Abstract
Introduction
Tight glycemic control and timely treatment can improve outcomes in patients with diabetes yet many remain sub-optimally controlled. The objective of the current study was to evaluate the effect of switching patients with sub-optimally controlled diabetes to the V-Go® (Valeritas Inc., Bridgewater, NJ, USA) Disposable Insulin Delivery device.
Methods
A retrospective analysis of electronic medical records was conducted to assess patients with sub-optimal glycemic control defined as a glycated hemoglobin (HbA1c) >7%, switched to V-Go. Blood glucose control defined as change from baseline in HbA1c, prescribed insulin doses, body weight, concomitant anti-hyperglycemic agents, and reported hypoglycemia were collected prior to switching to V-Go and during V-Go use.
Results
Two-hundred and four patients were evaluated during the study period. Overall, there was a significant decrease in HbA1c after switching to V-Go at the 14- and 27-week follow-up visits. The least-squares mean (LSM) change in HbA1c (95% confidence interval) from baseline to 14 weeks was −1.53% (−1.69% to −1.37%; P < 0.001), and from baseline to 27 weeks was −1.79% (−1.97% to −1.61%; P < 0.001). Significant reductions in mean HbA1c were achieved at both visits in all patient subsets: Patients with type 2 and type 1/latent autoimmune diabetes in adults (LADA); patients using insulin at baseline and patients naïve to insulin at baseline. Patients administering insulin at baseline required significantly less insulin on V-Go (86–99 LSM units/day at baseline to 58 LSM units/day at 27 weeks; P < 0.001). Across all patients, reported hypoglycemic events were no more frequent on V-Go than on previous therapy.
Conclusion
V-Go is safe and effective in patients with sub-optimally controlled diabetes requiring insulin therapy. Glycemic control improved significantly, less insulin was required, and hypoglycemic events were similar after patients switched to insulin delivery by V-Go.
Funding
Valeritas, Inc.
Electronic supplementary material
The online version of this article (doi:10.1007/s13300-015-0138-7) contains supplementary material, which is available to authorized users.
Keywords: Basal-bolus, Diabetes, Hyperglycemia, Insulin, Intensified, Mealtime, Prandial, V-Go®
Introduction
Diabetes mellitus is a prevalent disease on the rise with serious impact on healthcare costs and patient safety. In the United States alone there are 29.1 million patients with diabetes, including 8.1 million undiagnosed cases [1]. The majority are patients diagnosed with type 2 diabetes, and approximately 1.25 million patients are diagnosed with type 1 diabetes [1]. Long-term complications of diabetes include microvascular complications, stroke, kidney disease, blindness, and neuropathy and it is well established that tight glycemic control and timely treatment improve outcomes and reduce complications [2, 3].
Patients with type 1 diabetes require continuous insulin infusion or multiple daily injections (MDI) of insulin. Due to the decline of islet cell function over time it is likely that many patients with type 2 diabetes will eventually require insulin therapy as treatment is progressed.
In type 2 diabetes, insulin therapy is typically initiated with a single injection of basal insulin, and if targets are not met after active titration patients may be progressed to a basal-bolus regimen with MDI. Basal insulin therapy is sufficient for many patients; however, despite optimization of basal insulin evidence suggests <40% of patients with type 2 diabetes achieve glycemic targets [3]. In the Treating to Target in Type 2 diabetes study (ClinicalTrials.gov identifier, NCT00184600), most patients (82%) required insulin intensification to include mealtime bolus insulin by 3 years to achieve glycemic targets [4].
Increased complexity of treatment regimens leads to decreased adherence, which in turn impacts efficacy [5–7]. Insulin non-adherence has been correlated with patient perceptions of regimen inflexibility and the burden on one’s lifestyle [8]. Surprisingly, 72% of patients on MDI therapy report they never take injections outside of the home [9]. Addressing these treatment barriers may improve patient outcomes.
V-Go® (Valeritas, Inc., Bridgewater, NJ, USA), shown in Fig. 1, is a disposable, wearable insulin delivery device that delivers a continuous basal rate of insulin, as well as on-demand mealtime dosing. V-Go is available in basal rates of 20, 30, or 40 units/24 h and can administer up to an additional 36 units of insulin for mealtime bolus dosing in 2 unit increments. V-Go is filled with U-100 fast-acting insulin (insulin lispro, rDNA origin or insulin aspart, rDNA origin have been tested by Valeritas and found safe for use in V-Go) [10] and is affixed to the skin. The push of a button inserts a 4.6 mm 30 gauge stainless steel needle subcutaneously, which initiates delivery of a continuous preset basal rate of insulin. Patients can self-administer mealtime bolus doses by pressing the bolus ready button and the bolus delivery button through clothing for discreet insulin administration. V-Go uses a hypoallergenic and latex-free adhesive to adhere to the skin, and is designed to be removed and replaced every 24 h.
Fig. 1.
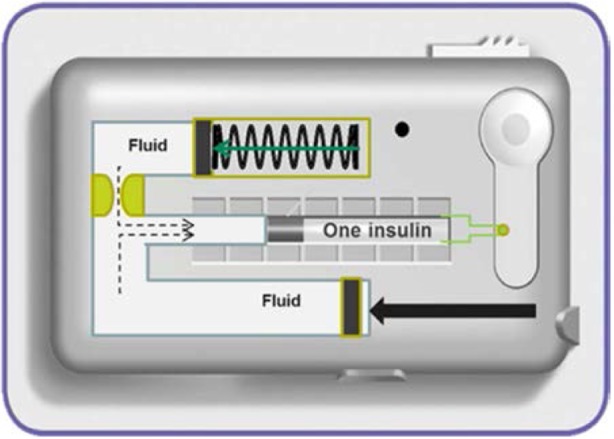
V-Go Disposable Insulin Delivery device
Use of V-Go has been associated with improved glycemic control [11–13]. An investigation done by Rosenfeld and colleagues showed a decrease in glycated hemoglobin (HbA1c) when patients were switched to insulin delivery by V-Go, and an increase in HBA1c following the cessation of V-Go [11]. The current study examined real-world use of V-Go in a specialized diabetes system. The purpose of this study was to evaluate glycemic control after patients with sub-optimally controlled diabetes on previous therapeutic regimens were switched to insulin therapy delivered by V-Go.
Methods
Study Design and Criteria
The study was conducted as a retrospective review of the electronic medical record (EMR) database for Diabetes America, a specialized diabetes comprehensive care clinic setting which includes 13 centers located across major metropolitan areas of Texas. Patients were prescribed V-Go by health care providers as part of their standard clinical practice with the goal of improving HbA1c levels. Baseline insulin doses, HbA1c, changes to concomitant medications, and weight were all factors considered by clinicians when determining the starting V-Go dose. Additionally, it was taken into consideration that delivering insulin via continuous subcutaneous infusion has been shown to typically reduce insulin requirements by 20–30% [14, 15]. Patient education and support included basic instruction on the use of V-Go by a member of the health care team and supportive written materials as well as access to a 24 h customer care center were provided by the manufacturer as is routine for all patients initiated on V-Go. Patients were managed per clinician standard of care including timing and frequency of follow-up visits and medication management. A systematic search using keywords identified potential patients switched to V-Go between April 1, 2013 and October 3, 2014 and patient charts were then reviewed against study inclusion and exclusion criteria to determine study eligibility. Inclusion criteria required (1) patients diagnosed with diabetes mellitus (type 1, type 2, or LADA); (2) age equal to or >21 years; (3) baseline HbA1c between 7% and 14% (within 6 weeks of V-Go initiation); (4) previously prescribed basal or basal-bolus insulin therapy or naïve to insulin therapy, with or without anti-hyperglycemic medications; and switched to insulin delivery by V-Go; and (5) a minimum of one subsequent HbA1c lab value on V-Go. Patients were excluded for (1) history of treatment with U-500 insulin preceding V-Go initiation or the non-Food and Drug Administration approved utilization of U-500 insulin delivery by V-Go; (2) receiving insulin delivery via an insulin pump immediately preceding V-Go initiation; (3) pregnancy or lactation; (4) undeterminable insulin dosing due to insufficient chart information; or (5) a history of pancreatic cancer.
The primary endpoint in the study was change in HbA1c from baseline. Secondary endpoints evaluated in the study included insulin dose, body weight, and hypoglycemic events. The study protocol was reviewed and approved by Allendale investigational review board, and a waiver of informed consent was approved.
Data Collection
Clinical and demographic data were extracted from the EMR at baseline and for all subsequent office visits when an HbA1c value was captured and the patient remained on V-Go. Clinical data extracted included HbA1c values, fasting plasma glucose levels, prescribed and patient reported insulin use, body weight, concomitant anti-hyperglycemic medications, and patient-reported hypoglycemic events. It is common to prescribe insulin dosing as a range, with a lower limit representing the primary dose excluding titration and correction, and the upper limit allowing additional units to optimize insulin therapy (titration, correction, sliding scale). Both the lower and upper limits of the prescribed baseline insulin use were collected in the study. Patient-reported insulin dosing was also captured when available for comparison to actual prescribed doses.
Concomitant anti-hyperglycemic medications were recorded at baseline and at each follow-up visit. Patients were categorized as having an increase, decrease or no change to baseline concomitant medications at the follow-up visit. An addition or removal of a medication, as well as a change in dose with a proven difference in efficacy over the previous dose qualified as a change in concomitant medications. The time course of the change in medications relative to the follow-up visit was also reviewed during the data collection process to assess whether adequate time had elapsed for any therapeutic benefit of the medication change to take effect. It was confirmed that in 90% of patients categorized as having a change in concomitant medications, at least 2 months had elapsed from the time of the change to the time of the follow-up HbA1c value, so any impact of the concomitant medication change would be reflected in the follow-up HbA1c value.
The principal investigator oversaw review of subject records to determine study eligibility, and data collection. Records from all sites were reviewed via the EMR database in Plano, Texas. Clinical results on V-Go were collected through March 31, 2015 for inclusion in the current study analysis.
Statistical Analysis
Independent statistical analyses were performed by the Department of Mathematics and Statistics at the University of Central Oklahoma. A one-factor repeated measures analysis of covariance (ANCOVA) model including a factor for time period and the baseline measurement as the covariate was performed to test for the differences from baseline for HbA1c, insulin dosage, and weight. The influence of baseline HbA1c on change in HbA1c was analyzed using a two-factor repeated measures analysis of variance (ANOVA) including factors for time period, baseline HbA1c range (7.1–8.9%, 9.0–10.4%, 10.5–13.9%), and interaction between the two factors. To test for differences in the mean weight (kg), total daily dose (TDD) of insulin, and HbA1c from baseline to week 14 on V-Go among those with either an increase, decrease, or no change to concomitant medications, a two-factor repeated measures ANOVA was performed for each variable with factors for time period, change in concomitant meds, and interaction between the two factors. For all of the tests, a spatial power covariance structure was modeled to adjust for the differences in the number of days between time periods. Changes from baseline for all analyses are expressed as least-squares means (LSM) with 2-sided 95% confidence intervals (CIs) unless otherwise noted.
If any ANOVA or ANCOVA resulted in a significant P value (P < 0.05) the analysis was followed by pairwise comparisons using Tukey’s adjustment for multiplicity. All tests were performed using proc mixed in SAS v.9.3 (SAS Institute Inc., Cary, NC, USA).
Results
Study Population
A database query identified 245 eligible patients based on inclusion criteria, of which 204 were included in the analysis. Prior use of U-500 regular insulin and undeterminable insulin dosing were the leading reasons for exclusion. All patients had one follow-up HbA1c result per protocol inclusion criteria and a second follow-up HbA1c result was available during the analysis period for 137 patients. The mean time from start of V-Go to the first follow-up visit was 13.87 ± 6.14 weeks and the mean time to the second follow-up visit was 26.86 ± 8.96 weeks. Results will therefore be presented for 14- and 27-week visits.
One-hundred and seventy-five patients were diagnosed with type 2 diabetes and 29 patients with type 1 diabetes or LADA. The majority of patients (n = 180) were using insulin at baseline and 24 patients were naïve to insulin at baseline. Patient characteristics are shown in Tables 1 and 2. The TDD of insulin was greater in patients with type 2 diabetes than in patients with type 1 diabetes or LADA. Patient-reported baseline TDD was 10% lower than the lower limit and 22% lower than the upper limit of the prescribed insulin dose range. At baseline, the majority of patients (66%) were taking concomitant anti-hyperglycemic medications with 53% of patients included in the study having already escalated treatment to two or more agents. As is to be expected in a comprehensive system where patients are referred for treatment, comorbidities were common with a majority of patients also diagnosed with hypertension (83%) and hyperlipidemia (69%).
Table 1.
Baseline characteristics
| Characteristic | All patients (n = 204) | Type 2 cohort (n = 175) | Type 1/LADA cohort (n = 29) | Insulin cohort (n = 180) | Naïve cohort (n = 24) |
|---|---|---|---|---|---|
| Gender | |||||
| Female | 116 (57) | 100 (57) | 16 (55) | 100 (56) | 16 (67) |
| Male | 88 (43) | 75 (43) | 13 (45) | 80 (44) | 8 (33) |
| Age (years) | 53 ± 13 | 55 ± 12 | 43 ± 13 | 54 ± 12 | 47 ± 13 |
| Range | 21–88 | 21–88 | 23–65 | 23–88 | 21–69 |
| Race | |||||
| Caucasian | 142 (69) | 121 (69) | 21 (72) | 126 (70) | 16 (67) |
| African American | 44 (22) | 38 (22) | 6 (21) | 42 (23) | 2 (8) |
| Undetermined | 18 (9) | 16 (9) | 2 (7) | 12 (7) | 6 (25) |
| Ethnicity: Hispanic | 32 (16) | 30 (17) | 2 (7) | 26 (14) | 6 (25) |
| Duration of diabetes (years) | 13.7 ± 8.4 | 13.2 ± 7.5 | 17.0 ± 12.4 | 14.5 ± 8.3 | 8.0 ± 6.7 |
| Range | 0.1–53 | 0.1–36 | 1.0–53 | 0.5–53 | 0.1–29 |
| Weight (kg) | 96.6 ± 21.1 | 98.0 ± 20.5 | 88.6 ± 23.2 | 97.1 ± 21.2 | 93.3 ± 20.1 |
| Range | 52.7–160.5 | 54.6–160.5 | 52.7–148.6 | 52.7–160.5 | 54.5–130.5 |
| BMI (km/m2) | 34.13 ± 7.43 | 34.62 ± 7.41 | 31.13 ± 6.95 | 34.28 ± 7.56 | 33.00 ± 6.44 |
| HbA1c (%) | |||||
| Mean ± SD | 9.63 ± 1.59 | 9.65 ± 1.62 | 9.48 ± 1.44 | 9.41 ± 1.46 | 11.28 ± 1.63 |
| ≥7% to <9.0% | 80 (39) | 68 (39) | 12 (41) | 78 (43) | 2 (8) |
| ≥9.0% to <10.5% | 62 (30) | 52 (30) | 10 (34) | 56 (31) | 6 (25) |
| ≥10.5% to <14.0% | 62 (30) | 55 (31) | 7 (24) | 46 (26) | 16 (67) |
| FPG (mg/dL) | 201 ± 73 | 196 ± 70 | 248 ± 89 | 197 ± 71 | 238 ± 82 |
| Comorbidities | |||||
| Hypertension | 169 (83) | 153 (87) | 16 (55) | 153 (85) | 16 (67) |
| Hyperlipidemia | 140 (69) | 120 (69) | 20 (69) | 119 (66) | 21 (88) |
| Renal disease | 21 (10) | 18 (10) | 3 (10) | 19 (11) | 2 (8) |
| Coronary artery disease | 27 (13) | 26 (15) | 1 (3) | 25 (14) | 2 (8) |
| Retinopathy | 33 (16) | 26 (15) | 7 (24) | 28 (16) | 5 (21) |
| Neuropathy | 48 (24) | 43 (25) | 5 (17) | 42 (23) | 6 (25) |
Data are n (%) or mean ± SD
BMI body mass index, FPG fasting plasma glucose, HbA1c glycated hemoglobin, LADA latent autoimmune diabetes in adults
Table 2.
Baseline anti-hyperglycemic medications
| Baseline anti-hyperglycemic medication | All patients (n = 204) | Type 2 cohort (n = 175) | Type 1/LADA cohort (n = 29) | Insulin cohort (n = 180) | Naïve cohort (n = 24) |
|---|---|---|---|---|---|
| Basal insulin dose (U/day) | |||||
| Patient reporteda | – | 53 ± 28 | 39 ± 17 | 51 ± 27 | – |
| Lower limit prescribed | – | 56 ± 31 | 41 ± 16 | 54 ± 30 | – |
| Upper limit prescribed | – | 60 ± 31 | 49 ± 22 | 58 ± 30 | – |
| Prescribed range | – | 12–120 | 18–100 | 12–220 | – |
| Insulin TDD (U/day) | |||||
| Patient reporteda | – | 78 ± 46 | 69 ± 31 | 77 ± 44 | – |
| Lower limit prescribed | – | 86 ± 50 | 86 ± 35 | 86 ± 48 | – |
| Upper limit prescribed | – | 98 ± 55 | 104 ± 41 | 99 ± 53 | – |
| Prescribed range | – | 16–310 | 31–180 | 16–310 | – |
| Concomitant medicationsb | |||||
| Metformin | 89 (44) | 80 (46) | 9 (31) | 77 (43) | 12 (50) |
| Sulfonylurea | 43 (21) | 40 (23) | 3 (10) | 34 (19) | 9 (38) |
| GLP-1 receptor agonist | 40 (20 | 37 (21) | 3 (10) | 38 (21) | 2 (8) |
| DPP-4 inhibitor | 18 (9) | 18 (10) | 0 (0) | 16 (9) | 2 (8) |
| DPP-4 I/Metformin | 17 (8) | 17 (10) | 0 (0) | 12 (7) | 5 (21) |
| SGLT-2 inhibitor | 11 (5) | 10 (6) | 1 (3) | 10 (6) | 1 (4) |
| TZD | 8 (4) | 8 (5) | 0 (0) | 8 (4) | 0 (0) |
Data are n (%) or mean ± SD
DDP-4 dipeptidyl peptidase-4, GLP-1 glucagon-like peptide-1, LADA latent autoimmune diabetes in adults, SGLT-2 sodium-glucose co-transporter-2, TDD total daily dose, TZD thiazolidinedione
aPatient reported mean insulin doses reflective for 121, 23, and 142 patients in type 2, type 1/LADA, and insulin cohorts, respectively
bConcomitant medications prescribed for <2% of population not included. Multiple medications are possible per patient
Glycemic Response to V-Go
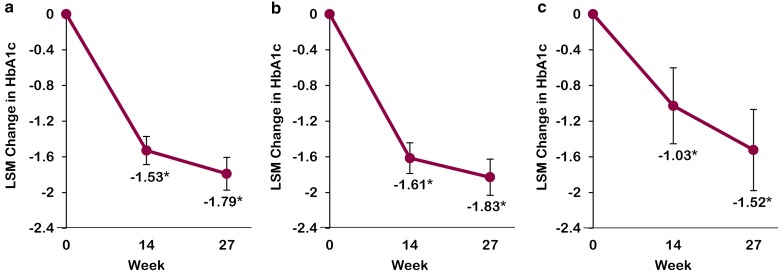
Overall, there was a significant decrease in HbA1c after switching to V-Go across all patient types. The HbA1c LSM change for the overall patient population and by types of diabetes is displayed in Fig. 2. HbA1c results were also analyzed by use of insulin at baseline prior to switching to V-Go. In patients administering insulin at baseline, the reduction in mean HbA1c from baseline to 14 weeks was −1.34% (−1.51% to −1.18%; P < 0.001) and from baseline to 27 weeks was −1.58% (−1.77% to −1.39%; P < 0.001). Patients naïve to insulin prior to baseline experienced the most substantial decrease in mean HbA1c after switching to V-Go, with a reduction in mean HbA1c from baseline to 14 weeks of −2.97% (−3.56% to −2.38%; P < 0.001) and a reduction from baseline to 27 weeks of −3.44% (−4.12% to −2.75%; P < 0.001).
Fig. 2.
Effects of insulin delivery by V-Go on HbA1c. a All patients (n = 204), b patients with type 2 diabetes (n = 175), and c patients with type 1 diabetes or LADA (n = 29). Change in HbA1c reported as LSM with corresponding 95% confidence intervals derived from a repeated measures mixed model for first recorded HbA1c on V-Go (14-week mean) and second recorded HbA1c on V-Go (27-week mean) from baseline (week 0). Time points represent the mean time elapsed between V-Go initiation and follow-up HbA1c for the total population. *P < 0.001 compared to baseline. HbA1c glycated hemoglobin, LADA latent autoimmune diabetes in adults, LSM least-squares mean
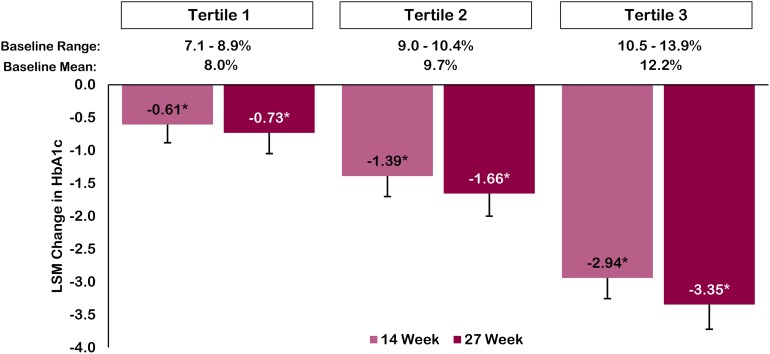
The blood glucose response was evaluated stratifying baseline HbA1c by tertile to determine if baseline HbA1c impacted the level of glycemic change (Fig. 3). Significant and progressive reductions in HbA1c were seen in all three subsets at both the 14-week and 27-week timepoints (P < 0.001).
Fig. 3.
V-Go glycemic response by baseline HbA1c tertile. Tertile 1 (n = 80), tertile 2 (n = 62), and tertile 3 (n = 62). Data are LSM change in HbA1c with corresponding 95% confidence interval derived from a repeated measures mixed model for first recorded HbA1c on V-Go (14-week mean) and second recorded HbA1c on V-Go (27-week mean) from baseline by tertile. Time points represent the mean time elapsed between V-Go initiation and follow-up HbA1c results for the total population. *P < 0.001 compared to baseline. HbA1c glycated hemoglobin, LSM least-squares mean
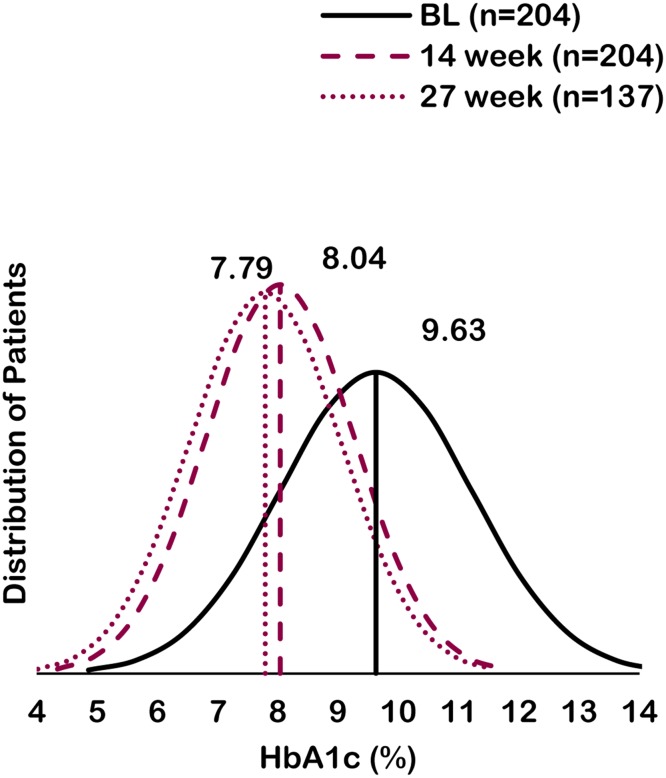
The distribution of HbA1c values for the study population at baseline was compared to the distribution at both follow-up HbA1c time points. Figure 4 plots the distribution of HbA1c values and presents overall arithmetic mean values at baseline, 14, and 27 weeks. On V-Go, the HbA1c distribution curve has narrowed and progressively shifted to the left, representing a reduction in variability and lower HbA1c values.
Fig. 4.
Change in HbA1c distribution. HbA1c data are arithmetic means at baseline (week 0) compared to first recorded HbA1c on V-Go (14-week mean) and second recorded HbA1c on V-Go (27-week mean). Curves represent the HbA1c distribution of patients for each time point based on available data. BL baseline, HbA1c glycated hemoglobin
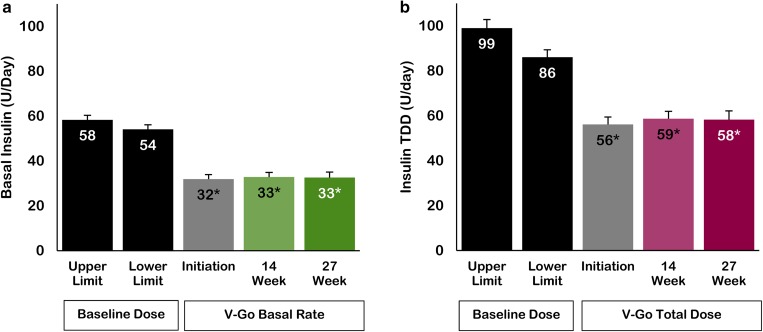
Insulin Dose on V-Go
Prescribed daily basal insulin and TDD at V-Go initiation, 14, and 27 weeks were analyzed after switching to V-Go for those patients administering insulin prior to V-Go (Fig. 5). For both TDD and basal insulin doses, there were statistically significant reductions in insulin requirements after switching to V-Go (P < 0.001). At 27 weeks, TDD on V-Go was 33% lower than the lower limit and 41% lower than the upper limit of the prescribed baseline dose range. Basal insulin rates were 39% lower than the lower limit and 46% lower than the upper limit of the prescribed baseline dose range. The mean daily insulin dose administered with V-Go at week 27 was 0.6 ± 0.19 units/kg/day. At both follow-up visits only 8.8% of patients received supplemental insulin, which was included in the reported insulin dosage during V-Go use.
Fig. 5.
Insulin dosage. a Basal insulin dose/rate. b Insulin TDD. Data reflects insulin cohort (n = 180). Insulin data are LSM with corresponding 95% confidence intervals derived from a repeated measures mixed model for baseline upper and lower limit prescribed dose range compared to V-Go initiation dose, dose at first recorded HbA1c on V-Go (14-week mean), and dose at second recorded HbA1c on V-Go (27-week mean). *P < 0.001 compared to baseline lower limit prescribed dose. HbA1c glycated hemoglobin, LSM least-squares mean, TDD total daily dose
Based on the significant reduction in basal insulin, a follow-up analysis was conducted to evaluate if the reduction in basal insulin dose impacted fasting plasma glucose. A paired t test analysis at 27 weeks demonstrated a significant reduction (−46 mg/dL from an arithmetic mean baseline of 182 mg/dL; P < 0.001) in a subset of patients (n = 67) with repeated fasting plasma glucose measures available in the EMR. This significant reduction occurred despite a 44% reduction (61 to 34 units/day; P < 0.001) in basal insulin for this subset.
In patients naïve to insulin at baseline the mean TDD of insulin was 54 units at 27 weeks. Of this mean TDD 57% was basal insulin and 43% was mealtime bolus insulin.
Mean insulin dose during V-Go use remained stable. However, reflected in this relatively stable mean dose are increases and decreases in basal and bolus doses by individual patients. Insulin titrations were analyzed separately for basal insulin and bolus insulin. The majority of titration occurred between baseline and 14 weeks. Increases in basal rate occurred in 24% of patients initiated on V-Go 20 or 30, and decreases in basal rate occurred in 6% of patients initiated on V-Go 30 or 40. Overall, nearly half of all patients had a titration in bolus dose with 27% increasing and 21% decreasing bolus dose use.
Evaluation of Efficacy Based on Changes to Concomitant Medications
Changes to concomitant anti-hyperglycemic medications were reviewed and data was analyzed to assess whether changes to concomitant medications may have impacted study outcomes. One-hundred and ten patients had no change to concomitant medications, 43 patients had increases, and 39 patients had decreases in concomitant medications. Twelve patients implemented multiple changes and were not able to be categorized. HbA1c, TDD of insulin, and weight prior to V-Go and at 14 weeks were compared for patients with increases, decreases, and no changes to anti-hyperglycemic concomitant medications (Table 3).
Table 3.
Clinical measures at baseline and on V-Go based on change in concomitant anti-hyperglycemic medications
| Clinical measure | Initiation of V-Go+ | ||
|---|---|---|---|
| No change in anti-hyperglycemic medication(s) (n = 110) | Increase in anti-hyperglycemic medication(s) (n = 43) | Decrease in anti-hyperglycemic medication(s) (n = 39) | |
| HbA1c (%) | |||
| Baseline | 9.48 (9.22–9.74) | 10.04 (9.62–10.46) | 9.35 (8.91–9.79) |
| On V-Go | 8.09 (7.83–8.35) | 8.08 (7.66–8.50) | 8.03 (7.59–8.47) |
| Insulin TDD (U/day) | |||
| Baseline | 80 (74–86) | 112* (102–123) | 65 (54–77) |
| On V-Go | 56 (50–62) | 68 (58–78) | 53 (43–64) |
| Weight (kg) | |||
| Baseline | 93 (89–97) | 105* (99–111) | 93 (87–100) |
| On V-Go | 94 (90–98) | 107* (101–114) | 95 (89–102) |
Data are least-squares mean with corresponding 95% confidence intervals derived from a repeated measures mixed model based on 14-week results. Baseline insulin TDD reflects prescribed lower limit TDD. Only those changes in concomitant anti-hyperglycemic medication(s) providing sufficient time for clinical effect were categorized as an increase or decrease
HbA1c glycated hemoglobin, TDD total daily dose
* P < 0.01 compared to same measure for both no change and decrease in concomitant anti-hyperglycemic medication(s)
All three groups experienced a significant reduction in HbA1c after switching to V-Go irrespective of changes to concomitant medications. There was no significant difference in HbA1c between the groups at baseline, nor at week 14, confirming that changes to concomitant medications were not a factor in the reduction in HbA1c seen with V-Go use. At baseline, patients with an increase in concomitant medications had a significantly higher mean TDD of insulin (P < 0.01); however, there was no significant difference in mean TDD between any of the groups after switching to V-Go. Patients with an increase in concomitant medications had a significantly higher mean weight at both baseline and on V-Go compared to patients with a decrease or no change in concomitant medications (P < 0.01).
Among all subjects there was a significant change in weight from baseline with insulin delivery by V-Go (P < 0.001). LSM weight was 96.6, 97.9, and 98.1 kg at baseline and at 14 and 27 weeks after switching to V-Go, respectively. Hypoglycemia captured from charts was similar during V-Go use compared to baseline with rates of 19, 20, and 22% at baseline, 14, and 27 weeks, respectively. One case of severe hypoglycemia was reported by a patient administering a basal rate of 20 units per day with V-Go and no bolus insulin. The patient did not require third party assistance and continued to use V-Go. Of the 204 subjects included in the study, 32 discontinued use of V-Go prior to the second HbA1c follow-up for reasons including: skin irritation (9), cost/insurance coverage (7), transitioned to an insulin pump (5), weight gain (2), undetermined reason (2), and did not prefer V-Go, pain, GI effect, hyperglycemia, hypoglycemia and lack of adherence to skin (1 each). Patient baseline characteristics were similar between those that continued therapy and those that discontinued V-Go.
Discussion
In this study, we examined the outcomes of 204 patients after being switched to insulin therapy delivered by V-Go. Due to the progressive nature of diabetes, treatment intensification is required to maintain acceptable blood glucose control and decrease the risk of adverse outcomes. Insulin is the most consistently effective and potent way to improve blood glucose control [16, 17]. Guidelines recommend basal insulin therapy plus mealtime boluses as a treatment intensification option delivered by either MDI or continuous subcutaneous infusion [18]. This retrospective analysis identified patients from a specialized comprehensive diabetes care clinic setting who had not achieved adequate blood glucose control with their current treatment regimen and were changed to insulin delivery with V-Go according to clinician judgment. The multi-clinic system treats a large number of patients who are referred from primary care sites for specialized care, which is reflected in the mean duration of diabetes of 13.7 years and a baseline HbA1c of 9.63% in the study population. After switching to V-Go, glycemic control improved regardless of patient type, baseline TDD, HbA1c, or treatment regimen used prior to V-Go, and this improvement was accomplished with a significantly lower TDD of insulin. The nearly 1.8% decrease in mean HbA1c seen after 27 weeks of V-Go use is clinically meaningful for any diabetic population, and it is even more significant considering the study population included difficult to manage patients referred for specialized care. The greatest number of diabetes complications may be avoided by improving glycemic control in patients with very poor control [19]. Sixty percent of patients included in the study had baseline HbA1c values over 9%, and 30% of patients included in the study had baseline HbA1c values over 10.5%. Patients in this highest HbA1c subset over 10.5% had substantial and statistically significant decreases in HbA1c with reductions of nearly 3% at 14 weeks and 3.35% at 27 weeks. As commonly reported for other diabetes treatments, the higher the baseline HbA1c at the time of treatment initiation, the greater the reduction in HbA1c.
Because insulin regimens can impact daily routines and lifestyles, convenience and ease of administration are a consideration when initiating and titrating insulin regimens. Intensification from basal insulin therapy to MDI therapy may be delayed due to the inconvenience of multiple injections and patients often do not adhere to a MDI regimen especially when injections are required to be taken outside the home. Data from this study for insulin dosing prior to V-Go use support this lack of adherence; in patients using insulin prior to V-Go, the patient-reported TDD of insulin dose was 10% lower than the lower limit and 22% lower than the upper limit of the prescribed range, confirming that patients were using less insulin than prescribed. V-Go may improve adherence with administering bolus doses considering insulin is readily available and can be discreetly administered [13]. A previous study noted patient satisfaction with V-Go stating it was simple to use, discreet, and comfortable to wear [11].
V-Go is indicated for any adult patient requiring insulin regardless of type of diabetes or use of concomitant anti-hyperglycemic medications. V-Go delivers a consistent and continuous basal insulin rate over a 24 h period, which may offer improved efficiency over subcutaneous basal injections. The on-demand bolus dosing feature may ease the transition to basal-bolus therapy when mealtime insulin is required in patients prescribed a basal only regimen or those naïve to insulin. Furthermore, in patients using MDI, the ability to deliver mealtime insulin as needed without an additional injection may facilitate patients getting the insulin they need to improve their glycemic control.
Fear of hypoglycemia has been reported as a reason patients delay starting insulin therapy [20] but in this study there was no difference in patient-reported hypoglycemia after switching to insulin therapy with V-Go. Fear of weight gain has been reported as another reason for delay in treatment intensification [20]. Patients in the study saw a mean increase in weight of only 1.5 kg from baseline to 27 weeks after switching to V-Go. Although the prescribed dose of insulin decreased, patients were likely administering their insulin more appropriately enabling a more efficient cellular uptake of glucose resulting in rehydration and weight gain. This change in weight was well-within what is expected with insulin therapy, and although the change was statistically significant, it was not clinically relevant.
Varying titration practices across clinicians in our centers could have impacted study results. The majority of titration that occurred was related to mealtime bolus dosing; however, no titration of bolus dosages occurred in approximately 50% of patients. It is likely that even greater reductions in HbA1c could have been achieved with additional insulin titration.
The V-Go insulin delivery device delivers a maximum of 76 units/day. In the current study, V-Go adequately met the insulin requirements of over 90% of study patients without the need for supplemental insulin, which is clinically significant considering the study included patients prescribed a range of insulin up to 310 units per day at baseline.
Study outcomes were analyzed according to subsets of patients who had an increase, a decrease, or no change to concomitant anti-hyperglycemic medications. The analysis showed that patients with an increase in concomitant medications weighed significantly more and were prescribed a higher TDD of insulin prior to V-Go use than those patients with no change or a medication decrease. This is not surprising, as higher insulin doses are typically prescribed in patients with increased body weight, and it is reasonable to escalate treatment with an additional medication in patients already receiving a high TDD of insulin. After 14 weeks on V-Go patients with an increase in concomitant medication continued to have a significantly higher weight; however, there was no difference in TDD of insulin used with V-Go between patients with an increase in medications and patients with a decrease or no change in concomitant medications. Additionally, all patients had a similar decrease in HbA1c regardless of concomitant medication status, which supports the conclusion that the addition or removal of concomitant medications did not impact the effectiveness of V-Go.
There are several limitations in our current investigation. The study was a retrospective database analysis and the current analysis did not include a parallel control group. The baseline data of the study group served as the control comparison and a systematic and careful review was performed to identify patients switched to V-Go to ensure there was no sample selection bias. Additionally, there were no educational initiatives or practice changes implemented during the study timeframe that could have contributed to improvement of glycemic control after patients switched to V-Go. To be included in the analysis, patients were required to have at least one follow-up office visit with an HbA1c result recorded so the data in our study may not be representative of all patients initiating V-Go therapy as discontinuation prior to a follow-up HbA1c was possible. Additionally, at the close of the analysis period 35 of the patients included had not returned for a second follow-up visit and, therefore, it is unknown whether or not they remained on V-Go after the first follow-up visit. Frequency of patient contact, forced insulin titration, and strict patient and practice adherence measures were not enforced, which reflects real-world diabetes management and standard of care. This may be considered a limitation as greater reductions in HbA1c may have been possible with additional patient contact and titrations, both in the study patients and as a standard of care. Analysis of insulin use relied on the prescribed ranges and patient reported use available in medical records; actual patient use may have differed. Hypoglycemia was self-reported by patients and recorded in medical records. In our experience, patients report any clinically relevant hypoglycemic event during their office visits, and events reported by patients are consistently recorded in medical records. No change in data recording process was made during the study timeframe, so these data limitations were consistent across baseline and V-Go visits and are not felt to have impacted the study conclusions.
Conclusions
Our study supports the safety and effectiveness of V-Go in improving glycemic control in patients with sub-optimally controlled diabetes requiring insulin. V-Go is an appropriate therapy for a broad range of patients; statistically significant reductions in HbA1c were seen with V-Go use in all subsets of patients including type 2, type 1/LADA, naïve to insulin, and patients administering insulin prior to V-Go. Reports of hypoglycemia were similar prior to and after switching to V-Go. Patients administering insulin at baseline experienced substantial decreases in HbA1c while requiring a lower TDD of insulin. V-Go offers an efficient and efficacious method of insulin delivery that can enhance patient compliance and optimize glycemic control.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
No funding or study product was provided to the study site, study participants, or study investigators. Valeritas, Inc., Bridgewater, NJ, USA provided funding for investigational review board review. The article processing charges for this publication were funded by Valeritas, Inc. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published. The authors would like to thank Donna Doherty, MS, RD, LD, CDE for assistance in data collection and study conduct, and Jessica Sanders and Ariel Webb from the University of Central Oklahoma for support with statistical analyses. The authors received writing/editorial support for manuscript preparation from Maria Paluselli, founder of Panaceum Clinical, LLC, funded by Valeritas, Inc.
Disclosures
Rosemarie Lajara has received speaker or consulting honorariums from Valeritas, Novo Nordisk, Astra Zeneca, Boehringer Ingelheim and Takeda. Dianne A. Fetchick and Tracy L. Morris declare they have no conflicts of interest. Carla Nikkel is currently employed and a shareholder of Valeritas, Inc. Findings from a portion of the dataset used in preparing this manuscript were presented at the Academy of Managed Care Pharmacy, American Association of Clinical Endocrinologists, American Diabetes Association, and the American Association of Diabetes Educators scientific sessions earlier this year (see the electronic supplementary material for full details).
Compliance with ethics guidelines
This study was reviewed and approved by Allendale investigational review board, and a waiver of informed consent was approved. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
References
- 1.American Diabetes Association (ADA). National Diabetes Statistics Report 2014. http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. Accessed 11 Aug 2015.
- 2.Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gallwitz B, Bretzel RG. How do we continue treatment in patients with type 2 diabetes when therapeutic goals are not reached with oral antidiabetes agents and lifestyle? Incretin versus insulin treatment. Diabetes Care. 2013;36(Suppl 2):S180–S189. doi: 10.2337/dcS13-2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holman RR, Farmer AJ, Davies MJ, et al. Three-year efficacy of complex insulin regimens in type 2 diabetes. N Engl J Med. 2009;361:1736–1747. doi: 10.1056/NEJMoa0905479. [DOI] [PubMed] [Google Scholar]
- 5.Asche CV, Bode B, Busk AK, Nair SR. The economic and clinical benefits of adequate insulin initiation and intensification in people with type 2 diabetes mellitus. Diabetes Obes Metab. 2012;14:47–57. doi: 10.1111/j.1463-1326.2011.01487.x. [DOI] [PubMed] [Google Scholar]
- 6.García-Pérez LE, Álvarez M, Dilla T, Gil-Guillén V, Orozco-Beltrán D. Adherence to therapies in patients with type 2 diabetes. Diabetes Ther. 2013;4:175–194. doi: 10.1007/s13300-013-0034-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peyrot M, Rubin RR, Kruger DF, Travis LB. Correlates of insulin injection omission. Diabetes Care. 2010;33:240–245. doi: 10.2337/dc09-1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peyrot M, Barnett AH, Meneghini LF, Schumm-Draeger PM. Factors associated with injection omission/non-adherence in the Global Attitudes of Patients and Physicians in Insulin Therapy study. Diabetes Obes Metab. 2012;14:1081. doi: 10.1111/j.1463-1326.2012.01636.x. [DOI] [PubMed] [Google Scholar]
- 9.Roper Global Diabetes Program. GfK Healthcare’s Roper US Diabetes Patient Market Study. 2011.
- 10.Valeritas, Inc. V-Go instructions for patient use. ART-037 Rev: H 09/2011. http://www.go-vgo.com/sites/default/files/upload/instructions-for-patient-use.pdf. Accessed 11 Aug 2015.
- 11.Rosenfeld CR, Bohannon NJ, Bode B, et al. The V-Go insulin delivery device used in clinical practice: patient perception and retrospective analysis of glycemic control. Endocr Pract. 2012;18(5):660–665. doi: 10.4158/EP11362.OR. [DOI] [PubMed] [Google Scholar]
- 12.Johns BR, Jones TC, Sink JH, Cooke CE. Real-world assessment of glycemic control after V-Go® initiation in an endocrine practice in the southeastern United States. J Diabetes Sci Technol. 2014;8(5):1060–1061. doi: 10.1177/1932296814537041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Winter A, Lintner M, Knezevich E. V-Go insulin delivery system versus multiple daily injections for patients with uncontrolled type 2 diabetes mellitus. J Diabetes Sci Technol. 2015;9(5):1111–1116. doi: 10.1177/1932296815580361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bode BW, Sabbah HT, Gross TM, Fredrickson LP, Davidson PC. Diabetes management in the new millennium using insulin pump therapy. Diabetes Metab Res Rev. 2002;18(Suppl 1):S14–S20. doi: 10.1002/dmrr.205. [DOI] [PubMed] [Google Scholar]
- 15.Reznik Y, Cohen O, Aronson R, et al. Insulin pump treatment compared with multiple daily injections for treatment of type 2 diabetes (OpT2mise): a randomised open-label controlled trial. Lancet 2014;384(9950):1265–1272. [DOI] [PubMed]
- 16.Owens DR. Stepwise intensification of insulin therapy in Type 2 diabetes management—exploring the concept of the basal-plus approach in clinical practice. Diabet Med. 2013;30(3):276–288. doi: 10.1111/dme.12019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nathan DM, Buse JB, Davidson MB, et al. Medical management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2009;32(1):193–203. doi: 10.2337/dc08-9025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Handelsman Y, Bloomgarden ZT, Grunberger G, et al. American Association of Clinical Endocrinologists and American College of Endocrinology—clinical practice guidelines for developing a diabetes mellitus comprehensive care plan—2015. Endocr Pract. 2015;21(Suppl 1):1–87. doi: 10.4158/EP15672.GLSUPPL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Diabetes Association (ADA) Standards of medical care—2015. Diabetes Care. 2015;38(Suppl. 1):S58–S66. doi: 10.2337/dc15-S012. [DOI] [PubMed] [Google Scholar]
- 20.Peyrot M, Rubin RR, Lauritzen T, et al. International DAWN Advisory Panel. Resistance to insulin therapy among patients and providers: results of the cross-national Diabetes Attitudes, Wishes, and Needs (DAWN) study. Diabetes Care. 2005;28:2673–2679. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.