit. The BioClinica Body Composition Phantom (BBCP) BMD and BMC values were within 2% with biases of 0.005 g/cm2 and −3.4g. However, lean and fat mass and %fat differed by 4.6 to 7.7% with biases of +463g, −496g and − 2.8%, respectively. In vivo comparison supported BBCP data; BMD and BMC were within ~2% but lean and fat mass and %fat differed from 1.6 to 4.9% with biases of +833g, −860g and −1.1%. As all body composition comparisons exceeded the recommended 2%, the new densitometer was recalibrated. Following recalibration, in vivo bias was lower (<0.05%) for lean and fat; −23g and −5g. Similarly, BBCP lean and fat agreement improved.
In conclusion, the BBCP behaves similarly, but not identical, to human in vivo measurements for densitometer cross-calibration. Spine phantoms, despite good BMD and BMC agreement, did not detect substantial lean and fat differences observed using BBCP and in vivo assessments. Consequently, spine phantoms are inadequate for DXA whole body composition cross-calibration.
Keywords: dual-energy x-ray absorptiometry, cross-calibration, whole body phantom, spine phantom, in vivo
INTRODUCTION
The need to cross-calibrate replacement DXA scanners is well recognized (1). More recently, the ISCD has published Official Positions describing recommendations for cross-calibration of DXA systems used for body composition (2) which are as follows:
When changing hardware, but not the entire system, or when replacing a system with the same technology (make and model), cross-calibration should be performed by having one technologist scan one phantom 10 times, with repositioning, before and after hardware change.
If a greater than 1% difference in mean BMD is observed, contact the manufacturer for service/correction.
If a greater than 2% difference in mean percent fat, fat mass or lean mass is observed, contact the manufacturer for service/correction.
However, there are only limited data validating this approach in practice. Moreover, as total body composition phantoms are not widely available, it is logical to assess if it is possible to utilize the much more widely available spine phantoms for this purpose.
Phantoms are at best “patient mimics,” and have constraints (3). For example, it is logical that the ideal body composition phantom, would be designed along the lines of the Hologic Total Body phantom which is the size of a human but therefore is large, heavy, costly to ship, and cumbersome for the operator to use (4), thus making it less than ideal in both the clinical setting and clinical trials. For the latter a semi-portable phantom is required that, preferably, can be carried and used by a single operator. The BioClinica Body Composition Phantom (BBCP), (BioClinica Inc, Princeton, NJ) is a design compromise between size and weight, to allow reasonably easy transit and the criteria of being managed by a single operator versus being anthropomorphically correct. Importantly, the BBCP can be scanned and analyzed using all major DXA platforms, thus making it suitable for multicenter clinical trials. To the authors knowledge this is the first publication evaluating this new body composition phantom.
Here, cross-calibration of a new DXA scanner of the same manufacturer and model as an existing (GE Lunar iDXA) unit is presented. The underpinning concept is that human in vivo measurements constitute the gold standard for densitometer cross-calibration and that spine phantoms would be less representative of fat and lean mass than either a total body phantom or human in vivo total body measurements. Additionally, we evaluated whether the BBCP has the potential to replicate human in vivo data for this purpose.
METHODS
Study design
Division 1 athletes were being longitudinally scanned on a GE Healthcare Lunar (Madison, WI) iDXA densitometer for body composition assessments to facilitate athletic training and injury rehabilitation. As a new iDXA densitometer was acquired, future scanning of this cohort was transferred to this new instrument. Consequently, it was recognized that cross-calibration for body composition measurement was required for accurate longitudinal assessment. To this end, phantoms and healthy volunteers were scanned on these two iDXA instruments. All scans were acquired and analyzed with enCORE software; version 13.31 for the existing scanner and version 14.1 for the new scanner. Thirty human volunteers were scanned on both instruments on the same day over a 36-day timespan. This exercise was categorized as a quality assurance activity and consequently determined IRB exempt by the University of Wisconsin Health Sciences Human Subjects Committee.
Phantoms
Three DXA spine phantoms and one prototype body composition phantom, detailed below, were measured thirty times on each densitometer without repositioning five days after the last human scans were obtained. These encapsulated spine phantoms were: 1. Lunar spine phantom, (GE Lunar, Madison WI); 2. Hologic Spine phantom, (Hologic Inc. Bedford MA) and 3. Bone Fide Phantom (BFP) (BioClinica, Princeton, NJ), see Figure 1. These three phantoms are of similar size and weight but have some characteristic differences. The Lunar phantom has an aluminum bar embedded in acrylic representing approximately 35% fat. The bar is straight edged, but each vertebra provides a different density value. The Hologic spine phantom is a true anthropomorphic phantom that mimics human spine anatomy, however, each vertebral body has similar densities. The insert is made of calcium hydroxyapatite, and the clear acrylic surround is hyper-physiological, being around 60% fat. The BFP is a shaped calcium hydroxyapatite bar with 4 “vertebrae,” each one of separate density and size. The acrylic is a two-phase mixture that provides a normal physiological soft-tissue of approximately 24%. The BFP is the only phantom that has been shown to match subject data for spine BMD by linear regression (5,6).
Figure 1. Encapsulated spine phantoms.
Three spine phantoms were evaluated for cross-calibration, A. GE Lunar (Madison, WI), B. Hologic (Bedford,MA) and C. BioClinica Bona Fide Phantom (Princeton, NJ)
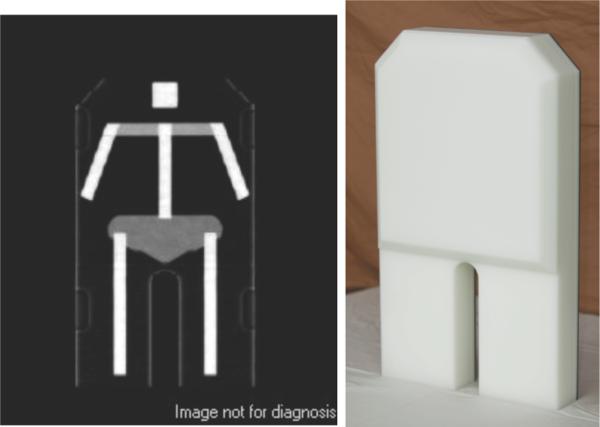
A prototype total body phantom, the BioClinica Body Composition Phantom (BBCP), (Figure 2) was also scanned. This phantom measures 60 cm in length, 36 cm in width, 9 cm in height and weighs approximately 16 kg and therefore does not replicate the adult human body mass or size. However, the phantom does replicate human body composition proportionally in that it contains high-density polyethylene, polyvinyl chloride and an aperture of aluminum to simulate different human soft tissue and bone compositions.
Figure 2. Body Composition Phantom.
BioClinica Body Composition Phantom Prototype (BBCP). Whole body phantom designed to emulate bone, lean and fat mass for the purpose of monitoring DXA scanners for body composition. The phantom measures 60 × 36 × 9 cm and weighs ~16 kg.
Participants
Thirty adult volunteers (15 male/15 female) were scanned once on each densitometer. Their mean (SD) age was 31.1 (10.8), range 20-60 years; and mean (SD) BMI was 24.1 (2.8), range 19.7-30.7 kg/m2. The entire body of all volunteers was contained within the scan field and positioning was per ISCD recommendations, i.e. NHANES style.(2) Both scans in each individual were obtained on the two scanners within 60 minutes and food ingestion and voiding were prohibited between scans.
Statistical Analysis
Agreement between the two densitometers was evaluated by linear regression and Bland-Altman analysis using Analyze-it software v2.3 (Leeds, UK).
RESULTS
Spine Phantoms
All three spine phantoms demonstrated a < 1% difference in L1-L4 mean BMD and BMC between the new and existing densitometer (Figure 3 and Table 1). The L1-L4 BMD mean biases between instruments were ≤ −0.010 g/cm2 with each phantom (Table 1).
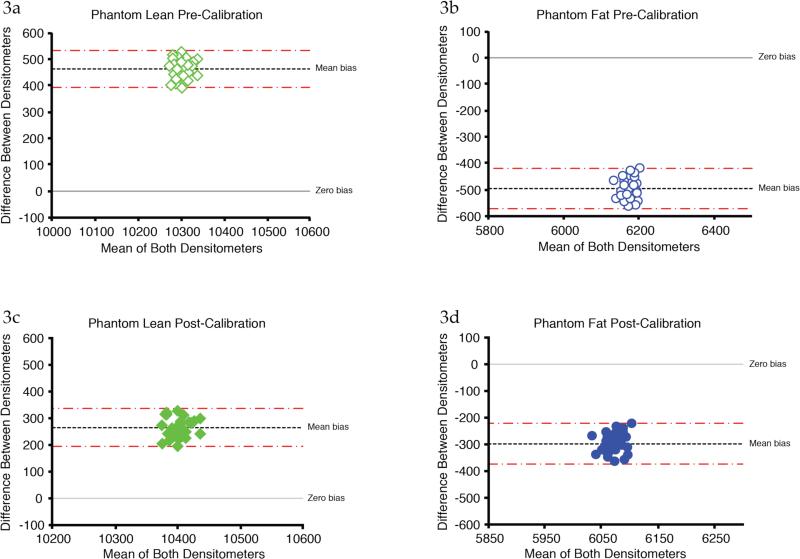
Figures 3. a-d: Bland-Altman Plots of Lean and Fat BioClinica Body Composition Phantom Data Before and After Recalibration.
Lean and fat differed between instruments by 4.6% & 7.8% with biases of +463 g & −496 g (3a-b). After recalibration, instrument agreement improved to 2.6% for lean and 4.8% in fat, with biases of +265 g and −298 g respectively (3c-d).
Table 1.
Phantom and Human In Vivo Data and Comparisons on the Existing and New Instrument
| GE Spine Phantom L1-L4 | BonaFide Phantom (BFP) L1-L4 | Hologic Phantom L1-L4 | Bioclinica Body Composition Phantom (BBCP) Total Body | Human In Vivo Total Body | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Bias | Existing Unit Mean | New Unit Mean | Bias | Existing Unit Mean | New Unit Mean | Bias | Existing Unit Mean | New Unit Mean | Bias | Existing Unit Mean | New Unit Mean | Bias | Existing Unit Mean | New Unit Mean | |
| BMD g/cm2 | −0.007 | 1.188 | 1.195 | −0.008 | 1.070 | 1.079 | −0.003 | 1.105 | 1.108 | 0.005 | 1.081 | 1.086 | 0.026 | 1.250 | 1.276 |
| Area cm2 | 0.252 | 51.29 | 51.04 | 0.269 | 44.77 | 44.51 | 0.512 | 52.46 | 51.95 | 0.067 | 497.6 | 497.7 | −11.3 | 2432 | 2420 |
| BMC g | −0.062 | 60.93 | 61.00 | −0.085 | 47.92 | 48.00 | 0.425 | 57.99 | 57.56 | −3.367 | 537.7 | 541.1 | −50.9 | 3051 | 3102 |
| Lean g | - | - | - | - | - | - | - | - | - | 462.9 | 10534 | 10071 | 832.9 | 54230 | 53397 |
| Fat g | - | - | - | - | - | - | - | - | - | −496.4 | 5924 | 6420 | −860.2 | 17507 | 18267 |
| Fat % | - | - | - | - | - | - | - | - | - | −2.84 | 34.9 | 37.7 | −1.14 | 23.4 | 24.6 |
Total Body Phantom
The total body mean BMD and BMC were < 1% different between the existing and new densitometer using the BBCP (Table 1). Mean total body BMD and BMC bias was 0.005 g/cm2 and 3.4 g respectively (Table 1). Total body mean lean and fat differed by 4.6% and 7.8% respective with corresponding mean biases of +463 g and −496 g (Figure 3a/b).
Human In Vivo Measurement
The total body lean and fat mass initially differed by 1.6% and 4.2% between the two densitometers with respective biases of +833 g and −860 g (Figure 3c-d and Table 1). As the total body fat value difference between instruments exceeded the recommended 2%, the manufacturer was contacted and the new densitometer was recalibrated to improve lean and fat mass agreement with the existing scanner. No adjustment was made to BMC or bone area.
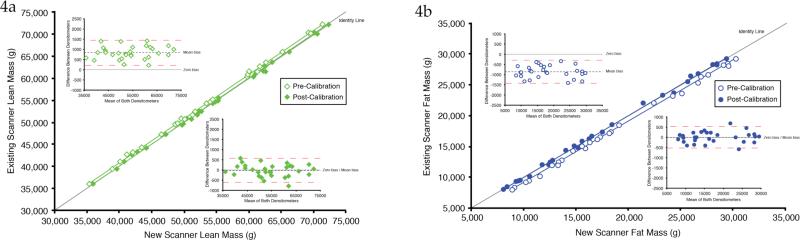
Post Recalibration Analysis
Following manufacturer recalibration, re-analysis of the human in vivo scans revealed lower bias for lean and fat down to a mean difference of −23 g and −5 g respectively (Figures 4a/b & Table 2) thereby decreasing the between-scanner difference to < 0.05%. Similarly, agreement of the body composition phantom lean and fat improved, although still exceeded the ISCD recommendation of <2% difference in body composition in that, despite recalibration, the BBCP biases for lean and fat were reduced to 265 g (2.5%) and −298 g (−4.8%) respectively. As spine BMD did not differ between instruments and the intended use of this instrument was soft tissue body composition assessment, BMD was not recalibrated and therefore the spine phantom re-analysis was not performed.
Figure 4. a-b: Lean and Fat In Vivo Data Before and After Recalibration.
Figure 4a depicts the total body lean mass agreement as assessed by linear regression and Bland-Altman plots prior to (open circles) and following densitometer re-calibration (closed circles). Figure 4b depicts the same evaluations for total body fat mass prior to (open diamonds) and following recalibration (closed symbols). Pre-recalibration the regression equations were y = 1.0037x + 637.37 for lean and y = 0.9953x – 774.61 for fat. Following re-calibration the regression equations were y = 0.9948x = 259.91 and y = 1.0034x – 64.702 respectively. There was a change in the slope and bias of 0.009 and 855.6 g respectively in lean and −0.008 and −855.6 g respectively in fat.
Table 2.
BBCP Phantom and Human Comparisons on the Existing and New Instrument Post Recalibration
| BBCP After Recalibration | Human In Vivo After Recalibration | |||||
|---|---|---|---|---|---|---|
| Bias | Existing Mean | New Mean | Bias | Existing Mean | New Mean | |
| Lean (g) | 264.7 | 10534 | 10269 | −22.7 | 54230 | 54252 |
| Fat (g) | −298.1 | 5924 | 6222 | −4.6 | 17507 | 17512 |
| %Fat (%) | −1.675 | 34.9 | 36.53 | 0.98 | 23.4 | 23.4 |
DISCUSSION
In this study, the ISCD recommendations (1,2) for body composition cross-calibration when replacing a densitometer were implemented. To the authors’ knowledge, this study is the first to compare data from spine phantoms and a total body phantom, with in vivo cross-calibration. Although spine phantoms are commonly used due to their wide accessibility, these data demonstrate that using of any of these three encapsulated spine phantoms does not adequately cross calibrate densitometers for body composition measurement. Importantly, even though the L1-L4 mean BMD differed by <1%, thus meeting the ISCD recommendations, spine phantom data did not detect the need for manufacturer recalibration for total body fat and lean mass measurement. This is not surprising given that spine phantoms are designed to mimic spine BMD, not total body fat/lean mass and moreover are not representative of total body size. This study suggests that human in vivo measurement is necessary for optimal total body DXA cross-calibration despite the same make and model densitometer. Utilization of these in vivo data demonstrated a need for manufacturer recalibration, which resulted in total body fat and lean mass measurements that were virtually identical between the two instruments in the in vivo sample, differing by much less than the recommended 2%.
The ISCD also recommends cross-calibration using an adequate total body phantom for lean and fat measurement before and after hardware change of the same make and model instrument.(2) Although there are limited data regarding cross-calibration for body composition with phantoms, to our knowledge, none of the existing studies were compared with in vivo cross-calibration.(7,8) Indeed, the ISCD Position Development Conference noted that additional research was needed to evaluate the link between in vivo cross-calibration and phantom measurements.(2) The data presented here are the first to compare phantom and in vivo evaluation for body composition cross-calibration assessment. In this study, data from the BioClinica prototype total body phantom were similar, but not identical to, the in vivo results in that fat and lean mass differences still exceeded 2% following instrument recalibration while the in vivo data were virtually identical. While not reaching the recommended level of agreement, it is notable that recalibration did substantially improve between scanner phantom agreement. To summarize, these data demonstrate that body composition results of this prototype BBCP body composition behaved similar to, but did not perfectly replicate, human data. It is noteworthy that this prototype phantom is designed to replicate percent fat of the average human, not the relatively low body fat proportion observed in this population (24%) which was selected to be similar to athletes,(~20% at UW).
It is possible that phantoms do not reproduce human in vivo results because current total body phantoms do not allow measurement of various mass ranges such as are generated with in vivo sampling. The fact that the single data point for lean and fat mass generated by this phantom are close to the in vivo regression lines, does suggests that phantoms, such as the BBCP, might be suitable for densitometer cross-calibration if the mass measured spanned a clinically relevant range. Emphasizing this important point, the ISCD Position paper states “An adequate phantom for scanner cross-calibration would have to show a similar range of relevant values as the patient cohort of interest.” (2) Further evaluation of phantoms that can be configured to a variety of mass and composition seems indicated and are in development. To this end, the results from this phantom are encouraging and provide support for the further development of the BBCP.
It is worthy of comment that two versions of software were utilized between the existing and new instruments. As new instruments are installed with the most current software, cross calibration between existing and new instruments will routinely occur using different software versions, consequently, this approach replicates a true clinical environment. One could postulate this would contribute to the bias as there can be measurement differences between software versions, however, recalibration of the new instrument, if needed, will address this off-set should it exist.
Limitations of the study include use of only a single total body phantom, that this phantom was a prototype, and that only a single make and model of densitometer was evaluated. The ability to evaluate other commercially available whole body phantoms would have been a substantial advantage. However, to our knowledge, such comparisons do not exist. Whether these findings would apply to other comparisons of like-model densitometers is not known. It is worthy of note that this study, and the ISCD recommendations cited in the introduction, apply to cross-calibration of the same make and model of densitometer. As DXA technology differs between manufacturers, ISCD does recommend in vivo cross-calibration when evaluating instruments for densitometers from different manufacturers.(2) Finally, as the in vivo sample used in this trial was a relatively young and non-obese group, these data might not be replicated using other populations. However, the sample in this exercise was selected, as it closely resembled the population that will be scanned on these instruments.
In conclusion, standard spine phantoms are inadequate for densitometer cross calibration for total body fat and lean measurements. Additionally, when replacing DXA scanners for the purpose of total body composition assessment, even with the same make and model instrument, in vivo cross-calibration is needed at this time to ensure comparable body composition results.
References
- 1.Baim S, Binkley N, Bilezikian JP, et al. Official positions of the International Society for Clinical Densitometry and Executive summary of the 2007 ISCD position development conference. J. Clin. Densitom. 2008;11:75–91. doi: 10.1016/j.jocd.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 2.Hangartner TN, Warner S, Braillon P, Jankowski L, Shepherd J. The Official Positions of the International Society for Clinical Densitometry: acquisition of dual-energy X-ray absorptiometry body composition and considerations regarding analysis and repeatability of measures. J. Clin. Densitom. 2013;16(4):520–36. doi: 10.1016/j.jocd.2013.08.007. [DOI] [PubMed] [Google Scholar]
- 3.Miller CG. Organization of the clinical trial by the sponsor. In: Pearson D, Miller CG, editors. Clinical Trials in Osteoporosis. Second ed. Springer-Verlag; London: 2007. pp. 75–90. [Google Scholar]
- 4.Anonymous . 2011-2012 Body Composition Procedures Manual National Health and Nutrition Examination Survey (NHANES) CDC; Atlanta, GA: pp. 6–27-6-30. [Google Scholar]
- 5.Pearson D, Cawte SA, Green DJ. A comparison of phantoms for cross-calibration of lumbar spine DXA. Osteoporos. Int. 2002;13:948–954. doi: 10.1007/s001980200132. [DOI] [PubMed] [Google Scholar]
- 6.Pearson D. Standardization and pre-trial quality control. In: Pearson D, Miller CG, editors. Clinical Trials in Osteoporosis. Springer; New York: 2002. pp. 43–65. [Google Scholar]
- 7.Guo Y, Franks PW, Brookshire T, Antonio Tataranni P. The intra- and inter-instrument reliability of DXA based on ex vivo soft tissue measurements. Obes. Res. 2004;12(12):1925–9. doi: 10.1038/oby.2004.241. [DOI] [PubMed] [Google Scholar]
- 8.Diessel E, Fuerst T, Njeh CF, et al. Evaluation of a new body composition phantom for quality control and cross-calibration of DXA devices. J. Appl. Physiol. 2000;89(2):599–605. doi: 10.1152/jappl.2000.89.2.599. [DOI] [PubMed] [Google Scholar]